Appendicitis
Topic: Medicine
 From HandWiki - Reading time: 30 min
From HandWiki - Reading time: 30 min
Appendicitis is inflammation of the appendix.[1] Symptoms commonly include right lower abdominal pain, nausea, vomiting, fever and decreased appetite.[1] However, approximately 40% of people do not have these typical symptoms.[1] Severe complications of a ruptured appendix include widespread, painful inflammation of the inner lining of the abdominal wall and sepsis.[2]
Appendicitis is primarily caused by a blockage of the hollow portion in the appendix.[3] This blockage typically results from a faecolith, a calcified "stone" made of feces.[4] Some studies show a correlation between appendicoliths and disease severity.[5] Other factors such as inflamed lymphoid tissue from a viral infection, intestinal parasites, gallstone, or tumors may also lead to this blockage.[4] When the appendix becomes blocked, it experiences increased pressure, reduced blood flow, and bacterial growth, resulting in inflammation.[4][6] This combination of factors causes tissue injury and, ultimately, tissue death.[7] If this process is left untreated, it can lead to the appendix rupturing, which releases bacteria into the abdominal cavity, potentially leading to severe complications.[7][8]
The diagnosis of appendicitis is largely based on the person's signs and symptoms.[6] In cases where the diagnosis is unclear, close observation, medical imaging, and laboratory tests can be helpful.[9] The two most commonly used imaging tests for diagnosing appendicitis are ultrasound and computed tomography (CT scan).[9] CT scan is more accurate than ultrasound in detecting acute appendicitis.[10] However, ultrasound may be preferred as the first imaging test in children and pregnant women because of the risks associated with radiation exposure from CT scans.[9] Although ultrasound may aid in diagnosis, its main role is in identifying important differentials, such as ovarian pathology in females or mesenteric adenitis in children.
File:En.Wikipedia-VideoWiki-Appendicitis.webm The standard treatment for acute appendicitis involves the surgical removal of the inflamed appendix.[4][6] This procedure can be performed either through an open incision in the abdomen (laparotomy) or using minimally invasive techniques with small incisions and cameras (laparoscopy). Surgery is essential to reduce the risk of complications or potential death associated with the rupture of the appendix.[2] Antibiotics may be equally effective in certain cases of non-ruptured appendicitis,[11][12][13] but 31% will undergo appendectomy within one year.[14] It is one of the most common and significant causes of sudden abdominal pain. In 2015, approximately 11.6 million cases of appendicitis were reported, resulting in around 50,100 deaths worldwide.[15][16] In the United States, appendicitis is one of the most common causes of sudden abdominal pain requiring surgery.[1] Annually, more than 300,000 individuals in the United States undergo surgical removal of their appendix.[17]
Signs and symptoms
The presentation of acute appendicitis includes acute abdominal pain, nausea, vomiting, and fever. As the appendix becomes more swollen and inflamed, it begins to irritate the adjoining abdominal wall. This leads the pain to localize at the right lower quadrant. This classic migration of pain may not appear in children under three years. This pain can be triggered by a sharp pain feeling. Pain from appendicitis may begin as dull pain around the navel. After several hours, the pain usually migrates towards the right lower quadrant, where it becomes localized. Symptoms include localized findings in the right iliac fossa. The abdominal wall becomes very sensitive to gentle pressure (palpation). There is pain in the sudden release of deep tension in the lower abdomen (Blumberg's sign). If the appendix is retrocecal (localized behind the cecum), even deep pressure in the right lower quadrant may fail to elicit tenderness (silent appendix). This is because the cecum, distended with gas, protects the inflamed appendix from pressure. Similarly, if the appendix lies entirely within the pelvis, there is typically a complete absence of abdominal rigidity. In such cases, a digital rectal examination elicits tenderness in the rectovesical pouch. Coughing causes point tenderness in this area (McBurney's point), called Dunphy's sign.
Causes
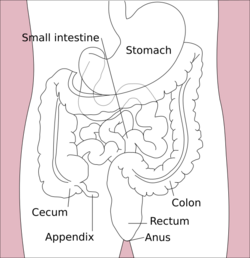

Acute appendicitis seems to be the result of a primary obstruction of the appendix.[18][3] Once this obstruction occurs, the appendix becomes filled with mucus and swells. This continued production of mucus leads to increased pressures within the lumen and the walls of the appendix. The increased pressure results in thrombosis and occlusion of the small vessels, and stasis of lymphatic flow. At this point, spontaneous recovery rarely occurs. As the occlusion of blood vessels progresses, the appendix becomes ischemic and then necrotic. As bacteria begin to leak out through the dying walls, pus forms within and around the appendix (suppuration). The result is appendiceal rupture (a 'burst appendix') causing peritonitis, which may lead to sepsis and in rare cases, death. These events are responsible for the slowly evolving abdominal pain and other commonly associated symptoms.[7]
The causative agents include bezoars, foreign bodies, trauma,[19][20] lymphadenitis and, most commonly, calcified fecal deposits that are known as appendicoliths or fecaliths.[21][22] The occurrence of obstructing fecaliths has attracted attention since their presence in people with appendicitis is higher in developed than in developing countries.[23] In addition, an appendiceal fecalith is commonly associated with complicated appendicitis.[24] Fecal stasis and arrest may play a role, as demonstrated by people with acute appendicitis having fewer bowel movements per week compared with healthy controls.[22][25]
The occurrence of a fecalith in the appendix was thought to be attributed to a right-sided fecal retention reservoir in the colon and a prolonged transit time. However, a prolonged transit time was not observed in subsequent studies.[26] Diverticular disease and adenomatous polyps were historically unknown and colon cancer was exceedingly rare in communities where appendicitis itself was rare or absent, such as various African communities. Studies have implicated a transition to a Western diet lower in fiber in rising frequencies of appendicitis as well as the other aforementioned colonic diseases in these communities.[27][28] And acute appendicitis has been shown to occur antecedent to cancer in the colon and rectum.[29] Several studies offer evidence that a low fiber intake is involved in the pathogenesis of appendicitis.[30][31][32] This low intake of dietary fiber is in accordance with the occurrence of a right-sided fecal reservoir and the fact that dietary fiber reduces transit time.[33]
Diagnosis
Template:ImageStackPopup The physician will ask questions to get the health history, assess the patient's symptoms, do a complete physical exam, and order both laboratory and imaging tests.[34] Appendicitis symptoms fall into two categories, typical and atypical.[35]
Typical appendicitis is characterized by a migratory right iliac fossa pain associated with nausea, and anorexia, which can occur with or without vomiting and localized muscle stiffness/ generalized guarding.[35] It is possible the pain could localize to the left lower quadrant in people with situs inversus totalis.[36] The combination of migrated umbilical pain to the right lower quadrant, loss of appetite for food, nausea, unsustained vomiting, and mild fever is classic.[35]
Atypical histories lack this typical progression and may include pain in the right lower quadrant as an initial symptom. Irritation of the peritoneum (inside lining of the abdominal wall) can lead to increased pain on movement, or jolting, for example going over speed bumps.[37] Atypical histories often require imaging with ultrasound or CT scanning.[2]
Signs
During the early stages of appendicitis diagnosis, it is common for physical exams to present inconspicuous findings. Signs of inflammation become noticeable as the disease progresses. These signs may include[38]
- Aure-Rozanova's sign: Increased pain on palpation with a finger in the right inferior lumbar triangle (can be a positive Blumberg's sign).[39]
- Bartomier-Michelson's sign: Increased pain on palpation at the right iliac region as the person being examined lies on their left side compared to when they lie on their back.[39]
- Dunphy's sign: Increased pain in the right lower quadrant by coughing.[40]
- Hamburger sign: The patient refuses to eat (anorexia is 80% sensitive for appendicitis)[41]
- Kocher's sign (Kosher's sign): From the person's medical history, the start of pain in the umbilical region with a subsequent shift to the right iliac region.[39]
- Massouh's sign: Developed in and popular in southwest England, the examiner performs a firm swish with their index and middle finger across the abdomen from the xiphoid process to the left and the right iliac fossa.[40]
- Obturator sign: The person being evaluated lies on her or his back with the hip and knee both flexed at ninety degrees. The examiner holds the person's ankle with one hand and knee with the other hand. The examiner rotates the hip by moving the person's ankle away from their body while allowing the knee to move only inward. A positive test is pain with internal rotation of the hip.[42]
- Psoas sign, also known as "Obraztsova's sign", is right lower-quadrant pain that is produced with either the passive extension of the right hip or by the active flexion of the person's right hip while supine. The pain that is elicited is due to inflammation of the peritoneum overlying the iliopsoas muscles and inflammation of the psoas muscles themselves. Straightening out the leg causes pain because it stretches these muscles while flexing the hip activates the iliopsoas and causes pain.[42]
- Rovsing's sign: Pain in the lower right abdominal quadrant with continuous deep palpation starting from the left iliac fossa upwards (counterclockwise along the colon). The thought is there will be increased pressure around the appendix by pushing bowel contents and air toward the ileocaecal valve provoking right-sided abdominal pain.[43]
- Rosenstein's sign (Sitkovsky's sign): Increased pain in the right iliac region as the person is being examined lies on their left side.[44]
- Perman's sign: In acute appendicitis palpation in the left iliac fossa may produce pain in the right iliac fossa.[45]
Laboratory tests
While there is no laboratory test specific for appendicitis, a complete blood count (CBC) is done to check for signs of infection or inflammation. Although 70–90 percent of people with appendicitis may have an elevated white blood cell (WBC) count, many other abdominal and pelvic conditions can cause the WBC count to be elevated.[46] However, a high WBC count may not alone represent a solid indicator of appendicitis but rather an inflammation[10] but the neutrophil ratio was more sensitive and specific for acute appendicitis.[47] Several routine and non-routine laboratory tests have been investigated for discriminating simple and complicated appendicitis, but their diagnostic accuracy is uncertain.[48]
In children, neutrophil-lymphocyte ratio (NLR) demonstrates a high degree of accuracy in the diagnosis of acute appendicitis and distinguishes complicated appendicitis from simple appendicitis.[49] 75–78 percent of the patients have neutrophilia.[40] Delta-neutrophil index (DNI) is a valuable parameter that helps in the diagnosis of histologically normal appendicitis and distinguishing between simple and complicated appendicitis.[50]
A C-reactive protein (CRP) blood test will be ordered by the doctor to find out if there are any further causes of inflammation.[34] The C-reactive protein/albumin (CRP/ALB) ratio can be a reliable predictor of complicated appendicitis.[51]
The urinalysis is important for ruling out a urinary tract infection as the cause of abdominal pain. The presence of more than 20 WBC per high-power field in the urine is more suggestive of a urinary tract disorder.[46]
If the patient is a female, a pregnancy test will be ordered.[34]
Imaging
In children, the clinical examination is important to determine which children with abdominal pain should receive immediate surgical consultation and which should receive diagnostic imaging.[52] Because of the health risks of exposing children to radiation, ultrasound is the preferred first choice with CT scan being a legitimate follow-up if the ultrasound is inconclusive.[53][54][55] CT scan is more accurate than ultrasound for the diagnosis of appendicitis in adults and adolescents. CT scan has a sensitivity of 94%, specificity of 95%. Ultrasonography had an overall sensitivity of 86%, a specificity of 81%.[56]
Ultrasound

Abdominal ultrasonography, preferably with doppler sonography, is useful to detect appendicitis, especially in children. Ultrasound can show the free fluid collection in the right iliac fossa, along with a visible appendix with increased blood flow when using color Doppler, and noncompressibility of the appendix, as it is essentially a walled-off abscess. Other secondary sonographic signs of acute appendicitis include the presence of echogenic mesenteric fat surrounding the appendix and the acoustic shadowing of an appendicolith.[57] In some cases (approximately 5%),[58] ultrasonography of the iliac fossa does not reveal any abnormalities despite the presence of appendicitis. This false-negative finding is especially true of early appendicitis before the appendix has become significantly distended. Also, false-negative findings are more common in adults where larger amounts of fat and bowel gas make visualizing the appendix technically difficult. Despite these limitations, sonographic imaging with experienced hands can often distinguish between appendicitis and other diseases with similar symptoms. Some of these conditions include inflammation of lymph nodes near the appendix or pain originating from other pelvic organs such as the ovaries or Fallopian tubes. Ultrasounds may be either done by the radiology department or by the emergency physician.[59]
-
Ultrasound showing appendicitis and an appendicolith.[60]
-
Ultrasound showing appendicitis and an appendicolith.[60]
-
Ultrasound of a normal appendix for comparison.
-
A normal appendix without and with compression. Absence of compressibility indicates appendicitis.[57]
Computed tomography


Where it is readily available, computed tomography (CT) has become frequently used, especially in people whose diagnosis is not obvious on history and physical examination. Although some concerns about interpretation are identified, a 2019 Cochrane review found that the sensitivity and specificity of CT for the diagnosis of acute appendicitis in adults was high.[61] Concerns about radiation tend to limit use of CT in pregnant women and in children, especially with the increasingly widespread usage of MRI.[62][63]
The accurate diagnosis of appendicitis is multi-tiered, with the size of the appendix having the strongest positive predictive value, while indirect features can either increase or decrease sensitivity and specificity. A size of over 6 mm is both 95% sensitive and specific for appendicitis.[64]
However, because the appendix can be filled with fecal material, causing intraluminal distention, this criterion has shown limited utility in more recent meta-analyses.[65] This is as opposed to ultrasound, in which the wall of the appendix can be more easily distinguished from intraluminal feces. In such scenarios, ancillary features such as increased wall enhancement as compared to adjacent bowel and inflammation of the surrounding fat, or fat stranding, can be supportive of the diagnosis. However, their absence does not preclude it. In severe cases with perforation, an adjacent phlegmon or abscess can be seen. Dense fluid layering in the pelvis can also result, related to either pus or enteric spillage. When patients are thin or younger, the relative absence of fat can make the appendix and surrounding fat stranding difficult to see.[65]
Magnetic resonance imaging
Magnetic resonance imaging (MRI) use has become increasingly common for diagnosis of appendicitis in children and pregnant patients due to the radiation dosage that, while of nearly negligible risk in healthy adults, can be harmful to children or the developing baby.[66] In pregnancy, it is more useful during the second and third trimester, particularly as the enlargening uterus displaces the appendix, making it difficult to find by ultrasound. The periappendiceal stranding that is reflected on CT by fat stranding on MRI appears as an increased fluid signal on T2 weighted sequences. First-trimester pregnancies are usually not candidates for MRI, as the fetus is still undergoing organogenesis, and there are no long-term studies to date regarding its potential risks or side effects.[67]
X-ray
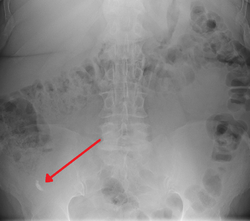
In general, plain abdominal radiography (PAR) is not useful in making the diagnosis of appendicitis and should not be routinely obtained from a person being evaluated for appendicitis.[68][69] Plain abdominal films may be useful for the detection of ureteral calculi, small bowel obstruction, or perforated ulcer, but these conditions are rarely confused with appendicitis.[70] An opaque fecalith can be identified in the right lower quadrant in fewer than 5% of people being evaluated for appendicitis.[46] A barium enema has proven to be a poor diagnostic tool for appendicitis. While failure of the appendix to fill during a barium enema has been associated with appendicitis, up to 20% of normal appendices do not fill.[70]
Scoring systems
Several scoring systems have been developed to try to identify people who are likely to have appendicitis.[71] The performance of scores such as the Alvarado score and the Pediatric Appendicitis Score, however, are variable.[72]
The Alvarado score is the most known scoring system. A score below 5 suggests against a diagnosis of appendicitis, whereas a score of 7 or more is predictive of acute appendicitis. In a person with an equivocal score of 5 or 6, a CT scan or ultrasound exam may be used to reduce the rate of negative appendectomy.
| Migratory right iliac fossa pain | 1 point |
| Anorexia | 1 point |
| Nausea and vomiting | 1 point |
| Right iliac fossa tenderness | 2 points |
| Rebound abdominal tenderness | 1 point |
| Fever | 1 point |
| High white blood cell count (leukocytosis) | 2 points |
| Shift to left (segmented neutrophils) | 1 point |
| Total score | 10 points |
|---|
Pathology
Even for clinically certain appendicitis, routine histopathology examination of appendectomy specimens is of value for identifying unsuspected pathologies requiring further postoperative management.[73] No sign of appendicitis in specimens, negative appendectomy, varies but has been estimated to occur in 13% of specimens.[74] Notably, appendix cancer is found incidentally in about 1% of appendectomy specimens.[75][76]
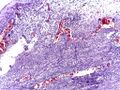
Pathology diagnosis of appendicitis can be made by detecting a neutrophilic infiltrate of the muscularis propria.
Periappendicitis (inflammation of tissues around the appendix) is often found in conjunction with other abdominal pathology.[77]
-
Micrograph of appendicitis and periappendicitis. H&E stain.
-
Micrograph of appendicitis showing neutrophils in the muscularis propria. H&E stain.
-
Acute suppurative appendicitis with perforation (at right). H&E stain.
| Pattern | Gross pathology | Light microscopy | Image | Clinical significance |
|---|---|---|---|---|
| Acute intraluminal inflammation | None visible |
|
190px | Probably none |
| Acuta mucosal inflammation | None visible |
|
May be secondary to enteritis. | |
| Suppurative acute appendicitis | May be inapparent.
|
|
190px | Can be presumed to be the primary cause of symptoms |
| Gangrenous/necrotizing appendicitis |
|
|
190px | Will perforate if untreated |
| Periappendicitis | May be inapparent.
|
|
190px | If isolated, probably secondary to other disease |
| Eosinophilic appendicitis | None visible |
|
Possibly parasitic, or eosinophilic enteritis. |
Differential diagnosis

Children: Gastroenteritis, mesenteric adenitis, Meckel's diverticulitis, intussusception, Henoch–Schönlein purpura, lobar pneumonia, urinary tract infection (abdominal pain in the absence of other symptoms can occur in children with UTI), new-onset Crohn's disease or ulcerative colitis, pancreatitis, and abdominal trauma from child abuse; distal intestinal obstruction syndrome in children with cystic fibrosis; typhlitis in children with leukemia.
Women: A pregnancy test is important for all women of childbearing age since an ectopic pregnancy can have signs and symptoms similar to those of appendicitis. Other obstetrical/ gynecological causes of similar abdominal pain in women include pelvic inflammatory disease, ovarian torsion, menarche, dysmenorrhea, endometriosis, and Mittelschmerz (the passing of an egg in the ovaries approximately two weeks before menstruation).[79]
Men: testicular torsion
Adults: new-onset Crohn disease, ulcerative colitis, regional enteritis, cholecystitis, renal colic, perforated peptic ulcer, pancreatitis, rectus sheath hematoma and epiploic appendagitis.
Elderly: diverticulitis, intestinal obstruction, colonic carcinoma, mesenteric ischemia, leaking aortic aneurysm.
The term "pseudoappendicitis" is used to describe a condition mimicking appendicitis.[80] It can be associated with Yersinia enterocolitica.[81]
Management
Acute appendicitis[82] is typically managed by surgery. While antibiotics are safe and effective for treating uncomplicated appendicitis,[11][12][83] 31% of people had a recurrence within a year and required an eventual appendectomy.[14] Antibiotics are less effective if an appendicolith is present.[84] While 51% of patients who were treated with antibiotics did not need an appendectomy three years after treatment,[85] the cost effectiveness of surgery versus antibiotics is unclear[86]
Using antibiotics to prevent potential postoperative complications in emergency appendectomy procedures is recommended, and the antibiotics are effective when given to a person before, during, or after surgery.[87]
Pain
Pain medications (such as morphine) do not appear to affect the accuracy of the clinical diagnosis of appendicitis and therefore should be given early in the patient's care.[88] Historically there were concerns among some general surgeons that analgesics would affect the clinical exam in children, and some recommended that they not be given until the surgeon was able to examine the person.[88]
Surgery

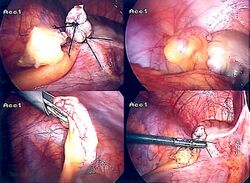

The surgical procedure for the removal of the appendix is called an appendectomy. A negative appendectomy constitutes the removal of a normal appendix with no sign of inflammation in histopathology examination. The prevalence of negative appendectomy varies but has been estimated to 13%.[74] Appendectomy can be performed through open or laparoscopic surgery. Laparoscopic appendectomy has several advantages over open appendectomy as an intervention for acute appendicitis.[89]
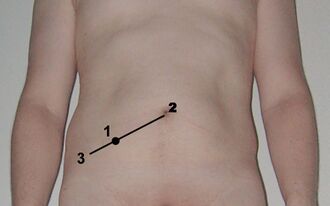
Open appendectomy
For over a century, laparotomy (open appendectomy) was the standard treatment for acute appendicitis.[90] This procedure consists of the removal of the infected appendix through a single large incision in the lower right area of the abdomen.[91] The incision in a laparotomy is usually 2 to 3 inches (51 to 76 mm) long.
During an open appendectomy, the person with suspected appendicitis is placed under general anesthesia to keep the muscles completely relaxed and to keep the person unconscious. The incision is two to three inches (76 mm) long, and it is made in the right lower abdomen, several inches above the hip bone. Once the incision opens the abdomen cavity, and the appendix is identified, the surgeon removes the infected tissue and cuts the appendix from the surrounding tissue. After careful and close inspection of the infected area, and ensuring there are no signs that surrounding tissues are damaged or infected. In case of complicated appendicitis managed by an emergency open appendectomy, abdominal drainage (a temporary tube from the abdomen to the outside to avoid abscess formation) may be inserted, but this may increase the hospital stay.[92][needs update][needs update] The surgeon will start closing the incision. This means sewing the muscles and using surgical staples or stitches to close the skin up. To prevent infections, the incision is covered with a sterile bandage or surgical adhesive.
Laparoscopic appendectomy
Laparoscopic appendectomy was introduced in 1983 and has become an increasingly prevalent intervention for acute appendicitis.[93] This surgical procedure consists of making three to four incisions in the abdomen, each 0.25 to 0.5 inches (6.4 to 12.7 mm) long. This type of appendectomy is made by inserting a special surgical tool called a laparoscope into one of the incisions. The laparoscope is connected to a monitor outside the person's body, and it is designed to help the surgeon inspect the infected area in the abdomen. The other two incisions are made for the specific removal of the appendix by using surgical instruments. Laparoscopic surgery requires general anesthesia, and it can last up to two hours. Laparoscopic appendectomy has several advantages over open appendectomy, including a shorter post-operative recovery, less post-operative pain, and a lower superficial surgical site infection rate. However, the occurrence of an intra-abdominal abscess is almost three times more prevalent in laparoscopic appendectomy than open appendectomy.[94]
Laparoscopic-assisted transumbilical appendectomy
In pediatric patients, the high mobility of the cecum allows externalization of the appendix through the umbilicus, and the entire procedure can be performed with a single incision. Laparoscopic-assisted transumbilical appendectomy is a relatively recent technique but with a long published series and very good surgical and aesthetic results.[95]
Pre-surgery
The treatment begins by keeping the person who will be having surgery from eating or drinking for a given period, usually overnight. An intravenous drip is used to hydrate the person who will be having surgery. Antibiotics given intravenously such as cefuroxime and metronidazole may be administered early to help kill bacteria and thus reduce the spread of infection in the abdomen and postoperative complications in the abdomen or wound. Equivocal cases may become more difficult to assess with antibiotic treatment and benefit from serial examinations. If the stomach is empty (no food in the past six hours), general anaesthesia is usually used. Otherwise, spinal anaesthesia may be used.
Once the decision to perform an appendectomy has been made, the preparation procedure takes approximately one to two hours. Meanwhile, the surgeon will explain the surgery procedure and will present the risks that must be considered when performing an appendectomy. (With all surgeries there are risks that must be evaluated before performing the procedures.) The risks are different depending on the state of the appendix. If the appendix has not ruptured, the complication rate is only about 3% but if the appendix has ruptured, the complication rate rises to almost 59%.[96] The most usual complications that can occur are pneumonia, hernia of the incision, thrombophlebitis, bleeding and adhesions. Evidence indicates that a delay in obtaining surgery after admission results in no measurable difference in outcomes to the person with appendicitis.[97][98] Most patients undergo emergency surgery, but delayed surgery (interval appendectomy) has been investigated for certain patients.[99] Delaying surgery for weeks may increase the risk of intra-abdominal abscess in patients suffering from appendicitis and presenting with an appendiceal mass (e.g., phlegmon or abscess).[99] The harms and benefits of delaying surgery for other complications are uncertain.[99]

The surgeon will explain how long the recovery process should take. Abdomen hair is usually removed to avoid complications that may appear regarding the incision.
In most cases, patients going in for surgery experience nausea or vomiting that require medication before surgery. Antibiotics, along with pain medication, may be administered before appendectomies.
After surgery

Hospital lengths of stay typically range from a few hours to a few days but can be a few weeks if complications occur. The recovery process may vary depending on the severity of the condition: if the appendix had ruptured or not before surgery. Appendix surgery recovery is generally much faster if the appendix does not rupture.[100] It is important that people undergoing surgery respect their doctor's advice and limit their physical activity so the tissues can heal. Recovery after an appendectomy may not require diet changes or a lifestyle change.
The length of hospital stays for appendicitis varies on the severity of the condition. A study from the United States found that in 2010, the average appendicitis hospital stay was 1.8 days. For stays where the person's appendix had ruptured, the average length of stay was 5.2 days.[8]
Prognosis
Most people with appendicitis recover quickly after surgical treatment, but complications can occur if treatment is delayed or if peritonitis occurs. Recovery time depends on age, condition, complications, and other circumstances, including the amount of alcohol consumption, but usually is between 10 and 28 days. For young children (around ten years old), the recovery takes three weeks.
The possibility of peritonitis is the reason why acute appendicitis warrants rapid evaluation and treatment. People with suspected appendicitis may have to undergo a medical evacuation. Appendectomies have occasionally been performed in emergency conditions (i.e., not in a proper hospital) when a timely medical evacuation was impossible.
Typical acute appendicitis responds quickly to appendectomy and occasionally will resolve spontaneously. If appendicitis resolves spontaneously, it remains controversial whether an elective interval appendectomy should be performed to prevent a recurrent episode of appendicitis. Atypical appendicitis (associated with suppurative appendicitis) is more challenging to diagnose and is more apt to be complicated even when operated early. In either condition, prompt diagnosis and appendectomy yield the best results with full recovery in two to four weeks usually. Mortality and severe complications are unusual but do occur, especially if peritonitis persists and is untreated.
Another entity known as the appendicular lump is talked about. It happens when the appendix is not removed early during infection, and the omentum and intestine adhere to it, forming a palpable lump. During this period, surgery is risky unless there is pus formation evident by fever and toxicity or by ultrasound. Medical management treats the condition.
An unusual complication of an appendectomy is "stump appendicitis": inflammation occurs in the remnant appendiceal stump left after a prior incomplete appendectomy.[101] Stump appendicitis can occur months to years after initial appendectomy and can be identified with imaging modalities such as ultrasound.[102]
History
The history of appendicitis traces back to ancient medical texts, though its clear clinical understanding emerged in the 19th century. Berengario da Carpi provided the first recorded description of the appendix in the 16th century, followed by Andreas Vesalius and Gabriele Falloppio. Clinical understanding progressed in the 18th and 19th centuries, marked by Lorenz Heister's autopsy findings, Claudius Aymand's surgical intervention, and J. Mestivier's operation for appendicitis. Prior to the use of the term appendicitis, it was described with terms including perityphlitis, typhlitis, paratyphlitis, and extra-peritoneal abscess of the right iliac fossa.[103] The term "appendicitis" was coined by the American physician Reginald Heber Fitz in 1886, leading to standardized diagnosis and treatment, including Charles McBurney's identification of McBurney's point. Modern appendectomy techniques evolved in the early 20th century, coinciding with advancements in pathology, notably demonstrated by Ludwig Aschoff in 1908.[104][105]
Epidemiology


Appendicitis is most common between the ages of 5 and 40.[107] In 2013, it resulted in 72,000 deaths globally, down from 88,000 in 1990.[108]
In the United States, there were nearly 293,000 hospitalizations involving appendicitis in 2010.[8] Appendicitis is one of the most frequent diagnoses for emergency department visits resulting in hospitalization among children ages 5–17 years in the United States.[109]
Adults presenting to the emergency department with a known family history of appendicitis are more likely to have this disease than those without.[110]
See also
- Evan O'Neill Kane
- Leonid Rogozov
References
- ↑ 1.0 1.1 1.2 1.3 "Appendicitis". Emergency Medicine Clinics of North America 14 (4): 653–671. November 1996. doi:10.1016/s0733-8627(05)70273-x. PMID 8921763.
- ↑ 2.0 2.1 2.2 Hobler, K. (Spring 1998). "Acute and Suppurative Appendicitis: Disease Duration and its Implications for Quality Improvement". Permanente Medical Journal 2 (2). http://www.thepermanentejournal.org/files/Spring1998/appendicitis.pdf. Retrieved 2016-10-26.
- ↑ 3.0 3.1 "Obstruction of appendix vermiformis causing acute appendicitis. An experimental study in the rabbit". Acta Chirurgica Scandinavica 148 (1): 63–72. 1982. PMID 7136413.
- ↑ 4.0 4.1 4.2 4.3 Harrison's principles of internal medicine. (18th ed.). New York: McGraw-Hill. 2012. pp. Chapter 300. ISBN 978-0-07-174889-6. http://accessmedicine.mhmedical.com/content.aspx?bookid=331&Sectionid=40727094. Retrieved 6 November 2014.
- ↑ Dölling, M; Rahimli, M; Pachmann, J (2024). "Hidden Appendicoliths and Their Impact on the Severity and Treatment of Acute Appendicitis". Journal of Clinical Medicine 13 (14): 4166. doi:10.3390/jcm13144166. PMID 39064205.
- ↑ 6.0 6.1 6.2 Emergency medicine: a comprehensive study guide (7th ed.). New York: McGraw-Hill. 2011. pp. Chapter 84. ISBN 978-0-07-174467-6. http://accessmedicine.mhmedical.com/content.aspx?bookid=348&Sectionid=40381551. Retrieved 6 November 2014.
- ↑ 7.0 7.1 7.2 Schwartz's principles of surgery (9th ed.). New York: McGraw-Hill, Medical Pub. Division. 2010. pp. Chapter 30. ISBN 978-0-07-154770-3.
- ↑ 8.0 8.1 8.2 "Trends in Rates of Perforated Appendix, 2001–2010". Healthcare Cost and Utilization Project (HCUP) Statistical Brief #159 (Rockville, MD: Agency for Healthcare Research and Quality). July 2013. PMID 24199256. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb159.pdf.
- ↑ 9.0 9.1 9.2 "Clinical practice. Suspected appendicitis". The New England Journal of Medicine 348 (3): 236–242. January 2003. doi:10.1056/nejmcp013351. PMID 12529465. http://faculty.vet.upenn.edu/gastro/documents/NEJMappendicitis.pdf. Retrieved 2017-11-01.
- ↑ 10.0 10.1 "Diagnosing appendicitis: evidence-based review of the diagnostic approach in 2014". The Western Journal of Emergency Medicine 15 (7): 859–871. November 2014. doi:10.5811/westjem.2014.9.21568. PMID 25493136.
- ↑ 11.0 11.1 Javanmard-Emamghissi, Hannah (2021). "Antibiotics as first-line alternative to appendicectomy in adult appendicitis: 90-day follow-up from a prospective, multicentre cohort study". The British Journal of Surgery 108 (11): 1351–1359. doi:10.1093/bjs/znab287. PMID 34476484. PMC 8499866. https://academic.oup.com/bjs/advance-article/doi/10.1093/bjs/znab287/6363089?searchresult=1. Retrieved 8 September 2021.
- ↑ 12.0 12.1 "Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials". BMJ 344. April 2012. doi:10.1136/bmj.e2156. PMID 22491789.
- ↑ "Appendicitis: Surgical vs. Medical Treatment | Science-Based Medicine" (in en-US). 2020-11-24. https://sciencebasedmedicine.org/appendicitis-surgical-vs-medical-treatment/.
- ↑ 14.0 14.1 Doleman, Brett; Fonnes, Siv; Lund, Jon N.; Boyd-Carson, Hannah; Javanmard-Emamghissi, Hannah; Moug, Susan; Hollyman, Marianne; Tierney, Gillian et al. (2024-04-29). "Appendectomy versus antibiotic treatment for acute appendicitis". The Cochrane Database of Systematic Reviews 2024 (4). doi:10.1002/14651858.CD015038.pub2. ISSN 1469-493X. PMID 38682788.
- ↑ "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1545–1602. October 2016. doi:10.1016/S0140-6736(16)31678-6. PMID 27733282.
- ↑ "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1459–1544. October 2016. doi:10.1016/s0140-6736(16)31012-1. PMID 27733281.
- ↑ "Surgery for appendicitis: is it necessary?". Surgical Infections 9 (4): 481–488. August 2008. doi:10.1089/sur.2007.079. PMID 18687030.
- ↑ "Significance of the obstructive factor in the genesis of acute appendicitis". Archives of Surgery 34 (3): 496–526. 1937. doi:10.1001/archsurg.1937.01190090121006.
- ↑ Fowler, Royal H. (April 1938). "The Rare Incidence of Acute Appendicitis Resulting from External Trauma". Annals of Surgery 107 (4): 529–539. doi:10.1097/00000658-193804000-00007. ISSN 0003-4932. PMID 17857157.
- ↑ Toumi, Zaher; Chan, Anthony; Hadfield, Matthew B.; Hulton, Neil R. (September 2010). "Systematic review of blunt abdominal trauma as a cause of acute appendicitis". Annals of the Royal College of Surgeons of England 92 (6): 477–482. doi:10.1308/003588410X12664192075936. ISSN 1478-7083. PMID 20513274.
- ↑ Hollerman, J.; Bernstein, MA; Kottamasu, SR; Sirr, SA (1988). "Acute recurrent appendicitis with appendicolith". The American Journal of Emergency Medicine 6 (6): 614–617. doi:10.1016/0735-6757(88)90105-2. PMID 3052484.
- ↑ 22.0 22.1 "An unusual localization of trichobezoar in the appendix". The Turkish Journal of Gastroenterology 22 (3): 357–358. June 2011. doi:10.4318/tjg.2011.0232. PMID 21805435.
- ↑ "The prevalence of appendiceal fecaliths in patients with and without appendicitis. A comparative study from Canada and South Africa". Annals of Surgery 202 (1): 80–82. July 1985. doi:10.1097/00000658-198507000-00013. PMID 2990360.
- ↑ "Appendiceal calculi and fecaliths as indications for appendectomy". Surgery, Gynecology & Obstetrics 171 (3): 185–188. September 1990. PMID 2385810.
- ↑ "Acute appendicitis related to faecal stasis". Annales Chirurgiae et Gynaecologiae 74 (2): 90–93. 1985. PMID 2992354.
- ↑ "Origin of acute appendicitis: fecal retention in colonic reservoirs: a case-control study". Surgical Infections 8 (1): 55–62. February 2007. doi:10.1089/sur.2005.04250. PMID 17381397.
- ↑ "The aetiology of appendicitis". The British Journal of Surgery 58 (9): 695–699. September 1971. doi:10.1002/bjs.1800580916. PMID 4937032.
- ↑ "Diverticular disease in urban Africans in South Africa". Digestion 24 (1): 42–46. 1982. doi:10.1159/000198773. PMID 6813167.
- ↑ "Acute appendicitis as a sign of a colorectal carcinoma". Journal of Surgical Oncology 20 (1): 17–20. May 1982. doi:10.1002/jso.2930200105. PMID 7078180.
- ↑ "Effect of dietary fibre on stools and the transit-times, and its role in the causation of disease". Lancet 2 (7792): 1408–1412. December 1972. doi:10.1016/S0140-6736(72)92974-1. PMID 4118696.
- ↑ "Fiber intake and childhood appendicitis". International Journal of Food Sciences and Nutrition 51 (3): 153–157. May 2000. doi:10.1080/09637480050029647. PMID 10945110.
- ↑ "Appendicectomy – becoming a rare event?". The Medical Journal of Australia 175 (1): 7–8. July 2001. doi:10.5694/j.1326-5377.2001.tb143501.x. PMID 11476215. http://www.mja.com.au/public/issues/175_01_020701/hugh/hugh.html.
- ↑ "Fibre and bowel transit times". The British Journal of Nutrition 45 (1): 77–82. January 1981. doi:10.1079/BJN19810078. PMID 6258626.
- ↑ 34.0 34.1 34.2 National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). (n.d.). Appendicitis – Diagnosis. Retrieved September 21, 2023, from https://www.niddk.nih.gov/health-information/digestive-diseases/appendicitis/diagnosis
- ↑ 35.0 35.1 35.2 Echevarria, S; Rauf, F; Hussain, N; Zaka, H; Farwa, UE; Ahsan, N; Broomfield, A; Akbar, A et al. (April 2023). "Typical and Atypical Presentations of Appendicitis and Their Implications for Diagnosis and Treatment: A Literature Review.". Cureus 15 (4). doi:10.7759/cureus.37024. PMID 37143626.
- ↑ Oh, JS; Kim, KW; Cho, HJ (September 2012). "Left-sided appendicitis in a patient with situs inversus totalis.". Journal of the Korean Surgical Society 83 (3): 175–178. doi:10.4174/jkss.2012.83.3.175. PMID 22977765.
- ↑ "Pain over speed bumps in diagnosis of acute appendicitis: diagnostic accuracy study". BMJ 345 (dec14 14). December 2012. doi:10.1136/bmj.e8012. PMID 23247977.
- ↑ Jones MW, Lopez RA, Deppen JG. Appendicitis. [Updated 2023 April 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan. Available from: https://www.ncbi.nlm.nih.gov/books/NBK493193/
- ↑ 39.0 39.1 39.2 Sachdeva, Anupam; Dutta, AK (2012). Advances in Pediatrics. JP Medical. p. 1432. ISBN 978-93-5025-777-7.
- ↑ 40.0 40.1 40.2 Al-Salem, Ahmed H. (2020). Atlas of Pediatric Surgery: Principles and Treatment (1st ed.). Cham: Springer. ISBN 978-3-030-29210-2.
- ↑ Virgilio, Christian de; Frank, Paul N.; Grigorian, Areg (2015) (in en). Surgery. Springer. p. 215. ISBN 978-1-4939-1726-6.
- ↑ 42.0 42.1 Wolfson, Allan B.; Cloutier, Robert L.; Hendey, Gregory W.; Ling, Louis J.; Schaider, Jeffrey J.; Rosen, Carlo L. (2014) (in en). Harwood-Nuss' Clinical Practice of Emergency Medicine. Wolters Kluwer Health. p. 5810. ISBN 978-1-4698-8948-1. https://books.google.com/books?id=cgMYBQAAQBAJ&pg=PT5810. Retrieved 15 June 2016. "Physical signs classically associated with acute appendicitis include Rovsing sign, psoas sign, and obturator sign."
- ↑ Rovsing, N.T. (1907). "Indirektes Hervorrufen des typischen Schmerzes an McBurney's Punkt. Ein Beitrag zur diagnostik der Appendicitis und Typhlitis" (in de). Zentralblatt für Chirurgie (Leipzig) 34: 1257–1259.
- ↑ Dunster, Edward Swift; Hunter, James Bradbridge; Sajous, Charles Euchariste de Medicis; Foster, Frank Pierce; Stragnell, Gregory; Klaunberg, Henry J.; Martí-Ibáñez, Félix (1922) (in en). International Record of Medicine and General Practice Clinics. New York Medical Journal. p. 663.
- ↑ Emil Samuel Perman (1856–1946), "About the indications for surgery in appendicitis and an account of cases of Sabbatsberg Hospital in Hygiea, 1904.
- ↑ 46.0 46.1 46.2 Gregory, Charmaine (2010). "Appendicitis". CDEM Self Study Modules. Clerkship Directors in Emergency Medicine. http://www.cdemcurriculum.org/ssm/gi/appy/appy.php.
- ↑ Şahbaz, NA; Bat, O; Kaya, B; Ulukent, SC; İlkgül, Ö; Özgün, MY; Akça, Ö (November 2014). "The clinical value of leucocyte count and neutrophil percentage in diagnosing uncomplicated (simple) appendicitis and predicting complicated appendicitis.". Ulusal Travma ve Acil Cerrahi Dergisi = Turkish Journal of Trauma & Emergency Surgery 20 (6): 423–426. doi:10.5505/tjtes.2014.75044. PMID 25541921.
- ↑ Sikander, Binyamin; Rosenberg, Jacob; Fonnes, Siv (May 2023). "Individual biomarkers in the blood are not yet applicable in diagnosing complicated appendicitis: A scoping review" (in en). The American Journal of Emergency Medicine 67: 100–107. doi:10.1016/j.ajem.2023.02.016. PMID 36842426. https://linkinghub.elsevier.com/retrieve/pii/S0735675723000839.
- ↑ Prasetya, D; Rochadi; Gunadi (December 2019). "Accuracy of neutrophil lymphocyte ratio for diagnosis of acute appendicitis in children: A diagnostic study.". Annals of Medicine and Surgery 48: 35–38. doi:10.1016/j.amsu.2019.10.013. PMID 31687137.
- ↑ Shin, DH; Cho, YS; Cho, GC; Ahn, HC; Park, SM; Lim, SW; Oh, YT; Cho, JW et al. (2017). "Delta neutrophil index as an early predictor of acute appendicitis and acute complicated appendicitis in adults.". World Journal of Emergency Surgery 12. doi:10.1186/s13017-017-0140-7. PMID 28747992.
- ↑ Zhao, X., Yang, J. and Li, J. (2023) The predictive value of the C-reactive protein/albumin ratio in adult patients with complicated appendicitis. Journal of Laboratory Medicine. https://doi.org/10.1515/labmed-2023-0069
- ↑ "Does this child have appendicitis?". JAMA 298 (4): 438–451. July 2007. doi:10.1001/jama.298.4.438. PMID 17652298.
- ↑ American College of Radiology, "Five Things Physicians and Patients Should Question", Choosing Wisely: an initiative of the ABIM Foundation (American College of Radiology), http://choosingwisely.org/wp-content/uploads/2012/04/5things_12_factsheet_Amer_Coll_Radiology.pdf, retrieved August 17, 2012
- ↑ "Effectiveness of a staged US and CT protocol for the diagnosis of pediatric appendicitis: reducing radiation exposure in the age of ALARA". Radiology 259 (1): 231–239. April 2011. doi:10.1148/radiol.10100984. PMID 21324843.
- ↑ "Acute appendicitis in young children: cost-effectiveness of US versus CT in diagnosis – a Markov decision analytic model". Radiology 250 (2): 378–386. February 2009. doi:10.1148/radiol.2502080100. PMID 19098225.
- ↑ "Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents". Annals of Internal Medicine 141 (7): 537–546. October 2004. doi:10.7326/0003-4819-141-7-200410050-00011. PMID 15466771.
- ↑ 57.0 57.1 "Ultrasound of pediatric appendicitis and its secondary sonographic signs: providing a more meaningful finding". Journal of Medical Radiation Sciences 63 (1): 59–66. March 2016. doi:10.1002/jmrs.154. PMID 27087976.
- ↑ "Sonographic diagnosis of acute appendicitis in children: a 3-year retrospective". Sonography 3 (3): 87–94. June 2016. doi:10.1002/sono.12068.
- ↑ Lee, Sun Hwa; Yun, Seong Jong (April 2019). "Diagnostic performance of emergency physician-performed point-of-care ultrasonography for acute appendicitis: A meta-analysis". The American Journal of Emergency Medicine 37 (4): 696–705. doi:10.1016/j.ajem.2018.07.025. PMID 30017693.
- ↑ 60.0 60.1 "UOTW #45 – Ultrasound of the Week". 25 April 2015. https://www.ultrasoundoftheweek.com/uotw-45/.
- ↑ Rud, Bo; Vejborg, Thomas S.; Rappeport, Eli D.; Reitsma, Johannes B.; Wille-Jørgensen, Peer (19 November 2019). "Computed tomography for diagnosis of acute appendicitis in adults". The Cochrane Database of Systematic Reviews 2019 (11). doi:10.1002/14651858.CD009977.pub2. ISSN 1469-493X. PMID 31743429.
- ↑ "Increasing utilization of abdominal CT in the Emergency Department of a secondary care center: does it produce better outcomes in caring for pediatric surgical patients?". Annals of Surgical Treatment and Research 87 (5): 239–244. November 2014. doi:10.4174/astr.2014.87.5.239. PMID 25368849.
- ↑ "Gastrointestinal imaging-practical magnetic resonance imaging approach". World Journal of Radiology 6 (8): 544–566. August 2014. doi:10.4329/wjr.v6.i8.544. PMID 25170393.
- ↑ "Suspected appendicitis in children: diagnostic importance of normal abdominopelvic CT findings with nonvisualized appendix". Radiology 250 (2): 531–537. February 2009. doi:10.1148/radiol.2502080624. PMID 19188320.
- ↑ 65.0 65.1 "US or CT for Diagnosis of Appendicitis in Children and Adults? A Meta-Analysis". Radiology 241 (1): 83–94. October 2006. doi:10.1148/radiol.2411050913. PMID 16928974.
- ↑ D'Souza, Nigel; Hicks, Georgina; Beable, Richard; Higginson, Antony; Rud, Bo (2021-12-14). Cochrane Colorectal Group. ed. "Magnetic resonance imaging (MRI) for diagnosis of acute appendicitis" (in en). Cochrane Database of Systematic Reviews 2021 (12). doi:10.1002/14651858.CD012028.pub2. PMID 34905621.
- ↑ "Magnetic resonance imaging of acute appendicitis in pregnancy: a 5-year multi-institutional study". American Journal of Obstetrics and Gynecology 213 (5): 693.e1–6. November 2015. doi:10.1016/j.ajog.2015.07.026. PMID 26215327.
- ↑ "Plain abdominal radiography in clinically suspected appendicitis: diagnostic yield, resource use, and comparison with CT". The American Journal of Emergency Medicine 17 (4): 325–328. July 1999. doi:10.1016/S0735-6757(99)90077-3. PMID 10452424.
- ↑ "Plain abdominal radiography as a routine procedure for acute abdominal pain of the right lower quadrant: prospective evaluation". World Journal of Surgery 23 (3): 262–264. March 1999. doi:10.1007/pl00013181. PMID 9933697.
- ↑ 70.0 70.1 APPENDICITIS from Townsend: Sabiston Textbook of Surgery on MD Consult
- ↑ Bahta, Nadir Noureldin Abdella; Rosenberg, Jacob; Fonnes, Siv (May 2023). "Many diagnostic tools for appendicitis: a scoping review". Surgical Endoscopy 37 (5): 3419–3429. doi:10.1007/s00464-023-09890-2. ISSN 1432-2218. PMID 36735050.
- ↑ "Does this child have appendicitis? A systematic review of clinical prediction rules for children with acute abdominal pain". Journal of Clinical Epidemiology 66 (1): 95–104. January 2013. doi:10.1016/j.jclinepi.2012.09.004. PMID 23177898.
- ↑ Abd Al-Fatah, Mohamed (2017). "Importance of histopathological evaluation of appendectomy specimens". Al-Azhar Assiut Medical Journal 15 (2): 97. doi:10.4103/AZMJ.AZMJ_19_17. ISSN 1687-1693.
- ↑ 74.0 74.1 Henriksen, Siri R.; Christophersen, Camilla; Rosenberg, Jacob; Fonnes, Siv (2023-05-23). "Varying negative appendectomy rates after laparoscopic appendectomy: a systematic review and meta-analysis" (in en). Langenbeck's Archives of Surgery 408 (1): 205. doi:10.1007/s00423-023-02935-z. ISSN 1435-2451. PMID 37219616. https://link.springer.com/10.1007/s00423-023-02935-z.
- ↑ Lee, Won-Suk; Choi, Sang Tae; Lee, Jung Nam; Kim, Keon Kug; Park, Yeon Ho; Baek, Jeong Heum (2011). "A retrospective clinicopathological analysis of appendiceal tumors from 3,744 appendectomies: a single-institution study". International Journal of Colorectal Disease 26 (5): 617–621. doi:10.1007/s00384-010-1124-1. ISSN 0179-1958. PMID 21234578.
- ↑ Henriksen, Siri Rønholdt; Rosenberg, Jacob; Fonnes, Siv (2023). "Other Pathologies Were Rarely Reported after Laparoscopic Surgery for Suspected Appendicitis: A Systematic Review and Meta-Analysis" (in en). Digestive Surgery 40 (3–4): 91–99. doi:10.1159/000531283. ISSN 0253-4886. PMID 37463567. https://karger.com/DSU/article/doi/10.1159/000531283.
- ↑ "Periappendicitis is a significant clinical finding". American Journal of Surgery 159 (6): 564–568. June 1990. doi:10.1016/S0002-9610(06)80067-X. PMID 2349982.
- ↑ Carr, Norman J. (2000). "The pathology of acute appendicitis". Annals of Diagnostic Pathology 4 (1): 46–58. doi:10.1016/S1092-9134(00)90011-X. ISSN 1092-9134. PMID 10684382.
- ↑ "Pelvic inflammatory disease (PID) Symptoms; Diseases and Conditions". Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/pelvic-inflammatory-disease/basics/symptoms/con-20022341.
- ↑ "Swine influenza (H1N1) and acute appendicitis". Heart & Lung 39 (6): 544–546. July 2010. doi:10.1016/j.hrtlng.2010.04.004. PMID 20633930.
- ↑ Yersinia enterocolitica infection in diarrheal patients. 27. August 2008. 741–752. doi:10.1007/s10096-008-0562-y. ISBN 978-0-9600805-6-4.
- ↑ "appendicitis". 15 June 2020. https://www.healthnsurgery.com/appendicitis-symptoms-causes-and-treatment/.
- ↑ "Meta-analysis of antibiotics versus appendicectomy for non-perforated acute appendicitis". The British Journal of Surgery 103 (6): 656–667. May 2016. doi:10.1002/bjs.10147. PMID 26990957.
- ↑ "Comparison of Antibiotic Therapy and Appendectomy for Acute Uncomplicated Appendicitis in Children: A Meta-analysis". JAMA Pediatrics 171 (5): 426–434. May 2017. doi:10.1001/jamapediatrics.2017.0057. PMID 28346589.
- ↑ "Comparing Surgery versus Antibiotics for Treating Adults with Uncomplicated Appendicitis - Evidence Update for Clinicians | PCORI" (in en). 2024-05-06. https://www.pcori.org/evidence-updates/comparing-surgery-versus-antibiotics-treating-adults-uncomplicated-appendicitis.
- ↑ "Efficacy and Safety of Nonoperative Treatment for Acute Appendicitis: A Meta-analysis". Pediatrics 139 (3): e20163003. March 2017. doi:10.1542/peds.2016-3003. PMID 28213607. http://discovery.ucl.ac.uk/1529248/1/Manuscript%20Pediatrics%20R1_with_figures.pdf.
- ↑ "Antibiotics versus placebo for prevention of postoperative infection after appendicectomy". The Cochrane Database of Systematic Reviews 2009 (3). July 2005. doi:10.1002/14651858.CD001439.pub2. PMID 16034862.
- ↑ 88.0 88.1 "Analgesia for children with acute abdominal pain and diagnostic accuracy". Archives of Disease in Childhood 93 (11): 995–997. November 2008. doi:10.1136/adc.2008.137174. PMID 18305071. http://www.bestbets.org/bets/bet.php?id=1404.
- ↑ "Laparoscopic versus open surgery for suspected appendicitis". The Cochrane Database of Systematic Reviews 2018 (11). November 2018. doi:10.1002/14651858.CD001546.pub4. PMID 30484855.
- ↑ "Appendicitis near its centenary". Annals of Surgery 200 (5): 567–575. November 1984. doi:10.1097/00000658-198411000-00002. PMID 6385879.
- ↑ "Appendicitis". National Institute of Diabetes and Digestive and Kidney Diseases. U.S. Department of Health and Human Services. http://digestive.niddk.nih.gov/ddiseases/pubs/appendicitis/.
- ↑ "Abdominal drainage to prevent intra-peritoneal abscess after appendectomy for complicated appendicitis". The Cochrane Database of Systematic Reviews 2021 (8). August 2021. doi:10.1002/14651858.CD010168.pub4. PMID 34402522.
- ↑ "Endoscopic appendectomy". Endoscopy 15 (2): 59–64. March 1983. doi:10.1055/s-2007-1021466. PMID 6221925.
- ↑ "CT predictors of failed laparoscopic appendectomy". Radiology 229 (2): 415–420. November 2003. doi:10.1148/radiol.2292020825. PMID 14595145.
- ↑ Sekioka, Akinori; Takahashi, Toshiaki; Yamoto, Masaya; Miyake, Hiromu; Fukumoto, Koji; Nakaya, Kengo; Nomura, Akiyoshi; Yamada, Yutaka et al. (December 2018). "Outcomes of Transumbilical Laparoscopic-Assisted Appendectomy and Conventional Laparoscopic Appendectomy for Acute Pediatric Appendicitis in a Single Institution". Journal of Laparoendoscopic & Advanced Surgical Techniques. Part A 28 (12): 1548–1552. doi:10.1089/lap.2018.0306. ISSN 1557-9034. PMID 30088968.
- ↑ "Appendicitis". Encyclopedia of Surgery. http://www.surgeryencyclopedia.com/A-Ce/Appendectomy.html. Retrieved 2010-02-01.
- ↑ "'Emergency' appendix surgery can wait: MDs". CBC News. 2010-09-21. http://www.cbc.ca/news/technology/emergency-appendix-surgery-can-wait-mds-1.921386.
- ↑ "Effect of delay to operation on outcomes in adults with acute appendicitis". Archives of Surgery 145 (9): 886–892. September 2010. doi:10.1001/archsurg.2010.184. PMID 20855760. "Delay of appendectomy for acute appendicitis in adults does not appear to adversely affect 30-day outcomes.".
- ↑ 99.0 99.1 99.2 Zhou, Shiyi; Cheng, Yao; Cheng, Nansheng; Gong, Jianping; Tu, Bing (2024-05-02). Cochrane Colorectal Group. ed. "Early versus delayed appendicectomy for appendiceal phlegmon or abscess" (in en). Cochrane Database of Systematic Reviews 2024 (5). doi:10.1002/14651858.CD011670.pub3. PMID 38695830.
- ↑ Appendicitis surgery, removal and reco very. Retrieved on 2010-02-01. .
- ↑ "Stump appendicitis: a comprehensive review of literature". The American Surgeon 72 (2): 162–166. February 2006. doi:10.1177/000313480607200214. PMID 16536249.
- ↑ "Stumped? It could be stump appendicitis". Sonography 4: 36–39. 2016. doi:10.1002/sono.12098.
- ↑ Krzyzak, Michael; Mulrooney, Stephen M.; Krzyzak, Michael; Mulrooney, Stephen M. (2020-06-11). "Acute Appendicitis Review: Background, Epidemiology, Diagnosis, and Treatment" (in en). Cureus 12 (6). doi:10.7759/cureus.8562. ISSN 2168-8184. PMID 32670699.
- ↑ Rondelli D (22 January 2017). "The early days in the history of appendectomy". https://hekint.org/2017/01/22/the-early-days-in-the-history-of-appendectomy/.
- ↑ "Perforating inflammation of the vermiform appendix with special reference to its early diagnosis and treatment". American Journal of the Medical Sciences (92): 321–346. 1886.
- ↑ "WHO Disease and injury country estimates". World Health Organization. 2009. https://www.who.int/healthinfo/global_burden_disease/estimates_country/en/index.html.
- ↑ "Acute appendicitis". British Journal of Hospital Medicine 73 (3): C46–48. March 2012. doi:10.12968/hmed.2012.73.sup3.C46. PMID 22411604.
- ↑ "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet 385 (9963): 117–171. January 2015. doi:10.1016/S0140-6736(14)61682-2. PMID 25530442.
- ↑ Wier, Lauren M.; Yu, Hao; Owens, Pamela L.; Washington, Raynard (June 2013). "Overview of Children in the Emergency Department, 2010". Healthcare Cost and Utilization Project Statistical Brief #157 (Agency for Healthcare Research and Quality). https://hcup-us.ahrq.gov/reports/statbriefs/sb157.jsp.
- ↑ Drescher, Michael; Marcotte, Shannon; Grant, Robert; Staff, Ilene (2012-12-01). "Family History is a Predictor for Appendicitis in Adults in the Emergency Department". Western Journal of Emergency Medicine 13 (6): 468–471. doi:10.5811/westjem.2011.6.6679. PMID 23359540. PMC 3555584. http://www.escholarship.org/uc/item/9zf1h82p.
External links
- CT of the abdomen showing acute appendicitis
- Appendicitis, history, diagnosis and treatment by Surgeons Net Education
- Appendicitis: Acute Abdomen and Surgical Gastroenterology from the Merck Manual Professional (content last modified September 2007)
- Appendicitis – Symptoms Causes and Treatment at Health N Surgery
| Classification | |
|---|---|
| External resources |
 |
 KSF
KSF![Ultrasound showing appendicitis and an appendicolith.[60]](https://handwiki.org/wiki/images/thumb/e/e0/UOTW_45_-_Ultrasound_of_the_Week_3.jpg/120px-UOTW_45_-_Ultrasound_of_the_Week_3.jpg)

![A normal appendix without and with compression. Absence of compressibility indicates appendicitis.[57]](https://handwiki.org/wiki/images/thumb/3/3e/Ultrasonography_of_a_normal_appendix_without_and_with_compression.jpg/120px-Ultrasonography_of_a_normal_appendix_without_and_with_compression.jpg)