Typical antipsychotic
Topic: Chemistry
 From HandWiki - Reading time: 11 min
From HandWiki - Reading time: 11 min
| Typical antipsychotic | |
|---|---|
| Drug class | |
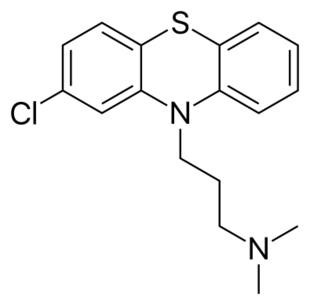 Skeletal formula of chlorpromazine, the first neuroleptic drug | |
| Synonyms | First generation antipsychotics, conventional antipsychotics, classical neuroleptics, traditional antipsychotics, major tranquilizers |

Typical antipsychotics (also known as major tranquilizers, and first generation antipsychotics) are a class of antipsychotic drugs first developed in the 1950s and used to treat psychosis (in particular, schizophrenia). Typical antipsychotics may also be used for the treatment of acute mania, agitation, and other conditions. The first typical antipsychotics to come into medical use were the phenothiazines, namely chlorpromazine which was discovered serendipitously.[1] Another prominent grouping of antipsychotics are the butyrophenones, an example of which is haloperidol. The newer, second-generation antipsychotics, also known as atypical antipsychotics, have largely supplanted the use of typical antipsychotics as first-line agents due to the higher risk of movement disorders in the latter.
Both generations of medication tend to block receptors in the brain's dopamine pathways, but atypicals at the time of marketing were claimed to differ from typical antipsychotics in that they are less likely to cause extrapyramidal symptoms (EPS), which include unsteady Parkinson's disease-type movements, internal restlessness, and other involuntary movements (e.g. tardive dyskinesia, which can persist after stopping the medication).[2] More recent research has demonstrated the side effect profile of these drugs is similar to older drugs, causing the leading medical journal The Lancet to write in its editorial "the time has come to abandon the terms first-generation and second-generation antipsychotics, as they do not merit this distinction."[3] While typical antipsychotics are more likely to cause EPS, atypicals are more likely to cause adverse metabolic effects, such as weight gain and increase the risk for type II diabetes.[4]
Clinical uses
Typical antipsychotics block the dopamine 2 receptor (D2) receptor, causing a tranquilizing effect.[5] It is thought that 60–80% of D2 receptors need to be occupied for antipsychotic effect.[5] For reference, the typical antipsychotic haloperidol tends to block about 80% of D2 receptors at doses ranging from 2 to 5 mg per day.[5] On the aggregate level, no typical antipsychotic is more effective than any other, though people will vary in which antipsychotic they prefer to take based on individual differences in tolerability and effectiveness.[5] Typical antipsychotics can be used to treat, e.g., schizophrenia or severe agitation.[5] Haloperidol, due to the availability of a rapid-acting injectable formulation and decades of use, remains the most commonly used antipsychotic for treating severe agitation in the emergency department setting.[5]
Adverse effects
Adverse effects vary among the various agents in this class of medications, but common effects include: dry mouth, muscle stiffness, muscle cramping, tremors, EPS and weight gain. EPS refers to a cluster of symptoms consisting of akathisia, parkinsonism, and dystonia. Anticholinergics such as benztropine and diphenhydramine are commonly prescribed to treat the EPS. 4% of users develop rabbit syndrome while on typical antipsychotics.[6]
There is a risk of developing a serious condition called tardive dyskinesia as a side effect of antipsychotics, including typical antipsychotics. The risk of developing tardive dyskinesia after chronic typical antipsychotic usage varies on several factors, such as age and gender, as well as the specific antipsychotic used. The commonly reported incidence of TD among younger patients is about 5% per year. Among older patients incidence rates as high as 20% per year have been reported. The average prevalence is approximately 30%.[7] There are few treatments that have consistently been shown to be effective for the treatment of tardive dyskinesia, though an VMAT2 inhibitor like valbenazine may help.[8] The atypical antipsychotic clozapine has also been suggested as an alternative antipsychotic for patients experiencing tardive dyskinesia.[9] Tardive dyskinesia may reverse upon discontinuation of the offending agent or it may be irreversible, withdrawal may also make tardive dyskinesia more severe.[10]
Neuroleptic malignant syndrome (NMS) is a rare, but potentially fatal side effect of antipsychotic treatment. NMS is characterized by fever, muscle rigidity, autonomic dysfunction, and altered mental status. Treatment includes discontinuation of the offending agent and supportive care.
The role of typical antipsychotics has come into question recently as studies have suggested that typical antipsychotics may increase the risk of death in elderly patients. A 2005 retrospective cohort study from the New England Journal of Medicine showed an increase in risk of death with the use of typical antipsychotics that was on par with the increase shown with atypical antipsychotics.[11] This has led some to question the common use of antipsychotics for the treatment of agitation in the elderly, particularly with the availability of alternatives such as mood stabilizing and antiepileptic drugs.
Potency
Traditional antipsychotics are classified as high-potency, mid-potency, or low-potency based on their potency for the D2 receptor:
| Potency | Examples | Adverse effect profile |
| high | fluphenazine and haloperidol | more extrapyramidal side effects (EPS) and less antihistaminic effects (e.g. sedation), alpha adrenergic antagonism (e.g. orthostatic hypotension), and anticholinergic effects (e.g. dry mouth) |
| middle | perphenazine and loxapine | intermediate D2 affinity, with more off-target effects than high-potency agents |
| low | chlorpromazine | less risk of EPS but more antihistaminic effects, alpha adrenergic antagonism, and anticholinergic effects |
Prochlorperazine (Compazine, Buccastem, Stemetil) and Pimozide (Orap) are less commonly used to treat psychotic states, and so are sometimes excluded from this classification.[12]
A related concept to D2 potency is the concept of "chlorpromazine equivalence", which provides a measure of the relative effectiveness of antipsychotics.[13][14] The measure specifies the amount (mass) in milligrams of a given drug that must be administered in order to achieve desired effects equivalent to those of 100 milligrams of chlorpromazine.[15] Another method is "defined daily dose" (DDD), which is the assumed average dose of an antipsychotic that an adult would receive during long-term treatment.[15] DDD is primarily used for comparing the utilization of antipsychotics (e.g. in an insurance claim database), rather than comparing therapeutic effects between antipsychotics.[15] Maximum dose methods are sometimes used to compare between antipsychotics as well.[15] It is important to note that these methods do not generally account for differences between the tolerability (i.e. the risk of side effects) or the safety between medications.[15]
For a list of typical antipsychotics organized by potency, see below:
Low potency
- Chlorpromazine
- Chlorprothixene
- Levomepromazine
- Mesoridazine
- Periciazine
- Promazine
- Thioridazine† (withdrawn by brand-name manufacturer and most countries)
Medium potency
- Loxapine
- Molindone
- Perphenazine
- Thiothixene
High potency
- Droperidol
- Flupentixol
- Fluphenazine
- Haloperidol
- Pimozide
- Prochlorperazine
- Thioproperazine
- Trifluoperazine
- Zuclopenthixol
Where: † indicates products that have since been discontinued.[16]
Long-acting injectables
Some typical antipsychotics have been formulated as a long-acting injectable (LAI), or "depot", formulation. Depot injections are also used on persons under involuntary commitment to force compliance with a court treatment order when the person would refuse to take daily oral medication. This has the effect of dosing a person who doesn't consent to take the drug. The United Nations Special Rapporteur On Torture has classified this as a human rights violation and cruel or inhuman treatment.[17]
The first LAI antipsychotics (often referred to as simply "LAIs") were the typical antipsychotics fluphenazine and haloperidol.[18] Both fluphenazile and haloperidol are formulated as decanoates, referring to the attachment of a decanoic acid group to the antipsychotic molecule.[18] These are then dissolved in an organic oil.[18] Together, these modifications prevent the active medications from being released immediately upon injection, attaining a slow release of the active medications (note, though, that the fluphenazine decanoate product is unique for reaching peak fluphenazine blood levels within 24 hours after administration[19]).[18] Fluphenazine decanoate can be administered every 7 to 21 days (usually every 14 to 28 days),[19] while haloperidol decanoate can be administered every 28 days, though some people receive more or less frequent injections.[18] If a scheduled injection of either haloperidol decanoate or fluphenazine decanoate is missed, recommendations for administering make-up injectable dose(s) or providing antipsychotics to be taken by mouth vary by, e.g., how long ago the last injection was and how many previous injections the person has received (i.e., if steady state levels of the medication have been reached or not).[19]
Both of the typical antipsychotic LAIs are inexpensive in comparison to the atypical LAIs.[18] Doctors usually prefer atypical LAIs over typical LAIs due to the differences in adverse effects between typical and atypical antipsychotics in general.[19]
History

The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic after an initial report in 1952.[5] It was first used in psychiatric institutions because of its powerful tranquilizing effect; at the time it was advertised as a "pharmacological lobotomy".[21] (Note that "tranquilizing" here only refers to changes in external behavior, while the experience a person has internally may be one of increased agitation but inability to express it.)[22]
Until the 1970s there was considerable debate within psychiatry on the most appropriate term to use to describe the new drugs.[23] In the late 1950s the most widely used term was "neuroleptic", followed by "major tranquilizer" and then "ataraxic".[23] The word neuroleptic was coined in 1955 by Delay and Deniker after their discovery (1952) of the antipsychotic effects of chlorpromazine.[23] It is derived from the Greek: "νεῦρον" (neuron, originally meaning "sinew" but today referring to the nerves) and "λαμβάνω" (lambanō, meaning "take hold of"). Thus, the word means taking hold of one's nerves. It was often taken to refer also to common effects such as reduced activity in general, as well as lethargy and impaired motor control. Although these effects are unpleasant and harmful, they were, along with akathisia, considered a reliable sign that the drug was working.[21] These terms have been largely replaced by the term "antipsychotic" in medical and advertising literature, which refers to the medication's more-marketable effects.[23]
See also
- Tranquilizer
- Atypical antipsychotic
- Tardive dyskinesia
- Schizophrenia
- Bipolar disorder
- Psychiatric survivors' movement
References
- ↑ "A history of antipsychotic drug development". Comprehensive Psychiatry 40 (6): 407–14. 1999. doi:10.1016/s0010-440x(99)90082-2. PMID 10579370.
- ↑ "A roadmap to key pharmacologic principles in using antipsychotics". Primary Care Companion to the Journal of Clinical Psychiatry 9 (6): 444–54. 2007. doi:10.4088/PCC.v09n0607. PMID 18185824.
- ↑ "The spurious advance of antipsychotic drug therapy". Lancet 373 (9657): 4–5. January 2009. doi:10.1016/S0140-6736(08)61765-1. PMID 19058841. http://www.thelancet.com/journals/lancet/issue/current?tab=past. Retrieved 2023-03-02.
- ↑ "Not found". http://www.rcpsych.ac.uk/healthadvice/treatmentswellbeing/antipsychoticmedication.aspx%7B%7Bfull%7D%7D.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 Schatzberg's Manual of Clinical Psychopharmacology (Ninth ed.). American Psychiatric Association Publishing. 2019. ISBN 978-1-61537-230-0. https://www.appi.org/Products/Psychopharmacology/Schatzbergs-Manual-of-Clinical-Psychopharmacology.
- ↑ "Prevalence of the rabbit syndrome". The American Journal of Psychiatry 143 (5): 656–7. May 1986. doi:10.1176/ajp.143.5.656. PMID 2870650.
- ↑ "Tardive dyskinesias and antipsychotics: a review". European Psychiatry 17 (3): 129–38. May 2002. doi:10.1016/S0924-9338(02)00647-8. PMID 12052573.
- ↑ Office of the Commissioner (24 March 2020). "FDA approves first drug to treat tardive dyskinesia" (in en). https://www.fda.gov/news-events/press-announcements/fda-approves-first-drug-treat-tardive-dyskinesia.
- ↑ "Clozapine and tardive dyskinesia in patients with schizophrenia: A systematic review". Journal of Psychopharmacology 33 (10): 1187–1198. October 2019. doi:10.1177/0269881119862535. PMID 31347436.
- ↑ "Tardive dyskinesia: MedlinePlus Medical Encyclopedia". https://medlineplus.gov/ency/article/000685.htm.[full citation needed]
- ↑ "Risk of death in elderly users of conventional vs. atypical antipsychotic medications". The New England Journal of Medicine 353 (22): 2335–41. December 2005. doi:10.1056/NEJMoa052827. PMID 16319382.
- ↑ Gitlin, Michael J. (1996). The psychotherapist's guide to psychopharmacology. New York: Free Press. p. 392. ISBN 0-684-82737-9.
- ↑ "Chlorpromazine equivalent doses for the newer atypical antipsychotics". The Journal of Clinical Psychiatry 64 (6): 663–7. June 2003. doi:10.4088/JCP.v64n0607. PMID 12823080.
- ↑ "Chlorpromazine equivalents versus defined daily doses: how to compare antipsychotic drug doses?". Journal of Clinical Psychopharmacology 23 (6): 657–9. December 2003. doi:10.1097/01.jcp.0000096247.29231.3a. PMID 14624195.
- ↑ 15.0 15.1 15.2 15.3 15.4 "How to compare doses of different antipsychotics: a systematic review of methods". Schizophrenia Research 149 (1–3): 141–8. September 2013. doi:10.1016/j.schres.2013.06.030. PMID 23845387.
- ↑ Martindale: The Complete Drug Reference. The Royal Pharmaceutical Society of Great Britain. 2013. http://www.medicinescomplete.com/mc/martindale/current/. Retrieved 2 November 2013.
- ↑ https://www.madinamerica.com/wp-content/uploads/2013/03/torture.pdf [bare URL PDF]
- ↑ 18.0 18.1 18.2 18.3 18.4 18.5 "When and how to use long-acting injectable antipsychotics" (in en). Current Psychiatry 11 (8): 40–43. 2012. https://www.mdedge.com/psychiatry/article/64796/schizophrenia-other-psychotic-disorders/when-and-how-use-long-acting.
- ↑ 19.0 19.1 19.2 19.3 "Long-acting injectable antipsychotics: What to do about missed doses" (in en). Current Psychiatry 17 (7): 10–12, 14–19, 56. 2018. https://www.mdedge.com/psychiatry/article/168776/schizophrenia-other-psychotic-disorders/long-acting-injectable.
- ↑ The text reads: "When the patient lashes out against 'them' - THORAZINE (brand of chlorpromazine) quickly puts an end to his violent outburst. 'Thorazine' is especially effective when the psychotic episode is triggered by delusions or hallucinations. At the outset of treatment, Thorazine's combination of antipsychotic and sedative effects provides both emotional and physical calming. Assaultive or destructive behavior is rapidly controlled. As therapy continues, the initial sedative effect gradually disappears. But the antipsychotic effect continues, helping to dispel or modify delusions, hallucinations and confusion, while keeping the patient calm and approachable. SMITH KLINE AND FRENCH LABORATORIES leaders in psychopharmaceutical research."
- ↑ 21.0 21.1 "The introduction of chlorpromazine in Belgium and the Netherlands (1951-1968); tango between old and new treatment features". Studies in History and Philosophy of Biological and Biomedical Sciences 42 (4): 443–52. December 2011. doi:10.1016/j.shpsc.2011.05.003. PMID 22035718. http://orbilu.uni.lu/handle/10993/2251.
- ↑ Muench, John (1 March 2010). "Adverse Effects Of Antipsychotics". American Family Physician 81 (5): 617–622. https://www.aafp.org/afp/2010/0301/p617.html. Retrieved 23 March 2021.
- ↑ 23.0 23.1 23.2 23.3 "What's in a name? The evolution of the nomenclature of antipsychotic drugs". Journal of Psychiatry & Neuroscience 27 (3): 168–75. May 2002. PMID 12066446.
 |
 KSF
KSF