Omega-3 acid ethyl esters
Topic: Chemistry
 From HandWiki - Reading time: 8 min
From HandWiki - Reading time: 8 min
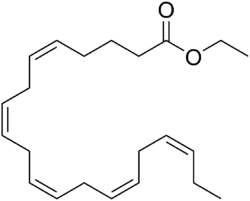 Chemical structure of ethyl eicosapentaenoate, an important omega-3-acid ethyl ester | |
| Combination of | |
|---|---|
| Eicosapentaenoic acid | Antilipemic agent |
| Docosahexaenoic acid | Antilipemic agent |
| Clinical data | |
| Trade names | Lovaza, Omtryg, others |
| AHFS/Drugs.com | Monograph |
| License data |
|
| Pregnancy category |
|
| Routes of administration | By mouth |
| ATC code |
|
| Legal status | |
| Legal status | |
| Identifiers | |
| CAS Number | |
| DrugBank | |
| UNII | |
| KEGG | |
Omega-3-acid ethyl esters are a mixture of ethyl eicosapentaenoic acid and ethyl docosahexaenoic acid, which are ethyl esters of the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) found in fish oil.[3] Together with dietary changes, they are used to treat high blood triglycerides which may reduce the risk of pancreatitis.[3][4] They are generally less preferred than statins, and use is not recommended by NHS Scotland as the evidence does not support a decreased risk of heart disease.[3][5][6] Omega-3-acid ethyl esters are taken by mouth.[3]
Common side effects include burping, nausea, and an upset abdomen.[3][5] Serious side effects may include liver problems and anaphylaxis.[3] While use in pregnancy has not been well studied, some omega-3 fatty acids appear beneficial.[1] How it works is not entirely clear.[3]
Omega-3-acid ethyl ester medicines were approved for medical use in the European Union in 2000 and in the United States in 2004.[3][6][7] Beyond the branded prescription formulation, it is also available as a generic medication and over the counter.[3][5] In 2020, it was the 199th most commonly prescribed medication in the United States, with more than 2 million prescriptions.[8][9]
Medical use
Omega-3 acid ethyl esters are used in addition to changes in diet to reduce triglyceride levels in adults with severe (≥ 500 mg/dL) hypertriglyceridemia.[10] In the European Union and other major markets outside the US, omega-3 acid ethyl esters are indicated for hypertriglyceridemia by itself, or in combination with a statin for people with mixed dyslipidemia.[2][6]
Intake of large doses (2.0 to 4.0 g/day) of long-chain omega-3 fatty acids as prescription drugs or dietary supplements are generally required to achieve significant (> 15%) lowering of triglycerides, and at those doses, the effects can be significant (from 20% to 35% and even up to 45% in individuals with levels greater than 500 mg/dL). It appears that both eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) lower triglycerides, but DHA appears to raise LDL cholesterol more than EPA, while DHA raises HDL cholesterol while EPA does not.[11]
Other fish-oil based drugs
Other omega-3 fish oil-based prescription drugs on the market have similar uses and mechanisms of action.[12]
- Ethyl eicosapentaenoic acid (Vascepa). EPA-only ethyl esters.[13]
- Omega-3 carboxylic acids (Epanova). This product contains free fatty acids, not ethyl esters.[14] It is currently withdrawn from the market by the manufacturer (AstraZeneca) and is thus unavailable to patients.[15] AstraZeneca voluntarily discontinued Phase III clinical trials for futility.[16]
Dietary supplements
There are many fish oil dietary supplements on the market.[17] There appears to be little difference in effect between dietary supplement and prescription forms of omega-3 fatty acids as to ability to lower triglycerides, but the ethyl ester products work less well when taken on an empty stomach or with a low-fat meal.[11] The ingredients of dietary supplements are not as carefully controlled as prescription products and have not been tested in clinical trials as such drugs have.[18] Prescription omega-3 products are more concentrated, requiring fewer softgels for the same daily dose.[17]
In people with CKD who require hemodialysis, there is a risk that vascular blockage due to clotting, may prevent dialysis therapy from being possible. Omega-3 fatty acids contribute to the production of eicosanoid molecules that reduce clotting. However, a Cochrane review in 2018 did not find clear evidence that omega-3 supplementation has any impact on the prevention of vascular blockage in people with CKD.[19] There was also moderate certainty that supplementation did not prevent hospitalisation or death within a 12-month period.[19]
Side effects
Special caution should be taken with people who have fish and shellfish allergies.[10] In addition, as with other omega-3 fatty acids, taking omega-3 acid ethyl esters puts people who are on anticoagulants at risk for prolonged bleeding time.[10][11]
Side effects include stomach ache, burping, and a bad taste; some people on very high doses (8g/day) in clinical trials had atrial fibrillation.[10]
Omega-3 acid ethyl esters have not been tested in pregnant women and are rated pregnancy category C; it is excreted in breast milk and the effects on infants are not known.[10]
Pharmacology
After ingestion, omega-3-acid ethyl esters are metabolized mostly in the liver like other dietary fatty acids.[2]
Mechanism of action
Omega-3-acid ethyl esters, like other omega-3 fatty acid-based drugs, appears to reduce production of triglycerides in the liver and to enhance clearance of triglycerides from circulating very low-density lipoprotein (VLDL) particles. The way it does that is not clear, but potential mechanisms include increased breakdown of fatty acids; inhibition of diglyceride acyltransferase, which is involved in biosynthesis of triglycerides in the liver; and increased activity of lipoprotein lipase in blood.[2][12] The synthesis of triglycerides is reduced in the liver because EPA and DHA are poor substrates for the enzymes responsible for triglyceride synthesis.
Physical and chemical properties
The active ingredient is concentrated omega-3 acid ethyl esters that are made from fish body oils that are purified and esterified.[20] For the Lovaza product, each 1000 mg softgel capsule contains 840 mg omega-3 fatty acids: eicosapentaenoic acid ethyl ester (460 mg) and docosahexaenoic acid ethyl ester (380 mg).[2]
History
Pronova BioPharma ASA had its roots in Norway's codfish liver oil industry. The company was founded in 1991 as a spinout from the JC Martens company, which in turn was founded in 1838 in Bergen, Norway.[21] Pronova developed the concentrated omega-3-acid ethyl esters formulation that is the active pharmaceutical ingredient of Lovaza.[20]
Pronova won approvals to market the drug, called Omacor in Europe (and initially in the US), in several European countries in 2001 after conducting a three and a half year trial in 11,000 subjects;[22] The company partnered with other companies like Pierre Fabre in France.[23] In 2004, Pronova licensed the US and Puerto Rican rights to Reliant Therapeutics, whose business model was in-licensing of cardiovascular drugs.[24] In that same year, Reliant and Pronova won FDA approval for the drug,[25] and it was launched in the US and Europe in 2005. Global sales in 2005 were $144M, and by 2008, they were $778M.[26] In 2007 GlaxoSmithKline acquired Reliant for $1.65 billion in cash.[27]
In 2009, generic companies Teva Pharmaceuticals and Par Pharmaceutical made clear their intentions to file Abbreviated New Drug Applications ("ANDAs") to bring generics to market, and in April 2009, Pronova sued them from infringing the key US patents covering Lovaza, US 5,656,667 (due to expire in April 2017), US 5,502,077 (exp March 2013). Subsequently, in May 2012, a district court ruled in Pronova's favor, saying that the patents were valid.[28][29][30] The generic companies appealed, and in September 2013, the Federal Circuit reversed, saying that because more than one year before Pronova's predecessor company applied for a patent, it had sent samples of the fish oil used in Lovaza to a researcher for testing. This event thus constituted "public use" that invalidated the patent in question.[31][32] Generic versions of Lovaza were introduced in America in April 2014.[33]
Pronovo has continued to manufacture the ingredients in Lovaza, and in 2012, BASF announced it would acquire Pronova for $844 million.[34] The deal closed in 2013.[35]
Brand names
- Lovaza] (US)/Omacor (Europe).[36] It was approved in the United States in 2004.[37]
- Omtryg is another brand of omega-3-acid ethyl esters developed by Trygg Pharma, Inc. and was approved by the FDA in 2004.[38]
- As of March 2016, there were four additional generic versions.[39]
References
- ↑ 1.0 1.1 "Omega-3 polyunsaturated fatty acids Use During Pregnancy" (in en). https://www.drugs.com/pregnancy/omega-3-polyunsaturated-fatty-acids.html.
- ↑ 2.0 2.1 2.2 2.3 2.4 "Omacor". Summary of Product Characteristics (SmPC). Electronic Medicines Compendium (EMC). 11 December 2019. https://www.medicines.org.uk/emc/medicine/10312.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 "Omega-3-acid Ethyl Esters Monograph for Professionals" (in en). American Society of Health-System Pharmacists. https://www.drugs.com/monograph/omega-3-acid-ethyl-esters.html.
- ↑ "A Review of Clinical Practice Guidelines for the Management of Hypertriglyceridemia: A Focus on High Dose Omega-3 Fatty Acids". Advances in Therapy 34 (2): 300–323. February 2017. doi:10.1007/s12325-016-0462-y. PMID 27981496.
- ↑ 5.0 5.1 5.2 British national formulary : BNF 76 (76 ed.). Pharmaceutical Press. 2018. pp. 206–207. ISBN 9780857113382.
- ↑ 6.0 6.1 6.2 "Omega-3 fatty acid medicines". 17 September 2018. https://www.ema.europa.eu/en/medicines/human/referrals/omega-3-fatty-acid-medicines.
- ↑ "Drug Approval Package: Omacor (Omega-3-Acid Ethyl Esters) NDA #021654". 24 December 1999. https://www.accessdata.fda.gov/drugsatfda_docs/nda/2004/21-654_Omacor.cfm.
- ↑ "The Top 300 of 2020". https://clincalc.com/DrugStats/Top300Drugs.aspx.
- ↑ "Omega-3-acid Ethyl Esters - Drug Usage Statistics". https://clincalc.com/DrugStats/Drugs/Omega3AcidEthylEsters.
- ↑ 10.0 10.1 10.2 10.3 10.4 "Lovaza Label". U.S. Food and Drug Administration. 2016. http://www.accessdata.fda.gov/drugsatfda_docs/label/2014/021654s041lbl.pdf. Updated labels available at "Lovaza approval history". U.S. Food and Drug Administration. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Set_Current_Drug&ApplNo=204977&DrugName=OMTRYG&ActiveIngred=OMEGA%2D3%2DACID%20ETHYL%20ESTERS&SponsorApplicant=TRYGG&ProductMktStatus=1&goto=Search.Label_ApprovalHistory.
- ↑ 11.0 11.1 11.2 "National Lipid Association Recommendations for Patient-Centered Management of Dyslipidemia: Part 2". Journal of Clinical Lipidology 9 (6 Suppl): S1–122.e1. 2015. doi:10.1016/j.jacl.2015.09.002. PMID 26699442.
- ↑ 12.0 12.1 "Overview of prescription omega-3 fatty acid products for hypertriglyceridemia". Postgraduate Medicine 126 (7): 7–18. November 2014. doi:10.3810/pgm.2014.11.2828. PMID 25387209.
- ↑ "Vascepa (icosapent ethyl)". CenterWatch. http://www.centerwatch.com/drug-information/fda-approved-drugs/drug/1215/vascepa-icosapent-ethyl.
- ↑ "Epanova (omega-3-carboxylic acids)". CenterWatch. http://www.centerwatch.com/drug-information/fda-approved-drugs/drug/1324/epanova-omega-3-carboxylic-acids.
- ↑ Food and Drug Administration, Center for Drug Evaluation and Research (2021). Approved Drug Products with Therapeutic Equivalence Evaluations (41 ed.). Food and Drug Administration. p. 830. https://fda.gov/media/71474/download.
- ↑ "AstraZeneca to discontinue Epanova trial, expects $100 million writedown" (in en). Reuters. 13 January 2020. https://in.reuters.com/article/us-astrazeneca-study/astrazeneca-to-discontinue-epanova-trial-expects-100-million-writedown-idINKBN1ZC0JQ. Retrieved 15 January 2020.
- ↑ 17.0 17.1 "A Comparative Overview of Prescription Omega-3 Fatty Acid Products". Pharmacy and Therapeutics 40 (12): 826–57. December 2015. PMID 26681905.
- ↑ "Hypertriglyceridemia Pharmacologic Therapy". Medscape Drugs & Diseases. 14 April 2015. http://emedicine.medscape.com/article/126568-treatment#d8.
- ↑ 19.0 19.1 "Omega-3 fatty acids for dialysis vascular access outcomes in patients with chronic kidney disease". The Cochrane Database of Systematic Reviews 2018 (11): CD011353. November 2018. doi:10.1002/14651858.CD011353.pub2. PMID 30480758.
- ↑ 20.0 20.1 "Omega-3 ethylester concentrate". Adis Insight. Springer Nature Switzerland AG. http://adis.springer.com/drugs/800002488.
- ↑ "170 Year History". Epax. http://www.epax.com/pages/history.
- ↑ "Pronova wins Omacor approval". Pharma Times. 22 March 2001. http://www.pharmatimes.com/Article/01-03-22/Pronova_wins_Omacor_approval.aspx.
- ↑ "Omacor approved". ICIS Chemical Business. 26 March 2001. http://www.icis.com/resources/news/2001/03/26/135355/omacor-approved/.
- ↑ "German Court Invalidates Omega-3 Drug Patent". Law360. 27 November 2007. http://www.law360.com/articles/40998/german-court-invalidates-omega-3-drug-patent.
- ↑ "Omega-3-acid ethyl esters (Lovaza, formerly Omacor)". National PBM Drug Monograph. October 2005. http://www.pbm.va.gov/clinicalguidance/drugmonographs/Omega3acidethylestersLovazaformerlyOmacor.pdf.
- ↑ "Pronova Biopharma Pharmaceutical Production Facility, Denmark". Pharmaceutical Technology. http://www.pharmaceutical-technology.com/projects/pronova-biopharma/.
- ↑ "GSK to Acquire Reliant Pharmaceuticals for $1.65B". Genetic Engineering News. 21 November 2007. http://www.genengnews.com/gen-news-highlights/gsk-to-acquire-reliant-pharmaceuticals-for-1-65b/27018604/.
- ↑ U.S. Patent 5,656,667
- ↑ U.S. Patent 5,502,077
- ↑ "US District Court rules in Pronova BioPharma's favour on Lovaza(TM) patents". Press Release. Pronova BioPharma. 29 May 2012. http://www.evaluategroup.com/Universal/View.aspx?type=Story&id=298783.
- ↑ "Fed. Circ. Nixes Pronova's Patent Win Against Teva, Par". Law360. 12 September 2013. http://www.law360.com/articles/472235/fed-circ-nixes-pronova-s-patent-win-against-teva-par.
- ↑ Pronova Biopharma Norge AS v. Teva Pharmaceuticals, Inc, USA and Par Pharmaceutical, Inc. and Par Pharmaceutical Companies, Inc. (United States Court of Appeals for the Federal Circuit 2012-1498, -1499 12 September 2013). Text
- ↑ "Teva puts GSK and Amarin on notice with generic Lovaza launch". FiercePharmaMarketing. 9 April 2014. http://www.fiercepharmamarketing.com/story/teva-puts-gsk-and-amarin-notice-generic-lovaza-launch/2014-04-09.
- ↑ "BASF to snap up fish oil drugmaker Pronova BioPharma in $844M buyout". FierceBiotech. 21 November 2012. http://www.fiercebiotech.com/story/basf-snap-fish-oil-drugmaker-pronova-biopharma-844m-buyout/2012-11-21.
- ↑ "BASF lands Pronova making it a top omega-3 maker". FierceManufacturing. 22 January 2013. http://www.fiercepharmamanufacturing.com/story/basf-lands-pronova-making-it-top-omega-3-maker/2013-01-22.
- ↑ "Omega-3-acid Ethyl Esters Brand Name Changed from Omacor to Lovaza". University of Utah Pharmacy Services. 15 August 2007. http://pharmacyservices.utah.edu/alerts/251.html.
- ↑ "A Comparative Overview of Prescription Omega-3 Fatty Acid Products". P & T 40 (12): 826–857. December 2015. PMID 26681905.
- ↑ Omtryg Label Revised April 2014
- ↑ "Omega-3 acid ethyl esters products". FDA. http://www.accessdata.fda.gov/scripts/cder/drugsatfda/index.cfm?fuseaction=Search.Overview&DrugName=OMEGA-3-ACID%20ETHYL%20ESTERS.
External links
- "Lovaza". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/lovaza.
- "Omega-3-acid ethyl esters". Drug Information Portal. U.S. National Library of Medicine. https://druginfo.nlm.nih.gov/drugportal/name/omega-3-acid%20ethyl%20esters.
 |
 KSF
KSF