Ayurveda
Topic: Chemistry
 From HandWiki - Reading time: 34 min
From HandWiki - Reading time: 34 min
| This article is part of a series on |
| Alternative and pseudo‑medicine |
|---|
 |
Ayurveda (/ˌɑːjʊərˈveɪdə, -ˈviː-/)[1] is an alternative medicine system with historical roots in the Indian subcontinent.[2] The theory and practice of Ayurveda is pseudoscientific.[3][4][5] The Indian Medical Association describes Ayurvedic practitioners who claim to practice medicine as quacks.[6] Ayurveda is heavily practiced in India and Nepal, where around 80% of the population report using it.[7][8][9][10]
Ayurveda therapies have varied and evolved over more than two millennia.[2] Therapies include herbal medicines, special diets, meditation, yoga, massage, laxatives, enemas, and medical oils.[11][12] Medicines are typically based on complex herbal compounds, minerals, and metal substances (perhaps under the influence of early Indian alchemy or rasa shastra). Ancient Ayurveda texts also taught surgical techniques, including rhinoplasty, kidney stone extractions, sutures, and the extraction of foreign objects.[13][14]
The main classical Ayurveda texts begin with accounts of the transmission of medical knowledge from the gods to sages, and then to human physicians.[15] In Sushruta Samhita (Sushruta's Compendium), Sushruta wrote that Dhanvantari, Hindu god of Ayurveda, incarnated himself as a king of Varanasi and taught medicine to a group of physicians, including Sushruta.[16][17] Ayurveda has been adapted for Western consumption, notably by Baba Hari Dass in the 1970s and Maharishi Ayurveda in the 1980s. Some scholars assert that Ayurveda originated in prehistoric times.[18][19] Ayurveda developed significantly during the Vedic period and later some of the non-Vedic systems such as Buddhism and Jainism also developed medical concepts and practices that appear in the classical Ayurveda texts.[20]
In Ayurveda texts, Doṣa balance is emphasized, and suppressing natural urges is considered unhealthy and claimed to lead to illness.[21] Ayurveda treatises describe three elemental doṣas viz. vāta, pitta and kapha, and state that balance (Skt. sāmyatva) of the doṣas results in health, while imbalance (viṣamatva) results in disease. Ayurveda treatises divide medicine into eight canonical components. Ayurveda practitioners had developed various medicinal preparations and surgical procedures from at least the beginning of the common era.[22]
There is no good evidence that Ayurveda is effective for treating any disease.[23] Ayurvedic preparations have been found to contain lead, mercury, and arsenic,[24] substances known to be harmful to humans. In a 2008 study, close to 21% of U.S. and Indian-manufactured patent Ayurvedic medicines sold through the Internet were found to contain toxic levels of heavy metals, specifically lead, mercury, and arsenic.[25] The public health implications of such metallic contaminants in India are unknown.[25]
Eight components
The earliest classical Sanskrit works on Ayurveda describe medicine as being divided into eight components (Skt. aṅga).[26][27] This characterization of the physician's art, "the medicine that has eight components" (Skt. cikitsāyām aṣṭāṅgāyāṃ चिकित्सायामष्टाङ्गायाम्), is first found in the Sanskrit epic the Mahābhārata, c. 4th century BCE.[28] The components are:[29][30][31]
- Kāyachikitsā: general medicine, medicine of the body
- Kaumāra-bhṛtya (Pediatrics): Discussions about prenatal and postnatal care of baby and mother; methods of conception; choosing the child's sex, intelligence, and constitution; childhood diseases; and midwifery[32]
- Śalyatantra: surgical techniques and the extraction of foreign objects
- Śhālākyatantra: treatment of ailments affecting openings or cavities in the upper body: ears, eyes, nose, mouth, etc.
- Bhūtavidyā: pacification of possessing spirits, and the people whose minds are affected by such possession
- Agadatantra/Vishagara-vairodh Tantra (Toxicology): includes epidemics; toxins in animals, vegetables and minerals; and keys for recognizing those anomalies and their antidotes
- Rasāyantantra: rejuvenation and tonics for increasing lifespan, intellect and strength
- Vājīkaraṇatantra: aphrodisiacs; treatments for increasing the volume and viability of semen and sexual pleasure; infertility problems; and spiritual development (transmutation of sexual energy into spiritual energy)
Principles and terminology

The word "ayurveda" is Sanskrit: आयुर्वेद, Āyurveda, meaning knowledge of life and longevity.[30]
The central theoretical ideas of Ayurveda developed in the mid-first millennium BCE, and show parallels with Sāṅkhya and Vaiśeṣika philosophies, as well as with Buddhism and Jainism.[34][35] Balance is emphasized, and suppressing natural urges is considered unhealthy and claimed to lead to illness.[21] For example, to suppress sneezing is said to potentially give rise to shoulder pain.[36] However, people are also cautioned to stay within the limits of reasonable balance and measure when following nature's urges.[21] For example, emphasis is placed on moderation of food intake,[37] sleep, and sexual intercourse.[21]
According to ayurveda, the human body is composed of tissues (dhatus), waste (malas), and biomaterials (doshas).[38] The seven dhatus are plasma (rasa), blood (rakta), muscles (māmsa), fat (meda), bone (asthi), marrow (majja), and semen (shukra). Like the medicine of classical antiquity, Ayurveda has historically divided bodily substances into five classical elements, (Sanskrit) panchamahabhuta, viz. earth, water, fire, air and ether.[39] There are also twenty gunas (qualities or characteristics) which are considered to be inherent in all matter. These are organized in ten pairs: heavy/light, cold/hot, unctuous/dry, dull/sharp, stable/mobile, soft/hard, non-slimy/slimy, smooth/coarse, minute/gross, and viscous/liquid.[40]
The three elemental bodily humors, the doshas or tridosha, are vata (space or air, equated with the nervous system), pitta (fire, equated with enzymes), and kapha (earth and water, equated with mucus). A parallel set of mental doshas termed satogun, rajogun, and tamogun control psychology. Each dosha has particular attributes and roles within the body and mind; the natural predominance of one or more doshas thus explains a person's physical constitution (prakriti) and personality.[38][41][42] Ayurvedic tradition holds that imbalance among the bodily and mental doshas is a major etiologic component of disease. One Ayurvedic view is that the doshas are balanced when they are equal to each other, while another view is that each human possesses a unique combination of the doshas which define this person's temperament and characteristics. In either case, it says that each person should modulate their behavior or environment to increase or decrease the doshas and maintain their natural state. Practitioners of Ayurveda must determine an individual's bodily and mental dosha makeup, as certain prakriti are said to predispose one to particular diseases.[43][38] For example, a person who is thin, shy, excitable, has a pronounced Adam's apple, and enjoys of esoteric knowledge is likely vata prakriti and therefore more susceptible to conditions such as flatulence, stuttering, and rheumatism.[38][44] Deranged vata is also associated with certain mental disorders due to excited or excess vayu (gas), although the Ayurvedic text Charaka Samhita also attributes "insanity" (unmada) to cold food and possession by the ghost of a sinful Brahman (brahmarakshasa).[38][43][45][46]
Ama (a Sanskrit word meaning "uncooked" or "undigested" ) is used to refer to the concept of anything that exists in a state of incomplete transformation. With regards to oral hygiene, it is claimed to be a toxic byproduct generated by improper or incomplete digestion.[47][48][49] The concept has no equivalent in standard medicine.
In medieval taxonomies of the Sanskrit knowledge systems, Ayurveda is assigned a place as a subsidiary Veda (upaveda).[50] Some medicinal plant names from the Atharvaveda and other Vedas can be found in subsequent Ayurveda literature.[51] Some other school of thoughts considers 'Ayurveda' as the 'Fifth Veda'.[52] The earliest recorded theoretical statements about the canonical models of disease in Ayurveda occur in the earliest Buddhist Canon.[53]
Practice
Ayurvedic practitioners regard physical existence, mental existence, and personality as their own unique units, with each element being able to influence the others.[clarification needed] This is a holistic approach used during diagnosis and therapy, and is a fundamental aspect of Ayurveda. Another part of Ayurvedic treatment says that there are channels (srotas) which transport fluids, and that the channels can be opened up by massage treatment using oils and Swedana (fomentation). Unhealthy, or blocked, channels are thought to cause disease.[54]
Diagnosis
Ayurveda has eight ways to diagnose illness, called Nadi (pulse), Mootra (urine), Mala (stool), Jihva (tongue), Shabda (speech), Sparsha (touch), Druk (vision), and Aakruti (appearance).[55] Ayurvedic practitioners approach diagnosis by using the five senses.[56] For example, hearing is used to observe the condition of breathing and speech.[39] The study of the lethal points or marman marma is of special importance.[40]
Treatment and prevention
Two of the eight branches of classical Ayurveda deal with surgery (Śalya-cikitsā and Śālākya-tantra), but contemporary Ayurveda tends to stress attaining vitality by building a healthy metabolic system and maintaining good digestion and excretion.[40] Ayurveda also focuses on exercise, yoga, and meditation.[57] One type of prescription is a Sattvic diet.
Ayurveda follows the concept of Dinacharya, which says that natural cycles (waking, sleeping, working, meditation etc.) are important for health. Hygiene, including regular bathing, cleaning of teeth, oil pulling, tongue scraping, skin care, and eye washing, is also a central practice.[39]
Substances used
Plant-based treatments in Ayurveda may be derived from roots, leaves, fruits, bark, or seeds such as cardamom and cinnamon. In the 19th century, William Dymock and co-authors summarized hundreds of plant-derived medicines along with the uses, microscopic structure, chemical composition, toxicology, prevalent myths and stories, and relation to commerce in British India.[58] Animal products used in Ayurveda include milk, bones, and gallstones. In addition, fats are prescribed both for consumption and for external use. Consumption of minerals, including sulphur, arsenic, lead, copper sulfate and gold, are also prescribed.[39] The addition of minerals to herbal medicine is called rasa shastra.
Ayurveda uses alcoholic beverages called Madya,[59] which are said to adjust the doshas by increasing Pitta and reducing Vatta and Kapha.[59] Madya are classified by the raw material and fermentation process, and the categories include: sugar-based, fruit-based, cereal-based, cereal-based with herbs, fermentated with vinegar, and tonic wines. The intended outcomes can include causing purgation, improving digestion or taste, creating dryness, or loosening joints. Ayurvedic texts describe Madya as non-viscid and fast-acting, and say that it enters and cleans minute pores in the body.[59]
Purified opium[60] is used in eight Ayurvedic preparations[61] and is said to balance the Vata and Kapha doshas and increase the Pitta dosha.[60] It is prescribed for diarrhea and dysentery, for increasing the sexual and muscular ability, and for affecting the brain. The sedative and pain-relieving properties of opium are considered in Ayurveda. The use of opium is found in the ancient Ayurvedic texts, and is first mentioned in the Sarngadhara Samhita (1300-1400 CE), a book on pharmacy used in Rajasthan in Western India, as an ingredient of an aphrodisiac to delay male ejaculation.[62] It is possible that opium was brought to India along with or before Muslim conquests.[61][63] The book Yoga Ratnakara (1700-1800 CE, unknown author), which is popular in Maharashtra, uses opium in a herbal-mineral composition prescribed for diarrhea.[62] In the Bhaisajya Ratnavali, opium and camphor are used for acute gastroenteritis. In this drug, the respiratory depressant action of opium is counteracted by the respiratory stimulant property of Camphor.[62] Later books have included the narcotic property for use as analgesic pain reliever.[62]
Cannabis indica is also mentioned in the ancient Ayurveda books, and is first mentioned in the Sarngadhara Samhita as a treatment for diarrhea.[62] In the Bhaisajya Ratnavali it is named as an ingredient in an aphrodisiac.[62]
Ayurveda says that both oil and tar can be used to stop bleeding,[39] and that traumatic bleeding can be stopped by four different methods: ligation of the blood vessel, cauterisation by heat, use of preparations to facilitate clotting, and use of preparations to constrict the blood vessels. Oils are also used in a number of ways, including regular consumption, anointing, smearing, head massage, application to affected areas,[64] and oil pulling. Liquids may also be poured on the patient's forehead, a technique called shirodhara.

Panchakarma
According to Ayurveda, panchakarma are techniques to eliminate toxic elements from the body.[66]
Current status
India
According to some sources, up to 80 percent of people in India use Ayurveda exclusively or combined with conventional Western medicine.[7][8]
In 1970, the Indian Medical Central Council Act which aimed to standardise qualifications for Ayurveda practitioners and provide accredited institutions for its study and research was passed by the Parliament of India.[67] In 1971, the Central Council of Indian Medicine (CCIM) was established under the Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha medicine and Homoeopathy (AYUSH), Ministry of Health and Family Welfare, to monitor higher education in Ayurveda in India.[68] The Indian government supports research and teaching in Ayurveda through many channels at both the national and state levels, and helps institutionalise traditional medicine so that it can be studied in major towns and cities.[69] The state-sponsored Central Council for Research in Ayurvedic Sciences (CCRAS) is designed to do research on Ayurveda.[70] Many clinics in urban and rural areas are run by professionals who qualify from these institutes.[67] (As of 2013), India has over 180 training centers offer degrees in traditional Ayurvedic medicine.[57]
To fight biopiracy and unethical patents, in 2001 the government of India set up the Traditional Knowledge Digital Library as a repository for formulations of various systems of Indian medicine, such as Ayurveda, Unani and Siddha.[71][72] The formulations come from over 100 traditional Ayurveda books.[73] An Indian Academy of Sciences document quoting a 2003-04 report states that India had 432,625 registered medical practitioners, 13,925 dispensaries, 2,253 hospitals and a bed strength of 43,803. 209 under-graduate teaching institutions and 16 post-graduate institutions.[74] Insurance companies cover expenses for Ayurvedic treatments in case of conditions such as spinal cord disorders, bone disorder, arthritis and cancer. Such claims constitute 5-10 percent of the country's health insurance claims.[75]
Maharashtra Andhashraddha Nirmoolan Samiti, an organisation dedicated to fighting superstition in India, considers Ayurveda to be pseudoscience.[76]
On 9 November 2014, India formed the Ministry of AYUSH. National Ayurveda Day is also observed in India on the birth of Dhanvantari that is Dhanteras.[77]
Other countries on the Indian subcontinent
About 75%-80% of the population of Nepal use Ayurveda,[9][10] and it is the most practiced form of medicine in the country.[78]
The Sri Lankan tradition of Ayurveda is similar to the Indian tradition. Practitioners of Ayurveda in Sri Lanka refer to Sanskrit texts which are common to both countries. However, they do differ in some aspects, particularly in the herbs used.
In 1980, the Sri Lankan government established a Ministry of Indigenous Medicine to revive and regulate Ayurveda.[79] The Institute of Indigenous Medicine (affiliated to the University of Colombo) offers undergraduate, postgraduate, and MD degrees in Ayurveda Medicine and Surgery, and similar degrees in unani medicine.[80] In the public system, there are currently 62 Ayurvedic hospitals and 208 central dispensaries, which served about 3 million people (about 11% of Sri Lanka's population) in 2010. In total, there are about 20,000 registered practitioners of Ayurveda in the country.[81][82]
According to the Mahavamsa, an ancient chronicle of Sinhalese royalty from the sixth century C.E., King Pandukabhaya of Sri Lanka (reigned 437 BCE to 367 BCE) had lying-in-homes and Ayurvedic hospitals (Sivikasotthi-Sala) built in various parts of the country. This is the earliest documented evidence available of institutions dedicated specifically to the care of the sick anywhere in the world.[83][84] Mihintale Hospital is the oldest in the world.[85]
Outside the Indian subcontinent
Ayurveda is a system of traditional medicine developed during antiquity and the medieval period, and as such is comparable to pre-modern Chinese and European systems of medicine. However, beginning in the 1960s, Ayurveda has been advertised as alternative medicine in the Western world. Due to different laws and medical regulations in the rest of the world, the unregulated practice and commercialisation of Ayurveda have raised ethical and legal issues. In some instances, Ayurvedic practices or terminology have also been adapted specifically for Western consumption, notably in the case of "Maharishi Ayurveda" in the 1980s. In some cases, this involved active fraud on the part of proponents of Ayurveda in an attempt to falsely represent the system as equal to the standards of modern medical research.[86][87][88]
Baba Hari Dass was an early proponent who helped bring Ayurveda to the US in the early 1970s. His teachings led to the establishment of the Mount Madonna Institute.[89] He invited several notable Ayurvedic teachers, including Vasant Lad, Sarita Shrestha, and Ram Harsh Singh. The Ayurvedic practitioner Michael Tierra wrote that "[t]he history of Ayurveda in North America will always owe a debt to the selfless contributions of Baba Hari Dass."[90]
In the United States, the practice of Ayurveda is not licensed or regulated by any state. The National Center for Complementary and Integrative Health says that "Few well-designed clinical trials and systematic research reviews suggest that Ayurvedic approaches are effective", warns against the issue of heavy metal poisoning, and emphasises the use of conventional health providers first.[91]
Classification and efficacy
Ayurvedic medicine is considered pseudoscientific because its premises are not based on science.[4][3] Both the lack of scientific soundness in the theoretical foundations of Ayurveda and the quality of research have been criticized.[4][92][93][94]
Although laboratory experiments suggest it is possible that some substances in Ayurveda might be developed into effective treatments, there is no evidence that any are effective in themselves.[95][96] Cancer Research UK states that there is no evidence that ayurvedic medicine helps treat cancer in people, and some Ayurvedic drugs contain toxic substances or interact with legitimate cancer drugs in a harmful way.[23]
Ethnologist Johannes Quack writes than although the rationalist movement Maharashtra Andhashraddha Nirmoolan Samiti officially labels Ayurveda – like astrology – a pseudoscience, these practices are in fact embraced by many of the movement's members.[5]
A review of the use of Ayurveda for cardiovascular disease concluded that the evidence is not convincing for the use of any Ayurvedic herbal treatment for heart disease or hypertension, but that many herbs used by Ayurvedic practitioners could be appropriate for further research.[97]
Research
In India, research in Ayurveda is undertaken by the Ministry of AYUSH, an abbreviation for the Department of Ayurveda, Yoga and Naturopathy, Unani, Siddha and Homoeopathy, through a national network of research institutes.[98]
In Nepal, the National Ayurvedic Training and Research Centre (NATRC) researches medicinal herbs in the country.[99]
In Sri Lanka, the Ministry of Health, Nutrition and Indigenous Medicine looks after the research in Ayurveda through various national research institutes.
Use of toxic metals
Rasa shastra, the practice of adding metals, minerals or gems to herbal preparations, may include toxic heavy metals such as lead, mercury and arsenic.[25] The public health implications of metals in rasa shastra in India is unknown.[25] Adverse reactions to herbs are described in traditional Ayurvedic texts, but practitioners are reluctant to admit that herbs could be toxic and that reliable information on herbal toxicity is not readily available. There is a communication gap between practitioners of modern medicine and Ayurveda.[100]
Some traditional Indian herbal medicinal products contain harmful levels of heavy metals, including lead.[101] For example, ghasard, a product commonly given to infants for digestive issues, has been found to have up to 1.6% lead concentration by weight, leading to lead encephalopathy.[102] A 1990 study on Ayurvedic medicines in India found that 41% of the products tested contained arsenic, and that 64% contained lead and mercury.[7] A 2004 study found toxic levels of heavy metals in 20% of Ayurvedic preparations made in South Asia and sold in the Boston area, and concluded that Ayurvedic products posed serious health risks and should be tested for heavy-metal contamination.[103] A 2008 study of more than 230 products found that approximately 20% of remedies (and 40% of rasa shastra medicines) purchased over the Internet from U.S. and Indian suppliers contained lead, mercury or arsenic.[25][104][105] A 2015 study of users in the United States found elevated blood lead levels in 40% of those tested, leading physician and former U.S. Air Force flight surgeon Harriet Hall to say that "Ayurveda is basically superstition mixed with a soupçon of practical health advice. And it can be dangerous."[106][107]
Heavy metals are thought of as active ingredients by advocates of Indian herbal medicinal products.[101] According to ancient Ayurvedic texts, certain physico-chemical purification processes such as samskaras or shodhanas (for metals) 'detoxify' the heavy metals in it.[108][109] These are similar to the Chinese pao zhi, although the Ayurvedic techniques are more complex and may involve physical pharmacy techniques as well as mantras. However, these products have nonetheless caused severe lead poisoning and other toxic effects.[104] Between 1978 and 2008, "more than 80 cases of lead poisoning associated with Ayurvedic medicine use [were] reported worldwide".[110] In 2012, the U.S. Centers for Disease Control and Prevention (CDC) linked Ayurvedic drugs to lead poisoning, based on cases where toxic materials were found in the blood of pregnant women who had taken Ayurvedic drugs.[111]
Ayurvedic practitioners argue that the toxicity of bhasmas (ash products) comes from improper manufacturing processes, contaminants, improper use of Ayurvedic medicine, quality of raw materials and that the end products and improper procedures are used by charlatans.[109]
In India, the government ruled that Ayurvedic products must be labelled with their metallic content.[112] However, in Current Science, a publication of the Indian Academy of Sciences, M. S. Valiathan said that "the absence of post-market surveillance and the paucity of test laboratory facilities [in India] make the quality control of Ayurvedic medicines exceedingly difficult at this time".[112] In the United States, most Ayurvedic products are marketed without having been reviewed or approved by the FDA. Since 2007, the FDA has placed an import alert on some Ayurvedic products in order to prevent them from entering the United States.[113] A 2012 toxicological review of mercury-based traditional herbo-metallic preparations concluded that the long-term pharmacotherapeutic and in-depth toxicity studies of these preparations are lacking.[114]
History
Some of the concepts of traditional Indian medicine have existed since the times of the Indus Valley Civilization.[115][116] The first recorded forms of Ayurveda as medical texts evolved from the Vedas.[117][118] Ayurveda is a discipline of the upaveda or "auxiliary knowledge" in Vedic tradition. The origins of Ayurveda are also found in Atharvaveda,[119] which contains 114 hymns and incantations described as magical cures for disease. There are various legendary accounts of the origin of Ayurveda, e.g. that it was received by Dhanvantari (or Divodasa) from Brahma.[17][39][120] Tradition also holds that the writings of Ayurveda were influenced by a lost text by the sage Agnivesa.[121]
Ayurveda is one of the few systems of medicine developed in ancient times that is still widely practiced in modern times.[122] As such, it is open to the criticism that its conceptual basis is obsolete and that its contemporary practitioners have not taken account of the developments of modern medicine.[123][124] Responses to this situation led to an impassioned debate in India during the early decades of the twentieth century, between proponents of unchanging tradition (śuddha "pure" ayurveda) and those who thought ayurveda should modernise and syncretize (aśuddha "impure, tainted" ayurveda).[125][126][127] The political debate about the place of ayurveda in contemporary India has continued to the present (2015), both in the public arena and in government.[128] Debate about the place of Ayurvedic medicine in the contemporary internationalized world also continues today (2015).[129][130]
Main texts
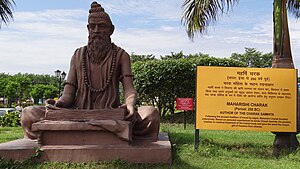
Many ancient works on Ayurvedic medicine are lost to posterity,[131] but manuscripts of three three principal early texts on Ayurveda have survived to the present day. These works are the Charaka Samhita, the Sushruta Samhita and the Bhela Samhita. The dating of these works is historically complicated since they each internally present themselves as composite works compiled by several editors. All past scholarship on their dating has been evaluated by Meulenbeld in volumes IA and IB of his History of Indian Medical Literature.[2] After considering the evidence and arguments concerning the Suśrutasaṃhitā, Meulenbeld states (IA, 348), "The Suśrutasaṃhitā is most probably the work of an unknown author who drew much of the material he incorporated in his treatise from a multiplicity of earlier sources from various periods. This may explain that many scholars yield to the temptation to recognize a number of distinct layers and, consequently, try to identify elements belonging to them. As we have seen, the identification of features thought to belong to a particular stratum is in many cases determined by preconceived ideas on the age of the strata and their supposed authors." The dating of this work to 600 BC was first proposed by Hoernle over a century ago,[132] but has long since been overturned by subsequent historical research. The current consensus amongst medical historians of South Asia is that the Suśrutasaṃhitā was compiled over a period of time starting with a kernel of medical ideas from the century or two BCE and then being revised by several hands into its present form by about 500 CE.[2][22] The view that the text was updated by the Buddhist scholar Nagarjuna in the 2nd century CE[133] has been disproved, although the last chapter of the work, the Uttaratantra, was added by an unknown later author before 500 CE.[2]
Similar arguments apply to the Charaka Samhita, written by Charaka, and the Bhela Samhita, attributed to Atreya Punarvasu, that are also dated to the 6th century BCE by non-specialist scholars[134][135][136] but are in fact, in their present form, datable to a period between the second and fifth centuries CE.[2][22][13] The Charaka Samhita was also updated by Dridhabala during the early centuries of the Common Era.[137]
The Bower Manuscript (dated to the Gupta era, between the 4th and the 6th century CE) includes of excerpts from the Bheda Samhita[138] and its description of concepts in Central Asian Buddhism. In 1987, A. F. R. Hoernle identified the scribe of the medical portions of the manuscript to be a native of India using a northern variant of the Gupta script, who had migrated and become a Buddhist monk in a monastery in Kucha. The Chinese pilgrim Fa Hsien (c. 337–422 AD) wrote about the healthcare system of the Gupta empire (320–550) and described the institutional approach of Indian medicine. This is also visible in the works of Charaka, who describes hospitals and how they should be equipped.[139]
Other early texts are the Agnivesha Samhita, Kasyapa Samhita and Harita Samhita. The original edition of the Agnivesha Samhita, by Agnivesa, is dated to 1500 BCE,[140] and it was later modified by Charaka.[141] Kasyapa Samhita includes the treatise of Jivaka Kumar Bhaccha[142] and is dated to the 6th century BCE.[143][144] While Harita Samhita is dated to an earlier period, it is attributed to Harita, who was a disciple of Punarvasu Atreya.[145] Some later texts are Astanga nighantu (8th Century) by Vagbhata, Paryaya ratnamala (9th century) by Madhava, Siddhasara nighantu (9th century) by Ravi Gupta, Dravyavali (10th Century), and Dravyaguna sangraha (11th century) by Chakrapani Datta, among others.[146]
Illnesses portrayed
Underwood and Rhodes state that the early forms of traditional Indian medicine identified fever, cough, consumption, diarrhea, dropsy, abscesses, seizures, tumours, and leprosy,[39] and that treatments included plastic surgery, lithotomy, tonsillectomy,[147] couching (a form of cataract surgery), puncturing to release fluids in the abdomen, extraction of foreign bodies, treatment of anal fistulas, treating fractures, amputations, cesarean sections,[Vagbhata 1][147] and stitching of wounds.[39] The use of herbs and surgical instruments became widespread.[39] During this period, treatments were also prescribed for complex ailments, including angina pectoris, diabetes, hypertension, and stones.[149][150]
Further development and spread
Ayurveda flourished throughout the Indian Middle Ages. Dalhana (fl. 1200), Sarngadhara (fl. 1300) and Bhavamisra (fl. 1500) compiled works on Indian medicine.[151] The medical works of both Sushruta and Charaka were also translated into the Chinese language in the 5th century,[152] and during the 8th century, they were translated into the Arabic and Persian language.[153] The 9th-century Persian physician Muhammad ibn Zakariya al-Razi was familiar with the text.[154][155] The Arabic works derived from the Ayurvedic texts eventually also reached Europe by the 12th century.[156][157] In Renaissance Italy, the Branca family of Sicily and Gaspare Tagliacozzi (Bologna) were influenced by the Arabic reception of the Sushruta's surgical techniques.[157]
British physicians traveled to India to observe rhinoplasty being performed using Indian methods, and reports on their rhinoplasty methods were published in the Gentleman's Magazine in 1794.[158] Instruments described in the Sushruta Samhita were further modified in Europe.[159] Joseph Constantine Carpue studied plastic surgery methods in India for 20 years and, in 1815, was able to perform the first major rhinoplasty surgery in the western world, using the "Indian" method of nose reconstruction.[160] In 1840 Brett published an article about this technique.[161]
During the period of British colonial rule in India, the practice of Ayurveda was not adopted by the British Indian Government, which was in favor of modern medicine. After Indian independence, there was more focus on Ayurveda and other traditional medical systems. Ayurveda became a part of the Indian National health care system, with state hospitals for Ayurveda established across the country. However, the treatments of traditional medicines were not always integrated with others.[162]
See also
- Acupuncture
- Aśvins
- Bachelor of Ayurveda, Medicine and Surgery
- Bhaisajyaguru
- Dhātu (Ayurveda)
- History of alternative medicine
- Homeopathy
- List of ineffective cancer treatments
- Ramuan
Footnotes
- ↑ Vāgbhaṭa's Aṣṭāṅgahṛdayasaṃhitā describes a procedure for the removal of a dead foetus from the womb of a living mother, and of a living child from the womb of a mother who has died (शारीरस्थान २, गर्भव्यापद्, २.२६-२७, २.५३).[148] Both these descriptions speak of removal of the fetus through the uterine passage. It is disputed to assert that early Indian Ayurvedic practitioner knew the caesarian section procedure. The earlier description of the Suśrutasaṃhitā (चिकित्सास्थान १५ "मूढगर्भ") is similar. A dead fetus is removed through the uterine passage and vagina. Although Suśruta does not describe removing a living child from a dead mother.
References
- ↑ "Ayurveda". Oxford University Press. https://en.oxforddictionaries.com/definition/ayurveda.
- ↑ 2.0 2.1 2.2 2.3 2.4 2.5 Meulenbeld, Gerrit Jan (1999). "Introduction". A History of Indian Medical Literature. Groningen: Egbert Forsten. ISBN 978-90-6980-124-7.
- ↑ 3.0 3.1 Pseudoscience: The Conspiracy Against Science. MIT Press. 2018. p. 293. ISBN 978-0-262-03742-6. https://books.google.com/books?id=dwFKDwAAQBAJ&pg=PA293. "Ayurveda, a traditional Indian medicine, is the subject of more than a dozen, with some of these "scholarly" journals devoted to Ayurveda alone..., others to Ayurveda and some other pseudoscience....Most current Ayurveda research can be classified as "tooth fairy science," research that accepts as its premise something not scientifically known to exist....Ayurveda is a long-standing system of beliefs and traditions, but its claimed effects have not been scientifically proven. Most Ayurveda researchers might as well be studying the tooth fairy. The German publisher Wolters Kluwer bought the Indian open-access publisher Medknow in 2011....It acquired its entire fleet of journals, including those devoted to pseudoscience topics such as An International Quarterly Journal of Research in Ayurveda."
- ↑ 4.0 4.1 4.2 Chapter 1: Thinking about psychiatry (4th ed.). Oxford University Press. 2019. p. 24. doi:10.1093/med/9780198795551.003.0001. ISBN 978-0-19-879555-1. https://books.google.com/books?id=626fDwAAQBAJ&pg=PA24. "These pseudoscientific theories may...confuse metaphysical with empirical claims (e.g....Ayurvedic medicine)"
- ↑ 5.0 5.1 Quack, Johannes (2011). Disenchanting India: Organized Rationalism and Criticism of Religion in India. Oxford University Press. pp. 213, 3. ISBN 978-0-19-981260-8. "ordinary members told me how they practice some of these pseudosciences, either privately or as certified doctors themselves, most often Ayurveda."
- ↑ "IMA Anti Quackery Wing". Indian Medical Association. https://www.ima-india.org/ima/free-way-page.php?pid=143. "The purpose of this compendium of court orders and various rules and regulations is to acquaint doctors regarding specific provisions and orders barring quackery by unqualified people, practitioners of Indian & Integrated Medicine to practice Modern Medicine."
- ↑ 7.0 7.1 7.2 Dargan, Paul I.; Gawarammana, Indika B.; Archer, John R.H.; House, Ivan M.; Shaw, Debbie; Wood, David M. (2008). "Heavy metal poisoning from Ayurvedic traditional medicines: An emerging problem?". International Journal of Environment and Health 2 (3/4): 463. doi:10.1504/IJENVH.2008.020936.
- ↑ 8.0 8.1 The majority of India's population uses Ayurveda exclusively or combined with conventional Western medicine, and it is practiced in varying forms in Southeast Asia. "Ayurvedic Medicine: An Introduction". U.S. Department of Health & Human Services, National Institutes of Health National Center for Complementary and Integrative Health (NCCIH). August 2008. http://nccih.nih.gov/health/ayurveda/introduction.htm.
- ↑ 9.0 9.1 "Weeklong programme to observe Health Day". The Himalayan Times. The Himalayan Times. 28 October 2013. http://thehimalayantimes.com/fullNews.php?headline=Weeklong+programme+to+observe+Health+Day&NewsID=395245. "In Nepal, 80 per cent of the population receives Ayurvedic medicine as first aid treatment."
- ↑ 10.0 10.1 Alam, Zulfeequar (2008). Herbal Medicines. New Delhi, India: A.P.H. Publishing. p. 122. ISBN 978-81-313-0358-0.
- ↑ "Ayurvedic medicine | Complementary and alternative therapy | Cancer Research UK". https://www.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/complementary-alternative-therapies/individual-therapies/ayurvedic-medicine.
- ↑ "What Is Ayurveda?" (in en). https://www.webmd.com/balance/guide/ayurvedic-treatments.
- ↑ 13.0 13.1 Wujastyk 2003a.
- ↑ Mukhopadhyaya, Girindranath (1913). The Surgical Instruments of the Hindus, with a Comparative Study of the Surgical Instruments of the Greek, Roman, Arab, and the Modern European Surgeons. Calcutta: Calcutta University. https://archive.org/details/cu31924012165522. Retrieved 16 October 2015.
- ↑ Zysk, Kenneth G. (1999). "Mythology and the Brāhmaṇization of Indian medicine: Transforming Heterodoxy into Orthodoxy". in Josephson, Folke. Categorisation and Interpretation. Meijerbergs institut för svensk etymologisk forskning, Göteborgs universitet. pp. 125–145. ISBN 978-91-630-7978-8.
- ↑ Bhishagratna, Kaviraj Kunjalal (1907). An English Translation of the Sushruta Samhita Based on Original Sanskrit text. Calcutta: K. K. Bhishagratna. p. 1. https://archive.org/stream/b24758619_0001#page/n103/mode/2up. Retrieved 16 October 2015.
- ↑ 17.0 17.1 Dhanvantari. (2010). In Encyclopædia Britannica. Retrieved 4 August 2010, from Encyclopædia Britannica Online
- ↑ Dinesh Kumar Tyagi (2005). Pharma Forestry A Field Guide To Medicinal Plants. Atlantic Publishers. p. 34. "Ayurveda, the organised and classic system of traditional medicine had known to the Indians from prehistoric times."
- ↑ Hansch, Corwin; Sammes, Peter George; Kennewell, Peter D.; John Bodenhan Taylor (1990). Comprehensive medicinal chemistry: the rational design, mechanistic study & therapeutic application of chemical compounds. Pergamon Press. p. 114. "The origin of Ayurveda is lost in antiquity. As was the case with many branches of human knowledge in prehistoric times, Ayurveda developed in close association with religion and mythology."
- ↑ Gupta, Pankaj; Vijay Kumar Sharma; Sharma, Sushma (2014). Healing Traditions of the Northwestern Himalayas. Springer. p. 23. ISBN 978-81-322-1925-5. https://books.google.com/books?id=CA7vAwAAQBAJ&pg=PA23.
- ↑ 21.0 21.1 21.2 21.3 Wujastyk 2003a, p. xviii
- ↑ 22.0 22.1 22.2 Sharma, Priya Vrat (1992). History of Medicine in India. New Delhi: Indian National Science Academy.
- ↑ 23.0 23.1 "Ayurvedic medicine". Cancer Research UK. 3 December 2018. https://about-cancer.cancerresearchuk.org/about-cancer/cancer-in-general/treatment/complementary-alternative-therapies/individual-therapies/ayurvedic-medicine. "There is no scientific evidence to prove that Ayurvedic medicine can treat or cure cancer, or any other disease."
- ↑ "Is Ayurveda treatment approved in the U.S?". WebMD. https://www.webmd.com/balance/qa/is-ayurveda-treatment-approved-in-the-us.
- ↑ 25.0 25.1 25.2 25.3 25.4 Saper RB; Phillips RS et al. (2008). "Lead, mercury, and arsenic in US- and Indian-manufactured medicines sold via the internet". JAMA 300 (8): 915–923. doi:10.1001/jama.300.8.915. PMID 18728265.
- ↑ Ācārya, Yādava Trivikramātmaja, ed (1945). "Sūtrasthāna 1.7-9". Suśrutasaṃhitā. Bombay: Nirṇayasāgara Press. pp. 2–3. https://archive.org/stream/sushrutasamhita/sushruta_samhita_critical#page/n229/mode/2up.
- ↑ Ācārya, Yādava Trivikramātmaja, ed (1941). "Sūtrasthāna 30.28". The Carakasaṃhitā of Caraka, with the commentary by Cakrapāṇidatta, edited by Yadavaśarman Trivikarama Ācārya. Bombay: Nirṇayasāgara Press. pp. 189. https://archive.org/stream/TheCarakasahitOrCharakasamhitaOfCarakaEditedByYadavaarman/Carakasamhita-Trikamji1941#page/n253/mode/2up.
- ↑ Wujastyk, Dominik (2003b). "Indian Medicine". in Flood, Gavin. The Blackwell Companion to Hinduism. Oxford: Blackwell. pp. 394. ISBN 978-1-4051-3251-0.
- ↑ Sharma, Priya Vrat (1999). Suśruta-Samhitā With English Translation of text…. 1. Varanasi: Chaukhambha Visvabharati. pp. 7–11.
- ↑ 30.0 30.1 Fields, Gregory P. (2001). Religious Therapeutics: Body and Health in Yoga, Ayurveda, and Tantra. SUNY Press. p. 36. ISBN 978-0-7914-4915-8.
- ↑ Bhishagratna, Kaviraj Kunja Lal (1907). An English Translation of the Sushruta Samhita Based on Original Sanskrit Text. 1. Calcutta: The Author. pp. 2–6. https://archive.org/stream/englishtranslati01susruoft#page/2/mode/2up.
- ↑ Swami Sadashiva Tirtha (1998). The Ãyurveda Encyclopedia: Natural Secrets to Healing, Prevention & Longevity. ISBN 0-9658042-2-4. https://archive.org/details/ayurvedaencyclop00tirt.
- ↑ Clifford, Terry (2003). Tibetan Buddhist Medicine and Psychiatry. 42. Motilal Banarsidass Publications. ISBN:81-208-1784-2.
- ↑ Comba, Antonella (2001). "Carakasaṃhitā, Śārīrasthāna~I and Vaiśeṣika Philosophy". in Meulenbeld, G. Jan. Studies on Indian Medical History. Delhi: Motilal Banarsidass. pp. 39–55.
- ↑ Basham, A. L. (1976). "The Practice of Medicine in Ancient and Medieval India". in Leslie, Charles. Asian Medical Systems. Berkeley: University of California Press. pp. 18–43.
- ↑ Namyata Pathak, A Raut, Ashok Vaidya Acute Cervical Pain Syndrome Resulting from Suppressed Sneezing – JAPI (Accessed on 29 October 2013)
- ↑ Chopra 2003, p. 75
- ↑ 38.0 38.1 38.2 38.3 38.4 Mishra, L; Singh, BB; Dagenais, S (March 2001). "Ayurveda: a historical perspective and principles of the traditional healthcare system in India". Alternative Therapies in Health & Medicine 42 (2): 36–42. PMID 11253415.
- ↑ 39.0 39.1 39.2 39.3 39.4 39.5 39.6 39.7 39.8 Underwood & Rhodes (2008)
- ↑ 40.0 40.1 40.2 Chopra 2003, p. 76, citing Sushrutasamhita 25.36.
- ↑ Payyappallimana, Unnikrishnan; Venkatasubramanian, Padma (31 March 2016). "Exploring Ayurvedic Knowledge on Food and Health for Providing Innovative Solutions to Contemporary Healthcare". Frontiers in Public Health 4 (57): 57. doi:10.3389/fpubh.2016.00057. PMID 27066472.
- ↑ Shilpa, S; Venkatesha Murthy, C.G. (January 2011). "Understanding personality from Ayurvedic perspective for psychological assessment: A case". Ayu (Institute for Post Graduate Teaching & Research in Ayurveda) 32 (1): 12–19. doi:10.4103/0974-8520.85716. PMID 22131752.
- ↑ 43.0 43.1 Ramu, M.G.; Venkataram, B.S. (January 1985). "Manovikara (mental disorders) in Ayurveda". Ancient Science of Life (Wolters Kluwer Medknow Publications) 4 (3): 165–73. PMID 22557473.
- ↑ Bhagwan Dash, Vaidya (1995). Fundamentals of Ayurvedic Medicine. Lotus Press. ISBN 978-81-220-0117-4.
- ↑ "Ayurvedic & Western approaches to the treatment of Schizophrenia". 21 September 2009. https://www.ayurvedacollege.com/blog/schizophrenia/#Types_of_insanity_unmada.
- ↑ Acharya, YT (1941). Charaka samhita. Commentary of Chakrapani. Bombay: Nirnayasagar Press.
- ↑ Kacera, Walter (2007). "Ama and Disease". Ayurvedic Tongue Diagnosis. Lotus Press. pp. 159–176. ISBN 978-0-940985-77-3.
- ↑ Amruthesh, Sunita (1 January 2008). "Dentistry and Ayurveda – IV: Classification and management of common oral diseases". Indian Journal of Dental Research 19 (1): 52–61. doi:10.4103/0970-9290.38933. PMID 18245925.
- ↑ Amruthesh, Sunita (2007). "Dentistry and Ayurveda-III (basics - ama, immunity, ojas, rasas, etiopathogenesis and prevention)". Indian Journal of Dental Research 18 (3): 112–9. doi:10.4103/0970-9290.33786. PMID 17687173.
- ↑ Madhusūdanasarasvatī (1912) (in sa). प्रस्थानभेदः श्रीमधुसूदनसरस्वत्या विरचितः. श्रीरङ्गम्: श्रीवाणिविलासमुद्रायन्त्रालय. p. 14. https://archive.org/stream/Prasthanabheda.by.Madhusudana.Sarasvati#page/n15/mode/2up. Retrieved 16 October 2015.
- ↑ Zysk, Kenneth G. (2010). Medicine in the {Veda}: Religious Healing in the {Veda} with Translations and Annotations of Medical Hymns from the {Rgveda and the Atharvaveda} and Renderings from the Corresponding Ritual Texts. New Delhi: Motilal Banarsidass. ISBN 978-81-208-1401-1.
- ↑ Sengupta, Pradip Kumar (2012) (in en). History of Science and Philosophy of Science: A Philosophical Perspective of the Logic of Ideas in Science. Longman. pp. 486. ISBN 978-81-317-1931-2. https://books.google.com/books?id=VNc9QvzCfLYC&pg=PA486. "Sometimes Ayurveda is also considered as the fifth Veda or Pañcama Veda."
- ↑ Zysk, Kenneth G. (1998). Asceticism and Healing in Ancient {India}: Medicine in the {Buddhist} Monastery. Delhi: Motilal Banarsidass. ISBN 978-81-208-1507-0.
- ↑ Wujastyk 2003a, pp. XIX–XX
- ↑ Mishra, L.; Singh, B. B.; Dagenais, S. (2001). "Healthcare and disease management in Ayurveda". Alternative Therapies in Health and Medicine 7 (2): 44–50. PMID 11253416.
- ↑ Chopra 2003, p. 79
- ↑ 57.0 57.1 "Ayurveda". Encarta. Redmond, WA: Microsoft. 2008. http://encarta.msn.com/encyclopedia_761596196/Ayurveda.html.
- ↑ Pharmacographia Indica, A history of principal drugs of vegetable origin in British India - Volume 1, William Dymock et al. (1890), London
- ↑ 59.0 59.1 59.2 Sekar, S. (2007). "Traditional alcoholic beverages from Ayurveda and their role on human health". Indian Journal of Traditional Knowledge 6 (1): 144–149. http://www.niscair.res.in/sciencecommunication/ResearchJournals/rejour/ijtk/Fulltextsearch/2007/January%202007/IJTK-Vol%206%281%29-January%202007-pp%20144-149.htm.
- ↑ 60.0 60.1 Mani, Dayanandan; Dhawan, Sunita S. (2011). "Scientific basis of therapeutic uses of opium poppy (Papaver somniferum) in Ayurveda". Acta Horticulturae (International Symposium on Papaver) (1036): 175–180. http://www.actahort.org/books/1036/1036_20.htm. Retrieved 7 December 2014.
- ↑ 61.0 61.1 "UNODC - Bulletin on Narcotics - 1955 Issue 3 - 001". https://www.unodc.org/unodc/en/data-and-analysis/bulletin/bulletin_1955-01-01_3_page002.html.
- ↑ 62.0 62.1 62.2 62.3 62.4 62.5 "Archived copy". http://www.new1.dli.ernet.in/data1/upload/insa/INSA_1/20005af3_31.pdf.
- ↑ Chopra 2003, p. 80
- ↑ Wujastyk 2003a, p. 20
- ↑ Finger, p. 66
- ↑ Ajanal, M; Nayak, S; Prasad, BS; Kadam, A (December 2013). "Adverse drug reaction and concepts of drug safety in Ayurveda: An overview.". Journal of Young Pharmacists 5 (4): 116–20. doi:10.1016/j.jyp.2013.10.001. PMID 24563588.
- ↑ 67.0 67.1 Wujastyk 2003a, p. XXII
- ↑ "Introduction to Central Council of Indian Medicine". Central Council of Indian Medicine (CCIM). http://ccimindia.org/introduction.html.
- ↑ Wujastyk 2003a, p. XVI
- ↑ "Welcome to Central Council for Research in Ayurveda and Siddha ( India )". Ccras.nic.in. http://ccras.nic.in/.
- ↑ "About TKDL". Traditional Knowledge Digital Library. http://www.tkdl.res.in/tkdl/LangDefault/Common/Abouttkdl.asp?GL=Eng.
- ↑ "Know Instances of Patenting on the UES of Medicinal Plants in India". PIB, Ministry of Environment and Forests. 6 May 2010. http://pib.nic.in/release/release.asp?relid=61511.
- ↑ "Source of Information". Traditional Knowledge Digital Library (Government of India). http://www.tkdl.res.in/tkdl/langdefault/common/sourceinfo.asp.
- ↑ Valiathan, M. S.. "Towards Ayurvedic Biology". Indian Academy of Sciences. http://www.ias.ac.in/academy/dvdocs/ayurvis.pdf.
- ↑ Roy, Shobha (2012-03-28). "Insurers stepping up cover for ayurveda treatment". The Hindu. http://www.thehindubusinessline.com/industry-and-economy/banking/insurers-stepping-up-cover-for-ayurveda-treatment/article3254964.ece.
- ↑ Quack, Johannes (2011). Disenchanting India: Organized Rationalism and Criticism of Religion in India. Oxford University Press. p. 213. ISBN 978-0-19-981260-8. "ordinary members told me how they practice some of these pseudosciences, either privately or as certified doctors themselves, most often Ayurveda."
- ↑ "National Ayurveda Day – Vikaspedia". http://vikaspedia.in/health/ayush/ayurveda-1/national-ayurveda-day.
- ↑ Guneratne, Arjun (2009). Culture and the Environment in the Himalaya. Routledge contemporary South Asia series, #24. New York: Routledge. pp. 84–85. ISBN 978-0-415-77883-1.
- ↑ "Ministry of Indigenous Medicine". http://www.ayurveda.gov.lk/dept.html.
- ↑ "Institute of indigenous Medicine". Iim.cmb.ac.lk. http://iim.cmb.ac.lk/.
- ↑ "Statistics Report". Sri Lanka Institute of Indigenous Medicine. November 2011. http://www.indigenousmedimini.gov.lk/Downloads/Statistics%20Report%20Final%202011.%20November.pdf.
- ↑ "About Us". The Ministry of Indigenous Medicine (Sri Lanka). 14 February 1980. http://www.indigenousmedimini.gov.lk/About_us.html.
- ↑ Aluvihare, Arjuna (November 1993). "Rohal Kramaya Lovata Dhayadha Kale Sri Lankikayo". Vidhusara Science Magazine.
- ↑ "Resource Mobilization in Sri Lanka's Health Sector". Harvard School of Public Health & Health Policy Programme, Institute of Policy Studies. February 1997. p. 19. http://www.hsph.harvard.edu/ihsg/publications/pdf/No-42.PDF.
- ↑ Müller-Dietz, Heinz E. (1975). "Die Krankenhaus-ruinen in Mihintale (Ceylon)". Historia Hospitalium 10: 65–71. PMID 11627253.
- ↑ Skolnick, Andrew A. (1991). "The Maharishi Caper: Or How to Hoodwink Top Medical Journals" (print). ScienceWriters: The Newsletter of the National Association of Science Writers (Fall). http://www.aaskolnick.com/naswmav.htm. Retrieved 23 January 2016. "From time to time, even the most prestigious science journals publish erroneous or fraudulent data, unjustified conclusions, and sometimes balderdash. Balderdash was the right word when The Journal of the American Medical Association (JAMA) published the article, "Maharishi Ayur-Veda: Modern Insights Into Ancient Medicine," in its 22/29 May issue. Discovering that they had been deceived by the article's authors, the editors published a correction in the 14 August issue, which was followed on 2 October by a six-page exposé on the people who had hoodwinked them.".
- ↑ Skolnick, Andrew A. (1991). "Maharishi Ayur-Veda: Guru's marketing scheme promises the world eternal 'perfect health'". JAMA 266 (13): 1741–2, 1744–5, 1749–50. doi:10.1001/jama.1991.03470130017003. PMID 1817475.
- ↑ "National Policy on Traditional Medicine and Regulation of Herbal Medicines". World Health Organization. May 2005. http://apps.who.int/medicinedocs/pdf/s7916e/s7916e.pdf.
- ↑ Constance Jones; James D. Ryan (2006). Encyclopedia of Hinduism. Infobase Publishing. p. 179. ISBN 9780816075645.
- ↑ Karta Purkh Singh Khalsa and Michael Tierra: "Independently, we both first learned Ayurvedic medicine from our respective spiritual mentors – myself with Baba Hari Dass and K.P., with Yogi Bhajan." (p.X); The way of Ayurvedic Herbs, Lotus Press, 2008, ISBN:978-0-9409-8598-8
- ↑ "Ayurvedic Medicine: In Depth". https://www.nccih.nih.gov/health/ayurvedic-medicine-in-depth.
- ↑ Sujatha, V (July 2011). "What could 'integrative' medicine mean? Social science perspectives on contemporary Ayurveda". Journal of Ayurveda and Integrative Medicine 2 (3): 115–23. doi:10.4103/0975-9476.85549. PMID 22022153.
- ↑ Manohar, PR (April 2013). "Uniform standards and quality control of research publications in the field of Ayurveda". Ancient Science of Life 32 (4): 185–6. doi:10.4103/0257-7941.131968. PMID 24991064.
- ↑ Bausell, R. Barker (2007). Snake Oil Science: The Truth About Complementary and Alternative Medicine. Oxford University Press. p. 259. ISBN 978-0-19-538342-3. https://archive.org/details/isbn_9780195313680.
- ↑ "Ayurveda". American Cancer Society. 26 August 2011. http://www.cancer.org/treatment/treatmentsandsideeffects/complementaryandalternativemedicine/mindbodyandspirit/ayurveda. "The effectiveness of Ayurveda has not been proven in scientific studies, but early research suggests that certain herbs may offer potential therapeutic value... Although Ayurveda has been largely untested by Western researchers, there is a growing interest in integrating some parts of the system into modern medical practice. In fact, a few of the herbs and substances have been purified into drugs that are used (along with other medicines) to treat cancer. Early studies suggest that other parts of Ayurveda may have potential therapeutic value."
- ↑ Patwardhan, Bhushan (2014-11-01). "Bridging Ayurveda with evidence-based scientific approaches in medicine". The EPMA Journal 5 (1): 19. doi:10.1186/1878-5085-5-19. ISSN 1878-5077. PMID 25395997.
- ↑ Mamtani, R.; Mamtani, R. (2005). "Ayurveda and Yoga in Cardiovascular Diseases". Cardiology in Review 13 (3): 155–162. doi:10.1097/01.crd.0000128730.31658.36. PMID 15834238.
- ↑ "Research in Ayurveda - About CCRAS". Central Council for Research in Ayurveda and Siddha. Department of AYUSH, Ministry of Health and Family Welfare. http://ccras.nic.in/about_ccras/about_research_in_ayurveda.htm.
- ↑ "China hands over Ayurveda research centre to govt". The Kathmandu Post. Kantipur Publications. http://www.ekantipur.com/the-kathmandu-post/2011/04/03/nation/china-hands-over-ayurveda-research-centre-to-govt/220180.html. "The centre will play a positive role in promotion and utilisation of Ayurveda in the country, by conducting research on medicinal herbs available here."
- ↑ Urmila, T.; Supriya, B. (2008). "Pharmacovigilance of ayurvedic medicines in India". Indian Journal of Pharmacology 40 (S1): 10–12. http://www.bioline.org.br/request?ph08015.
- ↑ 101.0 101.1 Ernst, E. (2002). "Heavy metals in traditional Indian remedies". European Journal of Clinical Pharmacology 57 (12): 891–896. doi:10.1007/s00228-001-0400-y. ISSN 0031-6970. PMID 11936709.
- ↑ Karri, Surya K.; Saper, Robert B.; Kales, Stefanos N. (January 2008). "Lead Encephalopathy Due to Traditional Medicines". Current Drug Safety 3 (1): 54–59. doi:10.2174/157488608783333907. ISSN 1574-8863. PMID 18690981.
- ↑ Saper, R. B.; Kales SN; Paquin, J et al. (2004). "Heavy metal content of ayurveda herbal medicine products". Journal of the American Medical Association 292 (23): 2868–73. doi:10.1001/jama.292.23.2868. PMID 15598918.
- ↑ 104.0 104.1 Ellin, Abby (17 September 2008). "Skin deep: ancient, but how safe?". The New York Times. https://www.nytimes.com/2008/09/18/fashion/18skin.html. "A report in the August 27 [2008] issue of The Journal of the American Medical Association found that nearly 21 percent of 193 ayurvedic herbal supplements bought online, produced in both India and the United States, contained lead, mercury or arsenic."
- ↑ Szabo, Liz (26 August 2008). "Study finds toxins in some herbal medicines". USA Today. https://www.usatoday.com/news/health/2008-08-26-ayurvedic-medicines_N.htm.
- ↑ Hall, Harriet (14 December 2017). "Ayurveda: Ancient Superstition, Not Ancient Wisdom". https://www.csicop.org/specialarticles/show/ayurveda_ancient_superstition_not_ancient_wisdom.
- ↑ "A cluster of lead poisoning among consumers of Ayurvedic medicine.". International Journal of Occupational and Environmental Health 21 (4): 303–307. 6 Apr 2015. doi:10.1179/2049396715Y.0000000009. PMID 25843124.
- ↑ CCRAS. "Guidelines for toxicity / safety profile evaluation of Ayurveda & Siddha plant drugs". CCRAS Guidelines. http://www.ccras.nic.in/pdf/Guidelinesfortoxicity.doc.
- ↑ 109.0 109.1 Katiyar, C. K. (2006). "Safety Aspects of Ayurveda". Ranbaxy Research Laboratories. http://www.yieldopedia.com/paneladmin/reports/ddd5b6c170eb4b6f1e956edf7e6b7904.pdf.
- ↑ Saper RB; Phillips RS; Sehgal A (August 2008). "Lead, mercury, and arsenic in US- and Indian-manufactured ayurvedic medicines sold via the internet". JAMA 300 (8): 915–923. doi:10.1001/jama.300.8.915. PMID 18728265.
- ↑ "Ayurveda linked to lead poisoning in US women". The Financial Express. 24 August 2012. http://www.financialexpress.com/news/ayurveda-linked-to-lead-poisoning-in-us-women/992558/0.
- ↑ 112.0 112.1 Valiathan, MS (2006). "Ayurveda: putting the house in order". Current Science 90 (1): 5–6. http://www.currentscience.ac.in/Downloads/article_id_090_01_0005_0006_0.pdf.
- ↑ "Use caution with Ayurvedic products". US FDA. https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm050798.htm.
- ↑ Kamath, Sushant U.; Pemiah, Brindha; Sekar, Rajan K.; Krishnaswamy, Sridharan; Sethuraman, Swaminathan; Krishnan, Uma Maheswari (2012-06-01). "Mercury-based traditional herbo-metallic preparations: a toxicological perspective" (in en). Archives of Toxicology 86 (6): 831–838. doi:10.1007/s00204-012-0826-2. ISSN 1432-0738. PMID 22441626.
- ↑ Issues in Pharmaceuticals by Disease, Disorder, or Organ System: 2011 Edition. 2012-01-09. p. 9. ISBN 978-1-4649-6756-6. https://books.google.com/books?id=XbhvXzqwCRsC&pg=PT9.
- ↑ Svoboda, Robert (1992). Ayurveda: Life, Health and Longevity. Penguin Books India. pp. 9–10. ISBN 978-0-14-019322-0. https://books.google.com/books?id=3lD-8u-KtJgC.
- ↑ T.S.S. Dikshith (2008). Safe Use of Chemicals: A Practical Guide. CRC Press. p. 16. ISBN 978-1-4200-8051-3. https://books.google.com/books?id=eetxXrKHmZIC&q=5000+bc+ayurveda+origins&pg=PA16.
- ↑ Mackenzie, Elizabeth R.; Rakel, Birgit (2006). Complementary and Alternative Medicine for Older Adults: A Guide to Holistic Approaches to Healthy Aging. Springer. p. 215. ISBN 978-0-8261-3806-4. https://archive.org/details/isbn_9780826138057.
- ↑ Narayanaswamy, V (1981). "Origin and Development of Ayurveda: (A Brief History)". Ancient Science of Life 1 (1): 1–7. PMID 22556454.
- ↑ Singh, Rana P. B.; Rana, Pravin S. (2002). Banaras Region: A Spiritual and Cultural Guide. Varanasi, India: Indica Books. p. 31. ISBN 978-81-86569-24-5.
- ↑ Ṭhākara, Vināyaka Jayānanda (1989). Methodology of Research in Ayurveda. Jamnagar, India: Gujarat Ayurved University Press. p. 7.
- ↑ Smith, Frederick M.; Wujastyk, Dagmar (2008). "Introduction". Modern and Global Ayurveda: Pluralism and Paradigms. New York, NY: SUNY Press. pp. 1–28. ISBN 978-0-7914-7816-5. OCLC 244771011.
- ↑ Leslie, Charles, ed (1976). Asian Medical Systems. Berkeley: University of California Press. pp. passim. ISBN 978-0-520-03511-9.
- ↑ Taylor, Carl. "The Place of Indigenous Medical Practitioners in the Modernization of Health Services". in Leslie, Charles. Asian Medical Systems. pp. 285–292.
- ↑ Leslie, Charles. The Ambiguites of Medical Revivalism in Modern India. pp. 356–367.
- ↑ Sharma, Shiv (1975). Ayurvedic Medicine: Past and Present. Calcutta: Dabur (S. K. Burman).
- ↑ Berger, Rachel (2013). Ayurveda made modern : political histories of indigenous medicine in North India, 1900-1955. New York, NY: Palgrave Macmillan. ISBN 978-0-230-28455-5.
- ↑ Wujastyk, Dominik (2008). The Evolution of Indian Government Policy on Ayurveda in the Twentieth Century. SUNY Press. pp. 43–76.
- ↑ Wujastyk, Dominik (2005). "Policy Formation and Debate Concerning the Government Regulation of Ayurveda in Great Britain in the 21st Century". Asian Medicine 1: 162–184. doi:10.1163/157342105777996719. http://discovery.ucl.ac.uk/1066/1/submission-article.pdf.
- ↑ Redy, Sita (2002). "Asian Medicine in America: The Ayurvedic Case". Annals of the American Academy of Political and Social Science 583: 97–121. doi:10.1177/000271620258300107.
- ↑ Meulenbeld, G. Jan (1999–2000). A history of Indian medical literature. IA. Groningen. pp. 689–699. ISBN 90-6980-124-8. OCLC 42207455. https://www.worldcat.org/oclc/42207455.
- ↑ Hoernle, A. F. Rudolf (1907) (in en). Osteology or the bones of the human body.. Oxford: Clarendon P.. OCLC 28563136.
- ↑ J. N. Roy; Braja Bihārī Kumāra. India and Central Asia: Classical to Contemporary Periods. Concept Publishing Company. p. 103.
- ↑ Leonore Loeb Adler; B. Runi Mukherji. Spirit Versus Scalpel: Traditional Healing and Modern Psychotherapy. Greenwood. p. 76.
- ↑ Saxena, Praveen K.. Development of Plant-Based Medicines: Conservation, Efficacy and Safety. Springer. p. 48.
- ↑ Mohammad Ali Jazayery; Winter, Werner (1988). Languages and Cultures: Studies in Honor of Edgar C. Polomé. Walter de Gruyter. p. 116. ISBN 978-3-11-010204-8. https://books.google.com/books?id=v56tj2EPZ-YC&pg=PA116.
- ↑ Glucklich, Ariel (2008). The Strides of Vishnu: Hindu Culture in Historical Perspective. Oxford, England: Oxford University Press. p. 141. ISBN 978-0-19-531405-2.
- ↑ Chattopadhyaya, Debiprasad (1991). History of Science and Technology in Ancient India: Formation of the theoretical fundamentals of natural science. p. 153.
- ↑ Singh, Upinder (2008). A History of Ancient and Early Medieval India: From the Stone Age to the 12th Century. Pearson. ISBN 978-81-317-1120-0. https://books.google.com/books?id=H3lUIIYxWkEC&q=Charaka+hospital&pg=PA543.
- ↑ K. Mangathayaru (2013). Pharmacognosy: An Indian perspective. Pearson Education. p. 36. ISBN 978-93-325-2026-4. https://books.google.com/books?id=2UQ8BAAAQBAJ&pg=PA36.
- ↑ Anil Kumar Mehta; Gupta, Naveen K.; R. N. Sharma (2002). Health & Harmony Through Ayurveda. B. Jain Publishers. p. 41. ISBN 978-81-7021-934-7. https://books.google.com/books?id=t4ymSRXTCaoC&pg=PT41.
- ↑ J. Chandy (1965). Indian Journal of Medical Education, Volume 5. p. 185.
- ↑ The Indo-Asian Culture, Volume 9. 1960. p. 61.
- ↑ Thorpe, Edgar; Thorpe, Showick. Pearson General Knowledge Manual 2009. Pearson. p. 196.
- ↑ K. R. Srikanthamurthy (2005). Biographical History of Indian Medicine: Pictorial. Chaukhambha Orientalia. pp. 33–35.
- ↑ Vaidya Bhagwan Dash. Materia Medica of Ayurveda: Based on: Madanapala's Nighantu. B. Jain Publishers. p. 14.
- ↑ 147.0 147.1 Magner, Lois N. (13 August 2002). A History of the Life Sciences, Revised and Expanded. CRC Press. p. 6. ISBN 978-0-8247-0824-5. https://books.google.com/books?id=YKJ6gVYbrGwC&pg=PA6. Retrieved 26 December 2016.
- ↑ Vāgbhaṭa (1939). Ashtanga Hridaya. https://archive.org/stream/Ashtanga.Hridaya.of.Vagbhata#page/n567/mode/2up. Retrieved 2 January 2017.
- ↑ Dwivedi, Girish; Dwivedi, Shridhar (2007). "History of Medicine: Sushruta – the Clinician – Teacher par Excellence". Indian Journal of Chest Diseases and Allied Sciences 49: 243–244. http://medind.nic.in/iae/t07/i4/iaet07i4p243.pdf. (Republished by National Informatics Centre, Government of India.)
- ↑ Lock et al., p. 836
- ↑ Wujastyk 2003a, p. XXVI
- ↑ Wujastyk, Dagmar (2002). Well-Mannered Medicine: Medical Ethics and Etiquette in Classical Ayurveda. Oxford University Press. ISBN 978-0-19-985627-5. https://books.google.com/books?id=6-BoAgAAQBAJ&q=ayurveda+translated+5th+chinese+CE&pg=PA17.
- ↑ Encyclopaedia of the History of Science, Technology, and Medicine in Non-Western Cultures. Springer. 2008-03-12. ISBN 978-1-4020-4559-2. Bibcode: 2008ehst.book.....S. https://books.google.com/books?id=kt9DIY1g9HYC&pg=PA168.
- ↑ Rhyner, Hans H. (1994). Ayurveda: The Gentle Health System. Motilal Banarsidass. p. 15. ISBN 978-81-208-1500-1. https://books.google.com/books?id=HlJ-20_iP6wC.
- ↑ Ramachandra S.K. Rao, Encyclopaedia of Indian Medicine: historical perspective, Volume 1, 2005, 94–98
- ↑ K. Mangathayaru (2013). Pharmacognosy: An Indian perspective. Pearson education. p. 54. ISBN 978-93-325-2026-4. https://books.google.com/books?id=2UQ8BAAAQBAJ&pg=PA54.
- ↑ 157.0 157.1 Lock 2001, p. 607
- ↑ Lock 2001, p. 651
- ↑ Lock 2001, p. 652
- ↑ Lock 2001, pp. 651–652
- ↑ Brett, F. H. (1840). A practical essay on some of the principal surgical diseases of India. Calcutta, India: W. Thacker & Company. p. 458. https://archive.org/stream/practicalessayon00bretuoft#page/458/mode/2up. Retrieved 6 January 2015.
- ↑ "Legal Status of Traditional Medicine and Complementary/Alternative Medicine: A Worldwide Review". World Health Organization (WHO). p. 132. http://apps.who.int/medicinedocs/en/d/Jh2943e/8.4.html.
Cited references
- Chopra, Ananda S. (2003). "Āyurveda". in Selin, Helaine. Medicine across cultures: history and practice of medicine in non-western cultures. Kluwer Academic. pp. 75–83. ISBN 978-1-4020-1166-5. https://books.google.com/books?id=of-gv8-pPcsC&pg=PA75.
- Dwivedi, Girish; Dwivedi, Shridhar (2007). "History of Medicine: Sushruta – the Clinician – Teacher par Excellence". Indian Journal of Chest Diseases and Allied Sciences 49: 243–244. http://medind.nic.in/iae/t07/i4/iaet07i4p243.pdf. (Republished by National Informatics Centre, Government of India.)
- Finger, Stanley (2001). Origins of Neuroscience: A History of Explorations into Brain Function. Oxford University Press. ISBN 978-0-19-514694-3.
- Kutumbian, P. (1999). Ancient Indian Medicine. Andhra Pradesh, India: Orient Longman. ISBN 978-81-250-1521-5.
- Lock, Stephen (2001). The Oxford Illustrated Companion to Medicine. Oxford University Press. ISBN 978-0-19-262950-0. https://archive.org/details/oxfordillustrate00step.
- Underwood, E. Ashworth; Rhodes, P. (2008). "History of Medicine". Encyclopædia Britannica (2008 ed.).
- Wujastyk, D. (2003a). The Roots of Ayurveda: Selections from Sanskrit Medical Writings. Penguin Books. ISBN 978-0-14-044824-5. https://books.google.com/books?id=sJOEMwrVyRcC&q=The+Roots+of+Ayurveda:+Selections+from+Sanskrit+Medical+Writings.&pg=PR1.
Further reading
- Drury, Heber (1873). The Useful plants of India. William H Allen & Co., London. ISBN 978-1-4460-2372-3. https://archive.org/stream/usefulplantsind01drurgoog#page/n5/mode/2up.
- Dymock, William (1890). Pharmacographia Indica A history of principal drugs of vegetable origin in British India. 1. London, Bombat, Calcutta: Kegan Paul, Trench, Trübner & Co, Education Society Press, Byculla, Thacker, Spink and Co. https://www.biodiversitylibrary.org/item/36345#page/1/mode/1up.
- Hoernle, Rudolf August Friedrich (1907). Studies in the Medicine of Ancient India: Part I: Osteology. Clarendon Press, Oxford. https://archive.org/stream/studiesinmedicin01hoeruoft#page/n3/mode/2up.
- Pattathu, Anthony George (2018). Ayurveda and Discursive Formations between Religion, Medicine and Embodiment: A Case Study from Germany. In: Lüddeckens, D., & Schrimpf, M. (2018). Medicine - religion - spirituality: Global perspectives on traditional, complementary, and alternative healing. Bielefeld: transcript Verlag. ISBN:978-3-8376-4582-8, pp. 133–166.
- Patwardhan, Kishore (2008). Pabitra Kumar Roy. ed. Concepts of Human Physiology in Ayurveda. Samyak Vak Series-14. Sarnath, Varanasi: Central Institute of Higher Tibetan Studies. pp. 53–73. ISBN 978-81-87127-76-5. http://cogprints.org/7033/1/Chapter_in_sowarigpa_and_ayurveda.pdf.
- Wise, Thomas T. (1845). Commentary on the Hindu System of Medicine. Calcutta: Thacker & Co.. https://archive.org/stream/commentaryonhind00wise#page/n3/mode/2up.
- Wujastyk, Dominik (2011). Indian Medicine. Oxford University Press. doi:10.1093/obo/9780195399318-0035. http://www.oxfordbibliographies.com/document/obo-9780195399318/obo-9780195399318-0035.xml.. A bibliographical survey of the history of Indian medicine.
- WHO guidelines on safety monitoring of herbal medicines in pharmacovigilance systems
- Use Caution With Ayurvedic Products - US Food and Drug Administration.
External links
- Ayurveda at Curlie
- Ayurveda: Benchmarks for trainings in traditional/complementary and alternative medicine World Health Organization (WHO)
- National Library of Ayurveda Medicine
 KSF
KSF