Obesogenic environment
 From Citizendium - Reading time: 11 min
From Citizendium - Reading time: 11 min
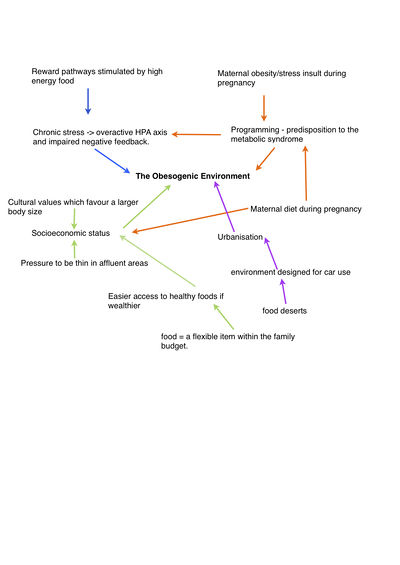
The obesogenic environment encompasses the environmental features of modern lifestyles that are postulated to contribute to the increasing prevalence of obesity; in particular, it is thought that the wide availability of food that is energy dense, palatable and inexpensive, combined with increasingly sedentary habits, favour an excess of energy intake over expenditure.[1]
The obesogenic environment.[edit]
Over the past 40 years the prevalence of obesity has become a cause for concern. The dramatic rise in rates of obesity amongst both adults and children means that, across the world, 1.46 billion adults and 70 million children are estimated to be overweight or obese in 2008[2], so what is it that is making us fat?
In 2011 the leading medical journal The Lancet published a series of articles on obesity[2]; these made a number of suggestions as to why obesity rates have risen, and continue to rise, so rapidly. Perhaps it is our environment that is to blame, and that obesity represents ‘a normal reaction to an abnormal environment.[2]
The notion that the environment may be associated with obesity is not new, with Rimm and White arguing over 25 years ago that obesity was a product of the environment. However, the term 'obesogenic environment' has recently been defined as 'the sum of influences that the surroundings, opportunities, or conditions of life have on promoting obesity in individuals or populations'.
Modern lifestyles.[edit]
Chronic stress and obesity.
In the UK, the number of people reporting feeling stressed has doubled since the 1990’s[3], even though the hours spent at work in the UK is average amongst other European countries,[4] the amount of unpaid work, mainly caring for children and housework done predominately by women is above average compared to other countries within the EU[4]. This survey only took into account the working population, suggesting that even though, the amount of time spent at work hasn’t increased, juggling family commitments and employment may lead to increased rates of stress related ill health.
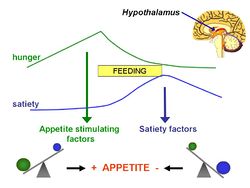
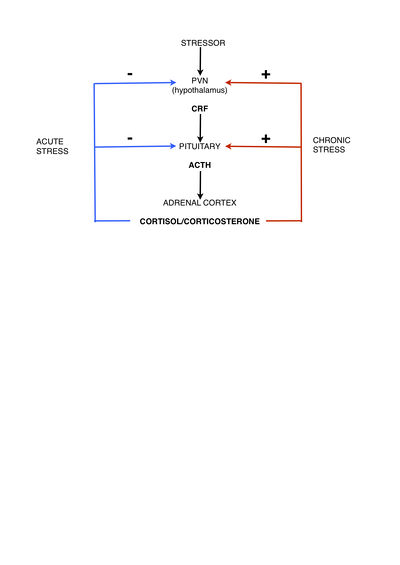
So, is it our fault we are getting fat? Experimental studies in laboratory animals show a clear relationship between stress and obesity; being chronically stressed increases the amount of 'comfort food' ingested by rats[5]. Chronic stress as opposed to acute stress, results in increased concentration of glucocorticoids (cortisol in humans and corticosterone in rodents) over a prolonged period of time[6]. High levels of glucocorticoid over a long period, rather than negatively feeding back on the hypothalamo-pituitary-adrenal (HPA) axis reducing the amount of glucocorticoids produced, become excitatory [6]. This is important and accounts for the differences in the reaction between acute and chronic stress responses. Eating ‘comfort food’, defined as food high in carbohydrate and sugar,[5] is proposed to dampen down the HPA axis decreasing anxiety levels associated with the excitatory effect of prolonged high glucocorticoid levels. Increased cortisol levels correlate with obesity, as seen in Cushing’s disease where a pathological overproduction of cortisol because of abnormal stimulation of the HPA axis leads to abdominal obesity. This increase in cortisol is also seen in stress and depressed individuals as compared to a control group.[7] But which comes first, the increase in cortisol or the obesity? Adipose tissue contains the enzyme 11-beta hydroxysteroid type one which converts inactive cortisone to cortisol, the more adipose tissue you have the more conversion[7], thus breaking this cycle may be important in tackling obesity. There is also significant evidence that high stress levels, leading to high cortisol levels, during pregnancy can lead to a predisposition for the offspring to be of a low birth weight who then go on to develop many of the adverse effects associated with obesity, predominantly the metabolic syndrome later in life.[8] The placenta forms the barrier between mother and fetus, and contains mechanisms to prevent the fetus from being overly exposed to high cortisol levels, this protection comes in the form of the enzyme 11 beta hydroxysteroid dehydrogenase type 2 which, in humans, converts active cortisol to inactive cortisone. Mothers who are exposed to high stress levels or who are given exogenous steroids override this enzyme barrier resulting in increased exposure of the fetus to glucocorticoids.These offspring have overexpression of glucocorticoid receptors in adipose tissue and an impaired response to stress.[8] Interestingly, in studies performed on rats, the alteration in receptors in the brain is also seen when pregnant rats are exposed either to psychosocial stress or exogenous glucocorticoid administration. The levels of mineralcorticoid receptors in the brains of these offspring are markedly reduced compared to their control counterparts.[9] This may be an important underlying reason for the hyperactivity of the HPA axis and the impaired negative feedback. There is also a reduction in the number of CRH type 2 receptors - these receptors produce anxiolytic behaviour, and an increase in CRH type one receptors which mediate the stress response. [9] This is interesting in relation to some of the chronic long term outcomes which are associated with fetal programming, depression is associated with increased CRH levels in the CSF and impaired negative feedback, and chronic stress is associated with high glucocorticoid levels and obesity - maternal stress seems to confound the effects making offspring more predisposed to these conditions. The rat model which was exposed to an exogenous glucocorticoid, dexamethosone, showed similarities to those exposed to psychosocial stress, however the offspring had a reduced number of both glucocorticoid receptors and mineralcorticoid receptors, suggesting higher level of impaired negative feedback. This model is useful for looking at the long term consequences of clinical practice in which steroids are given to pregnant women who are at risk of preterm labour in order for fetal lung development, rather than as a model for social stress as dexamethosone freely crosses the placenta. [9] So it seems stress insult during pregnancy causes adverse programming in the fetus, so it seems advantageous to have an attenuated stress response whilst pregnant to avoid high levels of glucocorticoids. This is the case in rats, but only occurs in later pregnancy, the response to any stressor (physical, psychological, immune) ACTH response is significantly reduced compared to virgin controls. This is thought to be caused by local endogenous opioid production which prevent neurone firing, it is also thought that this is mediated by allopregnanolone, a neuroactive progesterone metabolite, which is present in high levels in the later stages of pregnancy. Using a opioid receptor antagonist, naloxone, or a 5 alpha reductase inhibitor returns the HPA axis back to normal.[9]
Being obese in pregnancy also has a negative effect on the health of the offspring, and the prevalence of obesity in pregnancy is increasing.[10] The timing may be critical for the impact on the offspring, whether there is over nutrition during pregnancy or during both pregnancy and lactation.[10]It is suggested that maternal over-nutrition directly affects fetal brain development causing altered appetite, adipocyte differentiation and reduced energy expenditure.[10] Converse to the low birth weight, and subsequent ‘catch up growth,’ in children exposed to high glucocorticoid levels, in maternal obesity results in increased birth weight and a predisposition to being obese in childhood.[10]
Studies in people have also show that maternal diet in pregnancy, particularly one which is high in protein and low in carbohydrates, results in an overactive HPA axis and increased cortisol release in response to stress.[11] Interestingly it seems that the negative effects of ‘fetal programming’ are not limited to the direct offspring, but can also affect the next generation as well; research is currently being undertaken to see whether the next generation (the great grandchildren of the mother who received the original insult) are affected.
Socioeconomic status and obesity
Obesity rates vary across the globe and obesity can result from being both relatively rich or relatively poor, but this is related to the HDI of the particular country. In simple terms, if you are rich in a poor country you are likely to be obese. If you are poor in a rich country you are likely to be obese.
The prevalence of obesity is determined by both an individual’s socioeconomic status and the value of the countries Human development Index (HDI)?
A positive association is if you have a higher socioeconomic status then you are more likely to be fat.
A negative association is a lower socioeconomic status associated with a larger body size.
Originally looked into by Sobal and Stunkard in 1989 [12] and by McLaren in 2007[13], was the relationship between proportions of positive and negative associations as one moves across countries with a high human development index (HDI) to middle to lower.
McLaren's findings were similar to that of Sobal and Stunkard; Countries with a lower HDI had a larger proportion of positive associations than those with higher HDI, whilst the more developed countries with higher HDI values had a larger proportion of negative associations.
Why are obesity rates higher amongst those from a lower socioeconomic status than from a more wealthy background in a developed country?
It is widely thought that individuals from higher socioeconomic groups are able to purchase the commonly more expensive yet healthier foodstuffs, such as fruit, vegetables and lower fat milk. [14]
Bourdieu’s concept of “habitus” uses the concept of the body as a 'social metaphor' of a person’s status. A thin and slender body is likely to be more socially valued and materially viable than a fat one. Even in an obesogenic environment, these conceptual ideas may help maintain differences between classes for whom thinness is thought of an ideal of physical beauty.[15]
McLaren’s review also touched on location affluence. People that live in an affluent area have heightened pressure to be thin.[16], As well as the local amenities for physical activity and healthy food stuffs.
Why are obesity rates higher amongst those from a high socioeconomic status in a developing country?
It was covered in McLaren’s review, the suggestion by Monteiro that patterns of high energy expenditure among the poor and the cultural values that favour a larger body size, are likely to also contribute to the positive associations seen in low HDI countries. (Mentioned above) ,[17]
As a country's GDP increases, this causes a shift of obesity towards those with a lower SES.6
Urbanization and Car Reliance[edit]
Urbanization has occurred rapidly in many different places, with generally few restrictions on urban sprawl being implemented by local and national governments. In some cases this has lead to poorly designed suburbs with little thought being put into health and fitness. Along with the housing and other buildings, the infrastructure within and between these suburbs does not get designed from an active transport mindset. A case study, carried out in Australia, suggested that the transport systems there were largely designed for cars rather than people, resulting in urban environments with poor walkability, bikeability and public transport services[18]15. As a result of this, the amount of exercise taken by individuals will decrease because, for many people, exercise is not a necessity and will only be taken it if it is convenient.
As suburban sprawl expands, it often becomes a considerable distance to travel to various destinations (shops, schools, work, public transport and services). In these suburban environments, inactivity and obesity are shown to be common[19], mainly due to the fact that it is necessary to take transport rather than walk or cycle if the destinations were closer. Having said this, other studies have shown sharp decreases in the amount of active transport in places where land use, connectivity, population density etc have stayed roughly the same. This suggests that social influence plays an important role in the changes seen, and in particular in the shift towards a car reliant culture.
As suburbs have kept springing up, the centres of activity (ie. shopping malls, food outlets) have moved out of town, as the land and running costs are often cheaper than in the city centres and the possibility of expansion is greater. This is matched with a decrease in local access and encourages car use as the public transport links to these areas are often inadequate and infrequent, therefore placing restrictions on the freedom and independence of individuals which would not be present with the use of a car. As well as centres of activity relocating, many businesses have relocated out of town to take advantage of lower costs. This means that many people are commuting to more remote areas that are not likely to be covered efficiently by public transport, cycle lanes and so on, again increasing the need for a car and removing the small bit if exercise than an individual would get walking 500m to the bus stop for example.
As the need to own a car increases, the financial burden on many families and individuals is significant. Studies have shown that food is seen as a flexible item within the controllable household budget[20] so as the families’ finances are squeezed, the money spent on food is likely to decrease, with lower quality food and less healthy food being purchased, as these groups are generally lower in price. For low income groups who cannot afford a car, there is high dependence on local corner shops, which often stock less healthy foods and are more expensive than the large out of town supermarkets[21]. Looking at this issue from a different slant, as more households own a car, a larger supermarket shop can be done, meaning that for most of the time there is an abundance of food in the house which undoubtedly leads to unhealthy snacking and overeating in some cases. Even in households without a car, the introduction of delivery services from major supermarkets may lead to the same result.
Freund and Martin[22] suggest that the freedom and autonomy originally offered by the car is displaced by the necessity of having a car to keep up with the culture and lifestyle of today. It could be argued that, in most cases, individuals or families that own a car do in fact need it for something, and since they have a car, it gets used for all sorts of other journeys that wouldn’t have needed a car, and that could have been undertaken on foot, by bicycle or other more exercise friendly methods, therefore contributing to the significant increase in obesity seen in recent years.
Conclusion[edit]
In conclusion, the term 'obesogenic environment' in relation to the influence of environmental factors of modern lifestyle and society, such as chronic stress, socioeconomic status, urbanization and car reliance, has become a major talking-point in obesity research.
The influence of high glucocorticoid levels observed in individuals suffering from chronic stress has been shown to have a significant link with obesity, also portrayed through Cushing's Syndrome (high cortisol levels due to abnormal HPA axis stimulation) and its characteristic abdominal obesity. The effect of stress and glucocorticoids during pregnancy has also shown significance in determining obesity, with mothers exposed to stress during gestation altering the enzyme composition of the maternal-placental barrier thus allowing elevated exposure of glucocorticoids to the foetus, which has been shown to not alone affect their subsequent stress response and cognitive ability, but also predispose these individuals to aspects of the metabolic syndrome in adult life.
The influence of socioeconomic status was seen to be significant through individuals' continual exposure to 'healthy' yet expensive foods (ie. organic food stuff, low fat etc) whilst fatty/sugary foods tend to be less expensive and more available to individuals on a lower income.
Car reliance and the subsequent lack of exercise is an evident factor in the rising obesity epidemic. With the increasing need to owning a car affecting family finances, this prevents food from becoming a financial necessity and thus the budget spent in this area is tightened, resulting in perhaps lesser quality/beneficial food being purchased. Also, we are frankly becoming too reliant on the general ease of driving to our out-of-town destinations.
Overall, environmental factors here simply determining the availability and consumption of food and the levels of physical activity undertaken by individuals, are hugely significant and play an essential role in our current obese population.
References[edit]
- ↑ Chaput JP et al. (2011) Modern sedentary activities promote overconsumption of food in our current obesogenic environment Obes Rev 12:e12-20 PMID 20576006
- ↑ 2.0 2.1 2.2 Rutter H (2011) Where next for obesity? Lancet
- ↑ Health and safety executive, Work related stress-together we can tackle it
- ↑ 4.0 4.1 Parent-Thirion A (2007) Fourth European working conditions survey. European foundation for the improvement of living and working conditions.
- ↑ 5.0 5.1 Dallman M et al. (2003) Chronic stress and obesity: a new view of "comfort food PNAS 100: 11696-701
- ↑ 6.0 6.1 Pecorano N et al.(2004) Chronic stress promotes palatable feeding which reduces signs of stress: feedforward and feedback effects of chronic stress. Endocrinology 145: 3754-62
- ↑ 7.0 7.1 Foss B, Drystad SM (2011) Stress in obesity: cause or consequence? Med Hypotheses 77:7-10
- ↑ 8.0 8.1 Seckl J (2004) Prenatal glucocorticoids and long term programming Eur J Endocrinol 151:49-62
- ↑ 9.0 9.1 9.2 9.3 Brunton PJ and Russell J. Neuroendocrine control of maternal stress response and fetal programming by stress in pregnancy. (2011) Progress in Neuro-Psychopharmacology and biological psychiatry. (35): 1178-1191.
- ↑ 10.0 10.1 10.2 10.3 Drake A, Reynolds R (2010) Impact of maternal obesity on offspring obesity and cardiometabolic disease risk Reproduction 140:387-98
- ↑ Reynolds R et al.(2007) Stress responsiveness in adult life: Influence of mother’s diet in late pregnancy J Clin Endocrinol Metabol 92:2208-10
- ↑ Sobal J, Stunkard AJ (1989) Socioeconomic status and obesity: a review of the literature. Psychol Bull 105:260–75
- ↑ McLaren L (2007) Socioeconomic status and obesity Epidemiologic Reviews 29:29–48
- ↑ Power EM (2005) Determinants of healthy eating among low-income Canadians Can J Public Health 9:S37–8
- ↑ Rubinstein S, Caballero B (2000) Is Miss America an undernourished role model? (Letter). JAMA 283:1569
- ↑ McLaren L, Gauvin L(2003) Does the ‘average size’ of women in the neighbourhood influence a woman’s likelihood of body dissatisfaction? Health Place 9:327–35
- ↑ Monteiro CA et al. (2004) Socioeconomic status and obesity in adult populations of developing countries: a review Bull World Health Organ 82:940–6
- ↑ Mees P, O’Connell J, Stone J. (2008). Travel to work in Australian capital cities. 1976-2006. “Urban Policy and Research” 26(3): 363-78.
- ↑ Garrard, J. 2009. Taking action on obesogenic environments: Building a culture of active, connected communities. National Preventative Health Taskforce.
- ↑ Friel S, Conlon C. Food Poverty and Policy. Ireland: Combat Poverty Agency; 2004.
- ↑ Friel S, Harrington J, Thunhurst C., et al Standard of Healthy Living on the Island of Ireland. Cork: Food Safety Promotion Board; 2005.
- ↑ Freund, P., Martin, G., 1996. The commodity that is eating the world: the automobile, the environment, and capitalism. Capitalism, Nature and Socialism 7, 3–29.
 KSF
KSF