Opioid Withdrawal Syndrome
Topic: Chemistry
 From HandWiki - Reading time: 10 min
From HandWiki - Reading time: 10 min
Opioid withdrawal syndrome, is the characteristic syndrome of symptoms that arise from opioid withdrawal experienced when an opioid dependent user suddenly reduces or stops their use of opioids.[1]
All opioids, both recreational drugs and medications can lead to opioid withdrawal symptoms. Signs and symptoms of withdrawal include drug craving, anxiety, nervousness, gastrointestinal upset, sweating, and an increased heart rate.
Opioid withdrawal syndrome is caused by the increase in the number of opioid receptors in the locus coeruleus a nucleus in the brainstem following long-term use of opioids. Once the opioid is withdrawn, a high number of opioid receptors in the brain will be stimulated at the same time, leading to withdrawal symptoms. Without proper treatment of withdrawal, there is a high tendency of relapse of opioid usage.
Opioid withdrawal syndrome is usually treated by opioid replacement therapy, using methadone, buprenophrine, naltrexone and naloxone to slowly reduce the drug until it is completely eliminated.
Common opioid use
Heroin
Some individuals being prescribed with opioids may turn out misusing the drugs and opt for heroin, due to its lower price and availability in the underground market.[2] Heroin becomes a highly available option for illegal opioid abuse. The withdrawal effect can be settled with illegally self-purchased heroin, however, this may precipitate the problem into a more severe case.
Oxycodone and Hydrocodone
Oxycodone and hydrocodone are the two opioid analgesics that are being prescribed the most in US. Yet, they are also the most misused opioids that lead to medical errors in legal settings.
Codeine
Codeine is often prescribed to treat mild to moderate pain or used as cough suppressant. However, due to its pharmacological effects, codeine may lead to addiction and drug abuse by its users.
Fentenyl
Fentanyl is a synthetic opioid analgesic, which is 30 to 50 times more potent than heroin.[3] Due to its high potency, the risk of overdose is relatively higher when compared to the administration of other opioids with mild effects. Fentanyl's strong potency may lead to opioid withdrawal syndrome. This is because human body is highly sensitive to the dose of fentanyl. A slight change in fentanyl dose will create a huge response in human body. Therefore, the dose used in pain management should be very precise to minimise the symptoms due to withdrawal of drug use.
Signs and symptoms
All opioid withrawal produces similar signs and symptoms, and their severity and duration depends on the type of opioid taken.
The symptoms of opioid withdrawal syndrome can be divided into several areas: Gastrointestinal distress, Flu-like symptoms and Arousal of the nervous system[4].
Gastrointestinal distress: Pain in abdomen, diarrhoea, nausea, or vomiting may be experienced[4].
Flu-like symptoms: Excessive tear secretion, rhinorrhea, excessive sweating, uncontrolled shivering and goosebumps may be experienced[4].
Arousal of the nervous system: dilation of pupils, increase in blood pressure and heart rate, irritability and anxiety, restlessness, insomnia, tremor are often present. In some uncommon cases, low grade fever and tactile sensitivity may occur[4].
Others: There are other signs and symptoms including yawning, sneezing, anorexia, vertigo, muscle ache and leg cramps[4].
The order of symptoms and the most prominent symptoms can vary among individuals and across various opioid drugs. The onset of symptoms usually takes place after two to three half-life of the withdrawn opioid drug. If opioid withdrawal syndrome is left untreated, it can be uncomfortable and may be life threatening.
Pathophysiology
The locus coeruleus is the principal site in the brainstem that would trigger an onset of opioid withdrawal syndrome.
Locus coeruleus contains noradrenergic receptors. Long-term usage of opioid analgesic can lead to the proliferation of opioid receptors cells.[6][7] This is known as the adaptive mechanism to counteract the prolong suppression of pain signals. When the drug is absent, pain signals could not be suppressed, and due to the increase number of opioid receptors, the adaptive mechanism will be too overwhelming. Endogenous substances like cAMP will be abnormally high, leading to alteration of physiological condition which is known to be withdrawal symptoms.
Grey matter and nucleus raphe magnus are also involved in the development of opioid withdrawal syndrome.
Due to the difference in lipophilicity and mode of release between opioid analgesics, the severity and duration of withdrawal symptoms may differ.
The followings are the general descriptions of duration of opioid withdrawal symptoms[8]:
- High intake for a long duration (> 6 Months) is associated with more severe level of withdrawal symptoms.
- Short-acting or slow-released opioids result in more rapid onset and shorter duration of withdrawal symptoms.
- Longer-acting opioids results in slower onset but longer duration of withdrawal symptoms.
Diagnosis
In order to be diagnosed with opioid withdrawal syndrome, the individual should be either stopping (or reducing) heavy and prolonged intake of opioid drug or being administered with an opioid antagonist after a period of opioid use[9]. Three or more signs and symptoms listed above should develop within minutes to several days after cessation of opioid drug. The signs or symptoms should hamper the individuals social, occupational, or other aspects of life significantly.[9]
Severity of symptoms
The severity of symptoms can be assessed by validated withdrawal scales, such as the Clinical Opiate Withdrawal Scale (COWS).[10][11]
Treatment and Management
Behavior management strategies
Some drug users' behaviours may be too disruptive to manage, so that management strategies can be applied to address their behavior.
Medications (opioid agonist or opioid agonist-antagonists)
Medications should be used to manage opioid withdrawal over abrupt cessation of opioids. This is due to the fact that abrupt stopping of opioid use will lead to strong cravings which lead to relapse. The principle of managing the syndrome is to allow the concentration of drugs in blood to fall to near zero. This allows the body to adapt to the absence of drugs in order to reduce the withdrawal symptoms. The most commonly used strategy is to offer opioid drug users with long-acting opioid drugs and slowly taper the dose of the drug. Methadone and buprenorphine are often used in treating opioid withdrawal syndrome.They are opium derivatives that have a long half-life. This makes them long-acting drugs.
Methadone maintenance treatment (MMT)
Main article: Methadone maintenance
Methadone is an opioid agonist that is often prescribed to treat pain, since it has a similar structure to opioid analgesics and can target the opioid receptors to produce pain-killing effect.[12]
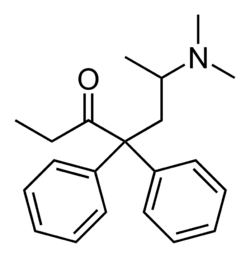
Methadone has long half-life such that it can be given once daily to ease the withdrawal symptoms. This can prevent the continuous consumption on other types of opioids such as heroin or morphine.
Buprenorphine
Buprenorphine is an opioid analgesic commonly used in clinical pain management.[13]

It is a mixed μ-receptor agonist-antagonist which preferentially target on μ-receptors at lower concentration.[14] Some research findings show that buprenorphine at low dose exhibits complex pharmacology on different types of opioid receptors, lead to its availability to act as an antagonist to these receptors [15][16][17][18][19][20]. Therefore, it is one of the possible pharmacological options in treating sudden opioid withdrawal [11], but the mechanisms of action are not yet fully known.


Similar to MMT, the buprenorphine treatment is approved by the United States Food and Drug Administration in 2002, but the self-purchase and administration of buprenorphine is limited under the Drug Addiction Treatment Act.
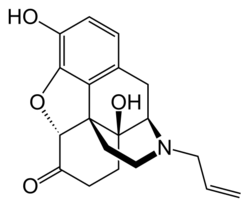
Naltrexone and naloxone
Naltrexone and naloxone are typical opioid antagonists readily used in clinical settings to produce detoxifaction effect.[7]

Naltrexone, unlike buprenorphine, is a pure opioid antagonist. It interacts the opioid receptors in a very different mechanism when compared to buprenorphine.
Naloxone has a chemical structure very similar to Naltrexone, differing only by the group bonded to the tertiary amine, where the branch is not attaching to the ring. In Naltrexone, the branch contains a cyclopropyl ring, while in Naloxone, the branch is a propene chain. The propene chain on Naloxone makes it a relatively more reactive compound such that it provides faster onset of effect.
External links
References
- ↑ Diagnostic and statistical manual of mental disorders : DSM-5. (5th ed.). American Psychiatric Association. 2013. pp. 547–549. ISBN 9780890425541.
- ↑ Abuse, National Institute on Drug (2020-04-17). "Opioid Overdose Crisis" (in en). https://www.drugabuse.gov/drugs-abuse/opioids/opioid-overdose-crisis.
- ↑ "American Carnage | Christopher Caldwell" (in en). https://www.firstthings.com/article/2017/04/american-carnage.
- ↑ 4.0 4.1 4.2 4.3 4.4 Sevarino, Kevin A (1 July 2019). "Opioid withdrawal in adults: Clinical manifestations, course, assessment, and diagnosis". https://www.uptodate.com/contents/opioid-withdrawal-in-adults-clinical-manifestations-course-assessment-and-diagnosis.
- ↑ Lin, Hause; Vartanian, Oshin (2018-06-07). "A Neuroeconomic Framework for Creative Cognition". Perspectives on Psychological Science 13. doi:10.1177/1745691618794945. https://www.researchgate.net/publication/325625804_A_Neuroeconomic_Framework_for_Creative_Cognition.
- ↑ Rehni, Ashish K.; Jaggi, Amteshwar S.; Singh, Nirmal (2013-02-01). "Opioid withdrawal syndrome: emerging concepts and novel therapeutic targets". CNS & neurological disorders drug targets 12 (1): 112–125. doi:10.2174/1871527311312010017. ISSN 1996-3181. PMID 23244430. https://www.ncbi.nlm.nih.gov/pubmed/23244430.
- ↑ 7.0 7.1 Shah, Mansi; Huecker, Martin R. (2020), "Opioid Withdrawal", StatPearls (StatPearls Publishing), PMID 30252268, http://www.ncbi.nlm.nih.gov/books/NBK526012/, retrieved 28 March 2020
- ↑ "Opioid withdrawal management: SA Health". https://www.sahealth.sa.gov.au/wps/wcm/connect/public+content/sa+health+internet/clinical+resources/clinical+topics/substance+misuse+and+dependence/substance+withdrawal+management/opioid+withdrawal+management.
- ↑ 9.0 9.1 "Yes, people can die from opiate withdrawal". https://ndarc.med.unsw.edu.au/blog/yes-people-can-die-opiate-withdrawal.
- ↑ "Clinical Opiate Withdrawal Scale". https://www.drugabuse.gov/sites/default/files/files/ClinicalOpiateWithdrawalScale.pdf.
- ↑ "Clinical Opiate Withdrawal Scale". http://www.naabt.org/documents/cows_induction_flow_sheet.pdf.
- ↑ "Opioid and Opiate Withdrawal: Symptoms and Treatments" (in en). https://www.healthline.com/health/opiate-withdrawal.
- ↑ Lutfy, Kabirullah; Cowan, Alan (Oct 2004). "Buprenorphine: A Unique Drug with Complex Pharmacology". Current neuropharmacology 2 (4): 395–402. doi:10.2174/1570159043359477. ISSN 1570-159X. PMID 18997874. PMC 2581407. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2581407/.
- ↑ Virginia, Leesa M. Prunty, PharmD. "Acute Opioid Withdrawal: Identification and Treatment Strategies" (in en). https://www.uspharmacist.com/article/acute-opioid-withdrawal-identification-and-treatment-strategies.
- ↑ Huang, P.; Kehner, G. B.; Cowan, A.; Liu-Chen, L. Y. (May 2001). "Comparison of pharmacological activities of buprenorphine and norbuprenorphine: norbuprenorphine is a potent opioid agonist". The Journal of Pharmacology and Experimental Therapeutics 297 (2): 688–695. ISSN 0022-3565. PMID 11303059. https://www.ncbi.nlm.nih.gov/pubmed/11303059.
- ↑ Negus, S. S.; Bidlack, J. M.; Mello, N. K.; Furness, M. S.; Rice, K. C.; Brandt, M. R. (Nov 2002). "Delta opioid antagonist effects of buprenorphine in rhesus monkeys". Behavioural Pharmacology 13 (7): 557–570. doi:10.1097/00008877-200211000-00005. ISSN 0955-8810. PMID 12409994. https://www.ncbi.nlm.nih.gov/pubmed/12409994.
- ↑ Sadée, W.; Rosenbaum, J. S.; Herz, A. (Oct 1982). "Buprenorphine: differential interaction with opiate receptor subtypes in vivo". The Journal of Pharmacology and Experimental Therapeutics 223 (1): 157–162. ISSN 0022-3565. PMID 6288917. https://www.ncbi.nlm.nih.gov/pubmed/6288917.
- ↑ Sadée, W.; Richards, M. L.; Grevel, J.; Rosenbaum, J. S. (1983). "In vivo characterization of four types of opioid binding sites in rat brain". Life Sciences 33 Suppl 1: 187–189. doi:10.1016/0024-3205(83)90474-5. ISSN 0024-3205. PMID 6141486. https://www.ncbi.nlm.nih.gov/pubmed/6141486.
- ↑ Villiger, J. W. (Mar 1984). "Binding of buprenorphine to opiate receptors. Regulation by guanyl nucleotides and metal ions". Neuropharmacology 23 (3): 373–375. doi:10.1016/0028-3908(84)90201-6. ISSN 0028-3908. PMID 6328350. https://www.ncbi.nlm.nih.gov/pubmed/6328350.
- ↑ Villiger, J. W.; Taylor, K. M. (1981-12-28). "Buprenorphine : characteristics of binding sites in the rat central nervous system". Life Sciences 29 (26): 2699–2708. doi:10.1016/0024-3205(81)90529-4. ISSN 0024-3205. PMID 6276633. https://www.ncbi.nlm.nih.gov/pubmed/6276633.
This article needs additional or more specific categories. (June 2020) |
 KSF
KSF




