Blood vessel disorder
Topic: Medicine
 From HandWiki - Reading time: 10 min
From HandWiki - Reading time: 10 min
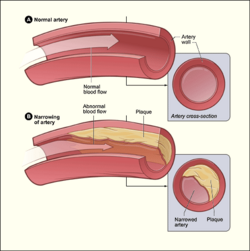
Blood vessel disorder generally refers to the narrowing, hardening or enlargement of arteries and veins. It is often due to the build-up of fatty deposits in the lumen of blood vessels or infection of the vessel wall. This can occur in various locations such as coronary blood vessels, peripheral arteries and veins. The narrowed arteries would block the blood supply to different organs and tissues.[1] In severe conditions, it may develop into more critical health problems like myocardial infarction, stroke or heart failure, which are some of the major reasons of death.[2]
There are many causes contributing to blood vessel disorder including high blood cholesterol and calcium levels, blood clot formation and inflammation of arteries. It is found that age, sedentary lifestyle, diets rich in lipids, smoking, diabetes and family history of cardiovascular diseases are common risk factors.[3] A mild degree of blood vessel disorder may be asymptomatic.[4] Blood tests on cholesterol and calcium level can be performed to monitor the risk of having the disorder. Additionally, techniques such as angiography and ultrasound imaging are useful tools for diagnosis.[5] It can be treated by both medication or surgery, depending on the type of blood vessel disorder.[citation needed]
Types of Blood Vessel Disorder
Atherosclerosis
Atherosclerosis is a developmental disease in the large arteries, defined by the accumulation of lipids, macrophages and fibrous materials in the intima.[1] When the endothelial cell of blood vessel is damaged, it loses the ability to regulate itself.[1] It results in inflammation as the macrophages irrupt the vessel wall.[1] Macrophages take up lipoprotein to form foam cells and release growth factor cytokines to attract more macrophages and smooth muscle cells.[1] A plaque is formed and proliferate to a larger size, gradually occluding the blood flow.[1] More importantly, it causes different complications that affect the whole body.[1]
Aneurysm
An aneurysm is a localized enlargement of arteries, characterized by a balloon-like bulge.[6] It results from the abnormal weakening of blood vessel wall.[7] Common types of aneurysm include abdominal aortic aneurysm, thoracic aortic aneurysm and intracranial aneurysm.[7] Most types of aneurysm, except intracranial aneurysm, are mainly caused by atherosclerosis.[7]
Raynaud’s Disease
Raynaud’s disease is a rare peripheral vascular syndrome that narrows blood vessels, generally in the hands and feet, due to cold or stressful emotion.[8] It is recognized by the reduction of blood flow to fingers and toes with periodic spasm and results in a drastic color change to white or blue.[8][9] The disease may further develop into ischaemic pain and necrosis of fingers or toes.[9] The pathology of Raynaud's disease starts with the activation of sympathetic nervous system triggered by cold or the feeling of stress.[8]
Venous thromboembolism
Venous thromboembolism (VTE) is a common peripheral venous disease. It is defined by the occlusion of venous blood vessels by blood clots. There are two major types of VTE: deep-vein thrombosis (DVT) and pulmonary embolism.[10] DVT is often found in the calf, accompanies with the swelling of limbs along the deep vein while pulmonary embolism causes chronic pulmonary hypertension.[11] VTE is the third deadliest cardiovascular disease in the world.[11] Haemostasis is the rapid development of blood clots for the purpose of reducing blood loss.[11] On the contrary, venous clots are formed much slower, in terms of several days or even weeks. Abnormality of coagulation during haemostasis, change in blood flow and endothelial failure may trigger VTE.[11]
Erythromelalgia
Erythromelalgia is a rare clinical disorder causing redness, burning sensation and intense pain in limbs.[12] It is more common to be found in lower limbs than upper limbs.[12] Erythromelalgia initiated from dysfunction of peripheral nerves that thickens the blood vessel walls, resulting in hyperaemic flow in limbs.[13]
Stroke
Stroke is a serious condition of blood vessel disorder caused by the stop of blood supply to the brain. Brain cells with ceased oxygen supply from blood will die in millions per second.[14] Not only is it one of the major causes of death around the world, it is also the cause of permanent disability. Two major types of stroke include ischemic stroke which is caused by atherosclerosis in the brain and hemorrhagic stroke which is the bleeding in the brain due to weakened blood vessel wall inside the brain.[citation needed]
Signs and symptoms
It is often asymptomatic in the early stages of blood vessel disorder.[4] When the disease develops, a variety of signs can be observed in different body parts. For instance, patients may have pale skin, cold hands and feet, and numb fingertips. These are mainly due to the reduction in blood flow to the limbs, resulting in a decrease in heat distribution to these areas. Ulcers and wounds would also take a much longer time to heal because of the impairment in blood clot formation process. Muscle weakness and cramping may occur as well, especially in the legs, because of the insufficient oxygen supply to muscle cells for metabolism.[citation needed]
Complications
The vascular system strongly influences the condition of the heart. It is also vital in the rest of the body as the blood vessels are in charge of carrying nutrients and the discard of metabolic wastes. Therefore, blood vessel disorder can cause serious complications in the whole body.[citation needed]
Coronary arteries are the blood vessels that supply to the heart for its normal function. Blood vessel disorders occur in coronary arteries would affect cardiac activity. For instance, due to atherosclerosis, the plaque would obstruct and causes ischaemia - the reduction of blood flow through the arteries. Ischaemia would then result in the decrease in oxygen supply to the heart, hence weaken the heart. It causes a vicious cycle as a weakened heart contraction would decrease blood supply to the body, including cardiac muscle (muscle of heart). Moreover, if the plaque suddenly ruptures in the heart, it will cause a heart attack.[citation needed]
Risk factors
Various factors may affect one's susceptibility to blood vessel disorders, including behavioural (e.g. smoking), demographic (e.g. age) and genetic (family history) factors. Most of these risk factors first promote the increase in blood pressure, followed by other symptoms and signs.[citation needed]
Age
The rise of blood pressure is correlated to ageing.[3] The arterial compliance - the amount of tension produced per stretch of arteries, decreases with age, and the stiffness of arteries increases with age.[3] The structural change in blood vessels causes the elderly to be more susceptible to hypertension, which leads to complications in arteries, the heart and even the brain.[citation needed]
Obesity
Having obesity would increase the risk of atherosclerosis.[1] A high-fat and high-cholesterol diet would result in an elevation of lipoprotein level, which is one of the constituents of plaque. Lipoprotein level above > 25–30 mg/dl is considered more susceptible by blood vessel disorders.[1]
Family history
Some of the blood vessel disorders are inherited. For instance, erythromelalgia is caused by the mutation of the SCN9A gene, which alters the neural pathway to blood vessels.[8] Genetic disorders that affect the circulatory, immune or neural system may contribute to hereditary blood vessel disorder. If one’s family history shows records of vascular disorders, it is more likely to inherit the same disease.[citation needed]
Smoking
Both active or passive smoking may bring harm to the vascular system.[15] For instance, cigarette smoking, cannabinoids and smokeless tobacco use were all found to raise blood pressure and increase the risk of stroke.[15] Moreover, cigar and cigarette smoking may also cause arterial stiffness.[15]
Medication
Some medications may have the side effect of increasing blood pressure and may even suppress the effect of anti-inflammatory drugs. Pain and anti-inflammatory drugs like Indomethacin, nonsteroidal anti-inflammatory drugs and piroxicam would retain water in the systemic circulation, raising the blood pressure.[16] Other types of medications like antidepressant, hormone and caffeine would also increase blood pressure.[citation needed]
Diagnosis
Doctors may look for signs of narrowed, enlarged or hardened arteries by performing a physical examination.[17] If blood vessel disorder is present, there will be a weak or even absent pulse under the narrowed area of the artery. The blood pressure in the affected limb would be lowered and whooshing sounds can be heard over the affected arteries using a stethoscope.[17] After that, the following tests could be adapted to further locate the point of narrowing or enlargement of blood vessels.[citation needed]
Angiography
Angiography is a medical imaging technique used to visualize the lumen of blood vessels.[18] A catheter, which is a long and thin tube, is inserted into a large artery in the arm or groin area. It is then guided along the artery to the targeted blood vessel to be examined. An imaging dye is loaded into the blood vessel through the catheter and the movement of the dye in the blood vessel is recorded as an angiogram.[18] Doctors could determine if there are any abnormalities in the blood vessel using fluoroscopy, computed tomography (CT) angiography or magnetic resonance (MR) angiography. After the catheter is removed, some pressure is applied to the incision site for 10 to 20 minutes to prevent excessive bleeding.[citation needed]
Vascular ultrasound
Vascular ultrasound is a non-invasive imaging method to examine the circulation inside blood vessels. Sound waves are transmitted through the tissues of the targeted area and they reflect on the blood cells moving within blood vessels.[19] The waves recorded are displayed as an image of the blood vessel and the speed of waves detected can be used to calculate the speed of blood flow inside the vessel.[20] When the rate of blood flow is too low, there may be a blockage of vessel. By evaluating blood flow in vessels, the severity and specific location of blood vessel disorder can be determined.[20]
Treatments
Different kinds of treatment should be adopted according to the type and severity of blood vessel disorder. Medications are usually prescribed to relieve specific symptoms arisen from the disease while surgery like angioplasty can be performed to provide a more long-lasting effect.[citation needed]
Surgery
Angioplasty is a procedure used to widen narrowed blood vessels, especially in coronary arteries. A long and thin tube called catheter is inserted into a large artery through an incision in the wrist, arm or groin area. The catheter is guided to the affected artery using a real-time x-ray video. A thin wire is then introduced into the blood vessel, delivering a small balloon to the affected area. The balloon is inflated to stretch the blood vessel and compress the fatty deposits against the wall of artery.[21] Hence, the vessel is widened and blood can flow through it freely to maintain adequate blood supply to different tissues. Finally, the balloon is deflated and removed. A stent may also be placed to provide support to the vessel wall and prevent it from re-narrowing.[22]
Medications
Beta blockers are medications that inhibit the sympathetic nervous system by blocking the beta adrenergic receptors. They can be used to slow down heart rate and decrease blood pressure by inhibiting beta receptors in the heart.[23] These medications also induce vasodilation by relaxing smooth muscle in blood vessels. Examples of beta blockers include carvedilol, metoprolol, and bisoprolol. [citation needed]
Calcium channel blockers are medications that prevent the movement of calcium ions across calcium channels. They can be used to relieve hypertension by causing vascular smooth muscle relaxation.[24] They also reduce the heart rate and contractility to lower the cardiac output, which in turn lower blood pressure. Amlodipine, hydralazine and dihydropyridine are examples of calcium channel blockers.[citation needed]
Other medications such as angiotensin-converting enzyme (ACE) inhibitors and diuretics can be used to relieve hypertension.[25] Statins and fibrates can also be prescribed to lower blood cholesterol level and hence reducing the risk of plaque formation in blood vessels.[26] Anti-platelet medications e.g. aspirin help reducing blood clot formation in vessels as well.
References
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Lusis, Aldons J. (September 2000). "Atherosclerosis". Nature 407 (6801): 233–241. doi:10.1038/35025203. PMID 11001066.
- ↑ "The top 10 causes of death". https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- ↑ 3.0 3.1 3.2 Pinto, E. (1 February 2007). "Blood pressure and ageing". Postgraduate Medical Journal 83 (976): 109–114. doi:10.1136/pgmj.2006.048371. PMID 17308214.
- ↑ 4.0 4.1 Høyer, Christian (2014), Diagnosis of Peripheral Arterial Disease Based on Distal Limb Pressures, 1, River Publisher, pp. 1–129, doi:10.13052/rp-oa9788793102781, ISBN 9788793102781
- ↑ Espinola-Klein, C. (2 April 2011). "Periphere arterielle Verschlusskrankheit" (in German). Der Internist 52 (5): 549–561. doi:10.1007/s00108-011-2814-7. PMID 21455686.
- ↑ Mironov, A (20 July 2009). "026 Pathogenetic factors and management of distal dissecting brain aneurysms". Journal of NeuroInterventional Surgery 1 (1): 83. doi:10.1136/jnis.2009.000851z.
- ↑ 7.0 7.1 7.2 Akers, Donald L.; Kerstein, Morris. D. (2014). "Aneurysm". AccessScience. doi:10.1036/1097-8542.034100.
- ↑ 8.0 8.1 8.2 8.3 Cooke, John P; Marshall, Janice M (3 September 2016). "Mechanisms of Raynaud's disease". Vascular Medicine 10 (4): 293–307. doi:10.1191/1358863x05vm639ra. PMID 16444858.
- ↑ 9.0 9.1 Kim, Youn Hwan; Ng, Siew-Weng; Seo, Heung Seok; Chang Ahn, Hee (November 2011). "Classification of Raynaud's disease based on angiographic features". Journal of Plastic, Reconstructive & Aesthetic Surgery 64 (11): 1503–1511. doi:10.1016/j.bjps.2011.05.017. PMID 21704575.
- ↑ Wolberg, Alisa S.; Rosendaal, Frits R.; Weitz, Jeffrey I.; Jaffer, Iqbal H.; Agnelli, Giancarlo; Baglin, Trevor; Mackman, Nigel (7 May 2015). "Venous thrombosis". Nature Reviews Disease Primers 1 (1): 15006. doi:10.1038/nrdp.2015.6. PMID 27189130.
- ↑ 11.0 11.1 11.2 11.3 Furie, Bruce; Furie, Barbara C. (28 August 2008). "Mechanisms of Thrombus Formation". New England Journal of Medicine 359 (9): 938–949. doi:10.1056/NEJMra0801082. PMID 18753650.
- ↑ 12.0 12.1 Davis, Mark Denis P. (March 2004). "Erythromelalgia". Mayo Clinic Proceedings 79 (3): 298. doi:10.4065/79.3.298. PMID 15008600.
- ↑ Daniels, Justin (2011). "Erythromelalgia". Harper's Textbook of Pediatric Dermatology. pp. 166.1–166.4. doi:10.1002/9781444345384.ch166. ISBN 978-1-4443-4538-4.
- ↑ Owens, Brian (25 June 2014). "Stroke". Nature 510 (7506): S1. doi:10.1038/510S1a. PMID 24964020. Bibcode: 2014Natur.510S...1O.
- ↑ 15.0 15.1 15.2 Katsiki, N.; Papadopoulou, S.K.; Fachantidou, A.I.; Mikhailidis, D.P. (May 2013). "Smoking and vascular risk: are all forms of smoking harmful to all types of vascular disease?". Public Health 127 (5): 435–441. doi:10.1016/j.puhe.2012.12.021. PMID 23453194.
- ↑ Johnson, Anthony G. (15 August 1994). "Do Nonsteroidal Anti-inflammatory Drugs Affect Blood Pressure? A Meta-Analysis". Annals of Internal Medicine 121 (4): 289–300. doi:10.7326/0003-4819-121-4-199408150-00011. PMID 8037411.
- ↑ 17.0 17.1 "Arteriosclerosis / atherosclerosis - Diagnosis and treatment". Mayo Clinic. https://www.mayoclinic.org/diseases-conditions/arteriosclerosis-atherosclerosis/diagnosis-treatment/drc-20350575.
- ↑ 18.0 18.1 Leopold, Jane A.; Faxon, David P. (2018). "Diagnostic Cardiac Catheterization and Coronary Angiography". in Jameson, J. Larry; Fauci, Anthony S.; Kasper, Dennis L. et al.. Harrison's Principles of Internal Medicine. McGraw-Hill Education. https://accessmedicine.mhmedical.com/content.aspx?bookid=2129§ionid=188731162.
- ↑ Thrush, Abigail (2006). Peripheral vascular ultrasound : how, why, and when. Elsevier Churchill Livingstone. ISBN 978-0-443-07283-3. OCLC 475766794. https://archive.org/details/peripheralvascul0000thru.[page needed]
- ↑ 20.0 20.1 Roman, Mary J; Naqvi, Tasneem Z; Gardin, Julius M; Gerhard-Herman, Marie; Jaff, Michael; Mohler, Emile; American Society of Echocardiography; Society for Vascular Medicine and Biology (29 June 2016). "American Society of Echocardiography Report". Vascular Medicine 11 (3): 201–211. doi:10.1177/1358863x06070511. PMID 17288128. http://www.asecho.org/wp-content/uploads/2013/05/Clinical-App-of-Noninvasive-Vasc-US-in-CV-Risk-Stratification.pdf.
- ↑ Serruys, Patrick W.; de Jaegere, Peter; Kiemeneij, Ferdinand; Macaya, Carlos; Rutsch, Wolfgang; Heyndrickx, Guy; Emanuelsson, Hakan; Marco, Jean et al. (25 August 1994). "A Comparison of Balloon-Expandable-Stent Implantation with Balloon Angioplasty in Patients with Coronary Artery Disease". New England Journal of Medicine 331 (8): 489–495. doi:10.1056/NEJM199408253310801. PMID 8041413. http://repub.eur.nl/pub/58398.
- ↑ Kempczinski, Richard (November 1987). "Intravascular stents to prevent occlusion and restenosis after transluminal angioplasty". Journal of Vascular Surgery 6 (5): 533. doi:10.1016/0741-5214(87)90320-x.
- ↑ Wiysonge, Charles S; Bradley, Hazel A; Volmink, Jimmy; Mayosi, Bongani M; Opie, Lionel H (20 January 2017). "Beta-blockers for hypertension". Cochrane Database of Systematic Reviews 1 (1): CD002003. doi:10.1002/14651858.CD002003.pub5. PMID 28107561.
- ↑ Mason, R.P.; Marche, P.; Hintze, T.H. (December 2003). "Novel Vascular Biology of Third-Generation L-Type Calcium Channel Antagonists". Arteriosclerosis, Thrombosis, and Vascular Biology 23 (12): 2155–2163. doi:10.1161/01.ATV.0000097770.66965.2A. PMID 14512371.
- ↑ Flather, Marcus D; Yusuf, Salim; Køber, Lars; Pfeffer, Marc; Hall, Alistair; Murray, Gordon; Torp-Pedersen, Christian; Ball, Stephen et al. (May 2000). "Long-term ACE-inhibitor therapy in patients with heart failure or left-ventricular dysfunction: a systematic overview of data from individual patients". The Lancet 355 (9215): 1575–1581. doi:10.1016/s0140-6736(00)02212-1. PMID 10821360.
- ↑ "Intensive versus moderate lipid lowering with statins after acute coronary syndromes". Obstetrics & Gynecology 104 (1): 188. July 2004. doi:10.1097/01.aog.0000133105.83326.47.
 |
 KSF
KSF