Selective serotonin reuptake inhibitor
Topic: Chemistry
 From HandWiki - Reading time: 48 min
From HandWiki - Reading time: 48 min
| Selective serotonin reuptake inhibitor | |
|---|---|
| Drug class | |
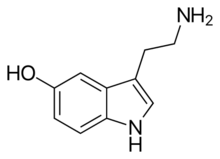 Serotonin, the neurotransmitter that is involved in the mechanism of action of SSRIs | |
| Class identifiers | |
| Synonyms | Serotonin-specific reuptake inhibitors, serotonergic antidepressants[1] |
| Use | Major depressive disorder, anxiety disorders, Post Traumatic Stress Disorder, Eating Disorders |
| ATC code | N06AB |
| Biological target | Serotonin transporter |
| Clinical data | |
| Drugs.com | Drug Classes |
| Consumer Reports | Best Buy Drugs |
| External links | |
| MeSH | D017367 |
Selective serotonin reuptake inhibitors (SSRIs) are a class of drugs that are typically used as antidepressants in the treatment of major depressive disorder, anxiety disorders, and other psychological conditions.
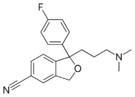
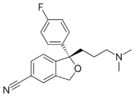
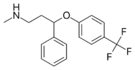
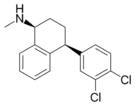
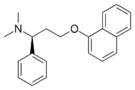
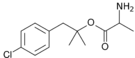
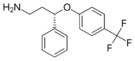
SSRIs primarily work by blocking serotonin reabsorption (reuptake) via the serotonin transporter, leading to gradual changes in brain signaling and receptor regulation, with some also interacting with sigma-1 receptors, particularly fluvoxamine, which may contribute to cognitive effects. Marketed SSRIs include six main antidepressants—citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, and sertraline—and dapoxetine, which is indicated for premature ejaculation. Fluoxetine has been approved for veterinary use in the treatment of canine separation anxiety.
SSRIs are the most widely prescribed antidepressants in many countries.[2] In adults, they are recommended as a first-line treatment for moderate to severe depression, while for mild depression non-drug treatments are preferred unless the patient chooses medication.[3] SSRIs have modest benefits over placebo, with uncertain clinical significance,[4] and may produce a substantial drug-specific response in only a minority of patients.[5] There is no consistent evidence linking depression to low serotonin levels, and long-term use may reduce serotonin concentrations.[6] Fifty years after their introduction, SSRIs remain widely used for depression, though their effectiveness, mechanisms, and role in medicalizing normal life remain debated.[7]
Medical uses
The main indication for SSRIs is major depressive disorder; however, they are frequently prescribed for anxiety disorders, such as social anxiety disorder, generalized anxiety disorder, panic disorder, obsessive–compulsive disorder (OCD), eating disorders, chronic pain, and, in some cases, for posttraumatic stress disorder (PTSD). They are also frequently used to treat depersonalization disorder, although with varying results.[8]
Depression
In adults
In 2022, the UK National Institute for Health and Care Excellence (NICE) recommended that antidepressants be offered as a first-line treatment for moderate to severe depression, but for mild depression, non-drug interventions are preferred unless the patient chooses medication.[3] They recommended that antidepressants should not be routinely offered for mild depression and should generally be used only if non-drug treatments fail or the patient prefers medication.[3]
In a 2018 review, all 21 studied antidepressants were more effective than placebo for major depressive disorder.[9] SSRIs remain the most widely prescribed antidepressants, emerging options like anti-inflammatory drugs and ketamine may have higher efficacy and remission rates in treating depression.[10]
The commonly used definition of antidepressant "response" as a 50% symptom reduction dichotomizes continuous data, which methodologists note can inflate effect sizes, exaggerate drug–placebo differences, and may not reliably indicate clinical significance.[11][12] A large FDA trial analysis found that SSRIs and other antidepressants produced only modest average benefits over placebo, with about 15% of patients experiencing a substantial drug-specific response.[5] SSRIs and other antidepressants may have average treatment effects that fall below the minimal important difference on common depression outcome measures, leaving their clinical significance in acute moderate-to-severe depression uncertain.[4]
There is no consistent evidence that depression is caused by lowered serotonin activity or concentrations, with some data suggesting that long-term antidepressant use may reduce serotonin levels.[6]
In children
The NICE Guideline recommends that SSRIs should not be used to treat depression in children and young people, except for fluoxetine, which may be considered for moderate to severe depression when psychological therapies alone are insufficient.[13] In the United States, they are approved for use in pediatric patients; however, individuals under 25 years of age should be closely monitored for an increased risk of suicidality, as indicated by the FDA black box warning.[14]
SSRIs have the best outcomes when combined with cognitive-behavioral therapy.[15] Their benefits are modest and tolerability varies.[16] The benefits may be clinically unimportant and there are uncertain effects on suicide risk.[17]
Social anxiety disorder
SSRIs show some evidence of effectiveness for social anxiety disorder, including reducing relapse and disability, but the overall quality of evidence is low to moderate and tolerability is slightly lower than placebo.[18]
Post-traumatic stress disorder
Two SSRIs are FDA-approved for PTSD: paroxetine and sertraline.[19] The 2023 VA/DoD guideline for PTSD recommends the SSRIs sertraline and paroxetine as first-line pharmacological treatments when trauma-focused therapy is unavailable or not preferred; evidence for other SSRIs is insufficient, and medications are recommended to be tailored to each patient's individual needs.[19] A 2022 Cochrane review found that SSRIs improve PTSD symptoms in 58% of patients compared with 35% on placebo (RR 0.66) and are considered first-line treatment.[20]
Generalized anxiety disorder
SSRIs are recommended by the National Institute for Health and Care Excellence (NICE) for the treatment of generalized anxiety disorder (GAD) in adults who have not responded to initial interventions such as education, self-help strategies, or psychological therapies.[21]
SSRIs are more effective than placebo for treating GAD with similar overall acceptability, though they increase dropout due to adverse effects.[22]
Obsessive–compulsive disorder
In Canada, SSRIs are a first-line treatment of adult obsessive–compulsive disorder (OCD).[23] In the UK, they are first-line treatment only with moderate to severe functional impairment and as second-line treatment for those with mild impairment, though, as of early 2019, this recommendation is being reviewed.[24][25]
SSRIs are more effective than placebo for reducing OCD symptoms and global severity in children and adolescents, and combining them with exposure therapy is probably more effective than using an SSRI alone.[26]
Panic disorder
SSRIs are approved to treat panic disorder.[27][28] SSRIs may be more effective than placebo in reducing panic disorder symptoms, but they are associated with a higher risk of adverse effects and may be less well tolerated.[29]
Eating disorders
Antidepressants are recommended as an alternative or additional first step to self-help programs in the treatment of bulimia nervosa.[30] SSRIs (fluoxetine in particular) are preferred over other anti-depressants due to their acceptability, tolerability, and superior reduction of symptoms in short-term trials. Long-term efficacy remains poorly characterized.
Similar recommendations apply to binge eating disorder.[30] SSRIs provide short-term reductions in binge eating behavior, but have not been associated with significant weight loss.[31]
Clinical trials have generated mostly negative results for the use of SSRIs in the treatment of anorexia nervosa.[32] Treatment guidelines from the National Institute of Health and Clinical Excellence[30] recommend against the use of SSRIs in this disorder. Those from the American Psychiatric Association note that SSRIs confer no advantage regarding weight gain, but that they may be used for the treatment of co-existing depression, anxiety, or OCD.[31]
Stroke recovery
SSRIs have been used off-label in the treatment of stroke patients, including those with and without symptoms of depression. A 2021 meta-analysis of randomized controlled clinical trials found no evidence pointing to their routine use to promote recovery following stroke.[33]
Premature ejaculation
SSRIs are effective for the treatment of premature ejaculation. Taking SSRIs on a chronic, daily basis is more effective than taking them prior to sexual activity.[34] The increased efficacy of treatment when taking SSRIs on a daily basis is consistent with clinical observations that the therapeutic effects of SSRIs generally take several weeks to emerge.[35] Sexual dysfunction ranging from decreased libido to anorgasmia is usually considered to be a significantly distressing side effect which may lead to noncompliance in patients receiving SSRIs.[36] However, for those with premature ejaculation, this very same side effect becomes the desired effect.
Other uses
SSRIs such as sertraline are effective in decreasing anger,[37] and fluoxetine has been proven effective in reduction of attack frequency and intensity for Raynaud syndrome.[38]
Side effects
Side effects vary among the individual drugs of this class. They may include akathisia.[39][40][41][42]
Sexual dysfunction
SSRIs can cause various types of sexual dysfunction such as anorgasmia, erectile dysfunction, diminished libido, genital numbness, and sexual anhedonia (pleasureless orgasm).[43] Sexual problems are common with SSRIs.[44] Poor sexual function is one of the most common reasons people stop the medication.[45]
The mechanism by which SSRIs may cause sexual side effects is not well understood as of 2021[update]. The range of possible mechanisms includes (1) nonspecific neurological effects (e.g., sedation) that globally impair behavior including sexual function; (2) specific effects on brain systems mediating sexual function; (3) specific effects on peripheral tissues and organs, such as the penis, that mediate sexual function; and (4) direct or indirect effects on hormones mediating sexual function.[46] Management strategies include: for erectile dysfunction the addition of a PDE5 inhibitor such as sildenafil; for decreased libido, possibly adding or switching to bupropion; and for overall sexual dysfunction, switching to nefazodone.[47] Buspirone is sometimes used off-label to reduce sexual dysfunction associated with the use of SSRIs.[48][49][50]
A number of non-SSRI drugs are not associated with sexual side effects (such as bupropion, mirtazapine, tianeptine, agomelatine, tranylcypromine, and moclobemide[51][52][53]).
Several studies have suggested that SSRIs may adversely affect semen quality.[54][55]
While trazodone (an antidepressant with alpha adrenergic receptor blockade) is a notorious cause of priapism, cases of priapism have also been reported with certain SSRIs (e.g., fluoxetine, citalopram).[56]
Post-SSRI sexual dysfunction
Post-SSRI sexual dysfunction (PSSD)[57][58] refers to a set of symptoms reported by some people who have taken SSRIs or other serotonin reuptake-inhibiting (SRI) drugs, in which sexual dysfunction symptoms persist for at least three months[59][60][61] after ceasing to take the drug. The status of PSSD as a legitimate and distinct pathology is contentious; several researchers have proposed that it should be recognized as a separate phenomenon from more common SSRI side effects.[62]
The reported symptoms of PSSD include reduced sexual desire or arousal, erectile dysfunction in males or loss of vaginal lubrication in females, persistent premature ejaculation (even in patients without a previous history of the condition),[63] difficulty having an orgasm or loss of pleasurable sensation associated with orgasm, and a reduction or loss of sensitivity in the genitals or other erogenous zones. Additional non-sexual symptoms are also commonly described, including emotional numbing, anhedonia, depersonalization or derealization, and cognitive impairment.[59][64] The duration of PSSD symptoms appears to vary among patients, with some cases resolving in months and others in years or decades; one analysis of patient reports submitted between 1992 and 2021 in the Netherlands listed a case which had reportedly persisted for 23 years.[60] The symptoms of PSSD are largely shared with post-finasteride syndrome (PFS) and post-retinoid sexual dysfunction (PRSD), two other poorly-understood conditions which have been suggested to share a common etiology with PSSD despite being associated with different types of medication.[65]
Diagnostic criteria for PSSD were proposed in 2022,[59] but as of 2023, there is no agreement on standards for diagnosis.[58] It is considered a distinct phenomenon from antidepressant discontinuation syndrome, post-acute withdrawal syndrome, and major depressive disorder,[64][62] and should be distinguished from sexual dysfunction associated with depression[64] and persistent genital arousal disorder.[58] There are limited treatment options for PSSD as of 2023 and no evidence that any individual approach is effective.[58] The mechanism by which SSRIs may induce PSSD is unclear.[64][58] However, various neurochemical, hormonal, and biochemical changes during SSRI use—such as reduced dopamine levels, increased serotonin, inhibition of nitric oxide synthase, and the blocking of cholinergic and alpha-1 adrenergic receptors—could account for their sexual adverse effects.[66][67] Additionally, SSRIs may cause peripheral changes by inhibiting serotonin receptors in peripheral nerves,[68][69] which may also play a role in PSSD. As of 2023, prevalence is unknown.[58] A 2020 review stated that PSSD is rare, underreported, and "increasingly identified in online communities".[70] A 2024 study investigating the prevalence of persistent post-treatment genital numbness among sexual and gender minority youth found 13.2% of SSRI users between the ages 15 and 29 reporting the symptom compared to 0.9% who had used other medications.[71]
Reports of PSSD have occurred with almost every SSRI (dapoxetine is an exception).[58] In 2019, the Pharmacovigilance Risk Assessment Committee of the European Medicines Agency (EMA) recommended that packaging leaflets of selected SSRIs and SNRIs should be amended to include information regarding a possible risk of persistent sexual dysfunction.[72] Following the EMA assessment, a safety review by Health Canada "could neither confirm nor rule out a causal link ... which was long lasting in rare cases", but recommended that "healthcare professionals inform patients about the potential risk of long-lasting sexual dysfunction despite discontinuation of treatment".[73] A 2023 review stated that ongoing sexual dysfunction after SSRI discontinuation was possible, but that cause and effect were undetermined.[58] The 2023 review cautioned that reports of sexual dysfunction cannot be generalized to wider practice as they are subject to a "high risk of bias", but agreed with the EMA assessment that cautionary labeling on SSRIs was warranted.[58]
On May 20, 2024, a lawsuit was filed by the organization Public Citizen, representing Dr. Antonei Csoka, against the United States Food and Drug Administration (FDA) for failing to act on a citizen petition submitted in 2018."Csoka v. FDA" (in en). https://www.citizen.org/litigation/csoka-v-fda/."FDA Sued Over Inaction on Citizen Petition Regarding Antidepressant Side Effects" (in en). 2024-05-20. https://www.citizen.org/news/fda-sued-over-inaction-on-citizen-petition-regarding-antidepressant-side-effects/. The petition seeks to have the risk of serious sexual side effects persisting after discontinuation mentioned in the product labels of SSRIs and SNRIs. The lawsuit was dismissed by the United States District Court for the District of Columbia on March 25, 2025, due to the plaintiff lacking legal standing, as the court found no specific informational or physical injury. The FDA has not mandated comprehensive PSSD warnings across all SSRI and SNRI labels, though fluoxetine (Prozac) has included a warning about persistent sexual side effects since 2011."Prozac (fluoxetine) Label". U.S. Food and Drug Administration. 2011-01-01. https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/018936s091lbl.pdf. Most other SSRI and SNRI labels address sexual dysfunction during use but not explicitly after discontinuation, and no broad public safety communications on PSSD have been issued by the FDA.
Emotional blunting
Certain antidepressants may cause emotional blunting, characterized by reduced intensity of both positive and negative emotions as well as symptoms of apathy, indifference, and amotivation.[74][75] It may be experienced as either beneficial or detrimental depending on the situation.[76] Higher doses of antidepressants seem to be more likely to produce emotional blunting than lower doses.[75] It can be decreased by reducing dosage, discontinuing the medication, or switching to a different antidepressant that may have less propensity for causing this side effect.[75] Specifically, this side effect has been particularly associated with serotonergic antidepressants like SSRIs and SNRIs and may be less with atypical antidepressants like bupropion, agomelatine, and vortioxetine.[75][77][78]
Confounding the understanding of emotional blunting is the fact that the same symptom can be caused by depression itself, and may instead be a sign of incomplete resolution of depression. However, there is a very large amount of subjective evidence showing that it is increasingly reported after starting the use of antidepressants, suggesting that antidepressants do induce emotional blunting. There does appear to be a positive correlation between depression symptoms (measured by HAD-D) and degree of emotional blunting (measured by OQuESA), but more research is needed to clarify the amount of contribution by depression contributes to this symptom.[75] One possible explanation of this side effect of SSRIs and SNRIs is that they decrease the resting-state functional connectivity of the dorsal medial prefrontal cortex.[75]
As many as one-third of patients experiencing emotional blunting do not report it as a side effect to their physician.[79]
Vision
Acute narrow-angle glaucoma is the most common and important ocular side effect of SSRIs, and often goes misdiagnosed.[80][81]
Cardiac
SSRIs do not appear to affect the risk of coronary heart disease (CHD) in those without a previous diagnosis of CHD.[82] A large cohort study suggested no substantial increase in the risk of cardiac malformations attributable to SSRI usage during the first trimester of pregnancy.[83] A number of large studies of people without known pre-existing heart disease have reported no EKG changes related to SSRI use.[84] The recommended maximum daily dose of citalopram and escitalopram was reduced due to concerns with QT prolongation.[85][86][87] In overdose, fluoxetine has been reported to cause sinus tachycardia, myocardial infarction, junctional rhythms, and trigeminy. Some authors have suggested electrocardiographic monitoring in patients with severe pre-existing cardiovascular disease who are taking SSRIs.[88]
In a 2023 study, a possible connection between SSRI usage and the onset of mitral valve regurgitation was identified, indicating that SSRIs could hasten the progression of degenerative mitral valve regurgitation (DMR), especially in individuals carrying 5-HTTLPR genotype. The study's authors suggest that genotyping should be performed on people with DMR to evaluate serotonin transporter (SERT) activity. They also urge practitioners to exercise caution when prescribing SSRIs to individuals with a familial history of DMR.[89][90][91]
Bleeding
SSRIs directly increase the risk of abnormal bleeding by lowering platelet serotonin levels, which are essential to platelet-driven hemostasis.[92] SSRIs interact with anticoagulants, like warfarin, and antiplatelet drugs, like aspirin.[93][94][95][96] This includes an increased risk of GI bleeding, and post operative bleeding.[93] The relative risk of intracranial bleeding is increased, but the absolute risk is very low.[97] SSRIs are known to cause platelet dysfunction.[98][99] This risk is greater in those who are also on anticoagulants, antiplatelet agents and NSAIDs (nonsteroidal anti-inflammatory drugs), as well as with the co-existence of underlying diseases such as cirrhosis of the liver or liver failure.[95][100]
Fracture risk
Evidence from longitudinal, cross-sectional, and prospective cohort studies suggests an association between SSRI usage at therapeutic doses and a decrease in bone mineral density, as well as increased fracture risk,[101][102][103][104] a relationship that appears to persist even with adjuvant bisphosphonate therapy.[105] However, because the relationship between SSRIs and fractures is based on observational data as opposed to prospective trials, the phenomenon is not definitively causal.[106] There also appears to be an increase in fracture-inducing falls with SSRI use, suggesting the need for increased attention to fall risk in elderly patients using the medication.[106] The loss of bone density does not appear to occur in younger patients taking SSRIs.[107]
Bruxism
SSRI and SNRI antidepressants may cause jaw pain/jaw spasm reversible syndrome (although it is not common). Buspirone appears to be successful in treating bruxism on SSRI/SNRI induced jaw clenching.[108][109][110]
Serotonin syndrome
Serotonin syndrome is typically caused by the use of two or more serotonergic drugs, including SSRIs.[111] Serotonin syndrome is a condition that can range from mild (most common) to deadly. Mild symptoms may consist of increased heart rate, fever, shivering, sweating, dilated pupils, myoclonus (intermittent jerking or twitching), as well as hyperreflexia.[112] Concomitant use of SSRIs or SNRIs for depression with a triptan for migraine does not appear to heighten the risk of the serotonin syndrome.[113] Taking monoamine oxidase inhibitors (MAOIs) in combination with SSRIs can be fatal, since MAOIs disrupt monoamine oxidase, an enzyme which is needed to break down serotonin and other neurotransmitters. Without monoamine oxidase, the body is unable to eliminate excess neurotransmitters, allowing them to build up to dangerous levels. The prognosis for recovery in a hospital setting is generally good if serotonin syndrome is correctly identified. Treatment consists of discontinuing any serotonergic drugs and providing supportive care to manage agitation and hyperthermia, usually with benzodiazepines.[114]
Suicide risk
Children and adolescents
Meta-analyses of short-duration randomized clinical trials have found that SSRI use is related to a higher risk of suicidal behavior in children and adolescents.[115][116][117] For instance, a 2004 U.S. Food and Drug Administration (FDA) analysis of clinical trials on children with major depressive disorder found statistically significant increases of the risks of "possible suicidal ideation and suicidal behavior" by about 80%, and of agitation and hostility by about 130%.[118] According to the FDA, the heightened risk of suicidality is within the first one to two months of treatment.[119][120][121] The National Institute for Health and Care Excellence (NICE) places the excess risk in the "early stages of treatment".[122] The European Psychiatric Association places the excess risk in the first two weeks of treatment and, based on a combination of epidemiological, prospective cohort, medical claims, and randomized clinical trial data, concludes that a protective effect dominates after this early period. A 2014 Cochrane review found that at six to nine months, suicidal ideation remained higher in children treated with antidepressants compared to those treated with psychological therapy.[121]
In 2004, the Medicines and Healthcare products Regulatory Agency (MHRA) in the United Kingdom judged fluoxetine (Prozac) to be the only antidepressant that offered a favorable risk-benefit ratio in children with depression, though it was also associated with a slight increase in the risk of self-harm and suicidal ideation.[123] Only two SSRIs are licensed for use with children in the UK, sertraline (Zoloft) and fluvoxamine (Luvox), for the treatment of obsessive–compulsive disorder. Fluoxetine is not licensed for this use.[124]
A 2007 comparison of aggression and hostility occurring during treatment with fluoxetine to placebo in children and adolescents found that no significant difference between the fluoxetine group and the placebo group.[125] There is also evidence that higher rates of SSRI prescriptions are associated with lower rates of suicide in children, though since the evidence is correlational, the true nature of the relationship is unclear.[126] A 2021 Swedish study, using a within-individual design, also found that young people (as well as adults) who have both attempted suicide and been prescribed SSRIs most commonly make the attempt before, rather than after, starting their SSRI prescription.[127]
Adults
It is unclear whether SSRIs affect the risk of suicidal behavior in adults.
- A 2005 meta-analysis of drug company data found no evidence that SSRIs increased the risk of suicide; however, important protective or hazardous effects could not be excluded.[128]
- A 2005 review observed that suicide attempts are increased in those who use SSRIs as compared to placebo and compared to therapeutic interventions other than tricyclic antidepressants. No difference risk of suicide attempts was detected between SSRIs versus tricyclic antidepressants.[129]
- A 2006 review suggests that the widespread use of antidepressants in the new "SSRI-era" appears to have led to a highly significant decline in suicide rates in most countries with traditionally high baseline suicide rates. The decline is particularly striking for women who, compared with men, seek more help for depression. Recent clinical data on large samples in the US, too, have revealed a protective effect of antidepressants against suicide.[130]
- A 2006 meta-analysis of randomized controlled trials suggests that SSRIs increase suicide ideation compared with placebo. However, the observational studies suggest that SSRIs did not increase suicide risk more than older antidepressants. The researchers stated that if SSRIs increase suicide risk in some patients, the number of additional deaths is very small because ecological studies have generally found that suicide mortality has declined (or at least not increased) as SSRI use has increased.[131]
- An additional meta-analysis by the FDA in 2006 found an age-related effect of SSRIs. Among adults younger than 25 years, results indicated that there was a higher risk for suicidal behavior. For adults between 25 and 64, the effect appears neutral on suicidal behavior, but possibly protective for suicidal behavior for adults between the ages of 25 and 64. For adults older than 64, SSRIs seem to reduce the risk of suicidal behavior.[115]
- In 2016, a review criticized the effects of the FDA Black Box suicide warning inclusion in the prescription. The authors discussed that the suicide rates might also increase as a consequence of the warning.[132] A 2019 review makes a similar claim, noting that instead of increasing the use of psychotherapy (as the FDA had hoped), the warning has increased the use of benzodiazepines.[133]
- A 2021 study on Swedish youth and adults between 2006 and 2013 (n = 538,577) finds that the highest frequency of suicides occurs at 30 days before, rather than after, the beginning of SSRI prescription. This indicates that SSRIs do not increase the risk of suicide and may reduce the risk.[127]
Risk of death
A 2017 meta-analysis found that antidepressants, including SSRIs, were associated with significantly increased risk of death (+33%) and new cardiovascular complications (+14%) in the general population.[134] Conversely, risks were not greater in people with existing cardiovascular disease.[134]
Pregnancy and breastfeeding
SSRI use in pregnancy has been associated with a variety of risks with varying degrees of proof of causation. As depression is independently associated with negative pregnancy outcomes, determining the extent to which observed associations between antidepressant use and specific adverse outcomes reflect a causative relationship has been difficult in some cases.[135] In other cases, the attribution of adverse outcomes to antidepressant exposure seems fairly clear.
SSRI use in pregnancy is associated with an increased risk of spontaneous abortion of about 1.7-fold.[136][137] Use is also associated with preterm birth.[138] According to some researches, decreased body weight of the child, intrauterine growth retardation, neonatal adaptive syndrome, and persistent pulmonary hypertension also was noted.[139]
A systematic review of the risk of major birth defects in antidepressant-exposed pregnancies found a small increase (3% to 24%) in the risk of major malformations and a risk of cardiovascular birth defects that did not differ from non-exposed pregnancies.[140] [141] Other studies have found an increased risk of cardiovascular birth defects among depressed mothers not undergoing SSRI treatment, suggesting the possibility of ascertainment bias, e.g. that worried mothers may pursue more aggressive testing of their infants.[142] Another study found no increase in cardiovascular birth defects and a 27% increased risk of major malformations in SSRI-exposed pregnancies.[137]
The FDA stated on July 19, 2006, that nursing mothers on SSRIs must discuss treatment with their physicians. However, the medical literature on the safety of SSRIs has determined that some SSRIs, like Sertraline and Paroxetine, are considered safe for breastfeeding.[143][144][145]
Neonatal abstinence syndrome
Several studies have documented neonatal abstinence syndrome, a syndrome of neurological, gastrointestinal, autonomic, endocrine, and/or respiratory symptoms among a large minority of infants with intrauterine exposure. These syndromes are short-lived, but insufficient long-term data are available to determine whether there are long-term effects.[146][147]
Persistent pulmonary hypertension
Persistent pulmonary hypertension (PPHN) is a serious and life-threatening, but very rare, lung condition that occurs soon after the birth of the newborn. Newborn babies with PPHN have high pressure in their lung blood vessels and are not able to get enough oxygen into their bloodstream. About 1 to 2 babies per 1000 babies born in the U.S. develop PPHN shortly after birth, and often they need intensive medical care. It is associated with about a 25% risk of significant long-term neurological deficits.[148] A 2014 meta analysis found no increased risk of persistent pulmonary hypertension associated with exposure to SSRI's in early pregnancy and a slight increase in risk associates with exposure late in pregnancy; "an estimated 286 to 351 women would need to be treated with an SSRI in late pregnancy to result in an average of one additional case of persistent pulmonary hypertension of the newborn".[149] A review published in 2012 reached conclusions very similar to those of the 2014 study.[150]
Neuropsychiatric effects in offspring
According to a 2015 review available data found that "some signal exists suggesting that antenatal exposure to SSRIs may increase the risk of ASDs (autism spectrum disorders)"[151] even though a large cohort study published in 2013[152] and a cohort study using data from Finland's national register between 1996 and 2010 and published in 2016 found no significant association between SSRI use and autism in offspring.[153] The 2016 Finland study also found no association with ADHD, but did find an association with increased rates of depression diagnoses in early adolescence.[153]
Bipolar switch
In adults and children with bipolar disorder, SSRIs may cause a bipolar switch from depression into hypomania/mania, mixed states, or rapid cycling.[154] When taken with mood stabilizers, the risk of switching is not increased; however, when taking SSRIs as a monotherapy, the risk of switching may be twice or three times that of the average.[155][156] The changes are not often easy to detect and require monitoring by family and mental health professionals.[157] This switch might happen even with no prior (hypo)manic episodes and might therefore not be foreseen by the psychiatrist.
SSRIs are less likely to cause switching compared to older tricyclic antidepressants.[155]
Interactions
The following drugs may precipitate serotonin syndrome in people on SSRIs:[158][159]
- Linezolid
- Monoamine oxidase inhibitors (MAOIs) including moclobemide, phenelzine, tranylcypromine, selegiline and methylene blue
- Lithium
- Sibutramine
- MDMA (ecstasy)
- Dextromethorphan
- Tramadol
- 5-HTP
- Pethidine/meperidine
- St. John's wort
- Yohimbe
- Tricyclic antidepressants (TCAs)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs)
- Buspirone
- Triptan
- Mirtazapine
- Methylene blue
Painkillers of the NSAIDs drug family may interfere and reduce efficiency of SSRIs and may compound the increased risk of gastrointestinal bleeds caused by SSRI use.[94][96][160] NSAIDs include:
There are several potential pharmacokinetic interactions between the various individual SSRIs and other medications. Most of these arise from the fact that every SSRI can inhibit certain P450 cytochrome enzymes.[161][162][163][164]
| Drug name | CYP1A2 | CYP2C9 | CYP2C19 | CYP2D6 | CYP3A4 | CYP2B6 |
|---|---|---|---|---|---|---|
| Citalopram | + | 0 | 0 | + | 0 | 0 |
| Escitalopram | 0 | 0 | 0 | + | 0 | 0 |
| Fluoxetine | + | ++ | +/++ | +++ | + | + |
| Fluvoxamine | +++ | ++ | +++ | + | + | + |
| Paroxetine | + | + | + | +++ | + | +++ |
| Sertraline | + | + | +/++ | + | + | + |
Legend:
0 – no inhibition
+ – mild/weak inhibition
++ – moderate inhibition
+++ – strong/potent inhibition
The CYP2D6 enzyme is entirely responsible for the metabolism of hydrocodone, codeine[165] and dihydrocodeine to their active metabolites (hydromorphone, morphine, and dihydromorphine, respectively), which in turn undergo phase 2 glucuronidation. These opioids (and to a lesser extent oxycodone, tramadol, and methadone) have interaction potential with selective serotonin reuptake inhibitors.[166][167] The concomitant use of some SSRIs (paroxetine and fluoxetine) with codeine may decrease the plasma concentration of active metabolite morphine, which may result in reduced analgesic efficacy.[168][169]
Another important interaction of certain SSRIs involves paroxetine, a potent inhibitor of CYP2D6, and tamoxifen, an agent commonly used in the treatment and prevention of breast cancer. Tamoxifen is a prodrug that is metabolised by the hepatic cytochrome P450 enzyme system, especially CYP2D6, to its active metabolites. Concomitant use of paroxetine and tamoxifen in women with breast cancer is associated with a higher risk of death, as much as a 91 percent increase in women who used it the longest.[170]
Overdose
SSRIs appear safer in overdose when compared with traditional antidepressants, such as the tricyclic antidepressants. This relative safety is supported by both case series and studies of deaths per number of prescriptions.[171] However, case reports of SSRI poisoning have indicated that severe toxicity can occur[172] and deaths have been reported following massive single ingestions,[173] although this is exceedingly uncommon when compared to the tricyclic antidepressants.[171]
Because of the wide therapeutic index of the SSRIs, most patients will have mild or no symptoms following moderate overdoses. The most commonly reported severe effect following SSRI overdose is serotonin syndrome; serotonin toxicity is usually associated with very high overdoses or multiple drug ingestion.[174] Other reported significant effects include coma, seizures, and cardiac toxicity.[171]
Poisoning is also known in animals, and some toxicity information is available for veterinary treatment.[175]
Discontinuation syndrome
Abrupt discontinuation of SSRIs, especially after prolonged therapy, causes a withdrawal syndrome, which may include symptoms such as nausea and vomiting, headache, dizziness, chills, body aches, paresthesias, insomnia, and brain zaps.[176] Serotonin reuptake inhibitors should not be abruptly discontinued after extended therapy, and whenever possible, should be tapered over several weeks to minimize discontinuation-related symptoms. SSRI-associated withdrawal symptoms are not typically referred to as a dependence syndrome. However, commentators have noted that such symptoms meet the definition of a physical and psychological dependence syndrome.[177]
Paroxetine may produce discontinuation-related symptoms at a greater rate than other SSRIs, though qualitatively similar effects have been reported for all SSRIs.[178][179] Discontinuation effects appear to be less for fluoxetine, perhaps owing to its long half-life and the natural tapering effect associated with its slow clearance from the body. One strategy for minimizing SSRI discontinuation symptoms is to switch the patient to fluoxetine and then taper and discontinue the fluoxetine.[178]
Mechanism of action
Serotonin reuptake inhibition
All SSRIs block the reuptake of serotonin through the serotonin transporter (SERT). This occurs in various anatomical sites, including the presynaptic terminals of serotonergic neurons in the central and peripheral nervous systems, enteric neurons and epithelial cells in the gastrointestinal tract, the pulmonary endothelium, and platelets.[180][181]
In the central nervous system, the majority of released serotonin is taken up by SERT. When this process is blocked, it stays in the synaptic gap longer than it normally would, and may repeatedly stimulate the receptors of the postsynaptic cell. In the short run, this leads to an increase in signaling across synapses in which serotonin serves as the primary neurotransmitter. On chronic dosing, the increased occupancy of post-synaptic serotonin receptors signals the pre-synaptic neuron to synthesize and release less serotonin. Serotonin levels within the synapse drop, then rise again, ultimately leading to downregulation of post-synaptic serotonin receptors.[182] Other, indirect effects may include increased norepinephrine output, increased neuronal cyclic AMP levels, and increased levels of regulatory factors such as BDNF and CREB.[183] Owing to the lack of a widely accepted comprehensive theory of the biology of mood disorders, there is no widely accepted theory of how these changes lead to the mood-elevating and anti-anxiety effects of SSRIs.
There has to be this consideration that also antidepressants should work as central nervous "stimulants" (with this terminus being a right description rudimentary, yet "stimulating" meant in another way as psychostimulants in not providing or sustaining focus or attention due to increased monoamine-availability in the synaptic cleft but an increased released serotonin for controlling ones longterm emotional conditioned state), in where due to their potent affinity[184] which is depicting how strong the tendency of a molecule is speaking about binding to their prefferable receptor-bindingsite (in antidepressants mostly speaking about the targeted serotonin- and noradrenalintransporters[185]) which is in general rule considered remarkabely higher than in statistics for their respective "high-making" relatives (like methylphenidate[186]), to occupy and inactivate receptortransporters such efficiantly to directly activate downstream-effects most prominently the downregulation of exacerbitable postsynaptic serotonin-5HT2A-and 1A receptors[187] as direct effect to this chances as a longterm regulation (then outcalled as therapeutic adwished effect due to its promised mood-elevating habituation).[188]
Sigma receptor ligands
| Medication | SERT | σ1 | σ2 | σ1 / SERT | |
|---|---|---|---|---|---|
| Citalopram | 1.16 | 292–404 | Agonist | 5,410 | 252–348 |
| Escitalopram | 2.5 | 288 | Agonist | ND | ND |
| Fluoxetine | 0.81 | 191–240 | Agonist | 16,100 | 296–365 |
| Fluvoxamine | 2.2 | 17–36 | Agonist | 8,439 | 7.7–16.4 |
| Paroxetine | 0.13 | ≥1,893 | ND | 22,870 | ≥14,562 |
| Sertraline | 0.29 | 32–57 | Antagonist | 5,297 | 110–197 |
| Values are Ki (nM). The smaller the value, the more strongly the drug binds to the site. | |||||
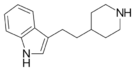
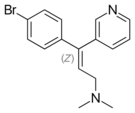
In addition to their actions as reuptake inhibitors of serotonin, some SSRIs are also, coincidentally, ligands of the sigma receptors.[189][190] Fluvoxamine is an agonist of the σ1 receptor, while sertraline is an antagonist of the σ1 receptor, and paroxetine does not significantly interact with the σ1 receptor.[189][190] None of the SSRIs have significant affinity for the σ2 receptor.[189][190] Fluvoxamine has by far the strongest activity of the SSRIs at the σ1 receptor.[189][190] High occupancy of the σ1 receptor by clinical dosages of fluvoxamine has been observed in the human brain in positron emission tomography (PET) research.[189][190] It is thought that agonism of the σ1 receptor by fluvoxamine may have beneficial effects on cognition.[189][190] In contrast to fluvoxamine, the relevance of the σ1 receptor in the actions of the other SSRIs is uncertain and questionable due to their very low affinity for the receptor relative to the SERT.[191]
Anti-inflammatory effects
The role of inflammation and the immune system in depression has been extensively studied. The evidence supporting this link has been shown in numerous studies over the past decade. Nationwide studies and meta-analyses of smaller cohort studies have uncovered a correlation between pre-existing inflammatory conditions such as type 1 diabetes, rheumatoid arthritis (RA), or hepatitis, and an increased risk of depression. Data also shows that using pro-inflammatory agents in the treatment of diseases like melanoma can lead to depression. Several meta-analytical studies have found increased levels of proinflammatory cytokines and chemokines in depressed patients.[192] This link has led scientists to investigate the effects of antidepressants on the immune system.
SSRIs were originally invented to increase levels of available serotonin in the extracellular spaces. However, the delayed response between when patients first begin SSRI treatment to when they see effects has led scientists to believe that other molecules are involved in the efficacy of these drugs.[193] To investigate the apparent anti-inflammatory effects of SSRIs, both Kohler et al. and Więdłocha et al. conducted meta-analyses which have shown that after antidepressant treatment the levels of cytokines associated with inflammation are decreased.[194][195] A large cohort study conducted by researchers in the Netherlands investigated the association between depressive disorders, symptoms, and antidepressants with inflammation. The study showed decreased levels of interleukin (IL)-6, a cytokine that has proinflammatory effects, in patients taking SSRIs compared to non-medicated patients.[196]
Treatment with SSRIs has shown reduced production of inflammatory cytokines such as IL-1β, tumor necrosis factor (TNF)-α, IL-6, and interferon (IFN)-γ, which leads to a decrease in inflammation levels and subsequently a decrease in the activation level of the immune response.[197] These inflammatory cytokines have been shown to activate microglia, which are specialized macrophages that reside in the brain. Macrophages are a subset of immune cells responsible for host defense in the innate immune system. Macrophages can release cytokines and other chemicals to cause an inflammatory response. Peripheral inflammation can induce an inflammatory response in microglia and can cause neuroinflammation. SSRIs inhibit proinflammatory cytokine production, which leads to less activation of microglia and peripheral macrophages. SSRIs not only inhibit the production of these proinflammatory cytokines, but they also have been shown to upregulate anti-inflammatory cytokines such as IL-10. Taken together, this reduces the overall inflammatory immune response.[197][198]
In addition to affecting cytokine production, there is evidence that treatment with SSRIs has effects on the proliferation and viability of immune system cells involved in both innate and adaptive immunity. Evidence shows that SSRIs can inhibit proliferation in T-cells, which are important cells for adaptive immunity, and can induce inflammation. SSRIs can also induce apoptosis, programmed cell death, in T-cells. The full mechanism of action for the anti-inflammatory effects of SSRIs is not fully known. However, there is evidence for various pathways to have a hand in the mechanism. One such possible mechanism is the increased levels of cyclic adenosine monophosphate (cAMP) as a result of interference with activation of protein kinase A (PKA), a cAMP-dependent protein. Other possible pathways include interference with calcium ion channels, or inducing cell death pathways like MAPK[199] and Notch signaling pathway.[200]
The anti-inflammatory effects of SSRIs have prompted studies of the efficacy of SSRIs in the treatment of autoimmune diseases such as multiple sclerosis, RA, inflammatory bowel diseases, and septic shock. These studies have been performed in animal models but have shown consistent immune regulatory effects. Fluoxetine, an SSRI, has also shown efficacy in animal models of graft vs. host disease.[199] SSRIs have also been used successfully as pain relievers in patients undergoing oncology treatment. The effectiveness of this has been hypothesized to be at least in part due to the anti-inflammatory effects of SSRIs.[198]
Pharmacogenetics
Large bodies of research are devoted to using genetic markers to predict whether patients will respond to SSRIs or have side effects that will cause their discontinuation, although these tests are not yet ready for widespread clinical use.[201]
Versus TCAs
There appears to be no significant difference in effectiveness between SSRIs and tricyclic antidepressants, which were the most commonly used class of antidepressants before the development of SSRIs.[202] However, SSRIs have the important advantage that their toxic dose is high, and, therefore, they are much more difficult to use as a means to commit suicide. Further, they have fewer and milder side effects. Tricyclic antidepressants also have a higher risk of serious cardiovascular side effects, which SSRIs lack.
SSRIs act on signal pathways such as cyclic adenosine monophosphate (cAMP) on the postsynaptic neuronal cell, which leads to the release of brain-derived neurotrophic factor (BDNF). BDNF enhances the growth and survival of cortical neurons and synapses.[183]
Pharmacokinetics
SSRIs vary in their pharmacokinetic properties.[163]
| SSRI | F (%) | Vd (L/kg) | logP | PPB (%) | Major metabolic enzymes (additional) | t1/2 (h) | Dose (mg) | Levels (ng/mL) |
|---|---|---|---|---|---|---|---|---|
| Citalopram | 80 | 12 | 3.76 | 80 | CYP2C19, CYP3A4 (CYP2D6) | 35 | 20–40 | 50–110 |
| Escitalopram | 80 | 12 | 3.5 | 56 | CYP3A4, CYP2C19 | 27–32 | 10–20 | 15–80 |
| Fluoxetine | 60–80 | 20–45 | 4.05 | 95 | CYP2D6, CYP2C9 (CYP2C19) | 24–96 | 20–60 | 120–500 |
| Fluvoxamine | 53 | 25 | 2.89 | 77 | CYP2D6 (CYP1A2) | 12–15 | 50–300 | 60–230 |
| Paroxetine | 50–90 | 17 | 3.6 | 95 | CYP2D6 | 21 | 20–50 | 30–120 |
| Sertraline | 80–95 | 20 | 5.1 | 98 | CYP2B6 (CYP2C19, CYP3A4, CYP2D6) | 25–26 | 50–200 | 10–150 |
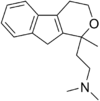
List of SSRIs
Marketed

Antidepressants
- Citalopram (Celexa)
- Escitalopram (Lexapro)
- Fluoxetine (Prozac)
- Fluvoxamine (Luvox)
- Paroxetine (Paxil)
- Sertraline (Zoloft)
Others
- Dapoxetine (Priligy)
Discontinued
Antidepressants
- Indalpine (Upstène)
- Zimelidine (Zelmid)
Never marketed
Antidepressants
- Alaproclate (GEA-654)
- Centpropazine
- Cericlamine (JO-1017)
- Femoxetine (Malexil; FG-4963)
- Ifoxetine (CGP-15210)
- Omiloxetine
- Panuramine (WY-26002)
- Pirandamine (AY-23713)
- Seproxetine ((S)-norfluoxetine)
Related drugs
Although described as SNRIs, duloxetine (Cymbalta), venlafaxine (Effexor), and desvenlafaxine (Pristiq) are in fact relatively selective as serotonin reuptake inhibitors (SRIs).[203] They are about at least 10-fold selective for inhibition of serotonin reuptake over norepinephrine reuptake.[203] The selectivity ratios are approximately 1:30 for venlafaxine, 1:10 for duloxetine, and 1:14 for desvenlafaxine.[203][204] At low doses, these SNRIs act mostly as SSRIs; only at higher doses do they also prominently inhibit norepinephrine reuptake.[205][206] Milnacipran (Ixel, Savella) and its stereoisomer levomilnacipran (Fetzima) are the only widely marketed SNRIs that inhibit serotonin and norepinephrine to similar degrees, both with ratios close to 1:1.[203][207]
Vilazodone (Viibryd) and vortioxetine (Trintellix) are SRIs that also act as modulators of serotonin receptors and are described as serotonin modulators and stimulators (SMS).[208] Vilazodone is a 5-HT1A receptor partial agonist while vortioxetine is a 5-HT1A receptor agonist and 5-HT3 and 5-HT7 receptor antagonist.[208] Litoxetine (SL 81–0385) and lubazodone (YM-992, YM-35995) are similar drugs that were never marketed.[209][210][211][212] They are SRIs and litoxetine is also a 5-HT3 receptor antagonist[209][210] while lubazodone is also a 5-HT2A receptor antagonist.[211][212]
History
Zimelidine was introduced in 1982 and was the first SSRI to be sold. Despite its efficacy, a statistically significant increase in cases of Guillain–Barré syndrome among treated patients led to its withdrawal in 1983. Fluoxetine, introduced in 1987, is commonly thought to be the first SSRI to be marketed.
Controversy
Fifty years after the introduction of fluoxetine and other SSRIs, these drugs remain widely used and often effective for depression, though their effectiveness, mechanisms of action, prescription patterns, and role in the medicalization of normal life remain debated.[7]
In other organisms
Fluoxetine was investigated as a potential environmental contaminant, but found to have 'limited accumulation' in comparison to other pharmaceutically active compounds.[213]
Veterinary use
An SSRI (fluoxetine) has been approved for veterinary use in treatment of canine separation anxiety.[214] Like in human medicine, fluoxetine is extensively used off-label in animal medicine. In dogs and cats, it is mainly prescribed off-label for behavior problems.[215]
See also
- List of antidepressants
- Noradrenergic and specific serotonergic antidepressant
- Serotonin releasing agent (SRA)
- Serotonin–norepinephrine reuptake inhibitor (SNRI)
- Serotonin–norepinephrine–dopamine reuptake inhibitor (SNDRI)
- Dapoxetine
References
- ↑ "7: Mood Disorders and Suicide". Abnormal Psychology: An Integrative Approach (Fifth ed.). Belmont, California: Wadsworth Cengage Learning. 2009. p. 239. ISBN 978-0-495-09556-9. OCLC 192055408.
- ↑ "Selective Serotonin Reuptake Inhibitors". Antidepressants: Past, Present and Future. Berlin: Springer. 2004. pp. 241–262. ISBN 978-3-540-43054-4. https://books.google.com/books?id=sO_hArhCxwMC&pg=PA241.
- ↑ 3.0 3.1 3.2 "Recommendations | Depression in adults: treatment and management | Guidance | NICE". 2022-06-29. https://www.nice.org.uk/guidance/ng222/chapter/recommendations.
- ↑ 4.0 4.1 Hengartner, Michael P.; Plöderl, Martin (2022-04-01). "Estimates of the minimal important difference to evaluate the clinical significance of antidepressants in the acute treatment of moderate-to-severe depression" (in en). BMJ Evidence-Based Medicine 27 (2): 69–73. doi:10.1136/bmjebm-2020-111600. ISSN 2515-446X. PMID 33593736.
- ↑ 5.0 5.1 Stone, Marc B.; Yaseen, Zimri S.; Miller, Brian J.; Richardville, Kyle; Kalaria, Shamir N.; Kirsch, Irving (2022-08-02). "Response to acute monotherapy for major depressive disorder in randomized, placebo controlled trials submitted to the US Food and Drug Administration: individual participant data analysis". BMJ (Clinical Research Ed.) 378. doi:10.1136/bmj-2021-067606. ISSN 1756-1833. PMID 35918097.
- ↑ 6.0 6.1 Moncrieff, Joanna; Cooper, Ruth E.; Stockmann, Tom; Amendola, Simone; Hengartner, Michael P.; Horowitz, Mark A. (2022-07-20). "The serotonin theory of depression: a systematic umbrella review of the evidence" (in en). Molecular Psychiatry 28 (8): 3243–3256. doi:10.1038/s41380-022-01661-0. ISSN 1476-5578. PMID 35854107.
- ↑ 7.0 7.1 Lancet, The (2025-05-10). "50 years of SSRIs: weighing benefits and harms" (in English). The Lancet 405 (10490): 1641. doi:10.1016/S0140-6736(25)00981-X. ISSN 0140-6736. PMID 40348448. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(25)00981-X/fulltext.
- ↑ "Understanding and treating depersonalisation disorder". Advances in Psychiatric Treatment 11 (2): 92–100. 2005. doi:10.1192/apt.11.2.92.
- ↑ "Comparative efficacy and acceptability of 21 antidepressant drugs for the acute treatment of adults with major depressive disorder: a systematic review and network meta-analysis". Lancet 391 (10128): 1357–1366. April 2018. doi:10.1016/S0140-6736(17)32802-7. PMID 29477251.
- ↑ Yuan, Ziqi; Chen, Zhenlei; Xue, Maoqiang; Zhang, Jie; Leng, Lige (2020). "Application of antidepressants in depression: A systematic review and meta-analysis". Journal of Clinical Neuroscience 80: 169–181. doi:10.1016/j.jocn.2020.08.013. ISSN 1532-2653. PMID 33099342.
- ↑ "Empirically derived criteria cast doubt on the clinical significance of antidepressant-placebo differences". Contemp Clin Trials 43: 60–2. July 2015. doi:10.1016/j.cct.2015.05.005. PMID 25979317. "The commonly used method of estimating the 'response' to drug treatment in clinical trials of antidepressants (arbitrarily set at a 50% reduction in symptoms), involves the categorisation of continuous data from symptom scales, and therefore does not provide an independent arbiter of clinical significance. Moreover, this method can exaggerate small differences between interventions such as antidepressants and placebo [28], and statisticians note that it can distort data and should be avoided [29], [30]. Response rates in double-blind antidepressant trials are typically about 50% in the drug groups and 35% in the placebo groups (e.g., [31], [32]). This 15% difference is often defended as clinically significant because 15% of depressed people who get better on antidepressants would not have gotten better on a placebo. However, a 50% reduction in symptoms is close to the mean and median of drug improvement rates in placebo-controlled antidepressant trials [31], [32], [33] and thus near the apex of the distribution curve. Thus, with an SD of 8 in change scores, a 15% difference in response rates is about (an odds ratio of 1.86, a relative risk of 0.77, and an NNT of 7) is exactly what one would expect from a mean 3-point difference in HAM-D scores [28]. Lack of response does not mean that the patient has not improved; it means that the improvement has been less, by as little as one point, than the arbitrary criterion chosen for defining a therapeutic response.".
- ↑ "Methodological Flaws, Conflicts of Interest, and Scientific Fallacies: Implications for the Evaluation of Antidepressants' Efficacy and Harm". Front Psychiatry 8. 2017. doi:10.3389/fpsyt.2017.00275. PMID 29270136. "Another common flaw is to report efficacy based on drug-placebo differences in response and remission rates (27). To come at binary constructs such as response and remission, continuous symptom rating scales are dichotomized along arbitrary cut-offs. However, methodologists have vigorously advised against the use of dichotomization (28–30) because it produces, among others, systematically inflated effect sizes (31–33).".
- ↑ "Depression in children and young people: identification and management". The National Institute for Health and Care Excellence (NICE). June 2019. http://www.nice.org.uk/guidance/ng134.
- ↑ Chu, Andrew; Wadhwa, Roopma (2023), "Selective Serotonin Reuptake Inhibitors", StatPearls (Treasure Island (FL): StatPearls Publishing), PMID 32119293, http://www.ncbi.nlm.nih.gov/books/NBK554406/, retrieved 2025-10-02
- ↑ Dwyer, Jennifer B.; Bloch, Michael H. (2019). "Antidepressants for Pediatric Patients". Current Psychiatry 18 (9): 26–42F. ISSN 1537-8276. PMID 31511767.
- ↑ Boaden, Katharine; Tomlinson, Anneka; Cortese, Samuele; Cipriani, Andrea (2020-09-02). "Antidepressants in Children and Adolescents: Meta-Review of Efficacy, Tolerability and Suicidality in Acute Treatment" (in English). Frontiers in Psychiatry 11. doi:10.3389/fpsyt.2020.00717. ISSN 1664-0640. PMID 32982805.
- ↑ "New generation antidepressants for depression in children and adolescents: a network meta-analysis". The Cochrane Database of Systematic Reviews 2021 (5). May 2021. doi:10.1002/14651858.CD013674.pub2. PMID 34029378.
- ↑ Williams, Taryn; Hattingh, Coenraad J.; Kariuki, Catherine M.; Tromp, Sean A.; van Balkom, Anton J.; Ipser, Jonathan C.; Stein, Dan J. (2017-10-19). "Pharmacotherapy for social anxiety disorder (SAnD)". The Cochrane Database of Systematic Reviews 10 (10). doi:10.1002/14651858.CD001206.pub3. ISSN 1469-493X. PMID 29048739.
- ↑ 19.0 19.1 "VA.gov | Veterans Affairs" (in en). https://www.ptsd.va.gov/professional/treat/txessentials/clinician_guide_meds.asp?utm_source=chatgpt.com.
- ↑ Williams, Taryn; Phillips, Nicole J.; Stein, Dan J.; Ipser, Jonathan C. (2022-03-02). "Pharmacotherapy for post traumatic stress disorder (PTSD)". The Cochrane Database of Systematic Reviews 2022 (3). doi:10.1002/14651858.CD002795.pub3. ISSN 1469-493X. PMID 35234292.
- ↑ "Update information | Generalised anxiety disorder and panic disorder in adults: management | Guidance | NICE". 2011-01-26. https://www.nice.org.uk/guidance/cg113/chapter/Update-information?utm_source=chatgpt.com.
- ↑ Kopcalic, Katarina; Arcaro, Justin; Pinto, Antonio; Ali, Shehzad; Barbui, Corrado; Curatoli, Chiara; Martin, Janet; Guaiana, Giuseppe (2025-01-30). "Antidepressants versus placebo for generalised anxiety disorder (GAD)". The Cochrane Database of Systematic Reviews 1 (1). doi:10.1002/14651858.CD012942.pub2. ISSN 1469-493X. PMID 39880377.
- ↑ "Canadian clinical practice guidelines for the management of anxiety, posttraumatic stress and obsessive-compulsive disorders". BMC Psychiatry 14 (Suppl 1): S1. 2014-07-02. doi:10.1186/1471-244X-14-S1-S1. PMID 25081580.
- ↑ "Overview | Obsessive-compulsive disorder and body dysmorphic disorder: treatment | Guidance | NICE". 2005-11-29. https://www.nice.org.uk/guidance/cg31.
- ↑ "2019 surveillance of obsessive-compulsive disorder and body dysmorphic disorder: treatment (NICE guideline CG31)". 2019. https://www.nice.org.uk/guidance/cg31/resources/2019-surveillance-of-obsessivecompulsive-disorder-and-body-dysmorphic-disorder-treatment-nice-guideline-cg31-pdf-8701091079109?utm_.
- ↑ Steele, Dale W.; Caputo, Eduardo L.; Kanaan, Ghid; Zahradnik, Michael L.; Brannon, Elizabeth; Freeman, Jennifer B.; Balk, Ethan M.; Trikalinos, Thomas A. et al. (2024-12-06). Diagnosis and Management of Obsessive Compulsive Disorders in Children: A Systematic Review (Report). Agency for Healthcare Research and Quality (AHRQ). doi:10.23970/ahrqepccer276. https://effectivehealthcare.ahrq.gov/products/obsessive-compulsive-disorder/research.
- ↑ "Panic disorder" (in en). 2021-02-16. https://www.nhs.uk/mental-health/conditions/panic-disorder/.
- ↑ "Panic Disorder: What You Need to Know - National Institute of Mental Health (NIMH)" (in en). https://www.nimh.nih.gov/health/publications/panic-disorder-when-fear-overwhelms.
- ↑ "Antidepressants versus placebo for panic disorder in adults". The Cochrane Database of Systematic Reviews 2018 (4). April 2018. doi:10.1002/14651858.CD010676.pub2. PMID 29620793.
- ↑ 30.0 30.1 30.2 "Eating disorders in over 8s: management". The National Institute for Health and Care Excellence (NICE). January 2004. http://www.nice.org.uk/nicemedia/pdf/CG9FullGuideline.pdf.
- ↑ 31.0 31.1 "Practice guideline for the treatment of patients with eating disorders". U.S. Department of Health and Human Services. http://www.guidelines.gov/content.aspx?id=9318+.
- ↑ "Evidence-based pharmacotherapy of eating disorders". The International Journal of Neuropsychopharmacology 15 (2): 189–207. March 2012. doi:10.1017/S1461145711000381. PMID 21414249.
- ↑ Legg, Lynn A.; Rudberg, Ann-Sofie; Hua, Xing; Wu, Simiao; Hackett, Maree L.; Tilney, Russel; Lindgren, Linnea; Kutlubaev, Mansur A. et al. (2021-11-15). "Selective serotonin reuptake inhibitors (SSRIs) for stroke recovery". The Cochrane Database of Systematic Reviews 2021 (11). doi:10.1002/14651858.CD009286.pub4. ISSN 1469-493X. PMID 34780067.
- ↑ "Premature ejaculation: state of the art". The Urologic Clinics of North America 34 (4): 591–599, vii–viii. November 2007. doi:10.1016/j.ucl.2007.08.011. PMID 17983899.
- ↑ "The Timing of Antidepressant Effects: A Comparison of Diverse Pharmacological and Somatic Treatments". Pharmaceuticals 3 (1): 19–41. January 2010. doi:10.3390/ph3010019. PMID 27713241.
- ↑ "Antidepressant-associated sexual dysfunction: impact, effects, and treatment". Drug, Healthcare and Patient Safety 2: 141–150. September 2010. doi:10.2147/DHPS.S7634. PMID 21701626.
- ↑ "Is Sertraline a Good Pharmacological Strategy to Control Anger? Results of a Systematic Review". Behavioral Sciences 9 (5): 57. May 2019. doi:10.3390/bs9050057. PMID 31126061.
- ↑ "Treatment of Raynaud's phenomenon with the selective serotonin reuptake inhibitor fluoxetine". Rheumatology 50 (9): 1038–1043. Sep 2001. doi:10.1093/rheumatology/40.9.1038. PMID 11561116.
- ↑ "The Mechanism of Drug-induced Akathsia". CNS Spectrums. 2011. PMID 21406165.
- ↑ "SSRI-induced extrapyramidal side-effects and akathisia: implications for treatment". Journal of Psychopharmacology 12 (2): 192–214. 1998. doi:10.1177/026988119801200212. PMID 9694033.
- ↑ "Selective serotonin reuptake inhibitor-induced akathisia". Journal of the American Pharmacists Association 49 (2): e28–36; quiz e37–38. 2009. doi:10.1331/JAPhA.2009.08083. PMID 19289334.
- ↑ "Movement disorders associated with the serotonin selective reuptake inhibitors". The Journal of Clinical Psychiatry 57 (10): 449–454. 1996. doi:10.4088/jcp.v57n1002. PMID 8909330.
- ↑ "Persistence of Sexual Dysfunction Side Effects after Discontinuation of Antidepressant Medications: Emerging Evidence". The Open Psychology Journal 1: 42–50. 2008. doi:10.2174/1874350100801010042. https://benthamopen.com/ABSTRACT/TOPSYJ-1-42. Retrieved 2021-04-15.
- ↑ "Strategies for managing sexual dysfunction induced by antidepressant medication". The Cochrane Database of Systematic Reviews 2013 (5). May 2013. doi:10.1002/14651858.CD003382.pub3. PMID 23728643.
- ↑ "Sexual dysfunction, depression, and the impact of antidepressants". Journal of Clinical Psychopharmacology 29 (2): 157–164. April 2009. doi:10.1097/jcp.0b013e31819c76e9. PMID 19512977.
- ↑ "Psychotropic medications and their effects on sexual function: diagnosis, biology, and treatment approaches". The Journal of Clinical Psychiatry 55 (9): 406–413. September 1994. PMID 7929021.
- ↑ "SSRI-Associated Sexual Dysfunction". The American Journal of Psychiatry 163 (9): 1504–1509; quiz 1664. 2006. doi:10.1176/appi.ajp.163.9.1504. PMID 16946173.
- ↑ "Buspirone". StatPearls. 17 January 2023. PMID 30285372. https://www.ncbi.nlm.nih.gov/books/NBK531477/. Retrieved 4 August 2024.
- ↑ "Erectile and Ejaculatory Dysfunction Associated with Use of Psychotropic Drugs: A Systematic Review". The Journal of Sexual Medicine 18 (8): 1354–1363. August 2021. doi:10.1016/j.jsxm.2021.05.016. PMID 34247952. "Buspirone, a non-benzodiazepine anxiolytic, have even demonstrated enhancement of sexual function in certain individuals. For this reason, they have been proposed as augmentation agents (antidotes) or substitution agents in patients with emerging sexual dysfunction after treatment with antidepressants.".
- ↑ "Management Strategies for Antidepressant-Related Sexual Dysfunction: A Clinical Approach". Journal of Clinical Medicine 8 (10): 1640. October 2019. doi:10.3390/jcm8101640. PMID 31591339.
- ↑ "Treatment-emergent sexual dysfunction related to antidepressants: a meta-analysis". Journal of Clinical Psychopharmacology 29 (3): 259–266. June 2009. doi:10.1097/JCP.0b013e3181a5233f. PMID 19440080.
- ↑ "Antidepressant-Associated Sexual Dysfunction: A Potentially Avoidable Therapeutic Challenge". Primary Psychiatry 10 (1): 55–61. 2003. http://www.primarypsychiatry.com/aspx/articledetail.aspx?articleid=1362. Retrieved 2013-02-19.
- ↑ "Sexual side effects of SSRI medications: potential treatment strategies for SSRI-induced female sexual dysfunction". Current Women's Health Reports 2 (6): 409–416. December 2002. PMID 12429073.
- ↑ "The effect of SSRIs on Semen quality: A systematic review and meta-analysis". Frontiers in Pharmacology 13. 2022. doi:10.3389/fphar.2022.911489. PMID 36188547.
- ↑ "Deleterious effects of selective serotonin reuptake inhibitor treatment on semen parameters in patients with lifelong premature ejaculation". International Journal of Impotence Research 24 (5): 171–173. September 2012. doi:10.1038/ijir.2012.12. PMID 22573230.
- ↑ "Unintended Consequences: A Review of Pharmacologically-Induced Priapism". Sexual Medicine Reviews 7 (2): 283–292. April 2019. doi:10.1016/j.sxmr.2018.09.002. PMID 30503727.
- ↑ "Off-label Uses of Selective Serotonin Reuptake Inhibitors (SSRIs)". Curr Neuropharmacol 20 (4): 693–712. 2022. doi:10.2174/1570159X19666210517150418. PMID 33998993.
- ↑ 58.0 58.1 58.2 58.3 58.4 58.5 58.6 58.7 58.8 "Selective serotonin reuptake inhibitors, post-treatment sexual dysfunction and persistent genital arousal disorder: A systematic review". Pharmacoepidemiol Drug Saf 32 (10): 1053–1067. June 2023. doi:10.1002/pds.5653. PMID 37294623. https://onlinelibrary.wiley.com/doi/10.1002/pds.5653. Retrieved 2023-08-15.
- ↑ 59.0 59.1 59.2 "Diagnostic criteria for enduring sexual dysfunction after treatment with antidepressants, finasteride and isotretinoin". The International Journal of Risk & Safety in Medicine 33 (1): 65–76. 1 January 2022. doi:10.3233/JRS-210023. PMID 34719438.
- ↑ 60.0 60.1 "Persistent sexual dysfunction after SSRI withdrawal: a scoping review and presentation of 86 cases from the Netherlands". Expert Opinion on Drug Safety 21 (4): 553–561. April 2022. doi:10.1080/14740338.2022.2007883. PMID 34791958.
- ↑ "A clinical review of antidepressants, their sexual side-effects, post-SSRI sexual dysfunction, and serotonin syndrome". Br J Nurs 32 (14): 678–682. July 2023. doi:10.12968/bjon.2023.32.14.678. PMID 37495413. https://e-space.mmu.ac.uk/632844/13/BJON%20Final%20Proof%20%28Copyright%20Safe%29.pdf. Retrieved 2024-03-22.
- ↑ 62.0 62.1 "Post-SSRI Sexual Dysfunction: A Literature Review". Sexual Medicine Reviews 6 (1): 29–34. January 2018. doi:10.1016/j.sxmr.2017.07.002. PMID 28778697. "There is still no definitive treatment for PSSD. Low-power laser irradiation and phototherapy have shown some promising results.".
- ↑ "Premature Ejaculation Associated with Citalopram Withdrawal". Annals of Pharmacotherapy 37 (12): 1804–1806. 2003. doi:10.1345/aph.1D214. PMID 14632589.
- ↑ 64.0 64.1 64.2 64.3 "Post-SSRI Sexual Dysfunction (PSSD): Biological Plausibility, Symptoms, Diagnosis, and Presumed Risk Factors". Sex Med Rev 10 (1): 91–98. January 2022. doi:10.1016/j.sxmr.2021.07.001. PMID 34627736.
- ↑ "Post-finasteride syndrome and post-SSRI sexual dysfunction: two sides of the same coin?". Endocrine 61 (2): 180–193. August 2018. doi:10.1007/s12020-018-1593-5. PMID 29675596.
- ↑ "Mechanisms and treatments of SSRI-induced sexual dysfunction". Perspect Psychiatr. Care 38 (3): 111–116. 2002. doi:10.1111/j.1744-6163.2002.tb00665.x. PMID 12385082.
- ↑ "Dopamine-dependent" side effects of selective serotonin reuptake inhibitors: a clinical review". J Clin Psychiatry 65 (8): 1064–1068. 2004. doi:10.4088/jcp.v65n0806. PMID 15323590.
- ↑ "Fluoxetine-induced changes in tactile sensation and sexual functioning among clinically depressed women". J Sex Marital Ther 31 (2): 113–128. 2005. doi:10.1080/00926230590477961. PMID 15859371.
- ↑ "Major depressive disorder, antidepressants, and sexual dysfunction". J Clin Psychiatry 67: 33–37. 2006. PMID 16848675.
- ↑ "Antidepressant-induced sexual dysfunction". Med J Aust 212 (7): 329–334. April 2020. doi:10.5694/mja2.50522. PMID 32172535.
- ↑ Pirani, Yassie; Delgado-Ron, J. Andrés; Marinho, Pedro; Gupta, Amit; Grey, Emily; Watt, Sarah; MacKinnon, Kinnon R.; Salway, Travis (2024-09-20). "Frequency of self-reported persistent post-treatment genital hypoesthesia among past antidepressant users: a cross-sectional survey of sexual and gender minority youth in Canada and the US" (in en). Social Psychiatry and Psychiatric Epidemiology 60 (7): 1771–1779. doi:10.1007/s00127-024-02769-0. ISSN 1433-9285. PMID 39302425. https://link.springer.com/article/10.1007/s00127-024-02769-0.
- ↑ PRAC recommendations on signals: Adopted at the 13-16 May 2019 PRAC meeting. European Medicines Agency. 11 June 2019. p. 5. https://www.ema.europa.eu/en/documents/prac-recommendation/prac-recommendations-signals-adopted-13-16-may-2019-prac-meeting_en.pdf. Retrieved 19 July 2023.
- ↑ "SSRIs, SNRIs: risk of persistent sexual dysfunction". Reactions Weekly (Springer) 1838 (5): 5. 16 January 2021. doi:10.1007/s40278-021-89324-7.
- ↑ "Emotional Blunting, Cognitive Impairment, Bone Fractures, and Bleeding as Possible Side Effects of Long-Term Use of SSRIs". Clin Neuropsychiatry 16 (2): 75–85. April 2019. PMID 34908941.
- ↑ 75.0 75.1 75.2 75.3 75.4 75.5 "Emotional Blunting in Patients With Major Depressive Disorder: A Brief Non-systematic Review of Current Research". Front Psychiatry 12. 2021. doi:10.3389/fpsyt.2021.792960. PMID 34970173.
- ↑ "Antidepressants: misnamed and misrepresented". World Psychiatry 14 (3): 302–303. October 2015. doi:10.1002/wps.20243. PMID 26407780.
- ↑ "Efficacy of agomelatine and escitalopram on depression, subjective sleep and emotional experiences in patients with major depressive disorder: a 24-wk randomized, controlled, double-blind trial". Int J Neuropsychopharmacol 16 (10): 2219–2234. November 2013. doi:10.1017/S1461145713000679. PMID 23823799.
- ↑ "Effectiveness of Vortioxetine on Emotional Blunting in Patients with Major Depressive Disorder with inadequate response to SSRI/SNRI treatment". J Affect Disord 283: 472–479. March 2021. doi:10.1016/j.jad.2020.11.106. PMID 33516560.
- ↑ Kikuchi, T; Iga, JI; Oosawa, M; Hoshino, T; Moriguchi, Y; Izutsu, M (June 2024). "A web-based survey on the occurrence of emotional blunting in patients with major depressive disorder in Japan: Patient perceptions and attitudes.". Neuropsychopharmacology Reports 44 (2): 321–332. doi:10.1002/npr2.12417. PMID 38616339.
- ↑ "Selective serotonin reuptake inhibitors: a review of its effects on intraocular pressure". Current Neuropharmacology 6 (4): 293–310. December 2008. doi:10.2174/157015908787386104. PMID 19587851.
- ↑ "SSRI-associated optic neuropathy". Eye 29 (9): 1233–1235. September 2015. doi:10.1038/eye.2015.119. PMID 26139049.
- ↑ "Antidepressant Use and Risk of Coronary Heart Disease: Meta-Analysis of Observational Studies". British Journal of Clinical Pharmacology 78 (4): 727–737. Mar 20, 2014. doi:10.1111/bcp.12383. PMID 24646010.
- ↑ "Antidepressant Use in Pregnancy and the Risk of Cardiac Defects". New England Journal of Medicine 370 (25): 2397–2407. 2014. doi:10.1056/NEJMoa1312828. PMID 24941178.
- ↑ "Selective serotonin reuptake inhibitors: infrequent medical adverse effects". Archives of Family Medicine 7 (1): 78–84. 1998. doi:10.1001/archfami.7.1.78. PMID 9443704.
- ↑ FDA (December 2018). "FDA Drug Safety". FDA. https://www.fda.gov/Drugs/DrugSafety/ucm269086.htm. Retrieved 2019-12-16.
- ↑ Citalopram and escitalopram: QT interval prolongation – new maximum daily dose restrictions (including in elderly patients), contraindications, and warnings . From Medicines and Healthcare products Regulatory Agency. Article date: December 2011
- ↑ "Clinical and ECG Effects of Escitalopram Overdose". http://m.utoledo.edu/med/gme/em/pdfs/ECG_escitalopram.pdf.
- ↑ "Speculations on difference between tricyclic and selective serotonin reuptake inhibitor antidepressants on their cardiac effects. Is there any?". Current Medicinal Chemistry 6 (6): 469–480. Jun 1999. doi:10.2174/0929867306666220330184544. PMID 10213794.
- ↑ "Deciphering the Connection of Serotonin to Degenerative Mitral Valve Regurgitation - Advances in Cardiology and Heart Surgery" (in en). https://www.nyp.org/advances-cardiology/deciphering-the-connection-of-serotonin-to-degenerative-mitral-valve-regurgitation.
- ↑ Castillero, Estibaliz; Fitzpatrick, Emmett; Keeney, Samuel J.; D'Angelo, Alex M.; Pressly, Benjamin B.; Simpson, Michael T.; Kurade, Mangesh; Erwin, W. Clinton et al. (2023-01-04). "Decreased serotonin transporter activity in the mitral valve contributes to progression of degenerative mitral regurgitation" (in en). Science Translational Medicine 15 (677). doi:10.1126/scitranslmed.adc9606. ISSN 1946-6234. PMID 36599005.
- ↑ "Serotonin can potentially accelerate degenerative mitral regurgitation, study says" (in en). 2023-01-29. https://www.news-medical.net/news/20230129/Serotonin-can-potentially-accelerate-degenerative-mitral-regurgitation-study-says.aspx.
- ↑ "Serotonin Reuptake Inhibitors and Risk of Abnormal Bleeding". The Psychiatric Clinics of North America 39 (3): 413–426. September 2016. doi:10.1016/j.psc.2016.04.010. PMID 27514297.
- ↑ 93.0 93.1 "Selective serotonin re-uptake inhibitors and the risk of bleeding". Expert Opinion on Drug Safety 4 (2): 337–344. March 2005. doi:10.1517/14740338.4.2.337. PMID 15794724.
- ↑ 94.0 94.1 The Maudsley prescribing guidelines in psychiatry. West Sussex: Wiley-Blackwell. 2012. ISBN 978-0-470-97969-3.
- ↑ 95.0 95.1 "Serotonin reuptake inhibitor antidepressants and abnormal bleeding: a review for clinicians and a reconsideration of mechanisms". The Journal of Clinical Psychiatry 71 (12): 1565–1575. December 2010. doi:10.4088/JCP.09r05786blu. PMID 21190637.
- ↑ 96.0 96.1 "Risk of upper gastrointestinal tract bleeding associated with selective serotonin reuptake inhibitors and venlafaxine therapy: interaction with nonsteroidal anti-inflammatory drugs and effect of acid-suppressing agents". Archives of General Psychiatry 65 (7): 795–803. July 2008. doi:10.1001/archpsyc.65.7.795. PMID 18606952.
- ↑ "Selective serotonin reuptake inhibitors and brain hemorrhage: a meta-analysis". Neurology 79 (18): 1862–1865. October 2012. doi:10.1212/WNL.0b013e318271f848. PMID 23077009.
- ↑ "Selective serotonin reuptake inhibitors and increased bleeding risk: are we missing something?". The American Journal of Medicine 119 (2): 113–116. February 2006. doi:10.1016/j.amjmed.2005.03.044. PMID 16443409.
- ↑ "Influence of antidepressants on hemostasis". Dialogues in Clinical Neuroscience 9 (1): 47–59. 2007. doi:10.31887/DCNS.2007.9.1/dhalperin. PMID 17506225.
- ↑ "Effects of selective serotonin reuptake inhibitors on platelet function: mechanisms, clinical outcomes and implications for use in elderly patients". Drugs & Aging 28 (5): 345–367. May 2011. doi:10.2165/11589340-000000000-00000. PMID 21542658.
- ↑ "Use of selective serotonin reuptake inhibitors and risk of fracture: a systematic review and meta-analysis". Journal of Bone and Mineral Research 27 (5): 1186–1195. May 2012. doi:10.1002/jbmr.1554. PMID 22258738.
- ↑ "Osteoporosis in patients taking selective serotonin reuptake inhibitors: a focus on fracture outcome". Endocrine 48 (1): 65–68. February 2015. doi:10.1007/s12020-014-0357-0. PMID 25091520. https://zenodo.org/record/845248. Retrieved 2019-07-01.
- ↑ "Drugs that may harm bone: Mitigating the risk". Cleveland Clinic Journal of Medicine 83 (4): 281–288. April 2016. doi:10.3949/ccjm.83a.15066. PMID 27055202.
- ↑ "Effects of Depression and Serotonergic Antidepressants on Bone: Mechanisms and Implications for the Treatment of Depression". Drugs & Aging 33 (1): 21–25. January 2016. doi:10.1007/s40266-015-0323-4. PMID 26547857.
- ↑ "Risk of fracture and the concomitant use of bisphosphonates with osteoporosis-inducing medications". The Annals of Pharmacotherapy 49 (4): 437–447. April 2015. doi:10.1177/1060028015569594. PMID 25667198.
- ↑ 106.0 106.1 "Do Selective Serotonin Reuptake Inhibitors (SSRIs) Cause Fractures?". Current Osteoporosis Reports 14 (5): 211–218. October 2016. doi:10.1007/s11914-016-0322-3. PMID 27495351.
- ↑ "Changes in volumetric BMD of radius and tibia upon antidepressant drug administration in young depressive patients". Journal of Musculoskeletal & Neuronal Interactions 12 (4): 224–229. December 2012. PMID 23196265.
- ↑ "SSRI-associated bruxism: A systematic review of published case reports". Neurology. Clinical Practice 8 (2): 135–141. April 2018. doi:10.1212/CPJ.0000000000000433. PMID 29708207.
- ↑ "Use of buspirone in selective serotonin reuptake inhibitor-induced sleep bruxism". European Psychiatry. Abstract of the 25th European Congress of Psychiatry 41: S855. 2017-04-01. doi:10.1016/j.eurpsy.2017.01.1701. ISSN 0924-9338. http://www.sciencedirect.com/science/article/pii/S0924933817317169. Retrieved 2020-04-18.
- ↑ "Duloxetine-induced nocturnal bruxism resolved by buspirone: case report". Clinical Neuropharmacology 34 (4): 137–138. 2011. doi:10.1097/WNF.0b013e3182227736. PMID 21768799.
- ↑ "Serotonin syndrome". The Ochsner Journal 13 (4): 533–540. 2013. PMID 24358002.
- ↑ "The serotonin syndrome". The New England Journal of Medicine 352 (11): 1112–1120. March 2005. doi:10.1056/nejmra041867. PMID 15784664.
- ↑ "Association of Coprescription of Triptan Antimigraine Drugs and Selective Serotonin Reuptake Inhibitor or Selective Norepinephrine Reuptake Inhibitor Antidepressants With Serotonin Syndrome". JAMA Neurology 75 (5): 566–572. May 2018. doi:10.1001/jamaneurol.2017.5144. PMID 29482205.
- ↑ (in en) Ferri's Clinical Advisor 2017: 5 Books in 1. Elsevier Health Sciences. 2016. pp. 1154–1155. ISBN 978-0-323-44838-3. https://books.google.com/books?id=rRhCDAAAQBAJ&pg=PA1154. Retrieved 2021-01-26.
- ↑ 115.0 115.1 "Clinical review: relationship between antidepressant drugs and suicidal behavior in adults". FDA. 2006-11-17. pp. 11–74. https://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdf.
- ↑ "Statistical Evaluation of Suicidality in Adults Treated with Antidepressants". FDA. 2006-11-17. pp. 75–140. https://www.fda.gov/ohrms/dockets/ac/06/briefing/2006-4272b1-01-FDA.pdf.
- ↑ "Antidepressant drug therapy and suicide in severely depressed children and adults: A case-control study". Archives of General Psychiatry 63 (8): 865–872. August 2006. doi:10.1001/archpsyc.63.8.865. PMID 16894062.
- ↑ "Review and evaluation of clinical data. Relationship between psychiatric drugs and pediatric suicidal behavior". FDA. 2004-08-16. pp. 42, 115. https://www.fda.gov/OHRMS/DOCKETS/ac/04/briefing/2004-4065b1-10-TAB08-Hammads-Review.pdf.
- ↑ "Antidepressant Use in Children, Adolescents, and Adults". U.S. Food and Drug Administration. https://www.fda.gov/drugs/drugsafety/informationbydrugclass/ucm096273.
- ↑ "FDA Medication Guide for Antidepressants". https://www.fda.gov/downloads/Drugs/DrugSafety/ucm088660.pdf%E2%80%8E.
- ↑ 121.0 121.1 "Psychological therapies versus antidepressant medication, alone and in combination for depression in children and adolescents". The Cochrane Database of Systematic Reviews 2014 (11). November 2014. doi:10.1002/14651858.CD008324.pub3. PMID 25433518.
- ↑ "Overview | Depression in adults: recognition and management | Guidance | NICE". 28 October 2009. https://www.nice.org.uk/guidance/CG90.
- ↑ "Report of the CSM expert working group on the safety of selective serotonin reuptake inhibitor antidepressants". MHRA. 2004-12-01. http://www.mhra.gov.uk/home/groups/pl-p/documents/drugsafetymessage/con019472.pdf.
- ↑ "Selective Serotonin Reuptake Inhibitors (SSRIs): Overview of regulatory status and CSM advice relating to major depressive disorder (MDD) in children and adolescents including a summary of available safety and efficacy data". MHRA. 2005-09-29. http://www.mhra.gov.uk/Safetyinformation/Safetywarningsalertsandrecalls/Safetywarningsandmessagesformedicines/CON019494.
- ↑ "Meta-analysis of aggression and/or hostility-related events in children and adolescents treated with fluoxetine compared with placebo". Journal of Child and Adolescent Psychopharmacology 17 (5): 713–718. October 2007. doi:10.1089/cap.2006.0138. PMID 17979590.
- ↑ "The relationship between antidepressant prescription rates and rate of early adolescent suicide". The American Journal of Psychiatry 163 (11): 1898–1904. November 2006. doi:10.1176/appi.ajp.163.11.1898. PMID 17074941.
- ↑ 127.0 127.1 Lagerberg, Tyra; Fazel, Seena; Sjölander, Arvid; Hellner, Clara; Lichtenstein, Paul; Chang, Zheng (March 2022). "Selective serotonin reuptake inhibitors and suicidal behaviour: a population-based cohort study". Neuropsychopharmacology 47 (4): 817–823. doi:10.1038/s41386-021-01179-z. PMID 34561608.
- ↑ "Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review". BMJ 330 (7488): 385. February 2005. doi:10.1136/bmj.330.7488.385. PMID 15718537.
- ↑ "Association between suicide attempts and selective serotonin reuptake inhibitors: systematic review of randomised controlled trials". BMJ 330 (7488): 396. February 2005. doi:10.1136/bmj.330.7488.396. PMID 15718539.
- ↑ "Do antidepressants t(h)reat(en) depressives? Toward a clinically judicious formulation of the antidepressant-suicidality FDA advisory in light of declining national suicide statistics from many countries". Journal of Affective Disorders 94 (1–3): 3–13. August 2006. doi:10.1016/j.jad.2006.04.003. PMID 16712945.
- ↑ "How have the selective serotonin reuptake inhibitor antidepressants affected suicide mortality?". The Australian and New Zealand Journal of Psychiatry 40 (11–12): 941–950. 2006. doi:10.1111/j.1440-1614.2006.01917.x. PMID 17054562.
- ↑ "Ten years after the FDA black box warning for antidepressant drugs: A critical narrative review". Archives of Clinical Psychiatry 43 (3): 60–66. 2016. doi:10.1590/0101-60830000000086.
- ↑ Fornaro, Michele; Anastasia, Annalisa; Valchera, Alessandro; Carano, Alessandro; Orsolini, Laura; Vellante, Federica; Rapini, Gabriella; Olivieri, Luigi et al. (2019-05-03). "The FDA "Black Box" Warning on Antidepressant Suicide Risk in Young Adults: More Harm Than Benefits?". Frontiers in Psychiatry 10. doi:10.3389/fpsyt.2019.00294. PMID 31130881.
- ↑ 134.0 134.1 "The Mortality and Myocardial Effects of Antidepressants Are Moderated by Preexisting Cardiovascular Disease: A Meta-Analysis". Psychother Psychosom 86 (5): 268–282. 2017. doi:10.1159/000477940. PMID 28903117.
- ↑ "Prenatal exposure to selective serotonin reuptake inhibitors and infant outcome". Therapeutic Drug Monitoring 34 (6): 607–614. December 2012. doi:10.1097/FTD.0b013e31826d07ea. PMID 23042258.
- ↑ "Pregnancy outcomes following exposure to serotonin reuptake inhibitors: a meta-analysis of clinical trials". Reproductive Toxicology 22 (4): 571–575. 2006. doi:10.1016/j.reprotox.2006.03.019. PMID 16720091. Bibcode: 2006RepTx..22..571R.
- ↑ 137.0 137.1 "Increasing the risk of spontaneous abortion and major malformations in newborns following use of serotonin reuptake inhibitors during pregnancy: A systematic review and updated meta-analysis". DARU Journal of Pharmaceutical Sciences 20 (1). 2012. doi:10.1186/2008-2231-20-75. PMID 23351929.
- ↑ "Selective serotonin reuptake inhibitor (SSRI) use during pregnancy and risk of preterm birth: a systematic review and meta-analysis". BJOG 123 (12): 1900–1907. November 2016. doi:10.1111/1471-0528.14144. PMID 27239775.
- ↑ "Risks of using SSRI / SNRI antidepressants during pregnancy and lactation". Interdisciplinary Toxicology 10 (1): 30–34. September 2017. doi:10.1515/intox-2017-0004. PMID 30123033.
- ↑ "Do findings differ across research design? The case of antidepressant use in pregnancy and malformations". Journal of Population Therapeutics and Clinical Pharmacology 19 (2): e334–348. 2012. PMID 22946124.
- ↑ "The fetal safety of fluoxetine: a systematic review and meta-analysis". Journal of Obstetrics and Gynaecology Canada 35 (4): 362–369. April 2013. doi:10.1016/S1701-2163(15)30965-8. PMID 23660045.
- ↑ "Selective serotonin reuptake inhibitors and malformations: case closed?". Seminars in Fetal & Neonatal Medicine 18 (1): 19–22. February 2013. doi:10.1016/j.siny.2012.10.004. PMID 23228547.
- ↑ "Breastfeeding Update: SDCBC's quarterly newsletter". Breastfeeding.org. http://www.breastfeeding.org/newsletter/v2i4/page2.html.
- ↑ "Using Antidepressants in Breastfeeding Mothers". kellymom.com. http://www.kellymom.com/health/meds/antidepressants-hale10-02.html.
- ↑ "SSRIs during breastfeeding: spotlight on milk-to-plasma ratio". Archives of Women's Mental Health 10 (2): 39–51. 2007. doi:10.1007/s00737-007-0173-0. PMID 17294355.
- ↑ "Paediatric outcomes following intrauterine exposure to serotonin reuptake inhibitors: a systematic review". Danish Medical Bulletin 58 (9): A4303. September 2011. PMID 21893008.
- ↑ "The use of psychotropic medication during pregnancy: how about the newborn?". Neuropsychiatric Disease and Treatment 9: 1257–1266. 2013. doi:10.2147/NDT.S36394. PMID 24039427.
- ↑ Persistent Newborn Pulmonary Hypertension at eMedicine
- ↑ "Prenatal exposure to antidepressants and persistent pulmonary hypertension of the newborn: systematic review and meta-analysis". BMJ 348. 2014. doi:10.1136/bmj.f6932. PMID 24429387.
- ↑ "Antidepressant use in pregnancy and persistent pulmonary hypertension of the newborn (PPHN): a systematic review". Reproductive Toxicology 34 (3): 293–297. November 2012. doi:10.1016/j.reprotox.2012.04.015. PMID 22564982. Bibcode: 2012RepTx..34..293T.
- ↑ "Prenatal antidepressant exposure and the risk of autism spectrum disorders in children. Are we looking at the fall of Gods?". Journal of Affective Disorders 182: 132–137. August 2015. doi:10.1016/j.jad.2015.04.048. PMID 25985383.
- ↑ "Use of selective serotonin reuptake inhibitors during pregnancy and risk of autism". The New England Journal of Medicine 369 (25): 2406–2415. December 2013. doi:10.1056/NEJMoa1301449. PMID 24350950.
- ↑ 153.0 153.1 "Gestational Exposure to Selective Serotonin Reuptake Inhibitors and Offspring Psychiatric Disorders: A National Register-Based Study". Journal of the American Academy of Child and Adolescent Psychiatry 55 (5): 359–366. May 2016. doi:10.1016/j.jaac.2016.02.013. PMID 27126849.
- ↑ Chris Aiken: Antidepressants in Bipolar II Disorder, May 14, 2019. In: psychiatrictimes.com
- ↑ 155.0 155.1 "Antidepressants in bipolar depression: an enduring controversy". International Journal of Bipolar Disorders 6 (1). December 2018. doi:10.1186/s40345-018-0133-9. PMID 30506151.
- ↑ "The risk of switch to mania in patients with bipolar disorder during treatment with an antidepressant alone and in combination with a mood stabilizer". The American Journal of Psychiatry 171 (10): 1067–1073. October 2014. doi:10.1176/appi.ajp.2014.13111501. PMID 24935197. https://figshare.com/articles/journal_contribution/27292893.
- ↑ "Complications of SSRI treatment". Journal of Child and Adolescent Psychopharmacology 11 (1): 1–4. 2001. doi:10.1089/104454601750143320. PMID 11322738.
- ↑ "Serotonin syndrome and other serotonergic disorders". Pain Medicine 4 (1): 63–74. March 2003. doi:10.1046/j.1526-4637.2003.03005.x. PMID 12873279.
- ↑ "The serotonin syndrome". The New England Journal of Medicine 352 (11): 1112–1120. March 2005. doi:10.1056/NEJMra041867. PMID 15784664.
- ↑ "Antidepressant effects of selective serotonin reuptake inhibitors (SSRIs) are attenuated by antiinflammatory drugs in mice and humans". Proceedings of the National Academy of Sciences of the United States of America 108 (22): 9262–9267. May 2011. doi:10.1073/pnas.1104836108. PMID 21518864.
- ↑ Goodman and Gilman's The Pharmacological Basis of Therapeutics (12th ed.). McGraw Hill Professional. 2010. ISBN 978-0-07-162442-8.
- ↑ Pharmacotherapy of Depression (2nd ed.). Springer. 2011. p. 49. doi:10.1007/978-1-60327-435-7. ISBN 978-1-60327-435-7. https://archive.org/details/pharmacotherapyd00cira.
- ↑ 163.0 163.1 163.2 "Pharmacokinetic considerations for current state-of-the-art antidepressants". Expert Opin Drug Metab Toxicol 15 (10): 831–847. October 2019. doi:10.1080/17425255.2019.1669560. PMID 31526279. https://ruj.uj.edu.pl/xmlui/handle/item/256191.
- ↑ "Dose-dependent inhibition of CYP1A2, CYP2C19 and CYP2D6 by citalopram, fluoxetine, fluvoxamine and paroxetine". European Journal of Clinical Pharmacology 51 (1): 73–78. 1996. doi:10.1007/s002280050163. PMID 8880055.
- ↑ "Opioid pharmacokinetic drug-drug interactions". The American Journal of Managed Care 17 (Suppl 11): S276–287. September 2011. PMID 21999760. https://www.ajmc.com/pubMed.php?pii=51946.
- ↑ "Paroxetine hydrochloride – Drug Summary". Physicians' Desk Reference, LLC. https://www.pdr.net/drug-summary/Paxil-paroxetine-hydrochloride-215.2678.
- ↑ "Opioid metabolism". Mayo Clinic Proceedings 84 (7): 613–624. July 2009. doi:10.4065/84.7.613. PMID 19567715.
- ↑ "Immunisation and pregnancy – who, what, when and why?". Australian Prescriber 40 (4): 122–124. August 2017. doi:10.18773/austprescr.2017.046. PMID 28947846.
- ↑ "New FDA black box warning for codeine: how will this affect dentists?". Anesthesia Progress 60 (2): 35–36. 2013. doi:10.2344/0003-3006-60.2.35. PMID 23763556.
- ↑ "Selective serotonin reuptake inhibitors and breast cancer mortality in women receiving tamoxifen: a population-based cohort study". BMJ 340: c693. February 2010. doi:10.1136/bmj.c693. PMID 20142325.
- ↑ 171.0 171.1 171.2 "Relative toxicity of selective serotonin reuptake inhibitors (SSRIs) in overdose". Journal of Toxicology. Clinical Toxicology 42 (3): 277–285. 2004. doi:10.1081/CLT-120037428. PMID 15362595.
- ↑ "Acute fluoxetine overdose: a report of 234 cases". The American Journal of Emergency Medicine 10 (2): 115–120. 1992. doi:10.1016/0735-6757(92)90041-U. PMID 1586402.
- ↑ "Fatal overdose with citalopram". Lancet 348 (9023): 339–340. 1996. doi:10.1016/S0140-6736(05)64513-8. PMID 8709713.
- ↑ "The serotonin syndrome. Implicated drugs, pathophysiology and management". Drug Safety 13 (2): 94–104. August 1995. doi:10.2165/00002018-199513020-00004. PMID 7576268.
- ↑ (in English) Veterinary Toxicology: Basic and Clinical Principles (2 ed.). Boston: Academic Press. 2012. pp. xii + 1438. ISBN 978-0-12-385926-6.
- ↑ Tamam, Lut; Ozpoyraz, Nurgul (2002-01-01). "Selective serotonin reuptake inhibitor discontinuation syndrome: A review" (in en). Advances in Therapy 19 (1): 17–26. doi:10.1007/BF02850015. ISSN 1865-8652. PMID 12008858. https://link.springer.com/article/10.1007/BF02850015.
- ↑ Nielsen, Margrethe; Hansen, Ebba Holme; Gøtzsche, Peter C. (2012). "What is the difference between dependence and withdrawal reactions? A comparison of benzodiazepines and selective serotonin re-uptake inhibitors" (in en). Addiction 107 (5): 900–908. doi:10.1111/j.1360-0443.2011.03686.x. ISSN 1360-0443. PMID 21992148. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1360-0443.2011.03686.x.
- ↑ 178.0 178.1 Practice Guideline for the Treatment of Patients With Major Depressive Disorder (third ed.). American Psychiatric Association. October 2010. ISBN 978-0-89042-338-7. https://psychiatryonline.org/pb/assets/raw/sitewide/practice_guidelines/guidelines/mdd.pdf. Retrieved 2018-07-22.
- ↑ "Selective serotonin reuptake inhibitor antidepressant treatment discontinuation syndrome: a review of the clinical evidence and the possible mechanisms involved". Frontiers in Pharmacology 4: 45. 2013. doi:10.3389/fphar.2013.00045. PMID 23596418.
- ↑ Beecher, Kate; Belmer, Arnauld; Bartlett, Selena E. (2019-01-01), Pilowsky, Paul M, ed., "Chapter 6 - Anatomy of the Serotonin Transporter", Serotonin (Boston: Academic Press): pp. 121–133, ISBN 978-0-12-800050-2, https://www.sciencedirect.com/science/article/abs/pii/B9780128000502000061, retrieved 2025-05-02
- ↑ Bertrand, Paul P.; Bertrand, Rebecca L. (2010-02-16). "Serotonin release and uptake in the gastrointestinal tract". Autonomic Neuroscience. Visceral Afferents 153 (1): 47–57. doi:10.1016/j.autneu.2009.08.002. ISSN 1566-0702. PMID 19729349. https://www.sciencedirect.com/science/article/abs/pii/S1566070209004251.
- ↑ Goodman and Gilman's pharmacological basis of therapeutics. New York: McGraw-Hill. 2001. pp. 459–461. ISBN 978-0-07-162442-8.
- ↑ 183.0 183.1 Kolb, Bryan and Wishaw Ian. An Introduction to Brain and Behavior. New York: Worth Publishers 2006, Print.
- ↑ "Affinity, efficacy and potency". Physics, Pharmacology and Physiology for Anaesthetists. Cambridge University Press. 2014. pp. 160–163. doi:10.1017/CBO9781107326200.066. ISBN 978-1-107-32620-0. https://www.cambridge.org/core/books/abs/physics-pharmacology-and-physiology-for-anaesthetists/affinity-efficacy-and-potency/69301BD1B8583E6905DE4B150AF21C22.
- ↑ "Beyond drug-drug interactions: Effects of transporter inhibition on endobiotics, nutrients and toxins". Expert Opinion on Drug Metabolism & Toxicology 13 (10): 1075–1087. 2017. doi:10.1080/17425255.2017.1372425. PMID 28847160.
- ↑ "Affinities of methylphenidate derivatives for dopamine, norepinephrine and serotonin transporters". Life Sciences 58 (12): 231–239. 1996. doi:10.1016/0024-3205(96)00052-5. PMID 8786705.
- ↑ "Antidepressant Treatment Reduces Serotonin-1A Autoreceptor Binding in Major Depressive Disorder". Biological Psychiatry 74 (1): 26–31. 2013. doi:10.1016/j.biopsych.2012.11.012. PMID 23374637.
- ↑ "Neuroprotective Effects of Antidepressants via Upregulation of Neurotrophic Factors in the MPTP Model of Parkinson's Disease". Molecular Neurobiology 55 (1): 554–566. January 2018. doi:10.1007/s12035-016-0342-0. PMID 27975170.
- ↑ 189.0 189.1 189.2 189.3 189.4 189.5 189.6 "Cognition and depression: the effects of fluvoxamine, a sigma-1 receptor agonist, reconsidered". Human Psychopharmacology 25 (3): 193–200. April 2010. doi:10.1002/hup.1106. PMID 20373470.
- ↑ 190.0 190.1 190.2 190.3 190.4 190.5 190.6 "Sigma-1 Receptor Agonists and Their Clinical Implications in Neuropsychiatric Disorders". Sigma Receptors: Their Role in Disease and as Therapeutic Targets. Advances in Experimental Medicine and Biology. 964. 2017. pp. 153–161. doi:10.1007/978-3-319-50174-1_11. ISBN 978-3-319-50172-7.
- ↑ "The opposite effects of fluvoxamine and sertraline in the treatment of psychotic major depression: a case report". Annals of General Psychiatry 9. May 2010. doi:10.1186/1744-859X-9-23. PMID 20492642.
- ↑ "Separation of ascorbic acid and 2-keto-L-gulonic acid". Current Neuropharmacology 61 (8): 1333–1334. August 1972. doi:10.2174/1570159X14666151208113700. PMID 27640518.
- ↑ "The serotonergic system in the neurobiology of depression: Relevance for novel antidepressants". Journal of Psychopharmacology 30 (1): 13–22. January 2016. doi:10.1177/0269881115609072. PMID 26464458.
- ↑ "Peripheral Alterations in Cytokine and Chemokine Levels After Antidepressant Drug Treatment for Major Depressive Disorder: Systematic Review and Meta-Analysis". Molecular Neurobiology 55 (5): 4195–4206. May 2018. doi:10.1007/s12035-017-0632-1. PMID 28612257. https://kclpure.kcl.ac.uk/portal/en/publications/peripheral-alterations-in-cytokine-and-chemokine-levels-after-antidepressant-drug-treatment-for-major-depressive-disorder(7fb3d49a-30e3-4cfd-9a1c-df003daf8dad).html. Retrieved 2018-09-17.
- ↑ "Effect of antidepressant treatment on peripheral inflammation markers – A meta-analysis". Progress in Neuro-Psychopharmacology & Biological Psychiatry 80 (Pt C): 217–226. January 2018. doi:10.1016/j.pnpbp.2017.04.026. PMID 28445690.
- ↑ "Association of depressive disorders, depression characteristics and antidepressant medication with inflammation". Translational Psychiatry 2 (2): e79. February 2012. doi:10.1038/tp.2012.8. PMID 22832816.
- ↑ 197.0 197.1 "Antidepressant therapies inhibit inflammation and microglial M1-polarization". Pharmacology & Therapeutics 163: 82–93. July 2016. doi:10.1016/j.pharmthera.2016.04.001. PMID 27101921.
- ↑ 198.0 198.1 "The role of macrophages in anti-inflammatory activity of antidepressant drugs". Immunobiology 222 (6): 823–830. June 2017. doi:10.1016/j.imbio.2016.07.001. PMID 27453459. https://ruj.uj.edu.pl/xmlui/handle/item/128345.
- ↑ 199.0 199.1 "Selective serotonin reuptake inhibitors as a novel class of immunosuppressants". International Immunopharmacology 20 (1): 148–156. May 2014. doi:10.1016/j.intimp.2014.02.030. PMID 24613205.
- ↑ "Selective serotonin reuptake inhibitors ameliorate MEGF10 myopathy". Human Molecular Genetics 28 (14): 2365–2377. July 2019. doi:10.1093/hmg/ddz064. PMID 31267131.
- ↑ "Genetic screening for SSRI drug response among those with major depression: great promise and unseen perils". Depression and Anxiety 24 (5): 350–357. 2007. doi:10.1002/da.20251. PMID 17096399.
- ↑ "Selective serotonin reuptake inhibitors versus tricyclic antidepressants: a meta-analysis of efficacy and tolerability". Journal of Affective Disorders 58 (1): 19–36. April 2000. doi:10.1016/S0165-0327(99)00092-0. PMID 10760555.
- ↑ 203.0 203.1 203.2 203.3 "Serotonin norepinephrine reuptake inhibitors: similarities and differences". Primary Psychiatry 16 (4): 25. 2009. http://primarypsychiatry.com/serotonin-norepinephrine-reuptake-inhibitors-similarities-and-differences/. Retrieved 2017-08-26.
- ↑ "Tolerability of serotonin norepinephrine reuptake inhibitor antidepressants". CNS Spectrums 13 (7 Suppl 11): 27–33. July 2008. doi:10.1017/s1092852900028297. PMID 18622372.
- ↑ Medical Pharmacology and Therapeutics E-Book. Elsevier Health Sciences. 2017. pp. 302–. ISBN 978-0-7020-7190-4. https://books.google.com/books?id=6b0tDwAAQBAJ&pg=PA302.
- ↑ Women's Mental Health, An Issue of Psychiatric Clinics – E-Book. Elsevier Health Sciences. 2010. pp. 389–. ISBN 978-1-4557-0061-5. https://books.google.com/books?id=5jpHNa19jFUC&pg=PA389. Retrieved 2017-08-26.
- ↑ "The Role of Levomilnacipran in the Management of Major Depressive Disorder: A Comprehensive Review". Current Neuropharmacology 14 (2): 191–199. 2016. doi:10.2174/1570159x14666151117122458. PMID 26572745.
- ↑ 208.0 208.1 "New-Generation, non-SSRI Antidepressants: Therapeutic Drug Monitoring and Pharmacological Interactions. Part 1: SNRIs, SMSs, SARIs". Current Medicinal Chemistry 24 (7): 772–792. 2018. doi:10.2174/0929867324666170712165042. PMID 28707591.
- ↑ 209.0 209.1 Lexicon of Psychiatry, Neurology, and the Neurosciences. Lippincott Williams & Wilkins. 2000. pp. 581–. ISBN 978-0-7817-2468-5. https://books.google.com/books?id=ea_QVG2BFy8C&pg=PA581. Retrieved 2017-08-26.
- ↑ 210.0 210.1 Progress in Drug Research. Birkhäuser. 2012. pp. 80–82. ISBN 978-3-0348-8391-7. https://books.google.com/books?id=-d8FCAAAQBAJ&pg=PA80.
- ↑ 211.0 211.1 "Serotonin reuptake inhibitors: the corner stone in treatment of depression for half a century – a medicinal chemistry survey". Current Topics in Medicinal Chemistry 6 (17): 1801–1823. 2006. doi:10.2174/156802606778249810. PMID 17017959.
- ↑ 212.0 212.1 "Selective Serotonin Reuptake Inhibitors (SSRIs) Past, Present and Future. Edited by S. Clare Standford, R.G. Landes Company". Human Psychopharmacology: Clinical and Experimental (Austin, Texas) 15 (6): 471. 1999. doi:10.1002/1099-1077(200008)15:6<471::AID-HUP211>3.0.CO;2-4. ISBN 1-57059-649-2.
- ↑ "Ranking of crop plants according to their potential to uptake and accumulate contaminants of emerging concern". Environmental Research (Elsevier BV) 170: 422–432. March 2019. doi:10.1016/j.envres.2018.12.048. PMID 30623890. Bibcode: 2019ER....170..422C.
- ↑ Fitzgerald, Kevin T.; Bronstein, Alvin C. (February 2013). "Selective serotonin reuptake inhibitor exposure". Topics in Companion Animal Medicine 28 (1): 13–17. doi:10.1053/j.tcam.2013.03.003. ISSN 1946-9837. PMID 23796482.
- ↑ Kaur, G; Voith, VL; Schmidt, PL (2016). "The use of fluoxetine by veterinarians in dogs and cats: a preliminary survey.". Veterinary Record Open 3 (1). doi:10.1136/vetreco-2015-000146. PMID 27110371.
External links
 |
 KSF
KSF