Stimulant
Topic: Chemistry
 From HandWiki - Reading time: 43 min
From HandWiki - Reading time: 43 min

Stimulants (also known as central nervous system stimulants, or psychostimulants, or colloquially as uppers) are a class of drugs that increase the activity of the brain and the spinal cord. They are used for various purposes, such as enhancing alertness, attention, motivation, cognition, mood, and physical performance. Some of the most common stimulants are caffeine, nicotine, amphetamine, methamphetamine, cocaine, and modafinil.
Stimulants work by affecting the levels of certain neurotransmitters, such as dopamine, norepinephrine, serotonin, histamine and acetylcholine, in the synapses between neurons. These neurotransmitters regulate various functions, such as arousal, reward, learning, memory, and emotion. By increasing their availability, stimulants can produce a range of effects, from mild stimulation to euphoria, depending on the dose, route of administration, and individual factors.
Stimulants have a long history of use, both for medical and non-medical purposes. They have been used to treat various conditions, such as narcolepsy, attention deficit hyperactivity disorder (ADHD), obesity, depression, and fatigue. They have also been used as recreational drugs, performance enhancers, and cognitive enhancers, by various groups of people, such as students, athletes, workers, and soldiers.
However, stimulants also have potential risks and side effects, such as addiction, tolerance, withdrawal, psychosis, anxiety, insomnia, cardiovascular problems, and neurotoxicity. The misuse and abuse of stimulants can lead to serious health and social consequences, such as overdose, dependence, crime, and violence. Therefore, the use of stimulants is regulated by laws and policies in most countries, and requires medical supervision and prescription in some cases.
Definition
A stimulant is an overarching term that covers many drugs including those that increase the activity of the central nervous system and the body,[1] drugs that are pleasurable and invigorating, or drugs that have sympathomimetic effects.[2] Sympathomimetic effects are those effects that mimic or copy the actions of the sympathetic nervous system. The sympathetic nervous system is a part of the nervous system that prepares the body for action, such as increasing the heart rate, blood pressure, and breathing rate. Stimulants can activate the same receptors as the natural chemicals released by the sympathetic nervous system and cause similar effects.[3]
Effects
Acute
Stimulants in therapeutic doses, such as those given to patients with attention deficit hyperactivity disorder (ADHD), increases ability to focus, vigor, sociability, libido and may elevate mood. However, in higher doses, stimulants may actually decrease the ability to focus, a principle of the Yerkes-Dodson Law. The Yerkes-Dodson Law is a psychological theory that describes how stress affects performance.[4] The theory says that there is an optimal level of stress that helps people perform better, but too much or too little stress can impair performance. The theory can be illustrated by an upside-down U-shaped curve, where the peak of the curve represents the optimal level of stress and performance.[4] The theory was developed by psychologists Robert Yerkes and John Dillingham Dodson in 1908, based on experiments with mice.[4] Drugs that stimulate the central nervous system, such as those used to treat ADHD, can improve the ability to focus and other aspects of mood and behavior when taken in appropriate doses. However, when taken in higher doses, these drugs can have the opposite effect and reduce the ability to focus. This is because the higher doses cause too much stress, which exceeds the optimal level and harms performance. In higher doses, stimulants may also produce euphoria, vigor, and a decreased need for sleep. Many, but not all, stimulants have ergogenic effects. The term "ergogenic" means "enhancing physical performance".[5] Ergogenic effects are those effects that improve physical performance or endurance. For example, if a drug makes run faster, lift heavier, or last longer, it is said to have ergogenic effects. Drugs such as ephedrine, pseudoephedrine, amphetamine and methylphenidate have well documented ergogenic effects, while cocaine has the opposite effect.[6] Neurocognitive enhancing effects of stimulants, specifically modafinil, amphetamine and methylphenidate have been reported in healthy adolescents by some studies,[7] and is a commonly cited reason among illicit drug users for use, particularly among college students in the context of studying.[7] Still, results of these studies is inconclusive: assessing the potential overall neurocognitive benefits of stimulants among healthy youth is challenging due to the diversity within the population, the variability in cognitive task characteristics, and the absence of replication of studies.[7] Research on the cognitive enhancement effects of modafinil in healthy non-sleep-deprived individuals has yielded mixed results, with some studies suggesting modest improvements in attention and executive functions while others show no significant benefits or even a decline in cognitive functions.[8][9][10]
In some cases, psychiatric phenomena may emerge such as stimulant psychosis, paranoia, and suicidal ideation. Acute toxicity has been reportedly associated with homicide, paranoia, aggressive behavior, motor dysfunction, and punding. The violent and aggressive behavior associated with acute stimulant toxicity may partially be driven by paranoia.[11] Most drugs classified as stimulants are sympathomimetics, that is they stimulate the sympathetic branch of the autonomic nervous system. This leads to effects such as mydriasis, increased heart rate, blood pressure, respiratory rate and body temperature.[2] When these changes become pathological, they are called arrhythmia, hypertension, and hyperthermia, and may lead to rhabdomyolysis, stroke, cardiac arrest, or seizures. However, given the complexity of the mechanisms that underlie these potentially fatal outcomes of acute stimulant toxicity, it is impossible to determine what dose may be lethal.[12]
Chronic
Assessment of the effects of stimulants is relevant given the large population currently taking stimulants. A systematic review of cardiovascular effects of prescription stimulants found no association in children, but found a correlation between prescription stimulant use and ischemic heart attacks.[13] A review over a four-year period found that there were few negative effects of stimulant treatment, but stressed the need for longer-term studies.[14] A review of a year long period of prescription stimulant use in those with ADHD found that cardiovascular side effects were limited to transient increases in blood pressure only.[15] Initiation of stimulant treatment in those with ADHD in early childhood appears to carry benefits into adulthood with regard to social and cognitive functioning, and appears to be relatively safe.[16]
Abuse of prescription stimulants (not following physician instruction) or of illicit stimulants carries many negative health risks. Abuse of cocaine, depending upon route of administration, increases risk of cardiorespiratory disease, stroke, and sepsis.[17] Some effects are dependent upon the route of administration, with intravenous use associated with the transmission of many disease such as Hepatitis C, HIV/AIDS and potential medical emergencies such as infection, thrombosis or pseudoaneurysm,[18] while inhalation may be associated with increased lower respiratory tract infection, lung cancer, and pathological restricting of lung tissue.[19] Cocaine may also increase risk for autoimmune disease[20][21][22] and damage nasal cartilage. Abuse of methamphetamine produces similar effects as well as marked degeneration of dopaminergic neurons, resulting in an increased risk for Parkinson's disease.[23][24][25][26]
Medical uses
Stimulants are widely used throughout the world as prescription medicines as well as without a prescription (either legally or illicitly) as performance-enhancing or recreational drugs. Among narcotics, stimulants produce a noticeable crash or comedown at the end of their effects. The most frequently prescribed stimulants as of 2013 were lisdexamfetamine (Vyvanse), methylphenidate (Ritalin), and amphetamine (Adderall).[27] It was estimated in 2015 that the percentage of the world population that had used cocaine during a year was 0.4%. For the category "amphetamines and prescription stimulants" (with "amphetamines" including amphetamine and methamphetamine) the value was 0.7%, and for MDMA 0.4%.[28]
Stimulants have been used in medicine for many conditions including obesity, sleep disorders, mood disorders, impulse control disorders, asthma, nasal congestion and, in case of cocaine, as local anesthetics.[29] Drugs used to treat obesity are called anorectics and generally include drugs that follow the general definition of a stimulant, but other drugs such as cannabinoid receptor antagonists also belong to this group.[30][31] Eugeroics are used in management of sleep disorders characterized by excessive daytime sleepiness, such as narcolepsy, and include stimulants such as modafinil and pitolisant.[32][33] Stimulants are used in impulse control disorders such as ADHD[34] and off-label in mood disorders such as major depressive disorder to increase energy, focus and elevate mood.[35] Stimulants such as epinephrine,[36] theophylline and salbutamol[37] orally have been used to treat asthma, but inhaled adrenergic drugs are now preferred due to less systemic side effects. Pseudoephedrine is used to relieve nasal or sinus congestion caused by the common cold, sinusitis, hay fever and other respiratory allergies; it is also used to relieve ear congestion caused by ear inflammation or infection.[38][39]
Depression
Stimulants were one of the first classes of drugs to be used in the treatment of depression, beginning after the introduction of the amphetamines in the 1930s.[40][41][42] However, they were largely abandoned for treatment of depression following the introduction of conventional antidepressants in the 1950s.[40][41] Subsequent to this, there has been a resurgence in interest in stimulants for depression in recent years.[43][44]
Stimulants produce a fast-acting and pronounced but transient and short-lived mood lift.[45][46][43][41] In relation to this, they are minimally effective in the treatment of depression when administered continuously.[45][46] In addition, tolerance to the mood-lifting effects of amphetamine has led to dose escalation and dependence.[44] Although the efficacy for depression with continuous administration is modest, it may still reach statistical significance over placebo and provide benefits similar in magnitude to those of conventional antidepressants.[47][48][49][50] The reasons for the short-term mood-improving effects of stimulants are unclear, but may relate to rapid tolerance.[45][46][41][51] Tolerance to the effects of stimulants has been studied and characterized both in animals[51][52][53][54] and humans.[55][56][57][58] Stimulant withdrawal is remarkably similar in its symptoms to those of major depressive disorder.[59][51][60][61]
Chemistry
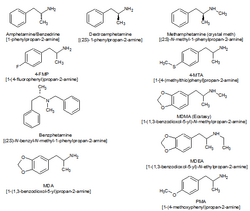
Classifying stimulants is difficult, because of the large number of classes the drugs occupy, and the fact that they may belong to multiple classes; for example, ecstasy can be classified as a substituted methylenedioxyphenethylamine, a substituted amphetamine and consequently, a substituted phenethylamine.[citation needed]
When referring to stimulants, the parent drug (e.g., amphetamine) will always be expressed in the singular[according to whom?]; with the word "substituted" placed before the parent drug (substituted amphetamines).
Major stimulant classes include phenethylamines and their daughter class substituted amphetamines.[62][63]
Amphetamines (class)
Substituted amphetamines are a class of compounds based upon the amphetamine structure;[64] it includes all derivative compounds which are formed by replacing, or substituting, one or more hydrogen atoms in the amphetamine core structure with substituents.[64][65][66] Examples of substituted amphetamines are amphetamine (itself),[64][65] methamphetamine,[64] ephedrine,[64] cathinone,[64] phentermine,[64] mephentermine,[64] bupropion,[64] methoxyphenamine,[64] selegiline,[64] amfepramone,[64] pyrovalerone,[64] MDMA (ecstasy), and DOM (STP). Many drugs in this class work primarily by activating trace amine-associated receptor 1 (TAAR1);[67] in turn, this causes reuptake inhibition and effluxion, or release, of dopamine, norepinephrine, and serotonin.[67] An additional mechanism of some substituted amphetamines is the release of vesicular stores of monoamine neurotransmitters through VMAT2, thereby increasing the concentration of these neurotransmitters in the cytosol, or intracellular fluid, of the presynaptic neuron.[68]
Amphetamines-type stimulants are often used for their therapeutic effects. Physicians sometimes prescribe amphetamine to treat major depression, where subjects do not respond well to traditional SSRI medications,[citation needed] but evidence supporting this use is poor/mixed.[44] Notably, two recent large phase III studies of lisdexamfetamine (a prodrug to amphetamine) as an adjunct to an SSRI or SNRI in the treatment of major depressive disorder showed no further benefit relative to placebo in effectiveness.[69] Numerous studies have demonstrated the effectiveness of drugs such as Adderall (a mixture of salts of amphetamine and dextroamphetamine) in controlling symptoms associated with ADHD. Due to their availability and fast-acting effects, substituted amphetamines are prime candidates for abuse.[70]
Cocaine analogues
Hundreds of cocaine analogues have been created, all of them usually maintaining a benzyloxy connected to the 3 carbon of a tropane. Various modifications include substitutions on the benzene ring, as well as additions or substitutions in place of the normal carboxylate on the tropane 2 carbon. Various compound with similar structure activity relationships to cocaine that aren't technically analogues have been developed as well.
Mechanisms of action
Most stimulants exert their activating effects by enhancing catecholamine neurotransmission. Catecholamine neurotransmitters are employed in regulatory pathways implicated in attention, arousal, motivation, task salience and reward anticipation. Classical stimulants either block the reuptake or stimulate the efflux of these catecholamines, resulting in increased activity of their circuits. Some stimulants, specifically those with empathogenic and hallucinogenic effects, also affect serotonergic transmission. Some stimulants, such as some amphetamine derivatives and, notably, yohimbine, can decrease negative feedback by antagonizing regulatory autoreceptors.[71] Adrenergic agonists, such as, in part, ephedrine, act by directly binding to and activating adrenergic receptors, producing sympathomimetic effects.
There are also more indirect mechanisms of action a drug can elicit activating effects. Caffeine is an adenosine receptor antagonist, and only indirectly increases catecholamine transmission in the brain.[72] Pitolisant is an histamine 3 (H3)-receptor inverse agonist. As histamine 3 (H3) receptors mainly act as autoreceptors, pitolisant decreases negative feedback to histaminergic neurons, enhancing histaminergic transmission.
The precise mechanism of action of some stimulants, such as modafinil, for treating symptoms of narcolepsy and other sleep disorders, remains unknown.[73][74][75][76][77]
Notable stimulants
Amphetamine
Amphetamine is a potent central nervous system (CNS) stimulant of the phenethylamine class that is approved for the treatment of attention deficit hyperactivity disorder (ADHD) and narcolepsy.[78] Amphetamine is also used off-label as a performance and cognitive enhancer, and recreationally as an aphrodisiac and euphoriant.[79][80][81][82] Although it is a prescription medication in many countries, unauthorized possession and distribution of amphetamine is often tightly controlled due to the significant health risks associated with uncontrolled or heavy use.[83][84] As a consequence, amphetamine is illegally manufactured in clandestine labs to be trafficked and sold to users.[85] Based upon drug and drug precursor seizures worldwide, illicit amphetamine production and trafficking is much less prevalent than that of methamphetamine.[85]
The first pharmaceutical amphetamine was Benzedrine, a brand of inhalers used to treat a variety of conditions.[86][87] Because the dextrorotary isomer has greater stimulant properties, Benzedrine was gradually discontinued in favor of formulations containing all or mostly dextroamphetamine. Presently, it is typically prescribed as mixed amphetamine salts, dextroamphetamine, and lisdexamfetamine.[86][88]
Amphetamine is a norepinephrine-dopamine releasing agent (NDRA). It enters neurons through dopamine and norepinephrine transporters and facilitates neurotransmitter efflux by activating TAAR1 and inhibiting VMAT2.[67] At therapeutic doses, this causes emotional and cognitive effects such as euphoria, change in libido, increased arousal, and improved cognitive control.[80][81][89] Likewise, it induces physical effects such as decreased reaction time, fatigue resistance, and increased muscle strength.[79] In contrast, supratherapeutic doses of amphetamine are likely to impair cognitive function and induce rapid muscle breakdown.[78][80][90] Very high doses can result in psychosis (e.g., delusions and paranoia), which very rarely occurs at therapeutic doses even during long-term use.[91][92] As recreational doses are generally much larger than prescribed therapeutic doses, recreational use carries a far greater risk of serious side effects, such as dependence, which only rarely arises with therapeutic amphetamine use.[78][90][91]
Caffeine

Caffeine is a stimulant compound belonging to the xanthine class of chemicals naturally found in coffee, tea, and (to a lesser degree) cocoa or chocolate. It is included in many soft drinks, as well as a larger amount in energy drinks. Caffeine is the world's most widely used psychoactive drug and by far the most common stimulant. In North America, 90% of adults consume caffeine daily.[93]
A few jurisdictions restrict the sale and use of caffeine. In the United States, the FDA has banned the sale of pure and highly concentrated caffeine products for personal consumption, due to the risk of overdose and death.[94] The Australian Government has announced a ban on the sale of pure and highly concentrated caffeine food products for personal consumption, following the death of a young man from acute caffeine toxicity.[95][96]In Canada, Health Canada has proposed to limit the amount of caffeine in energy drinks to 180 mg per serving, and to require warning labels and other safety measures on these products.[95]
Caffeine is also included in some medications, usually for the purpose of enhancing the effect of the primary ingredient,[97] or reducing one of its side-effects (especially drowsiness).[98] Tablets containing standardized doses of caffeine are also widely available.[99]
Caffeine's mechanism of action differs from many stimulants, as it produces stimulant effects by inhibiting adenosine receptors.[100] Adenosine receptors are thought to be a large driver of drowsiness and sleep, and their action increases with extended wakefulness.[101] Caffeine has been found to increase striatal dopamine in animal models,[102] as well as inhibit the inhibitory effect of adenosine receptors on dopamine receptors,[103] however the implications for humans are unknown. Unlike most stimulants, caffeine has no addictive potential. Caffeine does not appear to be a reinforcing stimulus, and some degree of aversion may actually occur, per a study on drug abuse liability published in an NIDA research monograph that described a group preferring placebo over caffeine.[104] In large telephone surveys only 11% reported dependence symptoms. However, when people were tested in labs, only half of those who claim dependence actually experienced it, casting doubt on caffeine's ability to produce dependence and putting societal pressures in the spotlight.[105]
Coffee consumption is associated with a lower overall risk of cancer.[106] This is primarily due to a decrease in the risks of hepatocellular and endometrial cancer, but it may also have a modest effect on colorectal cancer.[107] There does not appear to be a significant protective effect against other types of cancers, and heavy coffee consumption may increase the risk of bladder cancer.[107] A protective effect of caffeine against Alzheimer's disease is possible, but the evidence is inconclusive.[108][109][110] Moderate coffee consumption may decrease the risk of cardiovascular disease,[111] and it may somewhat reduce the risk of type 2 diabetes.[112] Drinking 1-3 cups of coffee per day does not affect the risk of hypertension compared to drinking little or no coffee. However those who drink 2–4 cups per day may be at a slightly increased risk.[113] Caffeine increases intraocular pressure in those with glaucoma but does not appear to affect normal individuals.[114] It may protect people from liver cirrhosis.[115] There is no evidence that coffee stunts a child's growth.[116] Caffeine may increase the effectiveness of some medications including ones used to treat headaches.[117] Caffeine may lessen the severity of acute mountain sickness if taken a few hours prior to attaining a high altitude.[118]
Ephedrine
Ephedrine is a sympathomimetic amine similar in molecular structure to the well-known drugs phenylpropanolamine and methamphetamine, as well as to the important neurotransmitter epinephrine (adrenaline). Ephedrine is commonly used as a stimulant, appetite suppressant, concentration aid, and decongestant, and to treat hypotension associated with anaesthesia.
In chemical terms, it is an alkaloid with a phenethylamine skeleton found in various plants in the genus Ephedra (family Ephedraceae). It works mainly by increasing the activity of norepinephrine (noradrenaline) on adrenergic receptors.[119] It is most usually marketed as the hydrochloride or sulfate salt.
The herb má huáng (Ephedra sinica), used in traditional Chinese medicine (TCM), contains ephedrine and pseudoephedrine as its principal active constituents. The same may be true of other herbal products containing extracts from other Ephedra species.
MDMA
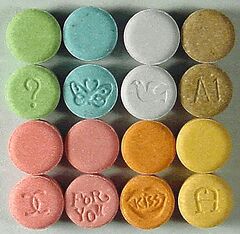
3,4-Methylenedioxymethamphetamine (MDMA, ecstasy, or molly) is a euphoriant, empathogen, and stimulant of the amphetamine class.[120] Briefly used by some psychotherapists as an adjunct to therapy, the drug became popular recreationally and the DEA listed MDMA as a Schedule I controlled substance, prohibiting most medical studies and applications. MDMA is known for its entactogenic properties. The stimulant effects of MDMA include hypertension, anorexia (appetite loss), euphoria, social disinhibition, insomnia (enhanced wakefulness/inability to sleep), improved energy, increased arousal, and increased perspiration, among others. Relative to catecholaminergic transmission, MDMA enhances serotonergic transmission significantly more, when compared to classical stimulants like amphetamine. MDMA does not appear to be significantly addictive or dependence forming.[121]
Due to the relative safety of MDMA, some researchers such as David Nutt have criticized the scheduling level, writing a satirical article finding MDMA to be 28 times less dangerous than horseriding, a condition he termed "equasy" or "Equine Addiction Syndrome".[122]
MDPV
Methylenedioxypyrovalerone (MDPV) is a psychoactive drug with stimulant properties that acts as a norepinephrine-dopamine reuptake inhibitor (NDRI).[123] It was first developed in the 1960s by a team at Boehringer Ingelheim.[124] MDPV remained an obscure stimulant until around 2004, when it was reported to be sold as a designer drug. Products labeled as bath salts containing MDPV were previously sold as recreational drugs in gas stations and convenience stores in the United States, similar to the marketing for Spice and K2 as incense.[125][126]
Incidents of psychological and physical harm have been attributed to MDPV use.[127][128]
Mephedrone
Mephedrone is a synthetic stimulant drug of the amphetamine and cathinone classes. Slang names include drone[129] and MCAT.[130] It is reported to be manufactured in China and is chemically similar to the cathinone compounds found in the khat plant of eastern Africa. It comes in the form of tablets or a powder, which users can swallow, snort, or inject, producing similar effects to MDMA, amphetamines, and cocaine.
Mephedrone was first synthesized in 1929, but did not become widely known until it was rediscovered in 2003. By 2007, mephedrone was reported to be available for sale on the Internet; by 2008 law enforcement agencies had become aware of the compound; and, by 2010, it had been reported in most of Europe, becoming particularly prevalent in the United Kingdom. Mephedrone was first made illegal in Israel in 2008, followed by Sweden later that year. In 2010, it was made illegal in many European countries, and, in December 2010, the EU ruled it illegal. In Australia, New Zealand, and the US, it is considered an analog of other illegal drugs and can be controlled by laws similar to the Federal Analog Act. In September 2011, the USA temporarily classified mephedrone as illegal, in effect from October 2011.
Mephedrone is neurotoxic and has abuse potential, predominantly exerted on 5-hydroxytryptamine (5-HT) terminals, mimicking that of MDMA with which it shares the same subjective sensations on abusers.[131][132][133]
Methamphetamine
Methamphetamine (contracted from N-methyl-alpha-methylphenethylamine) is a potent psychostimulant of the phenethylamine and amphetamine classes that is used to treat attention deficit hyperactivity disorder (ADHD) and obesity.[134][135][136] Methamphetamine exists as two enantiomers, dextrorotary and levorotary.[137][138] Dextromethamphetamine is a stronger CNS stimulant than levomethamphetamine;[90][137][138] however, both are addictive and produce the same toxicity symptoms at high doses.[138] Although rarely prescribed due to the potential risks, methamphetamine hydrochloride is approved by the United States Food and Drug Administration (USFDA) under the trade name Desoxyn.[135] Recreationally, methamphetamine is used to increase sexual desire, lift the mood, and increase energy, allowing some users to engage in sexual activity continuously for several days straight.[135][failed verification][139][unreliable source?]
Methamphetamine may be sold illicitly, either as pure dextromethamphetamine or in an equal parts mixture of the right- and left-handed molecules (i.e., 50% levomethamphetamine and 50% dextromethamphetamine).[139] Both dextromethamphetamine and racemic methamphetamine are schedule II controlled substances in the United States.[135] Also, the production, distribution, sale, and possession of methamphetamine is restricted or illegal in many other countries due to its placement in schedule II of the United Nations Convention on Psychotropic Substances treaty.[140][141] In contrast, levomethamphetamine is an over-the-counter drug in the United States.[note 1]
In low doses, methamphetamine can cause an elevated mood and increase alertness, concentration, and energy in fatigued individuals.[90][135] At higher doses, it can induce psychosis, rhabdomyolysis, and cerebral hemorrhage.[90][135] Methamphetamine is known to have a high potential for abuse and addiction.[90][135] Recreational use of methamphetamine may result in psychosis or lead to post-withdrawal syndrome, a withdrawal syndrome that can persist for months beyond the typical withdrawal period.[144] Unlike amphetamine and cocaine, methamphetamine is neurotoxic to humans, damaging both dopamine and serotonin neurons in the central nervous system (CNS).[134][136] Unlike the long-term use of amphetamine in prescription doses, which may improve certain brain regions in individuals with ADHD, there is evidence that methamphetamine causes brain damage from long-term use in humans;[134][136] this damage includes adverse changes in brain structure and function, such as reductions in gray matter volume in several brain regions and adverse changes in markers of metabolic integrity.[145][146][136] However, recreational amphetamine doses may also be neurotoxic.[147]
Methylphenidate
Methylphenidate is a stimulant drug that is often used in the treatment of ADHD and narcolepsy and occasionally to treat obesity in combination with diet restraints and exercise. Its effects at therapeutic doses include increased focus, increased alertness, decreased appetite, decreased need for sleep and decreased impulsivity. Methylphenidate is not usually used recreationally, but when it is used, its effects are very similar to those of amphetamines.
Methylphenidate acts as a norepinephrine-dopamine reuptake inhibitor, by blocking the norepinephrine transporter (NET) and the dopamine transporter (DAT). Methylphenidate has a higher affinity for the dopamine transporter than for the norepinephrine transporter, and so its effects are mainly due to elevated dopamine levels caused by the inhibited reuptake of dopamine, however increased norepinephrine levels also contribute to various of the effects caused by the drug.
Methylphenidate is sold under a number of brand names including Ritalin. Other versions include the long lasting tablet Concerta and the long lasting transdermal patch Daytrana.
Cocaine

Cocaine is an SNDRI. Cocaine is made from the leaves of the coca shrub, which grows in the mountain regions of South American countries such as Bolivia, Colombia, and Peru, regions in which it was cultivated and used for centuries mainly by the Aymara people. In Europe, North America, and some parts of Asia, the most common form of cocaine is a white crystalline powder. Cocaine is a stimulant but is not normally prescribed therapeutically for its stimulant properties, although it sees clinical use as a local anesthetic, in particular in ophthalmology.[148] Most cocaine use is recreational and its abuse potential is high (higher than amphetamine), and so its sale and possession are strictly controlled in most jurisdictions. Other tropane derivative drugs related to cocaine are also known such as troparil and lometopane but have not been widely sold or used recreationally.[149]
Nicotine
Nicotine is the active chemical constituent in tobacco, which is available in many forms, including cigarettes, cigars, chewing tobacco, and smoking cessation aids such as nicotine patches, nicotine gum, and electronic cigarettes. Nicotine is used widely throughout the world for its stimulating and relaxing effects. Nicotine exerts its effects through the agonism of nicotinic acetylcholine receptors, resulting in multiple downstream effects such as increase in activity of dopaminergic neurons in the midbrain reward system, and acetaldehyde one of the tobacco constituent decreased the expression of monoamine oxidase in the brain.[150] Nicotine is addictive and dependence forming. Tobacco, the most common source of nicotine, has an overall harm to user and self score 3 percent below cocaine, and 13 percent above amphetamines, ranking 6th most harmful of the 20 drugs assessed, as determined by a multi-criteria decision analysis.[151]
Phenylpropanolamine
Phenylpropanolamine (PPA; Accutrim; β-hydroxyamphetamine), also known as the stereoisomers norephedrine and norpseudoephedrine, is a psychoactive drug of the phenethylamine and amphetamine chemical classes that is used as a stimulant, decongestant, and anorectic agent.[152] It is commonly used in prescription and over-the-counter cough and cold preparations. In veterinary medicine, it is used to control urinary incontinence in dogs under trade names Propalin and Proin.
In the United States, PPA is no longer sold without a prescription due to a possible increased risk of stroke in younger women. In a few countries in Europe, however, it is still available either by prescription or sometimes over-the-counter. In Canada, it was withdrawn from the market on 31 May 2001.[153] In India, human use of PPA and its formulations were banned on 10 February 2011.[154]
Lisdexamfetamine
Lisdexamfetamine (Vyvanse, etc.) is an amphetamine-type medication, sold for use in treating ADHD.[155] Its effects typically last around 14 hours.[156] Lisdexamfetamine is inactive on its own and is metabolized into dextroamphetamine in the body.[56] Consequently, it has a lower abuse potential.[56]
Pseudoephedrine
Pseudoephedrine is a sympathomimetic drug of the phenethylamine and amphetamine chemical classes. It may be used as a nasal/sinus decongestant, as a stimulant,[157] or as a wakefulness-promoting agent.[158]
The salts pseudoephedrine hydrochloride and pseudoephedrine sulfate are found in many over-the-counter preparations, either as a single ingredient or (more commonly) in combination with antihistamines, guaifenesin, dextromethorphan, and/or paracetamol (acetaminophen) or another NSAID (such as aspirin or ibuprofen). It is also used as a precursor chemical in the illegal production of methamphetamine.
Catha edulis (Khat)

Khat is a flowering plant native to the Horn of Africa and the Arabian Peninsula.[159][160]
Khat contains a monoamine alkaloid called cathinone, a "keto-amphetamine". This alkaloid is said[by whom?] to cause excitement, loss of appetite, and euphoria. In 1980, the World Health Organization (WHO) classified it as a drug of abuse that can produce mild to moderate psychological dependence (less than tobacco or alcohol),[161] although the WHO does not consider khat to be seriously addictive.[160] It is banned in some countries, such as the United States, Canada, and Germany, while its production, sale, and consumption are legal in other countries, including Djibouti, Ethiopia, Somalia, Kenya and Yemen.[162]
Modafinil
Modafinil is an eugeroic medication, which means that it promotes wakefulness and alertness. Modafinil is sold under the brand name Provigil among others. Modafinil is used to treat excessive daytime sleepiness due to narcolepsy, shift work sleep disorder, or obstructive sleep apnea. While it has seen off-label use as a purported cognitive enhancer, the research on its effectiveness for this use is not conclusive.[163] Despite being a CNS stimulant, the addiction and dependence liabilities of modafinil are considered very low.[164][165][166] Although modafinil shares biochemical mechanisms with stimulant drugs, it is less likely to have mood-elevating properties.[165] The similarities in effects with caffeine are not clearly established.[167][168] Unlike other stimulants, modafinil does not induce a subjective feeling of pleasure or reward, which is commonly associated with euphoria, an intense feeling of well-being. Euphoria is a potential indicator of drug abuse, which is the compulsive and excessive use of a substance despite adverse consequences. In clinical trials, modafinil has shown no evidence of abuse potential, that is why modafinil is considered to have a low risk of addiction and dependence, however, caution is advised.[169][170]
Pitolisant
Pitolisant is an inverse agonist (antagonist) of the histamine 3 (H3) autoreceptor. As such, pitolisant is an antihistamine medication that also belongs to the class of CNS stimulants.[171][172][173][174] Pitolisant is also considered a medication of eugeroic class, which means that it promotes wakefulness and alertness. Pitolisant is the first eugeroic drug that acts by blocking the H3 autoreceptor.[175][176][177]
Pitolisant has been shown to be effective and well-tolerated for the treatment of narcolepsy with or without cataplexy.[177][176][175]
Pitolisant is the only non-controlled anti-narcoleptic drug in the United States .[175] It has shown minimal abuse risk in studies.[175][178]
Blocking the histamine 3 (H3) autoreceptor increases the activity of histamine neurons in the brain. The H3 autoreceptors regulate histaminergic activity in the central nervous system (and to a lesser extent, the peripheral nervous system) by inhibiting histamine biosynthesis and release upon binding to endogenous histamine.[179] By preventing the binding of endogenous histamine at the H3, as well as producing a response opposite to that of endogenous histamine at the receptor (inverse agonism), pitolisant enhances histaminergic activity in the brain.[180]
Recreational use and issues of abuse
Stimulants enhance the activity of the central and peripheral nervous systems. Common effects may include increased alertness, awareness, wakefulness, endurance, productivity, and motivation, arousal, locomotion, heart rate, and blood pressure, and a diminished desire for food and sleep. Use of stimulants may cause the body to reduce significantly its production of natural body chemicals that fulfill similar functions. Until the body reestablishes its normal state, once the effect of the ingested stimulant has worn off the user may feel depressed, lethargic, confused, and miserable. This is referred to as a "crash", and may provoke reuse of the stimulant.
Abuse of central nervous system (CNS) stimulants is common. Addiction to some CNS stimulants can quickly lead to medical, psychiatric, and psychosocial deterioration. Drug tolerance, dependence, and sensitization as well as a withdrawal syndrome can occur.[181] Stimulants may be screened for in animal discrimination and self-administration models which have high sensitivity albeit low specificity.[182] Research on a progressive ratio self-administration protocol has found amphetamine, methylphenidate, modafinil, cocaine, and nicotine to all have a higher break point than placebo that scales with dose indicating reinforcing effects.[183] A progressive ratio self-administration protocol is a way of testing how much an animal or a human wants a drug by making them do a certain action (like pressing a lever or poking a nose device) to get the drug. The number of actions needed to get the drug increases every time, so it becomes harder and harder to get the drug. The highest number of actions that the animal or human is willing to do to get the drug is called the break point. The higher the break point, the more the animal or human wants the drug. In contrast to the classical stimulants such as amphetamine, the effects of modafinil depend on what the animals or humans have to do after getting the drug. If they have to do a performance task, like solving a puzzle or remembering something, modafinil makes them work harder for it than placebo, and the subjects wanted to self-administer modafinil. But if they had to do a relaxation task, like listening to music or watching a video, the subjects did not want to self-administer modafinil. This suggests that modafinil is more rewarding when it helps the animals or humans do something better or faster, especially considering that modafinil is not commonly abused or depended on by people, unlike other stimulants.[183]
| Dependence potentials of common stimulants[161] | ||||
|---|---|---|---|---|
| Drug | Mean | Pleasure | Psychological dependence | Physical dependence |
| Cocaine | 2.39 | 3.0 | 2.8 | 1.3 |
| Tobacco | 2.21 | 2.3 | 2.6 | 1.8 |
| Amphetamine | 1.67 | 2.0 | 1.9 | 1.1 |
| Ecstasy | 1.13 | 1.5 | 1.2 | 0.7 |
Treatment for misuse
Psychosocial treatments, such as contingency management, have demonstrated improved effectiveness when added to treatment as usual consisting of counselling and/or case-management. This is demonstrated with a decrease in dropout rates and a lengthening of periods of abstinence.[184]
Testing
The presence of stimulants in the body may be tested by a variety of procedures. Serum and urine are the common sources of testing material although saliva is sometimes used. Commonly used tests include chromatography, immunologic assay, and mass spectrometry.[185]
See also
- Antidepressants
- Depressants
- Hallucinogens
- Nootropics
- Psychoanaleptics
Notes
References
- ↑ "stimulant – definition of stimulant in English | Oxford Dictionaries". https://en.oxforddictionaries.com/definition/stimulant.
- ↑ 2.0 2.1 Center for Substance Abuse Treatment (1999) (in en). Chapter 2—How Stimulants Affect the Brain and Behavior. Substance Abuse and Mental Health Services Administration (US). https://www.ncbi.nlm.nih.gov/books/NBK64328/.
- ↑ "Natural Sympathomimetic Drugs: From Pharmacology to Toxicology". Biomolecules 12 (12): 1793. November 2022. doi:10.3390/biom12121793. PMID 36551221.
- ↑ 4.0 4.1 4.2 "In search of optimal psychoactivation: stimulants as cognitive performance enhancers". Arh Hig Rada Toksikol 70 (3): 150–159. September 2019. doi:10.2478/aiht-2019-70-3298. PMID 32597132.
- ↑ "Definition of ERGOGENIC". https://www.merriam-webster.com/dictionary/ergogenic.
- ↑ Avois, L; Robinson, N; Saudan, C; Baume, N; Mangin, P; Saugy, M (7 January 2017). "Central nervous system stimulants and sport practice". British Journal of Sports Medicine 40 (Suppl 1): i16–i20. doi:10.1136/bjsm.2006.027557. ISSN 0306-3674. PMID 16799095.
- ↑ 7.0 7.1 7.2 Bagot, Kara Simone; Kaminer, Yifrah (1 April 2014). "Efficacy of stimulants for cognitive enhancement in non-attention deficit hyperactivity disorder youth: a systematic review". Addiction 109 (4): 547–557. doi:10.1111/add.12460. ISSN 1360-0443. PMID 24749160.
- ↑ "Effects of Modafinil (Provigil) on Memory and Learning in Experimental and Clinical Studies: From Molecular Mechanisms to Behaviour Molecular Mechanisms and Behavioural Effects". Current Molecular Pharmacology 16 (4): 507–516. 2023. doi:10.2174/1874467215666220901122824. PMID 36056861.
- ↑ "A review on modafinil: the characteristics, function, and use in critical care". Journal of Drug Assessment 9 (1): 82–86. 2020. doi:10.1080/21556660.2020.1745209. PMID 32341841.
- ↑ Rethinking Cognitive Enhancement. Oxford University Press. 2017. p. 116. ISBN 978-0-19-872739-2. https://books.google.com/books?id=aAIXDgAAQBAJ&pg=PA116.
- ↑ Morton, W. Alexander; Stockton, Gwendolyn G. (8 January 2017). "Methylphenidate Abuse and Psychiatric Side Effects". Primary Care Companion to the Journal of Clinical Psychiatry 2 (5): 159–164. doi:10.4088/PCC.v02n0502. ISSN 1523-5998. PMID 15014637.
- ↑ "Chapter 5—Medical Aspects of Stimulant Use Disorders" (in en). Treatment for Stimulant Use Disorders.Chapter 5—Medical Aspects of Stimulant Use Disorders. Center for Substance Abuse Treatment. Treatment for Stimulant Use Disorders. Rockville (MD): Substance Abuse and Mental Health Services Administration (US). 1999. https://www.ncbi.nlm.nih.gov/books/NBK64323/.
- ↑ Westover, Arthur N.; Halm, Ethan A. (9 June 2012). "Do prescription stimulants increase the risk of adverse cardiovascular events?: A systematic review". BMC Cardiovascular Disorders 12 (1): 41. doi:10.1186/1471-2261-12-41. ISSN 1471-2261. PMID 22682429.
- ↑ Fredriksen, Mats; Halmøy, Anne; Faraone, Stephen V.; Haavik, Jan (1 June 2013). "Long-term efficacy and safety of treatment with stimulants and atomoxetine in adult ADHD: a review of controlled and naturalistic studies". European Neuropsychopharmacology 23 (6): 508–527. doi:10.1016/j.euroneuro.2012.07.016. ISSN 1873-7862. PMID 22917983.
- ↑ Hammerness, Paul G.; Karampahtsis, Chris; Babalola, Ronke; Alexander, Mark E. (1 April 2015). "Attention-deficit/hyperactivity disorder treatment: what are the long-term cardiovascular risks?". Expert Opinion on Drug Safety 14 (4): 543–551. doi:10.1517/14740338.2015.1011620. ISSN 1744-764X. PMID 25648243.
- ↑ Hechtman, Lily; Greenfield, Brian (1 January 2003). "Long-term use of stimulants in children with attention deficit hyperactivity disorder: safety, efficacy, and long-term outcome". Paediatric Drugs 5 (12): 787–794. doi:10.2165/00148581-200305120-00002. ISSN 1174-5878. PMID 14658920.
- ↑ Sordo, L; Indave, BI; Barrio, G; Degenhardt, L; de la Fuente, L; Bravo, MJ (1 September 2014). "Cocaine use and risk of stroke: a systematic review.". Drug and Alcohol Dependence 142: 1–13. doi:10.1016/j.drugalcdep.2014.06.041. PMID 25066468.
- ↑ COUGHLIN, P; MAVOR, A (1 October 2006). "Arterial Consequences of Recreational Drug Use". European Journal of Vascular and Endovascular Surgery 32 (4): 389–396. doi:10.1016/j.ejvs.2006.03.003. PMID 16682239.
- ↑ Tashkin, D. P. (1 March 2001). "Airway effects of marijuana, cocaine, and other inhaled illicit agents". Current Opinion in Pulmonary Medicine 7 (2): 43–61. doi:10.1097/00063198-200103000-00001. ISSN 1070-5287. PMID 11224724.
- ↑ "Cocaine abuse and connective tissue disease". J Am Acad Dermatol 10 (3): 525. 1984. doi:10.1016/S0190-9622(84)80112-7. PMID 6725666.
- ↑ Ramón Peces; Navascués, RA; Baltar, J; Seco, M; Alvarez, J (1999). "Antiglomerular Basement Membrane Antibody-Mediated Glomerulonephritis after Intranasal Cocaine Use". Nephron 81 (4): 434–438. doi:10.1159/000045328. PMID 10095180.
- ↑ "Neurology of the vasculitides and connective tissue diseases". J. Neurol. Neurosurg. Psychiatry 65 (1): 10–22. 1998. doi:10.1136/jnnp.65.1.10. PMID 9667555.
- ↑ "Toxicity of amphetamines: an update". Arch. Toxicol. 86 (8): 1167–1231. August 2012. doi:10.1007/s00204-012-0815-5. PMID 22392347.
- ↑ "Methamphetamine-induced neurotoxicity: the road to Parkinson's disease". Pharmacol Rep 61 (6): 966–977. 2009. doi:10.1016/s1734-1140(09)70158-6. PMID 20081231. http://www.if-pan.krakow.pl/pjp/pdf/2009/6_966.pdf.
- ↑ "Intraneuronal dopamine-quinone synthesis: a review". Neurotox. Res. 1 (3): 181–195. February 2000. doi:10.1007/BF03033289. PMID 12835101.
- ↑ "Dopaminergic neuron-specific oxidative stress caused by dopamine itself". Acta Med. Okayama 62 (3): 141–150. June 2008. doi:10.18926/AMO/30942. PMID 18596830.
- ↑ "Top 100 Drugs for Q4 2013 by Sales – U.S. Pharmaceutical Statistics". https://www.drugs.com/stats/top100/sales.
- ↑ "World Drug Report 2015". p. 149. https://www.unodc.org/documents/wdr2015/World_Drug_Report_2015.pdf.
- ↑ Harper, S. J.; Jones, N. S. (1 October 2006). "Cocaine: what role does it have in current ENT practice? A review of the current literature". The Journal of Laryngology and Otology 120 (10): 808–811. doi:10.1017/S0022215106001459. ISSN 1748-5460. PMID 16848922.
- ↑ Kaplan, Lee M. (1 March 2005). "Pharmacological therapies for obesity". Gastroenterology Clinics of North America 34 (1): 91–104. doi:10.1016/j.gtc.2004.12.002. ISSN 0889-8553. PMID 15823441.
- ↑ Palamara, Kerri L.; Mogul, Harriette R.; Peterson, Stephen J.; Frishman, William H. (1 October 2016). "Obesity: new perspectives and pharmacotherapies". Cardiology in Review 14 (5): 238–258. doi:10.1097/01.crd.0000233903.57946.fd. ISSN 1538-4683. PMID 16924165.
- ↑ "The Voice of the Patient A series of reports from the U.S. Food and Drug Administration's (FDA's) Patient-Focused Drug Development Initiative". Center for Drug Evaluation and Research (CDER) U.S. Food and Drug Administration (FDA). https://www.fda.gov/downloads/ForIndustry/UserFees/PrescriptionDrugUserFee/UCM402907.pdf.
- ↑ Heal, David J; Smith, Sharon L; Gosden, Jane; Nutt, David J (7 January 2017). "Amphetamine, past and present – a pharmacological and clinical perspective". Journal of Psychopharmacology 27 (6): 479–496. doi:10.1177/0269881113482532. ISSN 0269-8811. PMID 23539642.
- ↑ Research, Center for Drug Evaluation and (26 June 2019). "Drug Safety and Availability - FDA Drug Safety Communication: Safety Review Update of Medications used to treat Attention-Deficit/Hyperactivity Disorder (ADHD) in adults" (in en). https://www.fda.gov/Drugs/DrugSafety/ucm279858.htm.
- ↑ Stotz, Gabriele; Woggon, Brigitte; Angst, Jules (1 December 1999). "Psychostimulants in the therapy of treatment-resistant depression Review of the literature and findings from a retrospective study in 65 depressed patients". Dialogues in Clinical Neuroscience 1 (3): 165–174. doi:10.31887/DCNS.1999.1.3/gstotz. ISSN 1294-8322. PMID 22034135.
- ↑ Doig RL (February 1905). "Epinephrin; especially in asthma". California State Journal of Medicine 3 (2): 54–5. PMID 18733372.
- ↑ Chu, Eric K.; Drazen, Jeffrey M. (1 June 2005). "Asthma". American Journal of Respiratory and Critical Care Medicine 171 (11): 1202–1208. doi:10.1164/rccm.200502-257OE. ISSN 1073-449X. PMID 15778490.
- ↑ Bicopoulos D, editor. AusDI: Drug information for the healthcare professional, 2nd edition. Castle Hill: Pharmaceutical Care Information Services; 2002.
- ↑ "Pseudoephedrine (By mouth) – National Library of Medicine". https://www.ncbi.nlm.nih.gov/pubmedhealth/PMHT0011888/.
- ↑ 40.0 40.1 "The creation of the concept of an antidepressant: an historical analysis". Soc Sci Med 66 (11): 2346–55. June 2008. doi:10.1016/j.socscimed.2008.01.047. PMID 18321627.
- ↑ 41.0 41.1 41.2 41.3 J. Moncrieff (13 April 2016). The Myth of the Chemical Cure: A Critique of Psychiatric Drug Treatment. Springer. pp. 121–. ISBN 978-0-230-58944-5. OCLC 1047624331. https://books.google.com/books?id=2tD7CwAAQBAJ&pg=PA121. "A well-known textbook of physical treatments described stimulants as having 'limited value in depression' because the euphoria they induce quickly wears off and 'the patient slips back' (Sargant & Slater 1944)."
- ↑ "Brief history of the medical and non-medical use of amphetamine-like psychostimulants". Exp Neurol 342: 113754. August 2021. doi:10.1016/j.expneurol.2021.113754. PMID 34000249.
- ↑ 43.0 43.1 "Stimulants for depression: On the up and up?". Aust N Z J Psychiatry 50 (3): 203–7. March 2016. doi:10.1177/0004867416634208. PMID 26906078.
- ↑ 44.0 44.1 44.2 "Psychostimulants in the treatment of depression: a review of the evidence". CNS Drugs 21 (3): 239–57. 2007. doi:10.2165/00023210-200721030-00004. PMID 17338594.
- ↑ 45.0 45.1 45.2 "Dopamine and Beyond: Implications of Psychophysical Studies of Intracranial Self-Stimulation for the Treatment of Depression". Brain Sci 12 (8): 1052. August 2022. doi:10.3390/brainsci12081052. PMID 36009115.
- ↑ 46.0 46.1 46.2 "The Convergence Model of Brain Reward Circuitry: Implications for Relief of Treatment-Resistant Depression by Deep-Brain Stimulation of the Medial Forebrain Bundle". Front Behav Neurosci 16: 851067. 2022. doi:10.3389/fnbeh.2022.851067. PMID 35431828.
- ↑ "Efficacy and tolerability of lisdexamfetamine as an antidepressant augmentation strategy: A meta-analysis of randomized controlled trials". J Affect Disord 226: 294–300. January 2018. doi:10.1016/j.jad.2017.09.041. PMID 29028590.
- ↑ "The Efficacy of Psychostimulants in Major Depressive Episodes: A Systematic Review and Meta-Analysis". J Clin Psychopharmacol 37 (4): 412–418. August 2017. doi:10.1097/JCP.0000000000000723. PMID 28590365.
- ↑ "Comparative efficacy and safety of stimulant-type medications for depression: A systematic review and network meta-analysis". J Affect Disord 292: 416–423. September 2021. doi:10.1016/j.jad.2021.05.119. PMID 34144366.
- ↑ "Augmentation strategies for treatment resistant major depression: A systematic review and network meta-analysis". J Affect Disord 302: 385–400. April 2022. doi:10.1016/j.jad.2021.12.134. PMID 34986373.
- ↑ 51.0 51.1 51.2 "Psychostimulant withdrawal as an inducing condition in animal models of depression". Neurosci Biobehav Rev 29 (4–5): 675–706. 2005. doi:10.1016/j.neubiorev.2005.03.012. PMID 15893821.
- ↑ "Development of a non-human primate model to support CNS translational research: Demonstration with D-amphetamine exposure and dopamine response". J Neurosci Methods 317: 71–81. April 2019. doi:10.1016/j.jneumeth.2019.02.005. PMID 30768951.
- ↑ "Development of a Semimechanistic Pharmacokinetic-Pharmacodynamic Model Describing Dextroamphetamine Exposure and Striatal Dopamine Response in Rats and Nonhuman Primates following a Single Dose of Dextroamphetamine". J Pharmacol Exp Ther 369 (1): 107–120. April 2019. doi:10.1124/jpet.118.254508. PMID 30733244.
- ↑ van Gaalen, Marcel M.; Schlumbohm, Christina; Folgering, Joost H.; Adhikari, Saugat; Bhattacharya, Chandrali; Steinbach, Douglas; Stratford, Robert E. (7 February 2019). "Development of a Semimechanistic Pharmacokinetic-Pharmacodynamic Model Describing Dextroamphetamine Exposure and Striatal Dopamine Response in Rats and Nonhuman Primates following a Single Dose of Dextroamphetamine". Journal of Pharmacology and Experimental Therapeutics (American Society for Pharmacology & Experimental Therapeutics (ASPET)) 369 (1): 107–120. doi:10.1124/jpet.118.254508. ISSN 0022-3565. PMID 30733244.
- ↑ "Lisdexamfetamine Dimesylate: Prodrug Delivery, Amphetamine Exposure and Duration of Efficacy". Clin Drug Investig 36 (5): 341–56. May 2016. doi:10.1007/s40261-015-0354-y. PMID 27021968.
- ↑ 56.0 56.1 56.2 "Pharmacokinetics and Pharmacodynamics of Lisdexamfetamine Compared with D-Amphetamine in Healthy Subjects". Front Pharmacol 8: 617. 2017. doi:10.3389/fphar.2017.00617. PMID 28936175.
- ↑ "Acute tolerance to subjective but not cardiovascular effects of d-amphetamine in normal, healthy men". J Clin Psychopharmacol 16 (1): 72–6. February 1996. doi:10.1097/00004714-199602000-00012. PMID 8834422.
- ↑ "Effects of repeated oral methamphetamine administration in humans". Psychopharmacology (Berl) 155 (4): 397–404. June 2001. doi:10.1007/s002130100727. PMID 11441429.
- ↑ "A 'crash' course on psychostimulant withdrawal as a model of depression". Trends Pharmacol Sci 23 (10): 475–82. October 2002. doi:10.1016/s0165-6147(02)02086-2. PMID 12368072.
- ↑ "Neural substrates of psychostimulant withdrawal-induced anhedonia". Curr Top Behav Neurosci. Current Topics in Behavioral Neurosciences (Berlin, Heidelberg) 3: 119–78. 2010. doi:10.1007/7854_2009_20. ISBN 978-3-642-03000-0. PMID 21161752.
- ↑ "Common substrates of dysphoria in stimulant drug abuse and primary depression: therapeutic targets". Int Rev Neurobiol. International Review of Neurobiology 65: 117–45. 2005. doi:10.1016/S0074-7742(04)65005-7. ISBN 978-0-12-366866-0. PMID 16140055.
- ↑ "Sulfur-substituted alpha-alkyl phenethylamines as selective and reversible MAO-A inhibitors: biological activities, CoMFA analysis, and active site modeling". J Med Chem 48 (7): 2407–19. April 2005. doi:10.1021/jm0493109. PMID 15801832.
- ↑ "Structure-activity relationships for locomotor stimulant effects and monoamine transporter interactions of substituted amphetamines and cathinones". Neuropharmacology 245: 109827. March 2024. doi:10.1016/j.neuropharm.2023.109827. PMID 38154512.
- ↑ 64.00 64.01 64.02 64.03 64.04 64.05 64.06 64.07 64.08 64.09 64.10 64.11 64.12 "Biosynthesis of amphetamine analogs in plants". Trends Plant Sci. 17 (7): 404–412. 2012. doi:10.1016/j.tplants.2012.03.004. PMID 22502775. "Substituted amphetamines, which are also called phenylpropylamino alkaloids, are a diverse group of nitrogen-containing compounds that feature a phenethylamine backbone with a methyl group at the α-position relative to the nitrogen (Figure 1). Countless variation in functional group substitutions has yielded a collection of synthetic drugs with diverse pharmacological properties as stimulants, empathogens and hallucinogens [3]. ... Beyond (1R,2S)-ephedrine and (1S,2S)-pseudoephedrine, myriad other substituted amphetamines have important pharmaceutical applications. The stereochemistry at the α-carbon is often a key determinant of pharmacological activity, with (S)-enantiomers being more potent. For example, (S)-amphetamine, commonly known as d-amphetamine or dextroamphetamine, displays five times greater psychostimulant activity compared with its (R)-isomer [78]. Most such molecules are produced exclusively through chemical syntheses and many are prescribed widely in modern medicine. For example, (S)-amphetamine (Figure 4b), a key ingredient in Adderall and Dexedrine, is used to treat attention deficit hyperactivity disorder (ADHD) [79]. ...
[Figure 4](b) Examples of synthetic, pharmaceutically important substituted amphetamines.". - ↑ 65.0 65.1 Glennon RA (2013). Foye's principles of medicinal chemistry (7th ed.). Philadelphia, USA: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 646–648. ISBN 978-1-60913-345-0. "The simplest unsubstituted phenylisopropylamine, 1-phenyl-2-aminopropane, or amphetamine, serves as a common structural template for hallucinogens and psychostimulants. Amphetamine produces central stimulant, anorectic, and sympathomimetic actions, and it is the prototype member of this class (39)."
- ↑ "Determination of ring- and N-substituted amphetamines as heptafluorobutyryl derivatives". Forensic Sci. Int. 49 (2): 205–213. March 1991. doi:10.1016/0379-0738(91)90081-s. PMID 1855720.
- ↑ 67.0 67.1 67.2 Miller GM (January 2011). "The emerging role of trace amine-associated receptor 1 in the functional regulation of monoamine transporters and dopaminergic activity". J. Neurochem. 116 (2): 164–176. doi:10.1111/j.1471-4159.2010.07109.x. PMID 21073468.
- ↑ "VMAT2: a dynamic regulator of brain monoaminergic neuronal function interacting with drugs of abuse". Ann. N. Y. Acad. Sci. 1216 (1): 86–98. January 2011. doi:10.1111/j.1749-6632.2010.05906.x. PMID 21272013. Bibcode: 2011NYASA1216...86E.
- ↑ Dale, Elena; Bang-Andersen, Benny; Sánchez, Connie (2015). "Emerging mechanisms and treatments for depression beyond SSRIs and SNRIs". Biochemical Pharmacology 95 (2): 81–97. doi:10.1016/j.bcp.2015.03.011. ISSN 0006-2952. PMID 25813654.
- ↑ Efforts of the National Institute on Drug Abuse to Prevent and Treat Prescription Drug Abuse , Testimony Before the Subcommittee on Criminal Justice, Drug Policy, and Human Resources Committee on Government Reform, United States House of Representatives, 26 July 2006
- ↑ Docherty, J R (7 January 2017). "Pharmacology of stimulants prohibited by the World Anti-Doping Agency (WADA)". British Journal of Pharmacology 154 (3): 606–622. doi:10.1038/bjp.2008.124. ISSN 0007-1188. PMID 18500382.
- ↑ (in en) Caffeine for the Sustainment of Mental Task Performance: Formulations for Military Operations.. Washington (DC): National Academies Press (US). 2001. https://www.ncbi.nlm.nih.gov/books/NBK223808/.
- ↑ "Modafinil Monograph for Professionals". American Society of Health-System Pharmacists. https://www.drugs.com/monograph/modafinil.html.
- ↑ "Update on the pharmacologic management of narcolepsy: mechanisms of action and clinical implications". Sleep Medicine 68: 97–109. April 2020. doi:10.1016/j.sleep.2019.09.001. PMID 32032921.
- ↑ "Modafinil". Prescriber's Guide: Stahl's Essential Psychopharmacology (6th ed.). Cambridge, United Kingdom: Cambridge University Press. March 2017. pp. 491–495. ISBN 978-1-108-22874-9.
- ↑ "Mechanisms of modafinil: A review of current research". Neuropsychiatric Disease and Treatment 3 (3): 349–364. June 2007. PMID 19300566.
- ↑ "Adenosine and Sleep". Handbook of Experimental Pharmacology 253: 359–381. 2019. doi:10.1007/164_2017_36. ISBN 978-3-030-11270-7. PMID 28646346.
- ↑ 78.0 78.1 78.2 "Adderall XR Prescribing Information". United States Food and Drug Administration. June 2013. p. 11. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s024lbl.pdf.
- ↑ 79.0 79.1 "Nutritional supplements and ergogenic AIDS". Prim. Care 40 (2): 487–505. June 2013. doi:10.1016/j.pop.2013.02.009. PMID 23668655. "Amphetamines and caffeine are stimulants that increase alertness, improve focus, decrease reaction time, and delay fatigue, allowing for an increased intensity and duration of training...
Physiologic and performance effects
• Amphetamines increase dopamine/norepinephrine release and inhibit their reuptake, leading to central nervous system (CNS) stimulation
• Amphetamines seem to enhance athletic performance in anaerobic conditions 39 40
• Improved reaction time
• Increased muscle strength and delayed muscle fatigue
• Increased acceleration
• Increased alertness and attention to task". - ↑ 80.0 80.1 80.2 "Chapter 13: Higher Cognitive Function and Behavioral Control". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. 2009. p. 318. ISBN 978-0-07-148127-4. "Therapeutic (relatively low) doses of psychostimulants, such as methylphenidate and amphetamine, improve performance on working memory tasks both in individuals with ADHD and in normal subjects...it is now believed that dopamine and norepinephrine, but not serotonin, produce the beneficial effects of stimulants on working memory. At abused (relatively high) doses, stimulants can interfere with working memory and cognitive control, as will be discussed below. It is important to recognize, however, that stimulants act not only on working memory function, but also on general levels of arousal and, within the nucleus accumbens, improve the saliency of tasks. Thus, stimulants improve performance on effortful but tedious tasks...through indirect stimulation of dopamine and norepinephrine receptors."
- ↑ 81.0 81.1 Montgomery KA (June 2008). "Sexual desire disorders". Psychiatry 5 (6): 50–55. PMID 19727285.
- ↑ "Misuse and diversion of stimulants prescribed for ADHD: a systematic review of the literature". J. Am. Acad. Child Adolesc. Psychiatry 47 (1): 21–31. January 2008. doi:10.1097/chi.0b013e31815a56f1. PMID 18174822. "Stimulant misuse appears to occur both for performance enhancement and their euphorogenic effects, the latter being related to the intrinsic properties of the stimulants (e.g., IR versus ER profile)...
Although useful in the treatment of ADHD, stimulants are controlled II substances with a history of preclinical and human studies showing potential abuse liability.". - ↑ "Convention on psychotropic substances". United Nations Treaty Collection. United Nations. http://treaties.un.org/Pages/ViewDetails.aspx?src=TREATY&mtdsg_no=VI-16&chapter=6&lang=en.
- ↑ "Methamphetamine facts". DrugPolicy.org. http://www.drugpolicy.org/drug-facts/methamphetamine-facts.
- ↑ 85.0 85.1 "World Drug Report 2006". United Nations Office on Drugs and Crime. 2006. pp. 128–135. http://www.unodc.org/pdf/WDR_2006/wdr2006_volume1.pdf.
- ↑ 86.0 86.1 "Amphetamine, past and present – a pharmacological and clinical perspective". J. Psychopharmacol. 27 (6): 479–496. June 2013. doi:10.1177/0269881113482532. PMID 23539642.
- ↑ Rasmussen N (July 2006). "Making the first anti-depressant: amphetamine in American medicine, 1929–1950". J. Hist. Med. Allied Sci. 61 (3): 288–323. doi:10.1093/jhmas/jrj039. PMID 16492800.
- ↑ "Adderall IR Prescribing Information". United States Food and Drug Administration. March 2007. p. 5. http://www.accessdata.fda.gov/drugsatfda_docs/label/2007/011522s040lbl.pdf.
- ↑ "Adderall XR Prescribing Information". United States Food and Drug Administration. June 2013. pp. 4–8. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021303s024lbl.pdf.
- ↑ 90.0 90.1 90.2 90.3 90.4 90.5 Goodman & Gilman's Pharmacological Basis of Therapeutics (12th ed.). New York: McGraw-Hill. 2010. ISBN 978-0-07-162442-8.
- ↑ 91.0 91.1 "Treatment for amphetamine psychosis (Review)". Cochrane Database of Systematic Reviews 2009 (1): CD003026. 2009. doi:10.1002/14651858.CD003026.pub3. PMID 19160215.
- ↑ Greydanus D. "Stimulant Misuse: Strategies to Manage a Growing Problem". American College Health Association. ACHA Professional Development Program. p. 20. http://www.acha.org/prof_dev/ADHD_docs/ADHD_PDprogram_Article2.pdf.
- ↑ Lovett R (24 September 2005). "Coffee: The demon drink?". New Scientist (2518). https://www.newscientist.com/article.ns?id=mg18725181.700. Retrieved 3 August 2009. (Subscription content?)
- ↑ Commissioner, Office of the (24 March 2020). "FDA warns companies to stop selling dangerous and illegal pure and highly concentrated caffeine products". https://www.fda.gov/news-events/press-announcements/fda-warns-companies-stop-selling-dangerous-and-illegal-pure-and-highly-concentrated-caffeine.
- ↑ 95.0 95.1 https://www.tga.gov.au/resources/publication/scheduling-decisions-interim/interim-decisions-and-invitation-further-comment-substances-referred-november-2019-acmsaccs-meetings/31-interim-decision-relation-caffeine
- ↑ https://www.health.gov.au/ministers/senator-the-hon-richard-colbeck/media/australia-to-protect-consumers-by-banning-sale-of-pure-caffeine-powder
- ↑ "Caffeine in the management of patients with headache". J Headache Pain 18 (1): 107. October 2017. doi:10.1186/s10194-017-0806-2. PMID 29067618.
- ↑ Bolton, S.; Null, G. (1981). "Caffeine: Psychological Effects, Use and Abuse". Orthomolecular Psychiatry 10 (3): 202–211. http://orthomolecular.org/library/jom/1981/pdf/1981-v10n03-p202.pdf.
- ↑ "Caffeine-Related Deaths: Manner of Deaths and Categories at Risk". Nutrients 10 (5): 611. May 2018. doi:10.3390/nu10050611. PMID 29757951.
- ↑ Nehlig, A.; Daval, J. L.; Debry, G. (1 August 2016). "Caffeine and the central nervous system: mechanisms of action, biochemical, metabolic and psychostimulant effects". Brain Research. Brain Research Reviews 17 (2): 139–170. doi:10.1016/0165-0173(92)90012-b. PMID 1356551.
- ↑ Bjorness, Theresa E; Greene, Robert W (8 January 2017). "Adenosine and Sleep". Current Neuropharmacology 7 (3): 238–245. doi:10.2174/157015909789152182. ISSN 1570-159X. PMID 20190965.
- ↑ Solinas, Marcello; Ferré, Sergi; You, Zhi-Bing; Karcz-Kubicha, Marzena; Popoli, Patrizia; Goldberg, Steven R. (1 August 2002). "Caffeine Induces Dopamine and Glutamate Release in the Shell of the Nucleus Accumbens" (in en). Journal of Neuroscience 22 (15): 6321–6324. doi:10.1523/JNEUROSCI.22-15-06321.2002. ISSN 0270-6474. PMID 12151508.
- ↑ "Oligomerization of adenosine A2A and dopamine D2 receptors in living cells". Biochemical and Biophysical Research Communications 306 (2): 544–9. Jun 2003. doi:10.1016/S0006-291X(03)00991-4. PMID 12804599.
- ↑ Fishchman, N; Mello, N. Testing for Abuse Liability of Drugs in Humans. Rockville, MD: U.S. Department of Health and Human Services Public Health Service Alcohol, Drug Abuse, and Mental Health Administration National Institute on Drug Abuse. p. 179. http://ww1.drugabuse.gov/pdf/monographs/92.pdf.
- ↑ "Caffeine use in children: what we know, what we have left to learn, and why we should worry". Neuroscience and Biobehavioral Reviews 33 (6): 793–806. 2009. doi:10.1016/j.neubiorev.2009.01.001. PMID 19428492.
- ↑ Nkondjock A (May 2009). "Coffee consumption and the risk of cancer: an overview". Cancer Lett. 277 (2): 121–5. doi:10.1016/j.canlet.2008.08.022. PMID 18834663.
- ↑ 107.0 107.1 Arab L (2010). "Epidemiologic evidence on coffee and cancer". Nutrition and Cancer 62 (3): 271–83. doi:10.1080/01635580903407122. PMID 20358464.
- ↑ "Caffeine intake and dementia: systematic review and meta-analysis". J. Alzheimers Dis. 20 (Suppl 1): S187–204. 2010. doi:10.3233/JAD-2010-091387. PMID 20182026.
- ↑ "Modulating Alzheimer's disease through caffeine: a putative link to epigenetics". J. Alzheimers Dis. 24 (2): 161–71. 2011. doi:10.3233/JAD-2011-110032. PMID 21427489.
- ↑ "Caffeine and coffee as therapeutics against Alzheimer's disease". J. Alzheimers Dis. 20 (Suppl 1): S117–26. 2010. doi:10.3233/JAD-2010-091249. PMID 20182037.
- ↑ "Long-term coffee consumption and risk of cardiovascular disease: a systematic review and a dose-response meta-analysis of prospective cohort studies.". Circulation 129 (6): 643–59. 11 February 2014. doi:10.1161/circulationaha.113.005925. PMID 24201300.
- ↑ van Dam RM (2008). "Coffee consumption and risk of type 2 diabetes, cardiovascular diseases, and cancer". Applied Physiology, Nutrition, and Metabolism 33 (6): 1269–1283. doi:10.1139/H08-120. PMID 19088789.
- ↑ "Habitual coffee consumption and risk of hypertension: a systematic review and meta-analysis of prospective observational studies". Am. J. Clin. Nutr. 93 (6): 1212–9. June 2011. doi:10.3945/ajcn.110.004044. PMID 21450934.
- ↑ "The effect of caffeine on intraocular pressure: a systematic review and meta-analysis". Graefes Arch. Clin. Exp. Ophthalmol. 249 (3): 435–42. March 2011. doi:10.1007/s00417-010-1455-1. PMID 20706731.
- ↑ "Coffee and liver diseases". Fitoterapia 81 (5): 297–305. 2010. doi:10.1016/j.fitote.2009.10.003. PMID 19825397.
- ↑ O'Connor A (2007). Never shower in a thunderstorm: surprising facts and misleading myths about our health and the world we live in (1st ed.). New York: Times Books. p. 144. ISBN 978-0-8050-8312-5. https://books.google.com/books?id=neuEbVUZik0C&pg=PA144. Retrieved 15 January 2014.
- ↑ "Treatment of acute migraine headache". Am Fam Physician 83 (3): 271–80. February 2011. PMID 21302868.
- ↑ Hackett PH (2010). "Caffeine at high altitude: java at base Camp". High Alt. Med. Biol. 11 (1): 13–7. doi:10.1089/ham.2009.1077. PMID 20367483.
- ↑ Merck Manuals EPHEDrine Last full review/revision January 2010
- ↑ Meyer, Jerrold S (21 November 2013). "3,4-methylenedioxymethamphetamine (MDMA): current perspectives". Substance Abuse and Rehabilitation 4: 83–99. doi:10.2147/SAR.S37258. ISSN 1179-8467. PMID 24648791.
- ↑ Nutt, David; King, Leslie A.; Saulsbury, William; Blakemore, Colin (24 March 2007). "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet 369 (9566): 1047–1053. doi:10.1016/S0140-6736(07)60464-4. ISSN 1474-547X. PMID 17382831.
- ↑ "Ecstasy 'no more dangerous than horse riding'". 7 February 2009. https://www.telegraph.co.uk/news/uknews/law-and-order/4537874/Ecstasy-no-more-dangerous-than-horse-riding.html.
- ↑ Simmler, L. D.; Buser, T. A.; Donzelli, M.; Schramm, Y; Dieu, L-H.; Huwyler, J.; Chaboz, S.; Hoener, M. C. et al. (2012). "Pharmacological characterization of designer cathinones in vitro". British Journal of Pharmacology 168 (2): 458–470. doi:10.1111/j.1476-5381.2012.02145.x. ISSN 0007-1188. PMID 22897747.
- ↑ US Patent 3478050 – 1-(3,4-methylenedioxy-phenyl)-2-pyrrolidino-alkanones
- ↑ "Abuse Of Fake 'Bath Salts' Sends Dozens To ER". KMBC.com. 23 December 2010. http://www.kmbc.com/news/26256067/detail.html.
- ↑ "MDPV Bath Salts Drug Over The Counter". http://healthybodydaily.com/dr-oz-in-case-you-missed-it/dr-oz-bath-salts-mdpv-bath-salts-drug-over-the-counter.
- ↑ Samantha Morgan (9 November 2010). "Parents cautioned against over the counter synthetic speed". NBC 33 News. http://www.nbc33tv.com/consumer-alert/parents-cautioned-against-over-the-counter-synthetic-speed.
- ↑ Kelsey Scram (6 January 2011). "Bath Salts Used to Get High". NBC 33 News. http://www.nbc33tv.com/news/bath-salts-used-to-get-high.
- ↑ Cumming, E. (22 April 2010). "Mephedrone: Chemistry lessons". The Daily Telegraph (London). https://www.telegraph.co.uk/health/7614099/Mephedrone-Chemistry-lessons.html.
- ↑ "Drugs crackdown hailed a success". BBC News. 8 March 2010. http://news.bbc.co.uk/1/hi/scotland/north_east/8555872.stm.
- ↑ "Cathinone neurotoxicity ("The "3Ms")". Curr Neuropharmacol 13 (1): 21–5. January 2015. doi:10.2174/1570159X13666141210225009. PMID 26074741.
- ↑ "Neurotoxicity Induced by Mephedrone: An up-to-date Review". Curr Neuropharmacol 15 (5): 738–749. 2017. doi:10.2174/1570159X14666161130130718. PMID 27908258.
- ↑ "Mephedrone and MDMA: A comparative review". Brain Res 1735: 146740. May 2020. doi:10.1016/j.brainres.2020.146740. PMID 32087112.
- ↑ 134.0 134.1 134.2 "15". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. 2009. p. 370. ISBN 978-0-07-148127-4. "Unlike cocaine and amphetamine, methamphetamine is directly toxic to midbrain dopamine neurons."
- ↑ 135.0 135.1 135.2 135.3 135.4 135.5 135.6 "Desoxyn Prescribing Information". United States Food and Drug Administration. December 2013. http://www.accessdata.fda.gov/drugsatfda_docs/label/2013/005378s028lbl.pdf.
- ↑ 136.0 136.1 136.2 136.3 "Methamphetamine toxicity and messengers of death". Brain Res. Rev. 60 (2): 379–407. May 2009. doi:10.1016/j.brainresrev.2009.03.002. PMID 19328213. "Neuroimaging studies have revealed that METH can indeed cause neurodegenerative changes in the brains of human addicts (Aron and Paulus, 2007; Chang et al., 2007). These abnormalities include persistent decreases in the levels of dopamine transporters (DAT) in the orbitofrontal cortex, dorsolateral prefrontal cortex, and the caudate-putamen (McCann et al., 1998, 2008; Sekine et al., 2003; Volkow et al., 2001a, 2001c). The density of serotonin transporters (5-HTT) is also decreased in the midbrain, caudate, putamen, hypothalamus, thalamus, the orbitofrontal, temporal, and cingulate cortices of METH-dependent individuals (Sekine et al., 2006) ...
Neuropsychological studies have detected deficits in attention, working memory, and decision-making in chronic METH addicts ...
There is compelling evidence that the negative neuropsychiatric consequences of METH abuse are due, at least in part, to drug-induced neuropathological changes in the brains of these METH-exposed individuals ...
Structural magnetic resonance imaging (MRI) studies in METH addicts have revealed substantial morphological changes in their brains. These include loss of gray matter in the cingulate, limbic, and paralimbic cortices, significant shrinkage of hippocampi, and hypertrophy of white matter (Thompson et al., 2004). In addition, the brains of METH abusers show evidence of hyperintensities in white matter (Bae et al., 2006; Ernst et al., 2000), decreases in the neuronal marker, N-acetylaspartate (Ernst et al., 2000; Sung et al., 2007), reductions in a marker of metabolic integrity, creatine (Sekine et al., 2002) and increases in a marker of glial activation, myoinositol (Chang et al., 2002; Ernst et al., 2000; Sung et al., 2007; Yen et al., 1994). Elevated choline levels, which are indicative of increased cellular membrane synthesis and turnover are also evident in the frontal gray matter of METH abusers (Ernst et al., 2000; Salo et al., 2007; Taylor et al., 2007).". - ↑ 137.0 137.1 "Hippocampus norepinephrine, caudate dopamine and serotonin, and behavioral responses to the stereoisomers of amphetamine and methamphetamine". J. Neurosci. 15 (2): 1308–1317. February 1995. doi:10.1523/JNEUROSCI.15-02-01308.1995. PMID 7869099.
- ↑ 138.0 138.1 138.2 "Human pharmacology of the methamphetamine stereoisomers". Clin. Pharmacol. Ther. 80 (4): 403–420. October 2006. doi:10.1016/j.clpt.2006.06.013. PMID 17015058.
- ↑ 139.0 139.1 "San Francisco Meth Zombies". Drugs, Inc. Season 4. Episode 1. 11 August 2013. 43 minutes in. ASIN B00EHAOBAO. National Geographic Channel. Archived from the original on 8 July 2016.
- ↑ United Nations Office on Drugs and Crime (2007). Preventing Amphetamine-type Stimulant Use Among Young People: A Policy and Programming Guide. New York: United Nations. ISBN 978-92-1-148223-2. http://www.unodc.org/pdf/youthnet/ATS.pdf. Retrieved 11 November 2013.
- ↑ "List of psychotropic substances under international control". International Narcotics Control Board. United Nations. August 2003. http://www.incb.org/pdf/e/list/green.pdf.
- ↑ "CFR TITLE 21: DRUGS FOR HUMAN USE: PART 341 – COLD, COUGH, ALLERGY, BRONCHODILATOR, AND ANTIASTHMATIC DRUG PRODUCTS FOR OVER-THE-COUNTER HUMAN USE". April 2015. https://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/cfrsearch.cfm?fr=341.80. "Topical nasal decongestants --(i) For products containing levmetamfetamine identified in 341.20(b)(1) when used in an inhalant dosage form. The product delivers in each 800 milliliters of air 0.04 to 0.150 milligrams of levmetamfetamine."
- ↑ "Levomethamphetamine". https://pubchem.ncbi.nlm.nih.gov/summary/summary.cgi?cid=36604#section=Identification.
- ↑ "A review of the clinical pharmacology of methamphetamine". Addiction 104 (7): 1085–1099. July 2009. doi:10.1111/j.1360-0443.2009.02564.x. PMID 19426289.
- ↑ "Meta-analysis of functional magnetic resonance imaging studies of inhibition and attention in attention-deficit/hyperactivity disorder: exploring task-specific, stimulant medication, and age effects". JAMA Psychiatry 70 (2): 185–198. February 2013. doi:10.1001/jamapsychiatry.2013.277. PMID 23247506.
- ↑ "Effect of psychostimulants on brain structure and function in ADHD: a qualitative literature review of magnetic resonance imaging-based neuroimaging studies". J. Clin. Psychiatry 74 (9): 902–917. September 2013. doi:10.4088/JCP.12r08287. PMID 24107764.
- ↑ Ellison, Gaylord D.; Eison, Michael S. (1983). "Continuous amphetamine intoxication: An animal model of the acute psychotic episode". Psychological Medicine 13 (4): 751–761. doi:10.1017/S003329170005145X. PMID 6320247. https://www.cambridge.org/core/journals/psychological-medicine/article/continuous-amphetamine-intoxication-an-animal-model-of-the-acute-psychotic-episode/7DEB3BCC38395608F1C4FE87529D4C8F.
- ↑ "Efectos psicológicos del consumo de la cocaína" (in es). 2020. https://www.avancepsicologos.com/efectos-psicologicos-del-consumo-de-la-cocaina/.
- ↑ AJ Giannini; WC Price (1986). "Contemporary drugs of abuse". American Family Physician 33: 207–213.
- ↑ Talhouth, Reinskje; Opperhuizen, Antoon; van Amsterdam G. C., Jan (October 2007). "Role of acetaldehyde in tobacco smoke addiction". European Neuropsychopharmacology 17 (10): 627–636. doi:10.1016/j.euroneuro.2007.02.013. PMID 17382522.
- ↑ Nutt, David J.; King, Leslie A.; Phillips, Lawrence D. (6 November 2010). "Drug harms in the UK: a multicriteria decision analysis". Lancet 376 (9752): 1558–1565. doi:10.1016/S0140-6736(10)61462-6. ISSN 1474-547X. PMID 21036393.
- ↑ Flavahan NA (April 2005). "Phenylpropanolamine constricts mouse and human blood vessels by preferentially activating alpha2-adrenoceptors". Journal of Pharmacology and Experimental Therapeutics 313 (1): 432–9. doi:10.1124/jpet.104.076653. PMID 15608085.
- ↑ "Advisories, Warnings and Recalls – 2001". Health Canada. 7 January 2009. http://www.hc-sc.gc.ca/ahc-asc/media/advisories-avis/2001-eng.php.
- ↑ "Drugs Banned in India". Directorate General of Health Services, Ministry of Health and Family Welfare, Government of India. Central Drugs Standard Control Organization. http://www.cdsco.nic.in/html/Drugsbanned.html.
- ↑ "Lisdexamfetamine: MedlinePlus Drug Information" (in en). https://medlineplus.gov/druginfo/meds/a607047.html.
- ↑ "Lisdexamfetamine Dimesylate Monograph for Professionals". American Society of Health-System Pharmacists. https://www.drugs.com/monograph/lisdexamfetamine-dimesylate.html.
- ↑ Hunter Gillies; Wayne E. Derman; Timothy D. Noakes; Peter Smith; Alicia Evans; Gary Gabriels (1 December 1996). "Pseudoephedrine is without ergogenic effects during prolonged exercise". Journal of Applied Physiology 81 (6): 2611–2617. doi:10.1152/jappl.1996.81.6.2611. PMID 9018513.
- ↑ Hodges, K; Hancock S; Currel K; Hamilton B; Jeukendrup AE (Feb 2006). "Pseudoephedrine enhances performance in 1500-m runners". Medicine and Science in Sports and Exercise 38 (2): 329–33. doi:10.1249/01.mss.0000183201.79330.9c. PMID 16531903.
- ↑ Dickens, Charles (1856). "The Orsons of East Africa". Household Words: A Weekly Journal, Volume 14. Bradbury & Evans. p. 176. https://books.google.com/books?id=EdUnAQAAIAAJ&pg=PA176. Retrieved 7 January 2014.
 (Free eBook)
(Free eBook)
- ↑ 160.0 160.1 Al-Mugahed, Leen (October 2008). "Khat chewing in Yemen: turning over a new leaf – Khat chewing is on the rise in Yemen, raising concerns about the health and social consequences". World Health Organization. https://www.who.int/bulletin/volumes/86/10/08-011008/en/.
- ↑ 161.0 161.1 "Development of a rational scale to assess the harm of drugs of potential misuse". Lancet 369 (9566): 1047–53. March 2007. doi:10.1016/S0140-6736(07)60464-4. PMID 17382831.
- ↑ Haight-Ashbury Free Medical Clinic, Journal of psychoactive drugs, Volume 41, (Haight-Ashbury Publications: 2009), p.3.
- ↑ Kredlow, M Alexandra; Keshishian, Ani; Oppenheimer, Sarah; Otto, Michael W (1 September 2019). "The Efficacy of Modafinil as a Cognitive Enhancer: A Systematic Review and Meta-Analysis". Journal of Clinical Psychopharmacology 39 (5): 455–461. doi:10.1097/jcp.0000000000001085. PMID 31433334.
- ↑ "A practical guide to the therapy of narcolepsy and hypersomnia syndromes". Neurotherapeutics 9 (4): 739–752. October 2012. doi:10.1007/s13311-012-0150-9. PMID 23065655.
- ↑ 165.0 165.1 "Provigil: Prescribing information". United States Food and Drug Administration. January 2015. http://www.accessdata.fda.gov/drugsatfda_docs/label/2015/020717s037s038lbl.pdf.
- ↑ "A Review of Pharmacologic Neurostimulant Use During Rehabilitation and Recovery After Brain Injury". Ann Pharmacother 55 (10): 1254–1266. October 2021. doi:10.1177/1060028020983607. PMID 33435717.
- ↑ "Practical use and risk of modafinil, a novel waking drug". Environmental Health and Toxicology 27: e2012007. 2012. doi:10.5620/eht.2012.27.e2012007. PMID 22375280.
- ↑ "Subjective effects of modafinil, a new central adrenergic stimulant in healthy volunteers: a comparison with amphetamine, caffeine and placebo". European Psychiatry 8 (4): 201–208. 1993. doi:10.1017/S0924933800002923.
- ↑ "Does modafinil produce euphoria?". The American Journal of Psychiatry 163 (6): 1109. June 2006. doi:10.1176/ajp.2006.163.6.1109. PMID 16741217.
- ↑ "Modafinil". StatPearls. Treasure Island (FL): StatPearls Publishing. February 2022. Template:NCBIBook.
- ↑ "Pitolisant". LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases. 24 January 2012. http://www.ncbi.nlm.nih.gov/books/NBK573784/.
- ↑ "Central Nervous System (CNS) Stimulants". LiverTox: Clinical and Research Information on Drug-Induced Liver Injury. National Institute of Diabetes and Digestive and Kidney Diseases. 22 January 2012. http://www.ncbi.nlm.nih.gov/books/NBK548702/.
- ↑ "Pitolisant Uses, Side Effects & Warnings". https://www.drugs.com/mtm/pitolisant.html.
- ↑ "List of CNS stimulants + Uses & Side Effects". https://www.drugs.com/drug-class/cns-stimulants.html.
- ↑ 175.0 175.1 175.2 175.3 "Pitolisant: A Review in Narcolepsy with or without Cataplexy". CNS Drugs 34 (2): 207–218. February 2020. doi:10.1007/s40263-020-00703-x. PMID 31997137.
- ↑ 176.0 176.1 Kollb-Sielecka, Marta; Demolis, Pierre; Emmerich, Joseph; Markey, Greg; Salmonson, Tomas; Haas, Manuel (1 May 2017). "The European Medicines Agency review of pitolisant for treatment of narcolepsy: summary of the scientific assessment by the Committee for Medicinal Products for Human Use". Sleep Medicine 33: 125–129. doi:10.1016/j.sleep.2017.01.002. PMID 28449891.
- ↑ 177.0 177.1 "Pitolisant (Wakix) for Narcolepsy". JAMA 326 (11): 1060–1061. 21 September 2021. doi:10.1001/jama.2021.1349. PMID 34546302.
- ↑ "Evaluating pitolisant as a narcolepsy treatment option". Expert Opinion on Pharmacotherapy 22 (2): 155–162. February 2021. doi:10.1080/14656566.2020.1817387. PMID 32941089.
- ↑ "Identification of two H3-histamine receptor subtypes". Molecular Pharmacology 38 (5): 610–613. November 1990. PMID 2172771. https://molpharm.aspetjournals.org/content/38/5/610.
- ↑ "pitolisant, a novel histamine-3 receptor competitive antagonist, and inverse agonist, in the treatment of excessive daytime sleepiness in adult patients with narcolepsy". Health Psychology Research 10 (3): 34222. 30 May 2022. doi:10.52965/001c.34222. PMID 35774905.
- ↑ "Addictiveness of central stimulants". Advances in Alcohol & Substance Abuse 9 (1–2): 9–26. 1990. doi:10.1300/J251v09n01_02. PMID 1974121.
- ↑ Huskinson, Sally L.; Naylor, Jennifer E.; Rowlett, James K.; Freeman, Kevin B. (7 January 2017). "Predicting abuse potential of stimulants and other dopaminergic drugs: Overview and recommendations". Neuropharmacology 87: 66–80. doi:10.1016/j.neuropharm.2014.03.009. ISSN 0028-3908. PMID 24662599.
- ↑ 183.0 183.1 Stoops, William W. (7 January 2017). "Reinforcing Effects of Stimulants in Humans: Sensitivity of Progressive-Ratio Schedules". Experimental and Clinical Psychopharmacology 16 (6): 503–512. doi:10.1037/a0013657. ISSN 1064-1297. PMID 19086771.
- ↑ Minozzi, Silvia; Saulle, Rosella; De Crescenzo, Franco; Amato, Laura (29 September 2016). "Psychosocial interventions for psychostimulant misuse". The Cochrane Database of Systematic Reviews 2016 (9): CD011866. doi:10.1002/14651858.CD011866.pub2. ISSN 1469-493X. PMID 27684277.
- ↑ AJ Giannini. Drug Abuse. Los Angeles, Health Information Press, 1999, pp.203–208
External links
- "Long Island Council on Alcohol & Drug Dependence – About Drugs – Stimulants". http://www.licadd.org/aboutdrugs.htm.
- "Online – Publications – Drugs of Abuse – Stimulants". http://ncadistore.samhsa.gov/catalog/results.aspx?h=drugs&topic=68.
- Asia & Pacific Amphetamine-Type Stimulants Information Centre (APAIC)
 |
 KSF
KSF