Borderline personality disorder
Topic: Medicine
 From HandWiki - Reading time: 58 min
From HandWiki - Reading time: 58 min
| Borderline personality disorder | |
|---|---|
| Other names | |
 | |
| Specialty | Psychiatry, clinical psychology |
| Symptoms | Unstable relationships, distorted sense of self, and intense emotions; impulsivity; recurrent suicidal and self-harming behavior; fear of abandonment; chronic feelings of emptiness; inappropriate anger; dissociation[5][6] |
| Complications | Suicide, self-harm[5] |
| Usual onset | Early adulthood[6] |
| Duration | Long term[5] |
| Causes | Genetic, neurobiologic, and psychosocial theories proposed |
| Diagnostic method | Based on reported symptoms[5] |
| Differential diagnosis | See § Differential diagnosis |
| Treatment | Behaviour therapy[5] |
| Prognosis | Improves over time,[6] remission occurs in 45% of patients over a wide range of follow-up periods[7][8][9][10][11] |
| Frequency | 5.9% (lifetime prevalence)[5] |
| Personality disorders |
|---|
| Cluster A (odd) |
| Cluster B (dramatic) |
| Cluster C (anxious) |
| Not specified |
Borderline personality disorder (BPD) is a personality disorder characterized by a pervasive, long-term pattern of significant interpersonal relationship instability, acute fear of abandonment, and intense emotional outbursts.[6][12][13] People with BPD frequently exhibit self-harming behaviours and engage in risky activities, primarily caused by difficulties in regulating emotions.[14][15][16] Symptoms such as dissociation, a pervasive sense of emptiness, and distorted sense of self are prevalent.[12]
Onset of symptoms can be triggered by events others perceive as normal,[12] with the disorder typically manifesting in early adulthood and persisting across diverse contexts.[6] BPD is often comorbid with substance use disorders,[17][18] depressive disorders, and eating disorders.[12] Studies estimate up to 10 percent of people with BPD die by suicide.[19][20] BPD faces significant stigmatization in media portrayals and the psychiatric field, leading to underdiagnosis and insufficient treatment.[21][22]
Causes of BPD are unclear and complex, implicating genetic, neurological, and psychosocial conditions in its development.[5][23] The current hypothesis suggests BPD is caused by an interaction between genetic factors and adverse childhood experiences.[24][25] BPD is significantly more common in people with a family history of BPD, particularly immediate relatives, suggesting genetic predisposition.[26] There is a risk of misdiagnosis, with BPD commonly confused with a mood disorder, substance use disorder, or other mental health disorders.[6] Therapeutic interventions predominantly involve psychotherapy, with dialectical behavior therapy (DBT) and schema therapy being the most effective.[5][22] Although pharmacotherapy cannot cure BPD, it may be employed to mitigate symptoms,[5] with atypical antipsychotics and selective serotonin reuptake inhibitor (SSRI) antidepressants commonly prescribed. Medications are used cautiously, show limited efficacy, and have minimal impact on neural function.[27][28][29] Despite the high utilization of healthcare resources by people with BPD,[30] up to half may show significant improvement over ten years with appropriate treatment.[6]
Estimation of BPD's prevalence varies. In the US, around 1% of the population are diagnosed with it.[31] BPD is more prevalent among adolescents and young adults than elderly, and symptoms may remit with age.[31] The term ‘borderline’ is debated, as it referred to concepts of borderline insanity and patients on the border between neurosis and psychosis, which are now considered clinically imprecise.[5][32]
Signs and symptoms

The distinguishing characteristics of borderline personality disorder (BPD) include a pervasive pattern of instability in one's interpersonal relationships and in one's self-image, with frequent oscillation between extremes of idealization and devaluation of others, alongside fluctuating moods and difficulty regulating intense emotional reactions. Dangerous or impulsive behaviors are commonly associated with BPD.[33]
Additional symptoms may encompass uncertainty about one's identity, values, morals, and beliefs; experiencing paranoid thoughts under stress; episodes of depersonalization; and, in moderate to severe cases, stress-induced breaks with reality or episodes of psychosis. It is also common for individuals with BPD to have comorbid conditions such as depressive or bipolar disorders, substance use disorders, eating disorders, post-traumatic stress disorder (PTSD), and attention deficit hyperactivity disorder (ADHD).[34]
Emotional dysregulation
Emotional dysregulation is a core feature of BPD and it is characterized by a difficulty in effectively managing emotional states.[35]: 1 It may involve high sensitivity to emotional stimuli, heightened emotional intensity, large and rapid mood shifts, tendency for negative emotions, and a slow return to baseline after emotional arousal.[36] Emotional dysregulation extends beyond emotions, affecting cognition, relationships, and behaviour.[37]: 899
Deficits in emotion regulation strategies are observed in BPD. These include resistance to accepting emotional responses, low flexibility to changing strategies, difficulty in identifying emotions, as well as a deficit in goal-directed behaviour, and in using healthy coping strategies.[38]: 108 [39]: 226 Maladaptive strategies to regulate their emotions include self-harm, rumination, avoidance, and thought suppression.[37]: 905 [40]: 21 [39]: 225
Emotional dysregulation is thought to be caused by an imbalance in the limbic system and the prefrontal cortex, particularly in the amygdala.[41]: 114–115 Dialectical behaviour therapy can be employed to help with emotional dysregulation.[39]: 224
Interpersonal relationships
Interpersonal relationships are significantly impacted in individuals with BPD, characterized by a heightened sensitivity to the behavior and actions of others. Individuals with BPD can be very conscious of and susceptible to their perceived or real treatment by others. Individuals may experience profound happiness and gratitude for perceived kindness, yet feel intense sadness or anger[42] towards perceived criticism or harm.[43] A notable feature of BPD is the tendency to engage in idealization and devaluation of others – that is to idealize and subsequently devalue others – oscillating between extreme admiration and profound mistrust or dislike.[44] This pattern, referred to as "splitting", can significantly influence the dynamics of interpersonal relationships.[45][46] In addition to this external "splitting", patients with BPD typically have internal splitting, i.e. vacillation between considering oneself a good person who has been mistreated (in which case anger predominates) and a bad person whose life has no value (in which case self-destructive or even suicidal behavior may occur). This splitting is also evident in black-and-white or all-or-nothing dichotomous thinking.[47]
Despite a strong desire for intimacy, individuals with BPD may exhibit insecure, avoidant, ambivalent, or fearfully preoccupied attachment styles in relationships, complicating their interactions and connections with others.[48] Family members, including parents of adults with BPD, may find themselves in a cycle of being overly involved in the individual's life at times and, at other times, significantly detached,[49] contributing to a sense of alienation within the family unit.[47] Anthropologist Rebecca Lester argues that BPD is a disorder of relationships and communication, namely that a person with BPD lacks the communication skills and knowledge to interact effectively with others within their society and culture given their life experience.[50]
Personality disorders, including BPD, are associated with an increased incidence of chronic stress and conflict, reduced satisfaction in romantic partnerships, domestic abuse, and unintended pregnancies.[51] Research indicates variability in relationship patterns among individuals with BPD. A portion of these individuals may transition rapidly between relationships, a pattern metaphorically described as "butterfly-like," characterized by fleeting and transient interactions and "fluttering" in and out of relationships.[52] Conversely, a subgroup, referred to as "attached," tends to establish fewer but more intense and dependent relationships. These connections often form rapidly, evolving into deeply intertwined and tumultuous bonds.[52] In certain cases, BPD may be recognized as a disability within the workplace, particularly if the condition's severity results in behaviors that undermine relationships, involve engagement in risky activities, or manifest as intense anger, thereby inhibiting the individual's ability to perform their job role effectively.[53] Individuals with BPD express higher levels of jealousy towards their partners in romantic relations.[54][55]
Manipulative behavior to obtain nurturance is considered by the DSM-IV-TR[56] and many mental health professionals to be a characteristic of borderline personality disorder.[56] In one research study, 88% of therapists reported that they have experienced manipulation attempts from patient(s).[57] Marsha Linehan has argued that doing so relies upon the assumption that people with BPD who communicate intense pain, or who engage in self-harm and suicidal behavior, do so to influence the behavior of others.[58] The impact of such behavior on others—often an intense emotional reaction in concerned friends, family members, and therapists—is thus assumed to have been the person's intention.[58] According to Linehan, their frequent expressions of intense pain, self-harming, or suicidal behavior may instead represent a method of mood regulation or an escape mechanism from situations that feel unbearable, however, making their assumed manipulative behavior an involuntary and unintentional response.[59]
Behavior
Behavioral patterns associated with BPD frequently involve impulsive actions, which may manifest as substance use disorders, binge eating, unprotected sexual encounters, and self-injury, among other self-harming practices.[60] These behaviors are a response to the intense emotional distress experienced by individuals with BPD, serving as an immediate but temporary alleviation of their emotional pain.[60] However, such actions typically result in feelings of shame and guilt, contributing to a recurrent cycle.[60] This cycle typically begins with emotional discomfort, followed by impulsive behavior aimed at mitigating this discomfort, only to lead to shame and guilt, which in turn exacerbates the emotional pain.[60] This escalation of emotional pain then intensifies the compulsion towards impulsive behavior as a form of relief, creating a vicious cycle. Over time, these impulsive responses can become an automatic mechanism for coping with emotional pain.[60] Interventions such as dialectical behavior therapy (DBT) and schema therapy aim to disrupt this cycle by improving emotional regulation, distress tolerance, and adaptive coping strategies.[61]
Self-harm and suicide
Self-harm and suicidal behaviors are core diagnostic criteria for BPD as outlined in the DSM-5.[6] Between 50% and 80% of individuals diagnosed with BPD engage in self-harm, with cutting being the most common method.[62] Other methods, such as bruising, burning, head banging, or biting, are also prevalent.[62] It is hypothesized that individuals with BPD might experience a sense of emotional relief following acts of self-harm.[63]
Estimates of the lifetime risk of death by suicide among individuals with BPD range between 3% and 10%, varying with the method of investigation.[64][47][65] There is evidence that a significant proportion of males who die by suicide may have undiagnosed BPD.[66]
The motivations behind self-harm and suicide attempts among individuals with BPD are reported to differ.[67] Nearly 70% of individuals with BPD engage in self-harm without the intention of ending their lives. Motivations for self-harm include expressing anger, self-punishment, inducing normal feelings or feelings of normality in response to dissociative episodes, and distraction from emotional distress or challenging situations.[67][non-primary source needed] Conversely, true suicide attempts by individuals with BPD frequently are motivated by the notion that others will be better off in their absence.[67][non-primary source needed]
Sense of self and self-concept
Individuals diagnosed with BPD frequently experience significant difficulties in maintaining a stable self-concept.[68] This identity disturbance manifests as uncertainty in personal values, beliefs, preferences, and interests.[69] They may also express confusion regarding their aspirations and objectives in terms of relationships and career paths. Such indeterminacy leads to feelings of emptiness and a profound sense of disorientation regarding their own identity.[69] Moreover, their self-perception can fluctuate dramatically over short periods, oscillating between positive and negative evaluations. Consequently, individuals with BPD might adopt their sense of self based on their surroundings or the people they interact with, resulting in a chameleon-like adaptation of identity.[70]
Dissociation and cognitive challenges
The heightened emotional states experienced by individuals with BPD can impede their ability to concentrate and cognitively function.[69] Additionally, individuals with BPD may frequently dissociate, which can be regarded as a mild to severe disconnection from physical and emotional experiences.[71] Observers may notice signs of dissociation in individuals with BPD through diminished expressiveness in their face or voice, or an apparent disconnection and insensitivity to emotional cues or stimuli.[71]
Researchers disagree about whether dissociation or a sense of emotional detachment and physical experiences impact the ability of people with BPD to recall the specifics of past events. A 1999 study reported that the specificity of autobiographical memory was decreased in BPD patients.[72] The researchers found that decreased ability to recall specifics was correlated with patients' levels of dissociation, which "may help them to avoid episodic information that would evoke acutely negative affect".[72][73]
Psychotic symptoms
BPD is predominantly characterized as a disorder involving emotional dysregulation, yet psychotic symptoms frequently occur in individuals with BPD, with about 20–50% of patients reporting psychotic symptoms.[74] These manifestations have historically been labeled as "pseudo-psychotic" or "psychotic-like", implying a differentiation from symptoms observed in primary psychotic disorders. Studies conducted in the 2010s suggest a closer similarity between psychotic symptoms in BPD and those in recognized psychotic disorders than previously understood.[74][75] The distinction of pseudo-psychosis has faced criticism for its weak construct validity and the potential to diminish the perceived severity of these symptoms, potentially hindering accurate diagnosis and effective treatment. Consequently, there are suggestions from some in the research community to categorize these symptoms as genuine psychosis, advocating for the abolishment of the distinction between pseudo-psychosis and true psychosis.[74][76] The DSM-5 identifies transient paranoia, exacerbated by stress, as a symptom of BPD.[6] Research has identified the presence of both hallucinations and delusions in individuals with BPD who do not possess an alternate diagnosis that would better explain these symptoms.[75] Further, phenomenological analysis indicates that auditory verbal hallucinations in BPD patients are indistinguishable from those observed in schizophrenia.[75][76] This has led to suggestions of a potential shared etiological basis for hallucinations across BPD and other disorders, including psychotic and affective disorders.[75]
Causes
The etiology, or causes, of BPD is multifaceted, with no consensus on a singular cause.[77] BPD may share a connection with post-traumatic stress disorder (PTSD), with both having a traumatic substrate.[78] While childhood trauma is a recognized contributing factor, the roles of congenital brain abnormalities, genetics, neurobiology, and non-traumatic environmental factors remain subjects of ongoing investigation.[77][79]
Genetics and heritability
Compared to other major psychiatric conditions, the exploration of genetic underpinnings in BPD remains novel.[80] Estimates suggest the heritability of BPD ranges from 37% to 69%,[81] indicating that human genetic variations account for a substantial portion of the risk for BPD within the population. Twin studies, which often form the basis of these estimates, may overestimate the perceived influence of genetics due to the shared environment of twins, potentially skewing results.[82]
Certain studies propose that personality disorders are significantly shaped by genetics, more so than many Axis I disorders, such as depression and eating disorders, and even surpassing the genetic impact on broad personality traits.[83] A twin study found that BPD ranks as the third most heritable among ten surveyed personality disorders.[83]
Research involving twin and sibling studies has shown a genetic component to traits associated with BPD, such as impulsive aggression; with the genetic contribution to behavior from serotonin-related genes appearing to be modest.[84]
A study conducted by Trull et al. in the Netherlands, which included 711 sibling pairs and 561 parents, aimed to identify genetic markers associated with BPD.[85] This research identified a linkage to genetic markers on chromosome 9 as relevant to BPD characteristics,[85] underscoring a significant genetic contribution to the variability observed in BPD features.[85] Prior findings from this group indicated that 42% of BPD feature variability could be attributed to genetics, with the remaining 58% owing to environmental factors.[85]
Among specific genetic variants under scrutiny as of 2012[update], the DRD4 7-repeat polymorphism (of the dopamine receptor D4) located on chromosome 11 has been linked to disorganized attachment, and in conjunction with the 10/10-repeat genotype of the dopamine transporter (DAT), it has been associated with issues with inhibitory control, both of which are characteristic of BPD.[86] Additionally, potential links to chromosome 5 are being explored, further emphasizing the complex genetic landscape influencing BPD development and manifestation.[87][88]
Psychosocial factors
Empirical studies have established a strong correlation between adverse childhood experiences such as child abuse, particularly child sexual abuse, and the onset of BPD later in life.[89][90][91] Reports from individuals diagnosed with BPD frequently include narratives of extensive abuse and neglect during early childhood, though causality remains a subject of ongoing investigation.[92] These individuals are significantly more prone to recount experiences of verbal, emotional, physical, or sexual abuse by caregivers,[93] alongside a notable frequency of incest and loss of caregivers in early childhood.[94]
Moreover, there have been consistent accounts of caregivers invalidating the individuals' emotions and thoughts, neglecting physical care, failing to provide the necessary protection, and exhibiting emotional withdrawal and inconsistency.[94] Specifically, female individuals with BPD reporting past neglect or abuse by caregivers have a heightened likelihood of encountering sexual abuse from individuals outside their immediate family circle.[94] Research also indicates that neurodevelopment variations such as autism spectrum traits, ADHD, or highly sensitive people (HSP) may increase vulnerability to trauma and subsequent borderline personality organization.[95]
The enduring impact of chronic maltreatment and difficulties in forming secure attachments during childhood has been hypothesized to potentially contribute to the development of BPD.[96] Marsha Linehan's biosocial developmental theory posits that BPD arises from the interaction between a child's inherent emotional vulnerability and an invalidating environment – an environment characterized by the neglect, ridicule, dismissal, or discouragement of a child's emotions and needs.[97]
Brain and neurobiologic factors
Research employing structural neuroimaging techniques, such as voxel-based morphometry, has reported variations in individuals diagnosed with BPD in specific brain regions that have been associated with the psychopathology of BPD. Reductions in volume enclosed have been observed in the hippocampus, orbitofrontal cortex, anterior cingulate cortex, and amygdala, among others, which are crucial for emotional self-regulation and stress management.[86]
In addition to structural imaging, a subset of studies utilizing magnetic resonance spectroscopy has investigated the neurometabolic profile within these affected regions. These investigations have focused on the concentrations of various neurometabolites, including N-acetylaspartate, creatine, compounds related to glutamate, and compounds containing choline. These studies aim to show the biochemical alterations that may underlie the symptomatology observed in BPD.[86]
Neurological patterns
Research has shown changes in two brain circuits implicated in the emotional dysregulation characteristic of BPD: firstly, an escalation in activity within brain circuits associated with experiencing severe emotional pain, and secondly, a decreased activation within circuits tasked with the regulation or suppression of these intense emotions. These dysfunctional activations predominantly occur within the limbic system, though individual variances necessitate further neuroimaging research to explore these patterns in detail.[98]
Contrary to earlier findings, individuals with BPD exhibit decreased amygdala activation in response to heightened negative emotional stimuli compared to control groups. John Krystal, the editor of Biological Psychiatry, commented on these findings, suggesting they contribute to understanding the innate neurological predisposition of individuals with BPD to lead emotionally turbulent lives, which are not inherently negative or unproductive.[98] This emotional volatility is consistently linked to disparities in several brain regions, emphasizing the neurobiological underpinnings of BPD.[99]
Mediating and moderating factors
Executive function and social rejection sensitivity
High sensitivity to social rejection is linked to more severe symptoms of BPD, with executive function playing a mediating role.[100] Executive function—encompassing planning, working memory, attentional control, and problem-solving—moderates how rejection sensitivity influences BPD symptoms. Studies demonstrate that individuals with lower executive function exhibit a stronger correlation between rejection sensitivity and BPD symptoms.[100] Conversely, higher executive function may mitigate the impact of rejection sensitivity, potentially offering protection against BPD symptoms.[100]
Diagnosis
The clinical diagnosis of BPD can be made through a psychiatric assessment conducted by a mental health professional, ideally a psychiatrist or psychologist. This comprehensive assessment integrates various sources of information to confirm the diagnosis, encompassing the patient's self-reported clinical history, observations made by the clinician during interviews, and corroborative details obtained from family members, friends, and medical records. It is crucial to thoroughly assess patients for co-morbid mental health conditions, substance use disorders, suicidal ideation, and any self-harming behaviors.[101]
An effective approach involves presenting the criteria of the disorder to the individual and inquiring if they perceive these criteria as reflective of their experiences. Involving individuals in the diagnostic process may enhance their acceptance of the diagnosis. Despite the stigma associated with BPD and previous notions of its untreatability, disclosing the diagnosis to individuals is generally beneficial. It provides them with validation and directs them to appropriate treatment options.[47]
The psychological evaluation for BPD typically explores the onset and intensity of symptoms and their impact on the individual's quality of life. Critical areas of focus include suicidal thoughts, self-harm behaviors, and any thoughts of harming others.[102] The diagnosis relies on both the individual's self-reported symptoms and the clinician's observations.[102] To exclude other potential causes of the symptoms, additional assessments may include a physical examination and blood tests, to exclude thyroid disorders or substance use disorders.[102]
There are differing models for classification of personality disorders. While personality disorders, including BPD, are diagnosed as separate entities in the DSM-5; in the ICD-11 classification of personality disorders, they are assessed in terms of severity levels, with trait and pattern specifiers serving to characterize the particular style of pathology.[103] There is also a hybrid model,[104] called the Alternative DSM-5 model for personality disorders, which defines BPD and five other PDs through disorder-specific combinations of pathological traits and areas of overall impairment.[103]
DSM-5
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) has eliminated the multiaxial diagnostic system,[105] integrating all disorders, including personality disorders, into Section II of the manual.[106] For a diagnosis of BPD, an individual must meet five out of nine specified diagnostic criteria.[107][108] The DSM-5 characterizes BPD as a pervasive pattern of instability in interpersonal relationships, self-image, affect, and a significant propensity towards impulsive behavior.[107][108] Marsha Linehan highlights the diagnostic challenges faced by mental health professionals in using the DSM criteria due to the broad range of behaviors they encompass.[109] To mitigate these challenges, Linehan categorizes BPD symptoms into five principal areas of dysregulation: emotions, behavior, interpersonal relationships, sense of self, and cognition.[109]
Moreover, the Alternative DSM-5 Model for Personality Disorders (AMPD), located in Section III of the DSM-5,[110] defines six specific personality disorders – one of them being BPD[111] – in terms of a description of the disorder; the characteristic manner in which the disorder impacts personality functioning, i.e. identity, self-direction, empathy and intimacy (criterion A); as well as a listing and description of the pathological personality traits associated with the disorder (criterion B).[112] In the case of BPD, this necessitates the identification of at least four out of seven maladaptive traits, these being: emotional lability, anxiousness, separation insecurity, depressivity, impulsivity, risk-taking, and hostility, of which at least one must be of the three last mentioned.[113]
International Classification of Diseases (ICD)
The World Health Organization's ICD-11 has replaced the categorical classification of personality disorders in the ICD-10 with a dimensional model containing a unified personality disorder (6D10) with severity specifiers, along with specifiers for prominent personality traits or patterns (6D11).[114] Among these is the borderline pattern (6D11.5), which is similar to the diagnosis of BPD.[115] The borderline pattern specifier is described in the ICD-11 as applicable to "individuals whose pattern of personality disturbance is characterized by a pervasive pattern of instability of interpersonal relationships, self-image, and affects, and marked impulsivity".[116] Borderline personality disorder has been found to be primarily associated with the ICD-11 trait domains of Negative Affectivity (6D11.0) and Disinhibition (6D11.3), reflecting core features such as emotional instability and impulsivity.[117] Previously, the ICD-10 had identified a condition akin to BPD, termed Emotionally unstable personality disorder (EUPD) (F60.3).[118]
The ICD-11 borderline pattern diagnosis has been criticized for being "indissociable" from negative affectivity upon undergoing regression and factor analyses.[119] A study has found that the diagnosis of borderline pattern does not provide additional insight beyond what is captured by other specifiers, positing that it may be redundant.[119] Apart from negative affectivity and disinhibition, research has found "substantial but mixed" associations with the other trait domains, underscoring the heterogeneity of the diagnosis, which aligns with the view of BPD as an "index of global personality pathology and severity, which aligns with the original metaphorical use of the term "borderline" or "borderland"".[117] It is suggested that it "therefore seems reasonable if the borderline pattern serves as a transitional specifier that eventually is phased out in the coming era".[117]
Millon's subtypes
Psychologist Theodore Millon proposed four subtypes of BPD, where individuals with BPD would exhibit none, one, or multiple subtypes.[120]
| Subtype | Features | Traits |
|---|---|---|
| Discouraged borderline | Including avoidant, depressive, and dependant features | Pliant, submissive, loyal, humble; feels vulnerable and in constant jeopardy; feels hopeless, depressed, helpless, and powerless. |
| Impulsive borderline | Including histrionic and antisocial features | Capricious, superficial, flighty, distractible, frenetic, and seductive; fearing loss, becomes agitated, and gloomy and irritable; potentially suicidal. |
| Petulant borderline | Including negativistic features | Negativistic, impatient, restless, as well as stubborn, defiant, sullen, pessimistic, and resentful; easily slighted and quickly disillusioned. |
| Self-destructive borderline | Including depressive and masochistic features | Inward-turning, intropunitively angry; conforming, deferential, and ingratiating behaviors have deteriorated; increasingly high-strung and moody; possibly suicidal. |
Misdiagnosis
Individuals with BPD are subject to misdiagnosis due to various factors, such as the overlap (comorbidity) of BPD symptoms with those of other disorders such as depression, psychotic disorders, PTSD, and bipolar disorder.[121][122] Misdiagnosis of BPD can lead to a range of adverse consequences. Diagnosis plays a crucial role in informing healthcare professionals about the patient's mental health status, guiding treatment strategies, and facilitating accurate reporting of successful interventions.[123] Consequently, misdiagnosis may deprive individuals of access to suitable psychiatric medications or evidence-based psychological interventions tailored to their specific disorders.[124]
Adolescence and prodrome
The onset of BPD symptoms typically occurs during adolescence or early adulthood, with possible early signs in childhood.[125] Predictive symptoms in adolescents include body image issues, extreme sensitivity to rejection, behavioral challenges, non-suicidal self-injury, seeking exclusive relationships, and profound shame.[47] Although many adolescents exhibit these symptoms without developing BPD, those who do are significantly more likely to develop the disorder and potentially face long-term social challenges.[47]
BPD is recognized as a stable and valid diagnosis during adolescence, supported by the DSM-5 and ICD-11.[126][127][128][129] Early detection and treatment of BPD in young individuals are emphasized in national guidelines across various countries, including the US, Australia, the UK, Spain, and Switzerland, highlighting the importance of early intervention.[128][130][131]
Historically, diagnosing BPD during adolescence was met with caution,[128][132][133] due to concerns about the accuracy of diagnosing young individuals,[134][135] the potential misinterpretation of normal adolescent behaviors, stigma, and the stability of personality during this developmental stage.[128] Despite these challenges, research has confirmed the validity and clinical utility of the BPD diagnosis in adolescents,[126][127][128][129] though misconceptions persist among mental health care professionals,[136][137][138] contributing to clinical reluctance in diagnosing and a key barrier to the provision of effective treatment BPD in this population.[136][139][140]
A diagnosis of BPD in adolescence can indicate the persistence of the disorder into adulthood,[141][142] Early diagnosis facilitates the development of effective treatment plans,[141][142] including family therapy, to support adolescents with BPD.[143]
Differential diagnosis and comorbidity
Lifetime co-occurring (comorbid) conditions are prevalent among individuals diagnosed with BPD. Individuals with BPD exhibit higher rates of comorbidity compared to those diagnosed with other personality disorders. These comorbidities include mood disorders (such as major depressive disorder and bipolar disorder), anxiety disorders (including panic disorder, social anxiety disorder, and post-traumatic stress disorder (PTSD)), other personality disorders (notably schizotypal, antisocial, and dependent personality disorder), substance use disorder, eating disorders (anorexia nervosa and bulimia nervosa), attention deficit hyperactivity disorder (ADHD),[144] somatic symptom disorder, and the dissociative disorders.[145] It is advised that a personality disorder diagnosis should be made cautiously during untreated mood episodes or disorders unless a comprehensive lifetime history supports the existence of a personality disorder.[146]
Comorbid Axis I disorders
| Axis I diagnosis | Overall (%) | Male (%) | Female (%) |
|---|---|---|---|
| Mood disorders | 75.0 | 68.7 | 80.2 |
| Major depressive disorder | 32.1 | 27.2 | 36.1 |
| Dysthymia | 9.7 | 7.1 | 11.9 |
| Bipolar I disorder | 31.8 | 30.6 | 32.7 |
| Bipolar II disorder | 7.7 | 6.7 | 8.5 |
| Anxiety disorders | 74.2 | 66.1 | 81.1 |
| Panic disorder with agoraphobia | 11.5 | 7.7 | 14.6 |
| Panic disorder without agoraphobia | 18.8 | 16.2 | 20.9 |
| Social phobia | 29.3 | 25.2 | 32.7 |
| Specific phobia | 37.5 | 26.6 | 46.6 |
| PTSD | 39.2 | 29.5 | 47.2 |
| Generalized anxiety disorder | 35.1 | 27.3 | 41.6 |
| Obsessive–compulsive disorder** | 15.6 | – | – |
| Substance use disorders | 72.9 | 80.9 | 66.2 |
| Any alcohol use disorder | 57.3 | 71.2 | 45.6 |
| Any non-alcohol substance use disorder | 36.2 | 44.0 | 29.8 |
| Eating disorders** | 53.0 | 20.5 | 62.2 |
| Anorexia nervosa** | 20.8 | 7 * | 25 * |
| Bulimia nervosa** | 25.6 | 10 * | 30 * |
| Eating disorder not otherwise specified** | 26.1 | 10.8 | 30.4 |
| Somatoform disorders** | 10.3 | 10 * | 10 * |
| Somatization disorder** | 4.2 | – | – |
| Hypochondriasis** | 4.7 | – | – |
| Somatoform pain disorder** | 4.2 | – | – |
| Psychotic disorders** | 1.3 | 1 * | 1 * |
| * Approximate values ** Values from 1998 study[145] – Value not provided by from both studies | |||
A 2008 study stated that 75% of individuals with BPD at some point meet criteria for mood disorders, notably major depression and bipolar I, with a similar percentage for anxiety disorders.[147][non-primary source needed] They found that 73% of individuals with BPD meet criteria for substance use disorders, and about 40% for PTSD.[147] A higher proportion of males meet criteria for substance use disorders, whereas females are more likely to have PTSD and eating disorders.[147] 38% of individuals with BPD were found to meet criteria for ADHD,[144] and 15% for autism spectrum disorder (ASD) in separate studies.[149][non-primary source needed]
Mood disorders
Seventy-five percent (75%) of individuals with BPD concurrently experience mood disorders, notably major depressive disorder (MDD) or bipolar disorder (BD),[46] complicating diagnostic clarity due to overlapping symptoms.[150][151][152] Distinguishing BPD from BD is particularly challenging, as behaviors which are part of diagnostic criteria for both BPD and BD may emerge during depressive or manic episodes in BD. However, these behaviours are likely to subside as mood normalises in BD to euthymia, but typically are pervasive in BPD.[153]
Differences between BPD and BD mood swings include their duration, with BD episodes typically lasting for at least two weeks at a time,[lower-alpha 1] in contrast to the rapid and transient mood shifts seen in BPD.[153][156][155] Additionally, BD mood changes are generally unresponsive to environmental stimuli, whereas BPD moods are. For example, a positive event might alleviate a depressive mood in BPD, responsiveness not observed in BD.[156] Furthermore, the euphoria in BPD lacks the racing thoughts and reduced need for sleep characteristic of BD,[156] though sleep disturbances have been noted in BPD.[157]
Historically, BPD was considered a milder form of BD,[158][159] or part of the bipolar spectrum. However, distinctions in phenomenology, family history, disease progression, and treatment responses refute a singular underlying mechanism for both conditions.[160] Research indicates only a modest association between BPD and BD, challenging the notion of a close spectrum relationship.[161][162]
Premenstrual dysphoric disorder
BPD is a psychiatric condition distinguishable from premenstrual dysphoric disorder (PMDD), despite some symptom overlap. BPD affects individuals persistently across all stages of the menstrual cycle, unlike PMDD, which is confined to the luteal phase and ends with menstruation.[163][164] While PMDD, affecting 3–8% of women,[165] includes mood swings, irritability, and anxiety tied to the menstrual cycle, BPD presents a broader, constant emotional and behavioral challenge irrespective of hormonal changes.
Comorbid personality disorders
Approximately 74% of individuals with BPD also fulfill criteria for another personality disorder during their lifetime, according to research conducted in 2008.[147] The most prevalent co-occurring disorders are from Cluster A (paranoid, schizoid, and schizotypal personality disorders), affecting about half of those with BPD, with schizotypal personality disorder alone impacting one-third of individuals. Being part of Cluster B, BPD patients also commonly share characteristics with other Cluster B disorders (antisocial, histrionic, and narcissistic personality disorders), with nearly half of individuals with BPD showing signs of these conditions, and narcissistic personality disorder affecting roughly one-third.[147] Cluster C disorders (avoidant, dependent, and obsessive-compulsive personality disorders) have the least comorbidity with BPD, with just under a third of individuals with BPD meeting the criteria for a Cluster C disorder.[147]
Management
The main approach to managing BPD is through psychotherapy, tailored to the individual's specific needs rather than applying a one-size-fits-all model based on the diagnosis alone.[25] While medications do not directly treat BPD, they are beneficial in managing comorbid conditions like depression and anxiety.[166] Evidence states short-term hospitalization does not offer advantages over community care in terms of enhancing outcomes or in the long-term prevention of suicidal behavior among individuals with BPD.[167]
Psychotherapy
Long-term, consistent psychotherapy stands as the preferred method for treating BPD, and engagement in any therapeutic approach tends to surpass the absence of treatment, particularly in diminishing self-harm impulses.[168] Among the effective psychotherapeutic approaches, dialectical behavior therapy (DBT), schema therapy, and psychodynamic therapies have shown efficacy, although improvements may require extensive time, often years of dedicated effort.[169]
Available treatments for BPD include dynamic deconstructive psychotherapy (DDP),[170] mentalization-based treatment (MBT), schema therapy, transference-focused psychotherapy, dialectical behavior therapy (DBT), and general psychiatric management.[47][171] The effectiveness of these therapies does not significantly vary between more intensive and less intensive approaches.[172]
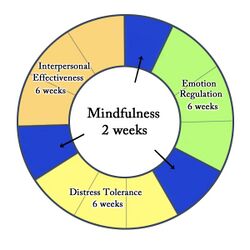
Transference-focused psychotherapy is designed to mitigate absolutist thinking by encouraging individuals to express their interpretations of social interactions and their emotions, thereby fostering more nuanced and flexible categorizations.[173] Dialectical behavior therapy (DBT), on the other hand, focuses on developing skills in four main areas: interpersonal communication, distress tolerance, emotional regulation, and mindfulness, aiming to equip individuals with BPD with tools to manage intense emotions and improve interpersonal relationships.[173][174][171]
Cognitive behavioral therapy (CBT) targets the modification of behaviors and beliefs through problem identification related to BPD, showing efficacy in reducing anxiety, mood symptoms, suicidal ideation, and self-harming actions.[5]
Mentalization-based therapy and transference-focused psychotherapy draw from psychodynamic principles, while DBT is rooted in cognitive-behavioral principles and mindfulness.[168] General psychiatric management integrates key aspects from these treatments and is seen as more accessible and less resource-intensive.[47] Studies suggest DBT and MBT may be particularly effective, with ongoing research into developing abbreviated forms of these therapies to enhance accessibility and reduce both financial and resource burdens on patients and providers.[175][176][168]
Schema therapy considers early maladaptive schemas, conceptualized as organized patterns that recur throughout life in response to memories, emotions, bodily sensations, and cognitions associated with unmet childhood needs.[177]
Additionally, mindfulness meditation has been associated with positive structural changes in the brain and improvements in BPD symptoms, with some participants in mindfulness-based interventions no longer meeting the diagnostic criteria for BPD after treatment.[178][179][180][181]
Medications
There are no clear pharmacological guidelines for borderline personality disorder; psychotherapy is considered the primary treatment, with medications used cautiously for common comorbidities.[29]
Recent randomized controlled trials show little evidence supporting medications like fluoxetine or lamotrigine for borderline personality disorder, highlighting a gap between common prescribing practices and current evidence.[27]
Ketamine for unresponsive depression in BPD requires further research.[182]
Despite the lack of solid evidence, SSRIs and SNRIs are prescribed off-label for BPD[27][29] and are typically considered adjunctive to psychotherapy.[29]
Pharmacological treatments appear to have minimal impact on brain activity and connectivity in borderline personality disorder patients during emotional processing, suggesting that observed neural alterations are largely independent of medication effects.[28]
Health care services
The disparity between those benefiting from treatment and those receiving it, known as the "treatment gap," arises from several factors. These include reluctance to seek treatment, healthcare providers' underdiagnosis, and limited availability and accessibility to advanced treatments.[183] Furthermore, establishing clear pathways to services and medical care remains a challenge, complicating access to treatment for individuals with BPD. Despite efforts, many healthcare providers lack the training or resources to address severe BPD effectively, an issue acknowledged by both affected individuals and medical professionals.[184]
In the context of psychiatric hospitalizations, individuals with BPD constitute approximately 20% of admissions.[185] While many engage in outpatient treatment consistently over several years, reliance on more restrictive and expensive treatment options, such as inpatient admission, tends to decrease over time.[186]
Service experiences vary among individuals with BPD.[187] Assessing suicide risk poses a challenge for clinicians, with patients underestimating the lethality of self-harm behaviors. The suicide risk among people with BPD is significantly higher than that of the general population, characterized by a history of multiple suicide attempts during crises.[188] About half of all individuals who commit suicide are diagnosed with a personality disorder, with BPD being the most common association.[189]
Problems in treatment
People with BPD are considered to be among the most challenging groups of patients to work with in therapy, requiring a high level of skill and training for the psychiatrists, therapists, and nurses involved in their treatment.[190] A majority of psychiatric staff report finding individuals with BPD moderately to extremely difficult to work with and more difficult than other client groups.[191] This largely negative view of BPD can result in people with BPD being terminated from treatment early, being provided harmful treatment, not being informed of their diagnosis of BPD, or being misdiagnosed.[192] Mental health professionals frequently refuse to provide services to those who have received a BPD diagnosis.[193]
With healthcare providers contributing to the stigma of a BPD diagnosis, seeking treatment can often result in the perpetuation of BPD features.[192] Efforts are ongoing to improve public and staff attitudes toward people with BPD.[194][195]
Prognosis
With treatment, the majority of people with BPD can find relief from distressing symptoms and achieve remission, defined as a consistent relief from symptoms for at least two years.[196][197] Remission rates are about 50 to 70% over five years.[198] The remission rate is estimated to be around 50% at 10 years, with 93% of people being able to achieve a 2-year remission and 86% achieving at least a 4-year remission, with a 30% risk of relapse over 10 years.[199]
Patient personality can play an important role during the therapeutic process, leading to better clinical outcomes. Recent research has shown that BPD patients undergoing dialectical behavior therapy (DBT) exhibit better clinical outcomes correlated with higher levels of the trait of agreeableness in the patient, compared to patients either low in agreeableness or not being treated with DBT. This association was mediated through the strength of a working alliance between patient and therapist; that is, more agreeable patients developed stronger working alliances with their therapists, which, in turn, led to better clinical outcomes.[200]
In addition to recovering from distressing symptoms, people with BPD can also achieve high levels of psychosocial functioning. A longitudinal study tracking the social and work abilities of participants with BPD found that six years after diagnosis, 56% of participants had good function in work and social environments, compared to 26% of participants when they were first diagnosed. Vocational achievement was generally more limited, even compared to those with other personality disorders. However, those whose symptoms had remitted were significantly more likely to have good relationships with a romantic partner and at least one parent, good performance at work and school, a sustained work and school history, and good psychosocial functioning overall.[201]
Epidemiology
BPD has a point prevalence of 1.6%[197] and a lifetime prevalence of 5.9% of the global population.[147][6][5][202][203] Within clinical settings, the occurrence of BPD is 6.4% among urban primary care patients,[204] 9.3% among psychiatric outpatients,[205] and approximately 20% among psychiatric inpatients.[206] Utilization of healthcare resources by individuals with BPD is high.[30] Up to half may show significant improvement in their condition, resulting in ineligibility for diagnosis of BPD, following a ten-year period with appropriate treatment.[6]
Regarding gender distribution, women are diagnosed with BPD three times more frequently than men in clinical environments.[6][202] Nonetheless, epidemiological research in the United States indicates no significant gender difference in the lifetime prevalence of BPD within the general population.[207][147] The relationship between BPD and ethnicity continues to be ambiguous, with divergent findings reported in the United States.[202] The overall prevalence of BPD in the U.S. prison population is thought to be 17%.[208]
Gender
In a clinic, up to 80% of patients are women, but this might not necessarily reflect the gender distribution in the entire population.[209] According to Joel Paris, the primary reason for gender disparities in clinical settings is that women are more likely to develop symptoms that prompt them to seek help. Statistics indicate that twice as many women as men in the community experience depression. Conversely, men more frequently meet criteria for substance use disorder and psychopathy, but tend not to seek treatment as often. Additionally, men and women with similar symptoms may manifest them differently. Men frequently exhibit behaviors such as increased alcohol consumption and criminal activity, while women may internalize anger, leading to conditions like depression and self-harm, such as cutting or overdosing. Hence, the gender gap observed in antisocial personality disorder and borderline personality disorder, which may share similar underlying pathologies but present different symptoms influenced by gender. In a study examining completed suicides among individuals aged 18 to 35, 30% of the suicides were attributed to people with BPD, with a majority being men, and almost none receiving treatment. Similar findings were reported in another study.[66]
Among men diagnosed with BPD, there is also evidence of a higher suicide rate: "men are more than twice as likely as women—18 percent versus 8 percent"—to die by suicide.[210]
There are also sex differences in personality traits and Axis I and II comorbidity.[211] Men with BPD are more likely to use substances recreationally, have explosive temper, high levels of novelty seeking and have (especially) antisocial, narcissistic, passive-aggressive or sadistic personality traits (male BPD being characterised by antisocial overtones[211]). Women with BPD are more likely to have eating, mood, anxiety, and post-traumatic stress disorders.[211]
History

The coexistence of intense, divergent moods within an individual was recognized by Homer, Hippocrates, and Aretaeus, the last describing the vacillating presence of impulsive anger, melancholia, and mania within a single person. Swiss physician Théophile Bonet revived the concept in 1684, and used the term folie maniaco-mélancolique,[215] to describe the phenomenon of unstable moods that followed an unpredictable course. Other writers noted the same pattern, including the American psychiatrist Charles H. Hughes in 1884 and J. C. Rosse in 1890, who called the disorder "borderline insanity".[216] In 1921, Emil Kraepelin identified an "excitable personality" that closely parallels the borderline features outlined in the current concept of BPD.[217]
The idea that there were forms of disorder that were neither psychotic nor simply neurotic began to be discussed in psychoanalytic circles in the 1930s.[218] The first formal definition of borderline disorder is widely acknowledged to have been written by Adolph Stern in 1938.[219][220] He described a group of patients who he felt to be on the borderline between neurosis and psychosis, who very often came from family backgrounds marked by trauma. He argued that such patients would often need more active support than that provided by classical psychoanalytic techniques.
The 1960s and 1970s saw a shift from thinking of the condition as borderline schizophrenia to thinking of it as a borderline affective disorder (mood disorder), on the fringes of bipolar disorder, cyclothymia, and dysthymia. In the DSM-II, stressing the intensity and variability of moods, it was called cyclothymic personality (affective personality).[141] While the term "borderline" was evolving to refer to a distinct category of disorder, psychoanalysts such as Otto Kernberg were using it to refer to a broad spectrum of issues, describing an intermediate level of personality organization[217] between neurosis and psychosis.[221]
After standardized criteria were developed by John Gunderson[222] to distinguish it from mood disorders and other Axis I disorders, BPD became a personality disorder diagnosis in 1980 with the publication of the DSM-III.[197] The diagnosis was distinguished from sub-syndromal schizophrenia, which was termed "schizotypal personality disorder".[221] The DSM-IV Axis II Work Group of the American Psychiatric Association finally decided on the name "borderline personality disorder", which is still in use by the DSM-5.[6] However, the term "borderline" has been described as uniquely inadequate for describing the symptoms characteristic of this disorder.[223]
Psychodynamic theorists have historically offered the most comprehensive theoretical models of BPD. Gunderson emphasized the patient's fundamental interpersonal hypersensitivity, which he viewed as partially genetic.[224] Kernberg sees the disorder as one involving disturbed object relations, marked by an excess of aggression and use of primitive defenses, such as splitting, projection, and projective identification.[225] Gerald Adler, writing from a self psychology perspective, viewed the disorder as resulting from the failure of evocative memory and characterized by an intolerance of aloneness.[226] Masterson hypothesized that the disorder resulted from core developmental problems with separation-individuation.[227] More recently, Mark L. Ruffalo has advanced the hypothesis that BPD is fundamentally a disorder of paradox or self-contradiction.[228]
Etymology
Earlier versions of the DSM—before the multiaxial diagnosis system—classified most people with mental health problems into two categories: the psychotics and the neurotics. Clinicians noted a certain class of neurotics who, when in crisis, appeared to straddle the borderline into psychosis.[229] The term "borderline personality disorder" was coined in American psychiatry in the 1960s. It became the preferred term over several competing names, such as "emotionally unstable character disorder" and "borderline schizophrenia," during the 1970s.[230][231] Borderline personality disorder was included in DSM-III (1980) despite not being universally recognized as a valid diagnosis.[232]
Society and culture
Stigma
The features of BPD include emotional instability, intense and unstable interpersonal relationships, a need for intimacy, and a fear of rejection. As a result, people with BPD often evoke intense emotions in those around them. Pejorative terms to describe people with BPD, such as "difficult", "treatment resistant", "manipulative", "demanding", and "attention seeking", are often used and may become a self-fulfilling prophecy, as the negative treatment of these individuals may trigger further self-destructive behavior.[21]
Since BPD can be a stigmatizing diagnosis even within the mental health community, some survivors of childhood abuse who are diagnosed with BPD are re-traumatized by the negative responses they receive from healthcare providers.[233] Certain experts, like Dr. Gillian Proctor and Dr. Karen Williams, argue it would be better to diagnose these people with post-traumatic stress disorder (PTSD), as this would acknowledge the impact of abuse on their behavior, especially in light of BPD's prevalence in women who have survived sexual assault or abuse, as well as reduce stigma.[234][235] Critics of the PTSD diagnosis argue that it medicalizes abuse rather than addressing the root causes in society.[236] Regardless, a diagnosis of PTSD does not encompass all aspects of the disorder (see brain abnormalities and terminology).
Some clients feel the diagnosis is helpful, allowing them to understand that they are not alone and to connect with others with BPD who have developed helpful coping mechanisms. However, others experience the term "borderline personality disorder" as a pejorative label rather than an informative diagnosis. They report concerns that their self-destructive behavior is incorrectly perceived as manipulative and that the stigma surrounding this disorder limits their access to health care.[237]
Physical violence
The stigma surrounding borderline personality disorder includes the belief that people with BPD are prone to violence toward others.[238] While movies and visual media often sensationalize people with BPD by portraying them as violent, the majority of researchers agree that people with BPD are unlikely to harm others physically.[238] Although people with BPD often struggle with experiences of intense anger, a defining characteristic of BPD is that they direct it inward toward themselves.[239]
One 2020 study found that BPD is individually associated with psychological, physical, and sexual forms of intimate partner violence (IPV), especially amongst men.[240][non-primary source needed] In terms of the AMPD trait facets, hostility (negative affectivity), suspiciousness (negative affectivity) and risk-taking (disinhibition) were most strongly associated with IPV perpetration for the total sample.[240]
In addition, adults with BPD have often experienced abuse in childhood, so many people with BPD adopt a "no-tolerance" policy toward expressions of anger of any kind.[239] Their extreme aversion to violence can cause many people with BPD to overcompensate and experience difficulties being assertive and expressing their needs.[239] This is one reason why people with BPD often choose to harm themselves over potentially causing harm to others.[239][67][238]
Credibility and validity of testimony
The credibility of individuals with personality disorders has been questioned at least since the 1960s.[241]: 2 Two concerns are the incidence of dissociation episodes among people with BPD and the belief that lying is not uncommon in those diagnosed with the condition.[242]
Terminology
Because of concerns around stigma, and because of a move away from the original theoretical basis for the term (see history), there is ongoing debate about renaming borderline personality disorder. While some clinicians agree with the current name, others argue that it should be changed,[243] since many who are labelled with borderline personality disorder find the name unhelpful, stigmatizing, or inaccurate.[243][244]
Alternative suggestions for names include emotional regulation disorder or emotional dysregulation disorder. Impulse disorder and interpersonal regulatory disorder are other valid alternatives, according to John G. Gunderson of McLean Hospital in the United States.[245] Another term suggested by psychiatrist Carolyn Quadrio is post-traumatic personality disorganization (PTPD), reflecting the condition's status as (often) both a form of chronic post-traumatic stress disorder (PTSD) as well as a personality disorder.[91] However, although many with BPD do have traumatic histories, some do not report any traumatic event, which suggests that BPD is not necessarily a trauma spectrum disorder.[246]
The Treatment and Research Advancements National Association for Personality Disorders (TARA-APD) campaigned unsuccessfully to change the name and designation of BPD in DSM-5, published in May 2013, in which the name "borderline personality disorder" remains unchanged, and it is not considered a trauma- and stressor-related disorder.[247]
Media
In literature, characters believed to exhibit signs of BPD include Catherine in Wuthering Heights (1847), Smerdyakov in The Brothers Karamazov (1880), and Harry Haller in Steppenwolf (1927).[248][249][250]
Films have also attempted to portray BPD, with characters in Margot at the Wedding (2007), Mr. Nobody (2009), Cracks (2009),[251] Truth (2013), Wounded (2013), Welcome to Me (2014),[252][253] and Tamasha (2015)[254] all suggested to show traits of the disorder. The behavior of Theresa Dunn in Looking for Mr. Goodbar (1975) is consistent with BPD, as suggested by Robert O. Friedel.[255] Films like Play Misty for Me (1971)[256] and Girl, Interrupted (1999, based on the memoir of the same name) suggest emotional instability characteristic of BPD,[257] while Single White Female (1992) highlights aspects such as identity disturbance and fear of abandonment.[256]: 235 Clementine in Eternal Sunshine of the Spotless Mind (2004) is noted to show classic BPD behavior,[258][259] and Carey Mulligan's portrayal in Shame (2011) is praised for its accuracy regarding BPD characteristics by psychiatrists.[260]
Television series like Crazy Ex-Girlfriend (2015) and the miniseries Maniac (2018) depict characters with BPD.[261] Traits of BPD and narcissistic personality disorders are observed in characters like Cersei and Jaime Lannister from A Song of Ice and Fire (1996) and its TV adaptation Game of Thrones (2011).[262] In The Sopranos (1999), Livia Soprano is diagnosed with BPD,[263] and even the portrayal of Bruce Wayne/Batman in the show Titans (2018) is said to include aspects of the disorder.[264] The animated series BoJack Horseman (2014) also features a main character with symptoms of BPD.[265]
Awareness
Awareness of BPD has been growing, with the U.S. House of Representatives declaring May as Borderline Personality Disorder Awareness Month in 2008.[266] Public figures like South Korean singer-songwriter Lee Sun-mi have opened up about their personal experiences with the disorder, bringing further attention to its impact on individuals' lives.[267]
See also
- Classification of personality disorders
- Identity disturbance
- Otto Kernberg
Notes
Citations
- ↑ A Dictionary of Hallucinations (1st ed.). New York: Springer. 2010. p. 74. ISBN 978-1-4419-1223-7. https://books.google.com/books?id=KJtQptBcZloC&pg=PA74. Retrieved 5 June 2020. "Borderline personality disorder (BPD) is also known as emotional regulation disorder (ERD), emotional intensity disorder (EID), and unstable personality disorder (UPD)."
- ↑ "Hysteria". Apa Psycnet (Taylor & Francis). 2000. doi:10.4324/9780203361085. ISBN 978-1-136-88680-5. https://psycnet.apa.org/record/2000-07204-000. Retrieved December 14, 2022.
- ↑ "Historical roots of histrionic personality disorder". Frontiers in Psychology 6 (1463): 1463. 25 September 2015. doi:10.3389/fpsyg.2015.01463. PMID 26441812.
- ↑ "ICD-11 – ICD-11 for Mortality and Morbidity Statistics". World Health Organization. https://icd.who.int/browse11/l-m/en#/http%3a%2f%2fid.who.int%2ficd%2fentity%2f953246526.
- ↑ 5.00 5.01 5.02 5.03 5.04 5.05 5.06 5.07 5.08 5.09 5.10 5.11 "Borderline Personality Disorder". https://www.nimh.nih.gov/health/topics/borderline-personality-disorder.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 6.12 American Psychiatric Association 2013, pp. 645, 663–6
- ↑ Skodol, Andrew E; Siever, Larry J; Livesley, W.John; Gunderson, John G; Pfohl, Bruce; Widiger, Thomas A (2002). "The borderline diagnosis II: biology, genetics, and clinical course". Biological Psychiatry 51 (12): 951–963. doi:10.1016/S0006-3223(02)01325-2. PMID 12062878.
- ↑ Skodol, Andrew E.; Bender, Donna S.; Pagano, Maria E.; Shea, M. Tracie; Yen, Shirley; Sanislow, Charles A.; Grilo, Carlos M.; Daversa, Maria T. et al. (2007-07-15). "Positive Childhood Experiences: Resilience and Recovery From Personality Disorder in Early Adulthood". The Journal of Clinical Psychiatry 68 (7): 1102–1108. doi:10.4088/JCP.v68n0719. ISSN 0160-6689. PMID 17685749.
- ↑ Zanarini, Mary C.; Frankenburg, Frances R.; Hennen, John; Reich, D. Bradford; Silk, Kenneth R. (2006). "Prediction of the 10-Year Course of Borderline Personality Disorder". American Journal of Psychiatry 163 (5): 827–832. doi:10.1176/ajp.2006.163.5.827. ISSN 0002-953X. PMID 16648323.
- ↑ Zanarini, Mary C.; Frankenburg, Frances R.; Reich, D. Bradford; Fitzmaurice, Garrett (2010). "Time to Attainment of Recovery From Borderline Personality Disorder and Stability of Recovery: A 10-year Prospective Follow-Up Study". American Journal of Psychiatry 167 (6): 663–667. doi:10.1176/appi.ajp.2009.09081130. ISSN 0002-953X. PMID 20395399.
- ↑ Zanarini, Mary C.; Frankenburg, Frances R.; Reich, D. Bradford; Fitzmaurice, Garrett (2012). "Attainment and Stability of Sustained Symptomatic Remission and Recovery Among Patients With Borderline Personality Disorder and Axis II Comparison Subjects: A 16-Year Prospective Follow-Up Study". American Journal of Psychiatry 169 (5): 476–483. doi:10.1176/appi.ajp.2011.11101550. ISSN 0002-953X. PMID 22737693.
- ↑ 12.0 12.1 12.2 12.3 "Borderline Personality Disorder". https://www.nimh.nih.gov/health/topics/borderline-personality-disorder.
- ↑ "Borderline personality disorder and emotion dysregulation". Development and Psychopathology (Cambridge University Press) 31 (3): 1143–1156. August 2019. doi:10.1017/S0954579419000658. PMID 31169118. https://www.cambridge.org/core/product/identifier/S0954579419000658/type/journal_article. Retrieved 5 April 2020.
- ↑ "The Role of Trauma in Early Onset Borderline Personality Disorder: A Biopsychosocial Perspective". Frontiers in Psychiatry 12. 23 September 2021. doi:10.3389/fpsyt.2021.721361. PMID 34630181.
- ↑ "Borderline personality disorder and childhood trauma: exploring the affected biological systems and mechanisms". BMC Psychiatry 17 (1). June 2017. doi:10.1186/s12888-017-1383-2. PMID 28619017. "[BPD] is a pervasive pattern of emotional dysregulation, impulsiveness, unstable sense of identity and difficult interpersonal relationships. [Prevalence is 0.2–1.8% for general community, 15–25% among] psychiatric inpatients and 10% of all psychiatric outpatients. [Linehan (1993) proposed BPD to] be the result of [...] biologically based temperamental vulnerabilities and [adverse/traumatic childhood experiences]. Several studies have shown that a diagnosis of BPD is associated with child abuse and neglect more than any other personality disorders, with a range between 30 and 90% in BPD patients.".
- ↑ "Borderline Personality Disorder". The National Institute of Mental Health. December 2017. https://www.nimh.nih.gov/health/topics/borderline-personality-disorder. "Other signs or symptoms may include: [...] Impulsive and often dangerous behaviors [...] Self-harming behavior [...]. Borderline personality disorder is also associated with a significantly higher rate of self-harm and suicidal behavior than the general public."
- ↑ "Alcohol Use Disorder and Antisocial and Borderline Personality Disorders". Alcohol Research: Current Reviews 40 (1). 2019. doi:10.35946/arcr.v40.1.05. PMID 31886107.
- ↑ Trull, Timothy J.; Freeman, Lindsey K.; Vebares, Tayler J.; Choate, Alexandria M.; Helle, Ashley C.; Wycoff, Andrea M. (19 September 2018). "Borderline personality disorder and substance use disorders: an updated review" (in en). Borderline Personality Disorder and Emotion Dysregulation 5 (1): 15. doi:10.1186/s40479-018-0093-9. ISSN 2051-6673. PMID 30250740.
- ↑ Sometimes I Act Crazy. Living With Borderline Personality Disorder. Wiley & Sons. 2004. p. 206. ISBN 978-0-471-22286-6. https://archive.org/details/sometimesiactcra00jero.
- ↑ Kaurin, Aleksandra; Dombrovski, Alexandre; Hallquist, Michael; Wright, Aidan (2020-12-10). "Momentary Interpersonal Processes of Suicidal Surges in Borderline Personality Disorder". Psychological Medicine 52 (13): 2702–2712. doi:10.1017/S0033291720004791. PMID 33298227. "People diagnosed with borderline personality disorder (BPD) are at high risk of dying by suicide: almost all report chronic suicidal ideation, 84% of patients with BPD engage in suicidal behavior, 70% attempt suicide, with a mean of 3.4 lifetime attempts per individual, and 5–10% die by suicide (Black et al., 2004; McGirr et al., 2007; Soloff et al., 1994).".
- ↑ 21.0 21.1 "Borderline personality disorder, stigma, and treatment implications". Harvard Review of Psychiatry 14 (5): 249–256. 2006. doi:10.1080/10673220600975121. PMID 16990170. https://static1.squarespace.com/static/5e7bbc0adb05de74ea06f6a0/t/5ea1c293f38c3a5c41f7ed9e/1587659411794/Aviram+BPD+and+Stigma+Har+Rev+Psychiatry.pdf. Retrieved 2024-12-24. "The stigmatization of BPD is likely to be a result of several characteristics of the BPD syndrome. [... Pejorative] terms such as "difficult," "treatment resistant," "manipulative," "demanding," and "attention seeking" [are used to describe such individuals. This] can have an impact upon the treater's a priori expectations. [... Such] stigmatization is likely to be a result of several [behaviour characteristics of individuals with BPD, and the fact that] psychotherapy with [them] may involve disturbing and frightening behavior, including intense anger, chronic suicidal ideation, self-injury, and suicide attempts. [... Clinicians, under the stigma, may] see lower levels of [their patient's] functioning as deliberate and within [ones] control, or as manipulation, or as a rejection of help, [and may therefore respond] in unintentially damaging ways, [possibly by withdrawing] physically and emotionally. [...] It has been found that when one person has negative expectations of another, the former changes his or her behavior toward the latter. These interpersonal situations have been described as self-fulfilling prophecies.".
- ↑ 22.0 22.1 "Emotional Processes in Borderline Personality Disorder: An Update for Clinical Practice". Journal of Psychotherapy Integration 27 (4): 425–438. 2017. doi:10.1037/int0000044. PMID 29527105. "[Clinicians] may hesitate to [provide treatment for BPD patients] due to discomfort working with the high-risk behaviours and intense interpersonal and emotional dysregulation typical of [the disorder. Treatments supported by empirical evidence include Dialectical behavior therapy, Mentalization-based treatment, Transference-focused psychotherapy, Schema-focused therapy, and General Psychiatric Management... On the psychopathology side, it's possible that] emotional reactivity may be [more] pronounced [...] in response to social stressors and in interpersonal and self-conscious emotions (e.g., anger, shame) [...] Emotional vulnerability in BPD may also vary across specific emotions, [to which] sadness, hostility, and fear [are particularly damaging].".
- ↑ Clinical Practice Guideline for the Management of Borderline Personality Disorder. Melbourne: National Health and Medical Research Council. 2013. pp. 40–41. ISBN 978-1-86496-564-3. "In addition to the evidence identified by the systematic review, the Committee also considered a recent narrative review of studies that have evaluated biological and environmental factors as potential risk factors for BPD (including prospective studies of children and adolescents, and studies of young people with BPD)"
- ↑ Chapman, Jennifer; Jamil, Radia T.; Fleisher, Carl; Torrico, Tyler J. (2025), "Borderline Personality Disorder", StatPearls (Treasure Island, Fla.: StatPearls Publishing), PMID 28613633, https://www.ncbi.nlm.nih.gov/books/NBK430883/, retrieved 2025-06-10, "The current hypothesis is that BPD is caused by an interaction between genetic factors and adverse childhood experiences affecting brain development via neuropeptides and hormones. The relative importance of these factors is unclear."
- ↑ 25.0 25.1 "Borderline personality disorder". Lancet 377 (9759): 74–84. January 2011. doi:10.1016/s0140-6736(10)61422-5. PMID 21195251. "The causes are not yet clear. Genetic factors and adverse life events seem to interact to lead to the disorder. Neurobiological research suggests that abnormalities in the frontolimbic networks are associated with many of the symptoms. Data for the effectiveness of pharmacotherapy vary, and evidence is not yet robust. Specific forms of psychotherapy seem to be beneficial for at least some of the problems frequently reported in [BPD] patients [... As of 2011,] there is no evidence to suggest that one specific form of psychotherapy is more effective than another.".
- ↑ Amad, Ali; Ramoz, Nicolas; Thomas, Pierre; Jardri, Renaud; Gorwood, Philip (2014-03-01). "Genetics of borderline personality disorder: Systematic review and proposal of an integrative model". Neuroscience & Biobehavioral Reviews 40: 6–19. doi:10.1016/j.neubiorev.2014.01.003. ISSN 0149-7634. PMID 24456942. https://www.sciencedirect.com/science/article/pii/S0149763414000062. "[We] performed a systematic review of the literature concerning the genetics of BPD, including familial and twin studies, association studies, and gene–environment interaction studies. [...] Familial and twin studies largely support the potential role of a genetic vulnerability at the root of BPD, with an estimated heritability of approximately 40%. [There] is evidence for both gene–environment interactions and correlations. However, association studies for BPD are sparse, making it difficult to draw clear conclusions.".
- ↑ 27.0 27.1 27.2 "Pharmacotherapy for Borderline Personality Disorder: an Update of Published, Unpublished and Ongoing Studies". Current Psychiatry Reports 22 (37). 2020. doi:10.1007/s11920-020-01164-1. PMID 32504127. PMC 7275094. https://link.springer.com/content/pdf/10.1007/s11920-020-01164-1.pdf. Retrieved 30 May 2021. "[To evaluate continued drug treatments in people with a diagnosis of BPD,] we identified seven new RCTs [randomized controlled trials] and newly available data for an older RCT [...] The new findings do not support fluoxetine as a treatment option for suicide and self-harm prevention. A large effectiveness study did not detect beneficial effects of lamotrigine in routine care. The prevalent use of medications in BPD is still not reflected or supported by the current evidence. More research is needed regarding [...] SSRIs [and] quetiapine, but also with respect to [individuals with BPD and other] distinct comorbid conditions.".
- ↑ 28.0 28.1 "Effects of pharmacological treatments on emotional tasks in borderline personality disorder: A review of functional magnetic resonance imaging studies". Journal of Affective Disorders 288: 50–57. June 2021. doi:10.1016/j.jad.2021.03.088. PMID 33839558.
- ↑ 29.0 29.1 29.2 29.3 "Pharmacological Management of Borderline Personality Disorder and Common Comorbidities". CNS Drugs 37 (6): 489–497. 31 May 2023. doi:10.1007/s40263-023-01015-6. PMID 37256484. "Comorbidity with other mental disorders is common in individuals with BPD [... Despite no drug has been approved specifically for the treatment of BPD,] various medications are routinely prescribed off label [, but] agreement among clinical guidelines [is lacking]. Comorbidity [of] other psychiatric disorders is considered [the] main [reason for the effectiveness of] pharmacological treatment and polypharmacy[. Patients receiving] BPD-specific psychotherapy usually require fewer medications[.]".
- ↑ 30.0 30.1 "Borderline personality disorder: resource utilisation costs in Ireland". Irish Journal of Psychological Medicine 38 (3): 169–176. September 2021. doi:10.1017/ipm.2018.30. PMID 34465404.
- ↑ 31.0 31.1 Ellison, William D.; Rosenstein, Lia K.; Morgan, Theresa A.; Zimmerman, Mark (2018-10-16). "Community and Clinical Epidemiology of Borderline Personality Disorder" (in en). Psychiatric Clinics of North America 41 (4): 561–573. doi:10.1016/j.psc.2018.07.008. PMID 30447724. https://digitalcommons.trinity.edu/cgi/viewcontent.cgi?article=1149&context=psych_faculty. "BPD tends to be more prevalent in adult women than adult men, [but] this gender split is not apparent among adolescents. [...] BPD has been found to decrease and even remit as individuals age. [...] BPD [has] a point prevalence around 1%. [Prevalence differ between subpopulations, being] substantially higher [for psychiatric population, around 12% for outpatient and 22% for inpatient.] Research also suggests [potential] differences [between] ethnic groups[. Deliberate] self-harm [...] differs among ethnic groups, [with] African-American individuals [reporting] more affective instability and emotion dysregulation, but less suicidal behavior and deliberate self-harm, than White American individuals with the disorder.".
- ↑ "Borderline personality disorder: ontogeny of a diagnosis". The American Journal of Psychiatry 166 (5): 530–539. May 2009. doi:10.1176/appi.ajp.2009.08121825. PMID 19411380.
- ↑ Smith, Melinda; Segal, Jeanne (2 November 2018). "Borderline Personality Disorder". https://www.helpguide.org/mental-health/personality-disorders/borderline-personality-disorder.
- ↑ ((DSM-5 Task Force)) (2013). Diagnostic and Statistical Manual of Mental Disorders: DSM-5. American Psychiatric Association. ISBN 978-0-89042-554-1. OCLC 863153409.
- ↑ Carpenter, Ryan W.; Trull, Timothy J. (2012-12-13). "Components of Emotion Dysregulation in Borderline Personality Disorder: A Review" (in en). Current Psychiatry Reports 15 (1). doi:10.1007/s11920-012-0335-2. ISSN 1535-1645. PMID 23250816.
- ↑ Multiple sources:
- Carpenter, Ryan W.; Trull, Timothy J. (2012-12-13). "Components of Emotion Dysregulation in Borderline Personality Disorder: A Review" (in en). Current Psychiatry Reports 15 (1): 1. doi:10.1007/s11920-012-0335-2. ISSN 1535-1645. PMID 23250816.
- Glenn, Catherine R.; Klonsky, E. David (2009). "Emotion Dysregulation as a Core Feature of Borderline Personality Disorder". Journal of Personality Disorders 23 (1): 21. doi:10.1521/pedi.2009.23.1.20. ISSN 0885-579X. PMID 19267659. https://guilfordjournals.com/doi/abs/10.1521/pedi.2009.23.1.20.
- Ebner-Priemer, Ulrich W.; Houben, Marlies; Santangelo, Philip; Kleindienst, Nikolaus; Tuerlinckx, Francis; Oravecz, Zita; Verleysen, Gregory; Van Deun, Katrijn et al. (2015). "Unraveling affective dysregulation in borderline personality disorder: A theoretical model and empirical evidence." (in en). Journal of Abnormal Psychology 124 (1): 187–189. doi:10.1037/abn0000021. ISSN 1939-1846. PMID 25603359. https://doi.apa.org/doi/10.1037/abn0000021.
- Bayes, Adam; Parker, Gordon; McClure, Georgia (2016-11-01). "Emotional dysregulation in those with bipolar disorder, borderline personality disorder and their comorbid expression". Journal of Affective Disorders 204: 104. doi:10.1016/j.jad.2016.06.027. ISSN 0165-0327. PMID 27344618. https://www.sciencedirect.com/science/article/pii/S0165032716305183.
- Fitzpatrick, Skye; Dixon-Gordon, Katherine L.; Turner, Cassandra J.; Chen, Spencer X.; Chapman, Alexander (2023-05-01). "Emotion Dysregulation in Personality Disorders" (in en). Current Psychiatry Reports 25 (5): 224. doi:10.1007/s11920-023-01418-8. ISSN 1535-1645. PMID 37036627.
- ↑ 37.0 37.1 Chapman, Alexander L. (2019-06-06). "Borderline personality disorder and emotion dysregulation" (in en). Development and Psychopathology 31 (3): 1143–1156. doi:10.1017/S0954579419000658. ISSN 0954-5794. PMID 31169118. https://www.cambridge.org/core/journals/development-and-psychopathology/article/abs/borderline-personality-disorder-and-emotion-dysregulation/EA2CB1C041307A34392F49279C107987.
- ↑ Bayes, Adam; Parker, Gordon; McClure, Georgia (2016). "Emotional dysregulation in those with bipolar disorder, borderline personality disorder and their comorbid expression" (in en). Journal of Affective Disorders 204: 103–111. doi:10.1016/j.jad.2016.06.027. PMID 27344618. https://linkinghub.elsevier.com/retrieve/pii/S0165032716305183.
- ↑ 39.0 39.1 39.2 Fitzpatrick, Skye; Dixon-Gordon, Katherine L.; Turner, Cassandra J.; Chen, Spencer X.; Chapman, Alexander (2023-05-01). "Emotion Dysregulation in Personality Disorders" (in en). Current Psychiatry Reports 25 (5): 223–231. doi:10.1007/s11920-023-01418-8. ISSN 1535-1645. PMID 37036627.
- ↑ Glenn, Catherine R.; Klonsky, E. David (2009). "Emotion Dysregulation as a Core Feature of Borderline Personality Disorder". Journal of Personality Disorders 23 (1): 20–28. doi:10.1521/pedi.2009.23.1.20. ISSN 0885-579X. PMID 19267659. https://guilfordjournals.com/doi/abs/10.1521/pedi.2009.23.1.20.
- ↑ Sicorello, Maurizio; Schmahl, Christian (2021). "Emotion dysregulation in borderline personality disorder: A fronto–limbic imbalance?" (in en). Current Opinion in Psychology 37: 114–120. doi:10.1016/j.copsyc.2020.12.002. PMID 33422855. https://linkinghub.elsevier.com/retrieve/pii/S2352250X20302128.
- ↑ "Interpersonal Problems and Negative Affect in Borderline Personality and Depressive Disorders in Daily Life". Clinical Psychological Science (Sage Publishing) 5 (3): 470–484. 2017. doi:10.1177/2167702616677312. PMID 28529826. "[We] assessed the relations between momentary negative affect (hostility, sadness, fear) and interpersonal problems (rejection, disagreement) in a sample of 80 BPD and 51 depressed outpatients at 6 time-points over 28 days [...] Results revealed a mutually reinforcing relationship between disagreement and hostility, rejection and hostility, and between rejection and sadness in both groups, at the momentary and day level. The mutual reinforcement between hostility and rejection/disagreement was significantly stronger in the BPD group.".
- ↑ "Introduction to special issue: cognition and emotion in borderline personality disorder". Journal of Behavior Therapy and Experimental Psychiatry 36 (3): 167–72. September 2005. doi:10.1016/j.jbtep.2005.06.001. PMID 16018875.
- ↑ Linehan 1993, p. 146
- ↑ "What Is BPD: Symptoms". http://www.borderlinepersonalitydisorder.com/understading-bpd/.
- ↑ 46.0 46.1 Disordered Personalities. Rapid Psychler Press. 2005. pp. 255–310. ISBN 978-1-894328-09-8.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 47.7 "Clinical practice. Borderline personality disorder". The New England Journal of Medicine 364 (21): 2037–2042. May 2011. doi:10.1056/NEJMcp1007358. PMID 21612472.
- ↑ "Attachment and borderline personality disorder: implications for psychotherapy". Psychopathology 38 (2): 64–74. 2005. doi:10.1159/000084813. PMID 15802944.
- ↑ "Family relationships of adults with borderline personality disorder". Comprehensive Psychiatry 37 (1): 43–51. 1996. doi:10.1016/S0010-440X(96)90050-4. PMID 8770526.
- ↑ Lester, Rebecca J (February 2013). "Lessons from the borderline: Anthropology, psychiatry, and the risks of being human". Feminism & Psychology 23 (1): 70–77. doi:10.1177/0959353512467969. ISSN 0959-3535. http://journals.sagepub.com/doi/10.1177/0959353512467969.
- ↑ "Borderline personality disorder symptoms as predictors of 4-year romantic relationship dysfunction in young women: addressing issues of specificity". Journal of Abnormal Psychology 109 (3): 451–460. August 2000. doi:10.1037/0021-843X.109.3.451. PMID 11016115.
- ↑ 52.0 52.1 "Patterns of interpersonal behaviors and borderline personality characteristics". Personality and Individual Differences 42 (2): 193–200. 2007-01-01. doi:10.1016/j.paid.2006.06.010. ISSN 0191-8869.
- ↑ "Borderline personality disorder and disability". AAOHN Journal 59 (4): 158–60. April 2011. doi:10.1177/216507991105900401. PMID 21462898.
- ↑ Cameranesi, Margherita (2016). "Battering typologies, attachment insecurity, and personality disorders: A comprehensive literature review". Aggression and Violent Behavior 28: 29–46. doi:10.1016/j.avb.2016.03.005.
- ↑ "Management of borderline personality disorder: a review of psychotherapeutic approaches". World Psychiatry 5 (1): 15–20. February 2006. PMID 16757985.
- ↑ 56.0 56.1 American Psychiatric Association 2000, p. 705
- ↑ "Psychological masculinity, femininity, and tactics of manipulation in patients with borderline personality disorder". Archives of Psychiatry and Psychotherapy (1): 45–53. 2013. ISSN 2083-828X. https://www.researchgate.net/publication/259344581. Retrieved 14 March 2024.
- ↑ 58.0 58.1 Linehan 1993, p. 14
- ↑ Linehan 1993, p. 15
- ↑ 60.0 60.1 60.2 60.3 60.4 Manning 2011, p. 18
- ↑ Giesen-Bloo, J., van Dyck, R., Spinhoven, P., et al. (2006). Outpatient psychotherapy for borderline personality disorder: randomized trial of schema-focused therapy vs transference-focused psychotherapy. Archives of General Psychiatry, 63(6), 649–658. doi:10.1001/archpsyc.63.6.649.
- ↑ 62.0 62.1 "[Borderline personality disorder, self-mutilation and suicide: literature review]" (in fr). L'Encéphale 34 (5): 452–8. October 2008. doi:10.1016/j.encep.2007.10.007. PMID 19068333.
- ↑ "Physical and social pains in borderline disorder and neuroanatomical correlates: a systematic review". Current Psychiatry Reports 16 (5). May 2014. doi:10.1007/s11920-014-0443-2. PMID 24633938.
- ↑ "Suicidality in Borderline Personality Disorder.". Medicina (Kaunas) 55 (6): 223. 2019. doi:10.3390/medicina55060223. PMID 31142033.
- ↑ Borderline Personality Disorder: A Clinical Guide (2nd ed.). American Psychiatric Publishing, Inc. 2008. p. 9. ISBN 978-1-58562-335-8.
- ↑ 66.0 66.1 Treatment of Borderline Personality Disorder. A Guide to Evidence-Based Practice. The Guilford Press. 2008. pp. 21–22.
- ↑ 67.0 67.1 67.2 67.3 "Reasons for suicide attempts and nonsuicidal self-injury in women with borderline personality disorder". Journal of Abnormal Psychology 111 (1): 198–202. February 2002. doi:10.1037/0021-843X.111.1.198. PMID 11866174.
- ↑ Vater, Aline; Schröder, Michela; Weißgerber, Susan; Roepke, Stefan; Schütz, Astrid (March 2015). "Self-concept structure and borderline personality disorder: Evidence for negative compartmentalization". Journal of Behavior Therapy and Experimental Psychiatry (Elsevier) 46: 50–58. doi:10.1016/j.jbtep.2014.08.003. PMID 25222626. https://www.sciencedirect.com/science/article/abs/pii/S0005791614000731. "Borderline personality disorder (BPD) is characterized by an unstable and incongruent self-concept. [...] The results of our study show that patients with BPD exhibit more compartmentalized self-concepts than non-clinical and depressed individuals, i.e., they have difficulties incorporating both positive and negative traits within separate self-aspects.".
- ↑ 69.0 69.1 69.2 Manning 2011, p. 23
- ↑ "Diagnosing borderline personality disorder". CMAJ 184 (16): 1789–1794. November 2012. doi:10.1503/cmaj.090618. PMID 22988153.
- ↑ 71.0 71.1 Manning 2011, p. 24
- ↑ 72.0 72.1 "Autobiographical memory and dissociation in borderline personality disorder". Psychological Medicine 29 (6): 1397–1404. November 1999. doi:10.1017/S0033291799001208. PMID 10616945. https://www.cambridge.org/core/journals/psychological-medicine/article/abs/autobiographical-memory-and-dissociation-in-borderline-personality-disorder/FE4B6F11C259022D29FB3F351FEB9147.
- ↑ "A systematic scoping review of dissociation in borderline personality disorder and implications for research and clinical practice: Exploring the fog". Australian and New Zealand Journal of Psychiatry 56 (10): 1252–1264. 2022-02-13. doi:10.1177/00048674221077029. PMID 35152771.
- ↑ 74.0 74.1 74.2 Pull, Charles B.; Janca, Aleksandar, eds (January 2013). "Psychotic symptoms in patients with borderline personality disorder: prevalence and clinical management". Current Opinion in Psychiatry 26 (1): 113–9. doi:10.1097/YCO.0b013e32835a2ae7. PMID 23168909. "Of patients with BPD about 20–50% report psychotic symptoms. Hallucinations can be similar to those in patients with psychotic disorders in terms of phenomenology, emotional impact, and their persistence over time [...] terms like pseudo-psychotic or quasi-psychotic are misleading and should be avoided [...] and current diagnostic systems might require revision to emphasise psychotic symptoms.".
- ↑ 75.0 75.1 75.2 75.3 "Hallucinations in borderline personality disorder: Prevalence, characteristics and associations with comorbid symptoms and disorders". Scientific Reports 7 (1). October 2017. doi:10.1038/s41598-017-13108-6. PMID 29066713. Bibcode: 2017NatSR...713920N.
- ↑ 76.0 76.1 "Auditory Verbal Hallucinations in Borderline Personality Disorder and the Efficacy of Antipsychotics: A Systematic Review". Frontiers in Psychiatry 9. 31 July 2018. doi:10.3389/fpsyt.2018.00347. PMID 30108529.
- ↑ 77.0 77.1 "Borderline personality disorder". Mayo Clinic. http://www.mayoclinic.com/health/borderline-personality-disorder/DS00442/DSECTION=3.
- ↑ "The phenomenological and conceptual interface between borderline personality disorder and PTSD". The American Journal of Psychiatry 150 (1): 19–27. January 1993. doi:10.1176/ajp.150.1.19. PMID 8417576.
- ↑ "Pathways to the development of borderline personality disorder". Journal of Personality Disorders 11 (1): 93–104. 1997. doi:10.1521/pedi.1997.11.1.93. PMID 9113824.
- ↑ "Past, present, and future of genetic research in borderline personality disorder". Current Opinion in Psychology 21: 60–68. June 2018. doi:10.1016/j.copsyc.2017.09.002. PMID 29032046.
- ↑ "Family Study of Borderline Personality Disorder and Its Sectors of Psychopathology". JAMA: The Journal of the American Medical Association 68 (7): 753–762. August 2011. doi:10.1001/archgenpsychiatry.2011.65. PMID 3150490.
- ↑ "Genetics of patients with borderline personality disorder". The Psychiatric Clinics of North America 23 (1): 1–9. March 2000. doi:10.1016/S0193-953X(05)70139-8. PMID 10729927.
- ↑ 83.0 83.1 "A twin study of personality disorders". Comprehensive Psychiatry 41 (6): 416–425. 2000. doi:10.1053/comp.2000.16560. PMID 11086146.
- ↑ "Trauma, genes, and the neurobiology of personality disorders". Annals of the New York Academy of Sciences 1032 (1): 104–116. December 2004. doi:10.1196/annals.1314.008. PMID 15677398. Bibcode: 2004NYASA1032..104G.
- ↑ 85.0 85.1 85.2 85.3 "Possible Genetic Causes of Borderline Personality Disorder Identified". sciencedaily.com. 20 December 2008. https://www.sciencedaily.com/releases/2008/12/081216114100.htm.
- ↑ 86.0 86.1 86.2 "Brain structure and function in borderline personality disorder". Brain Structure & Function 217 (4): 767–782. October 2012. doi:10.1007/s00429-012-0379-4. PMID 22252376.
- ↑ "Genome-wide analyses of borderline personality features". Molecular Psychiatry 19 (8): 923–929. August 2014. doi:10.1038/mp.2013.109. PMID 23979607.
- ↑ Bassir Nia, Anahita; Eveleth, Matthew C.; Gabbay, Jonathan M.; Hassan, Yonis J.; Zhang, Bosi; Perez-Rodriguez, M. Mercedes (2018). "Past, present, and future of genetic research in borderline personality disorder". Current Opinion in Psychology 21: 60–68. doi:10.1016/j.copsyc.2017.09.002. ISSN 2352-2518. PMID 29032046.
- ↑ "Child Development and Personality Disorder". The Psychiatric Clinics of North America 31 (3): 477–493, vii. September 2008. doi:10.1016/j.psc.2008.03.005. PMID 18638647. http://ereserve.library.utah.edu/Annual/PSY/6330/Crowell/child.pdf. Retrieved 2025-01-08.
- ↑ Trauma and recovery. New York: Basic Books. 1992. ISBN 978-0-465-08730-3. https://archive.org/details/traumarecovery00herm_0.
- ↑ 91.0 91.1 "Axis One/Axis Two: A disordered borderline". Australian and New Zealand Journal of Psychiatry 39: A97–A153. December 2005. doi:10.1111/j.1440-1614.2005.01674_39_s1.x. https://www.researchgate.net/publication/295309096. Retrieved 2025-01-08. Alt URL
- ↑ "Borderline personality disorder and childhood trauma: Evidence for a causal relationship". Current Psychiatry Reports 11 (1): 63–68. February 2009. doi:10.1007/s11920-009-0010-4. PMID 19187711. https://link.springer.com/article/10.1007/s11920-009-0010-4. "[An] association [between childhood trauma and BPD] is consistently shown across studies. [While we] do not dispute that the etiology of BPD is likely [multifactorial, we] argue that [...] childhood trauma plays a role in this model as an etiologic factor.".
- ↑ "Borderline personality disorder: Understanding this challenging mental illness". Mayo Clinic. http://www.mayoclinic.org/diseases-conditions/borderline-personality-disorder/basics/risk-factors/con-20023204.
- ↑ 94.0 94.1 94.2 "Biparental failure in the childhood experiences of borderline patients". Journal of Personality Disorders 14 (3): 264–273. 2000. doi:10.1521/pedi.2000.14.3.264. PMID 11019749. https://guilfordjournals.com/doi/abs/10.1521/pedi.2000.14.3.264.
- ↑ Matthies, Swantje D; Philipsen, Alexandra (2014). "Common ground in Attention Deficit Hyperactivity Disorder (ADHD) and Borderline Personality Disorder (BPD)–review of recent findings" (in en). Borderline Personality Disorder and Emotion Dysregulation 1 (1): 3. doi:10.1186/2051-6673-1-3. ISSN 2051-6673. PMID 26843958.
- ↑ "Attachment and psychopathology in adulthood". Handbook of attachment. New York: Guilford Press. 1999. pp. 497–519.
- ↑ "A Biosocial Developmental Model of Borderline Personality: Elaborating and Extending Linehan's Theory". Psychological Bulletin 135 (3): 495–510. May 2009. doi:10.1037/a0015616. PMID 19379027.
- ↑ 98.0 98.1 "Neural correlates of negative emotionality in borderline personality disorder: an activation-likelihood-estimation meta-analysis". Biological Psychiatry 73 (2): 153–160. January 2013. doi:10.1016/j.biopsych.2012.07.014. PMID 22906520.
- ↑ "Neural correlates of emotion processing in borderline personality disorder". Psychiatry Research 172 (3): 192–199. June 2009. doi:10.1016/j.pscychresns.2008.07.010. PMID 19394205. "BPD patients demonstrated greater differences in activation than controls, when viewing negative pictures compared with rest, in the amygdala, fusiform gyrus, primary visual areas, superior temporal gyrus (STG), and premotor areas, while healthy controls showed greater differences than BPD patients in the insula, middle temporal gyrus and dorsolateral prefrontal cortex.".
- ↑ 100.0 100.1 100.2 "Rejection Sensitivity and Executive Control: Joint predictors of Borderline Personality features". Journal of Research in Personality 42 (1): 151–168. February 2008. doi:10.1016/j.jrp.2007.04.002. PMID 18496604.
- ↑ "Borderline personality disorder: Epidemiology, pathogenesis, clinical features, course, assessment, and diagnosis". UpToDate. Wolters Kluwer. https://www.uptodate.com/contents/borderline-personality-disorder-epidemiology-pathogenesis-clinical-features-course-assessment-and-diagnosis. Retrieved 11 March 2023.
- ↑ 102.0 102.1 102.2 "Personality Disorders: Tests and Diagnosis". Mayo Clinic. http://www.mayoclinic.com/health/personality-disorders/DS00562/DSECTION=tests-and-diagnosis.
- ↑ 103.0 103.1 Clark, Lee Anna (2025-05-01). "Wherefrom and Whither PD? Recent Developments and Future Possibilities in DSM-5 and ICD-11 Personality Disorder Diagnosis" (in en). Current Psychiatry Reports 27 (5): 267–277. doi:10.1007/s11920-025-01602-y. ISSN 1535-1645. PMID 40108080. PMC 12003573. https://doi.org/10.1007/s11920-025-01602-y.
- ↑ Rodriguez-Seijas, Craig; Ruggero, Camilo; Eaton, Nicholas R.; Krueger, Robert F. (2019). "The DSM-5 Alternative Model for Personality Disorders and Clinical Treatment: a Review" (in en). Current Treatment Options in Psychiatry 6 (4): 284–298. doi:10.1007/s40501-019-00187-7. ISSN 2196-3061. https://link.springer.com/10.1007/s40501-019-00187-7.
- ↑ Krueger, Robert F.; Hobbs, Kelsey A. (2020). "An Overview of the DSM-5 Alternative Model of Personality Disorders". Psychopathology 53 (3-4): 126–132. doi:10.1159/000508538. ISSN 0254-4962. PMID 32645701. PMC 7529724. https://doi.org/10.1159/000508538.
- ↑ Gintner, Gary G. (2014). "DSM-5 Conceptual Changes: Innovations, Limitations and Clinical Implications". The Professional Counselor 4 (3): 179–190. doi:10.15241/ggg.4.3.179. http://tpcjournal.nbcc.org/category/pdf-articles/volumes/volume-4/volume-4-issue-3/.
- ↑ 107.0 107.1 Leichsenring, Falk; Fonagy, Peter; Heim, Nikolas; Kernberg, Otto F.; Leweke, Frank; Luyten, Patrick; Salzer, Simone; Spitzer, Carsten et al. (2024). "Borderline personality disorder: a comprehensive review of diagnosis and clinical presentation, etiology, treatment, and current controversies" (in en). World Psychiatry 23 (1): 4–25. doi:10.1002/wps.21156. ISSN 2051-5545. PMID 38214629. "The DSM‐5 characterizes BPD as a pervasive pattern of instability of interpersonal relationships, self‐image and affects, and marked impulsivity, emerging by early adulthood and present in a variety of contexts, as indicated by five or more of a set of nine criteria 27 (see Table 1).".
- ↑ 108.0 108.1 American Psychiatric Association 2013, pp. 663–8
- ↑ 109.0 109.1 Manning 2011, p. 13
- ↑ Rodriguez-Seijas, Craig; Ruggero, Camilo; Eaton, Nicholas R.; Krueger, Robert F. (September 2019). "The DSM-5 Alternative Model for Personality Disorders and Clinical Treatment: a Review" (in en). Current Treatment Options in Psychiatry 6 (4): 284–298. doi:10.1007/s40501-019-00187-7. ISSN 2196-3061. https://link.springer.com/10.1007/s40501-019-00187-7.
- ↑ Christopher Fowler, J.; Sharp, Carla; Kalpakci, Allison; Madan, Alok; Clapp, Joshua; Allen, Jon G.; Christopher Frueh, B.; Oldham, John M. (2015-01-01). "A dimensional approach to assessing personality functioning: examining personality trait domains utilizing DSM-IV personality disorder criteria". Comprehensive Psychiatry 56: 75–84. doi:10.1016/j.comppsych.2014.09.001. ISSN 0010-440X. PMID 25261890. https://www.sciencedirect.com/science/article/pii/S0010440X14002521. "The number of specific PDs was reduced from 10 to 6 (antisocial, avoidant, borderline, narcissistic, obsessive–compulsive, and schizotypal) as well as a diagnosis of "personality disorder—trait specified" that can be made when criteria for a specific disorder are not met, but a personality disorder is assessed as present [23].".
- ↑ Zimmermann, Johannes; Kerber, André; Rek, Katharina; Hopwood, Christopher J.; Krueger, Robert F. (2019-08-13). "A Brief but Comprehensive Review of Research on the Alternative DSM-5 Model for Personality Disorders" (in en). Current Psychiatry Reports 21 (9): 92. doi:10.1007/s11920-019-1079-z. ISSN 1535-1645. PMID 31410586.
- ↑ Hines, Alexandra; Kushner, Madeline L.; Stumpp, Nicole; Semcho, Stephen; Bridges, Eric; Croom, Hannah; Rahman, Abrar; Cecil, Sarah et al. (2024). "Different routes to the same destination? Comparing Diagnostic and Statistical Manual of Mental Disorders, fifth edition Section II- and alternative model of personality disorder-defined borderline personality disorder." (in en). Personality Disorders: Theory, Research, and Treatment 15 (5): 352–360. doi:10.1037/per0000676. ISSN 1949-2723. PMID 39073371. "In the Alternative Model of Personality Disorders (AMPD) presented in Section III (Emerging Measures and Models) of DSM-5, BPD is represented by at least moderate impairment in self (e.g., identity and self-direction) and/ or interpersonal (e.g., empathy and intimacy) functioning (i.e., Criterion A) and at least four of seven trait facets (i.e., Criterion B): emotional lability, anxiousness, separation insecurity, depressivity, impulsivity, risk-taking, and hostility.".
- ↑ Bach, Bo; First, Michael B. (2018-10-29). "Application of the ICD-11 classification of personality disorders". BMC Psychiatry 18 (1): 351. doi:10.1186/s12888-018-1908-3. ISSN 1471-244X. PMID 30373564.
- ↑ Mulder, Roger T. (2021). "ICD-11 Personality Disorders: Utility and Implications of the New Model". Frontiers in Psychiatry 12. doi:10.3389/fpsyt.2021.655548. ISSN 1664-0640. PMID 34040555.
- ↑ Tyrer, Peter; Mulder, Roger; Kim, Youl-Ri; Crawford, Mike J. (2019-05-07). "The Development of the ICD-11 Classification of Personality Disorders: An Amalgam of Science, Pragmatism, and Politics" (in en). Annual Review of Clinical Psychology 15: 481–502. doi:10.1146/annurev-clinpsy-050718-095736. ISSN 1548-5943. PMID 30601688. https://www.annualreviews.org/content/journals/10.1146/annurev-clinpsy-050718-095736.
- ↑ 117.0 117.1 117.2 Simon, Jonatan; Lambrecht, Bastian; Bach, Bo (2023-04-06). "Cross-walking personality disorder types to ICD-11 trait domains: An overview of current findings" (in English). Frontiers in Psychiatry 14. doi:10.3389/fpsyt.2023.1175425. ISSN 1664-0640. PMID 37091704.
- ↑ Lai, Ching Man; Leung, Freedom; You, Jianing; Cheung, Fanny (August 2012). "Are DSM-IV-TR Borderline Personality Disorder, ICD-10 Emotionally Unstable Personality Disorder, and CCMD-III Impulsive Personality Disorder Analogous Diagnostic Categories Across Psychiatric Nomenclatures?" (in en). Journal of Personality Disorders 26 (4): 551–567. doi:10.1521/pedi.2012.26.4.551. ISSN 0885-579X. PMID 22867506. http://guilfordjournals.com/doi/10.1521/pedi.2012.26.4.551. "There is no exact diagnostic label termed as BPD in the tenth edition of International Classification of Diseases (ICD-10; World Health Organization, 1992). After burgeoning evidence regarding the validity of BPD, the ICD has grudgingly introduced a derivative category coined as emotionally unstable personality disorder (EUPD) with the impulsive (EUPD-I) and borderline subtypes (EUPD-B).".
- ↑ 119.0 119.1 "Borderline, where are you? A psychometric approach to the personality domains in the International Classification of Diseases, 11th Revision (ICD-11)". Personality Disorders 14 (3): 355–359. June 2022. doi:10.1037/per0000592. PMID 35737563. "The borderline pattern was a last-minute addendum to the ICD-11 whose accommodation within the diagnostic system of PDs has not yet been studied in depth. In this study, we found that the borderline construct is internally consistent and is a good predictor of severity. However, it shares most of its variance with the five initial ICD-11 domains and cannot be factorially uncoupled from negative affectivity. Furthermore, it adds nothing to the prediction of severity when the other domains are considered. Some of these findings warrant further comment.".
- ↑ Personality Disorders in Modern Life. Hoboken, New Jersey: John Wiley & Sons. 2004. pp. 482–88. ISBN 978-0-471-23734-1.
- ↑ "Prescribing and borderline personality disorder". Australian Prescriber 39 (2): 49–53. April 2016. doi:10.18773/austprescr.2016.019. PMID 27340322.
- ↑ "Borderline Personality Disorder Symptoms in College Students: The Complex Interplay between Alexithymia, Emotional Dysregulation and Rumination". PLOS ONE 11 (6). 2016. doi:10.1371/journal.pone.0157294. PMID 27348858. Bibcode: 2016PLoSO..1157294M.
- ↑ Sartorius, Norman (2015). "Why do we need a diagnosis? Maybe a syndrome is enough?". Dialogues in Clinical Neuroscience 17 (1): 6–7. doi:10.31887/DCNS.2015.17.1/nsartorius. PMID 25987858.
- ↑ Paris, Joel; Black, Donald W. (2015). "Borderline Personality Disorder and Bipolar Disorder". The Journal of Nervous and Mental Disease 203 (1): 3–7. doi:10.1097/nmd.0000000000000225. ISSN 0022-3018. PMID 25536097.
- ↑ Linehan 1993, p. 49
- ↑ 126.0 126.1 "Fact or fiction: diagnosing borderline personality disorder in adolescents". Clinical Psychology Review 28 (6): 969–81. July 2008. doi:10.1016/j.cpr.2008.02.004. PMID 18358579.
- ↑ 127.0 127.1 National Collaborating Centre for Mental Health (UK) (2009). Young People With Borderline Personality Disorder. British Psychological Society. https://www.ncbi.nlm.nih.gov/books/NBK55399/. Retrieved 23 September 2020.
- ↑ 128.0 128.1 128.2 128.3 128.4 "Borderline personality disorder in adolescence". Pediatrics 134 (4): 782–93. October 2014. doi:10.1542/peds.2013-3677. PMID 25246626. https://publications.aap.org/pediatrics/article-pdf/134/4/782/1098814/peds_2013-3677.pdf. Retrieved 23 September 2020.
- ↑ 129.0 129.1 "The Lifetime Course of Borderline Personality Disorder". Canadian Journal of Psychiatry 60 (7): 303–8. July 2015. doi:10.1177/070674371506000702. PMID 26175388.
- ↑ National Health and Medical Research Council (Australia) (2013). Clinical practice guideline for the management of borderline personality disorder. National Health and Medical Research Council. ISBN 978-1-86496-564-3. OCLC 948783298.
- ↑ "Overview | Borderline personality disorder: recognition and management | Guidance | NICE". 28 January 2009. https://www.nice.org.uk/guidance/cg78.
- ↑ "Adolescence and Personality Disorders". Treatment of Personality Disorders. Boston: Springer US. 1999. pp. 77–95. doi:10.1007/978-1-4757-6876-3_7. ISBN 978-1-4419-3326-3. http://link.springer.com/10.1007/978-1-4757-6876-3_7. Retrieved 23 September 2020.
- ↑ "Borderline personality disorder in adolescents: prevalence, diagnosis, and treatment strategies". Adolescent Health, Medicine and Therapeutics 9: 199–210. 23 November 2018. doi:10.2147/ahmt.s156565. PMID 30538595.
- ↑ American Psychiatric Association. Work Group on Borderline Personality Disorder. (2001). Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association. OCLC 606593046.
- ↑ World Health Organization (1992). The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines.. World Health Organization. ISBN 978-92-4-068283-2. OCLC 476159430.
- ↑ 136.0 136.1 "Moving forward: closing the gap between research and practice for young people with BPD". Current Opinion in Psychology 37: 77–81. August 2020. doi:10.1016/j.copsyc.2020.08.008. PMID 32916475.
- ↑ "Diagnosing BPD in Adolescents: More good than harm". Journal of the Canadian Academy of Child and Adolescent Psychiatry 27 (3): 155–156. August 2018. PMID 30038651.
- ↑ "Diagnosis of personality disorders in adolescents: a study among psychologists". Child and Adolescent Psychiatry and Mental Health 7 (1): 3. February 2013. doi:10.1186/1753-2000-7-3. PMID 23398887.
- ↑ "Borderline Personality Disorder in Young People: Are We There Yet?". Journal of Clinical Psychology 71 (8): 778–91. August 2015. doi:10.1002/jclp.22205. PMID 26192914. http://doi.wiley.com/10.1002/jclp.22205. Retrieved 23 September 2020.
- ↑ "Working around a contested diagnosis: borderline personality disorder in adolescence". Health 17 (1): 37–56. January 2013. doi:10.1177/1363459312447253. PMID 22674745.
- ↑ 141.0 141.1 141.2 American Psychiatric Association 2000
- ↑ 142.0 142.1 Child and Adolescent Psychological Disorders: Comprehensive Textbook. New York: Oxford University Press. 1999.
- ↑ Linehan 1993, p. 98
- ↑ 144.0 144.1 "Comorbid attention-deficit/hyperactivity disorder in borderline patients defines an impulsive subtype of borderline personality disorder". Journal of Personality Disorders 24 (6): 812–822. December 2010. doi:10.1521/pedi.2010.24.6.812. PMID 21158602.[non-primary source needed]
- ↑ 145.0 145.1 "Axis I comorbidity of borderline personality disorder". The American Journal of Psychiatry 155 (12): 1733–1739. December 1998. doi:10.1176/ajp.155.12.1733. PMID 9842784.
- ↑ "Bipolar II Disorder: Frequent, Valid, and Reliable". Canadian Journal of Psychiatry. Revue Canadienne de Psychiatrie 64 (8): 541–543. August 2019. doi:10.1177/0706743719855040. PMID 31340672.
- ↑ 147.0 147.1 147.2 147.3 147.4 147.5 147.6 147.7 147.8 "Prevalence, correlates, disability, and comorbidity of DSM-IV borderline personality disorder: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions". The Journal of Clinical Psychiatry 69 (4): 533–545. April 2008. doi:10.4088/JCP.v69n0404. PMID 18426259.
- ↑ "Axis I comorbidity of borderline personality disorder". The American Journal of Psychiatry 155 (12): 1733–1739. December 1998. doi:10.1176/ajp.155.12.1733. PMID 9842784.
- ↑ "Borderline personality disorder and autism spectrum disorder in females: A cross-sectional study". Clinical Neuropsychiatry 5 (1): 22–30. 2008. http://www.clinicalneuropsychiatry.org/pdf/04_ryden_hetta.pdf. Retrieved 7 February 2013.
- ↑ "Distinguishing borderline personality disorder from bipolar disorder: differential diagnosis and implications". The American Journal of Psychiatry 153 (9): 1202–1207. September 1996. doi:10.1176/ajp.153.9.1202. PMID 8780426.
- ↑ American Psychiatric Association Practice Guidelines (October 2001). "Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Association". The American Journal of Psychiatry 158 (10 Suppl): 1–52. doi:10.1176/appi.ajp.158.1.1. PMID 11665545.
- ↑ "Differential Diagnosis of Borderline Personality Disorder". BPD Today. http://www.borderlinepersonalitytoday.com/main/diffdx.htm.
- ↑ 153.0 153.1 153.2 Chapman & Gratz 2007, p. 87
- ↑ "Affective instability as rapid cycling: theoretical and clinical implications for borderline personality and bipolar spectrum disorders". Bipolar Disorders 8 (1): 1–14. February 2006. doi:10.1111/j.1399-5618.2006.00283.x. PMID 16411976.
- ↑ 155.0 155.1 Chapman & Gratz 2007, p. 88
- ↑ 156.0 156.1 156.2 Manic-depressive illness. Oxford: Oxford University Press. 1990. p. 108. ISBN 978-0-19-503934-4. https://archive.org/details/manicdepressivei00good/page/108.
- ↑ "Chronic sleep disturbances and borderline personality disorder symptoms". Journal of Consulting and Clinical Psychology 81 (5): 941–947. October 2013. doi:10.1037/a0033201. PMID 23731205.
- ↑ "The nosologic status of borderline personality: clinical and polysomnographic study". The American Journal of Psychiatry 142 (2): 192–198. February 1985. doi:10.1176/ajp.142.2.192. PMID 3970243.
- ↑ "The interface between borderline personality disorder and affective disorder". The American Journal of Psychiatry 142 (3): 277–788. March 1985. doi:10.1176/ajp.142.3.277. PMID 2857532.
- ↑ "Borderline or bipolar? Distinguishing borderline personality disorder from bipolar spectrum disorders". Harvard Review of Psychiatry 12 (3): 140–145. 2004. doi:10.1080/10673220490472373. PMID 15371068.
- ↑ Manic-depressive illness. Oxford: Oxford University Press. 1990. p. 336. ISBN 978-0-19-503934-4. https://archive.org/details/manicdepressivei00good/page/336.
- ↑ "Borderline personality-bipolar spectrum relationship". Progress in Neuro-Psychopharmacology & Biological Psychiatry 30 (1): 68–74. January 2006. doi:10.1016/j.pnpbp.2005.06.010. PMID 16019119.
- ↑ "The Cerebellum and Premenstrual Dysphoric Disorder". AIMS Neuroscience 1 (2): 120–141. 2014. doi:10.3934/Neuroscience.2014.2.120. PMID 28275721. Bibcode: 2014AIMES...1..120R.
- ↑ "Clinical practice. Premenstrual dysphoric disorder". The New England Journal of Medicine 348 (5): 433–8. January 2003. doi:10.1056/NEJMcp012067. PMID 12556546.
- ↑ "Treatment of premenstrual dysphoric disorder". Women's Health 9 (6): 537–56. November 2013. doi:10.2217/whe.13.62. PMID 24161307.
- ↑ "CG78 Borderline personality disorder (BPD): NICE guideline". Nice.org.uk. 28 January 2009. http://www.nice.org.uk/Guidance/CG78/NiceGuidance/pdf/English.
- ↑ "Is hospitalization useful for suicidal patients with borderline personality disorder?". Journal of Personality Disorders 18 (3): 240–247. June 2004. doi:10.1521/pedi.18.3.240.35443. PMID 15237044.
- ↑ 168.0 168.1 168.2 "Psychotherapy of borderline personality disorder". Acta Psychiatrica Scandinavica 120 (5): 373–377. November 2009. doi:10.1111/j.1600-0447.2009.01448.x. PMID 19807718.
- ↑ "Efficacy of Psychotherapies for Borderline Personality Disorder: A Systematic Review and Meta-analysis". JAMA Psychiatry 74 (4): 319–328. April 2017. doi:10.1001/jamapsychiatry.2016.4287. PMID 28249086. https://research.vu.nl/en/publications/845f5460-273e-4150-b79d-159f37aa36a0. Retrieved 12 December 2019.
- ↑ Psychodynamic psychiatry in clinical practice (5th ed.). Washington, D.C.: American Psychiatric Publishing. 2014. pp. 445–448.
- ↑ 171.0 171.1 "What Works in the Treatment of Borderline Personality Disorder". Current Behavioral Neuroscience Reports 4 (1): 21–30. 2017. doi:10.1007/s40473-017-0103-z. PMID 28331780.
- ↑ "Psychotherapy for Borderline Personality Disorder: Progress and Remaining Challenges". Current Psychiatry Reports 19 (3). March 2017. doi:10.1007/s11920-017-0766-x. PMID 28271272.
- ↑ 173.0 173.1 "An Exploration of Common Elements in Dialectical Behavior Therapy, Mentalization Based Treatment and Transference Focused Psychotherapy in the Treatment of Borderline Personality Disorder". Clinical Social Work Journal 42 (1): 61–69. 1 March 2014. doi:10.1007/s10615-013-0456-z. ISSN 0091-1674.
- ↑ "Understanding Borderline Personality Disorder". Integrated Modular Treatment for Borderline Personality Disorder. Cambridge, England: Cambridge University Press. 2017. pp. 29–38. doi:10.1017/9781107298613.004. ISBN 978-1-107-29861-3. https://zenodo.org/record/4384573. Retrieved 14 March 2024.
- ↑ "Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder". Archives of General Psychiatry 63 (7): 757–766. July 2006. doi:10.1001/archpsyc.63.7.757. PMID 16818865.
- ↑ "Effectiveness of different psychotherapy approaches in the treatment of borderline personality disorder". Current Psychiatry Reports 12 (1): 56–60. February 2010. doi:10.1007/s11920-009-0083-0. PMID 20425311.
- ↑ Young, Jeffrey E; Klosko, Janet S; Weishaar, Marjorie E (2003). "Schema Therapy for Borderline Personality Disorder". Schema Therapy: A Practitioner's Guide. New York: Guilford Press. pp. 306–372. ISBN 978-1-59385-372-3.
- ↑ "Special issue on mindfulness neuroscience". Social Cognitive and Affective Neuroscience 8 (1): 1–3. January 2013. doi:10.1093/scan/nss104. PMID 22956677.
- ↑ "Mechanisms of white matter change induced by meditation training". Frontiers in Psychology 5 (1220): 1220. 2014. doi:10.3389/fpsyg.2014.01220. PMID 25386155.
- ↑ "Beyond borderline personality disorder: the mindful brain". Social Work 59 (4): 297–302. October 2014. doi:10.1093/sw/swu030. PMID 25365830.
- ↑ "A feasibility study of mindfulness-based cognitive therapy for individuals with borderline personality disorder". Psychology and Psychotherapy 84 (2): 184–200. June 2011. doi:10.1348/147608310X516387. PMID 22903856.
- ↑ Kwan, Angela T. H.; Lakhani, Moiz; Singh, Gurkaran; Le, Gia Han; Wong, Sabrina; Teopiz, Kayla M.; Dev, Donovan A.; Manku, Arshpreet Singh et al. (2024-11-20). "Ketamine for the Treatment of Psychiatric Disorders: A Systematic Review and Meta-Analysis". CNS Spectrums 29 (5): 354–361. doi:10.1017/S1092852924000580. ISSN 1092-8529. PMID 39564613.
- ↑ "Treatment of Borderline Personality Disorder". BPDFamily.com. 26 July 2014. http://bpdfamily.com/content/treatment-borderline-personality-disorder.
- ↑ "Key stakeholders' experiences and expectations of the care system for individuals affected by borderline personality disorder: An interpretative phenomenological analysis towards co-production of care". PLOS ONE 17 (9). 2022-09-22. doi:10.1371/journal.pone.0274197. PMID 36137103. Bibcode: 2022PLoSO..1774197F.
- ↑ "Treatment histories of borderline inpatients". Comprehensive Psychiatry 42 (2): 144–150. 2001. doi:10.1053/comp.2001.19749. PMID 11244151.
- ↑ "Mental health service utilization by borderline personality disorder patients and Axis II comparison subjects followed prospectively for 6 years". The Journal of Clinical Psychiatry 65 (1): 28–36. January 2004. doi:10.4088/JCP.v65n0105. PMID 14744165.
- ↑ "Travelling through the system: the lived experience of people with borderline personality disorder in contact with psychiatric services". Journal of Psychiatric and Mental Health Nursing 10 (4): 393–401. August 2003. doi:10.1046/j.1365-2850.2003.00617.x. PMID 12887630.
- ↑ "Assessing Suicide Risk in Patients With Borderline Personality Disorder". Psychiatric Times. Psychiatric Times Vol 21 No 8 21 (8). 1 July 2004. http://www.psychiatrictimes.com/articles/assessing-suicide-risk-patients-borderline-personality-disorder.
- ↑ "Borderline personality disorder". Lancet 364 (9432): 453–461. 2004. doi:10.1016/S0140-6736(04)16770-6. PMID 15288745.
- ↑ "The difficult patient. The role of 'scientific psychiatry' in understanding patients with chronic schizophrenia or severe personality disorder". The British Journal of Psychiatry 174 (3): 187–190. March 1999. doi:10.1192/bjp.174.3.187. PMID 10448440.
- ↑ "Experience, knowledge and attitudes of mental health staff regarding clients with a borderline personality disorder". International Journal of Mental Health Nursing 11 (3): 186–191. September 2002. doi:10.1046/j.1440-0979.2002.00246.x. PMID 12510596.
- ↑ 192.0 192.1 "Borderline Personality Disorder: To diagnose or not to diagnose? That is the question". International Journal of Mental Health Nursing 29 (5): 972–981. 19 May 2020. doi:10.1111/inm.12737. ISSN 1445-8330. PMID 32426937.
- ↑ Manning 2011, p. ix
- ↑ "Attitudes of registered psychiatric nurses towards patients diagnosed with borderline personality disorder". Contemporary Nurse 21 (1): 43–49. 2006. doi:10.5172/conu.2006.21.1.43. PMID 16594881. https://researchonline.federation.edu.au/vital/access/services/Download/vital:236/DS1. Retrieved 16 March 2024.
- ↑ "Borderline personality disorder: attitudinal change following training". The Australian and New Zealand Journal of Psychiatry 38 (7): 554–559. July 2004. doi:10.1111/j.1440-1614.2004.01409.x. PMID 15255829.
- ↑ "The longitudinal course of borderline psychopathology: 6-year prospective follow-up of the phenomenology of borderline personality disorder". The American Journal of Psychiatry 160 (2): 274–283. February 2003. doi:10.1176/appi.ajp.160.2.274. PMID 12562573.
- ↑ 197.0 197.1 197.2 "Borderline Personality Disorder: An Overview". Psychiatric Times. July 2004. http://www.psychiatrictimes.com/articles/borderline-personality-disorder-overview-0.
- ↑ Álvarez-Tomás, Irene; Ruiz, José; Guilera, Georgina; Bados, Arturo (2019). "Long-term clinical and functional course of borderline personality disorder: A meta-analysis of prospective studies". European Psychiatry 56 (1): 75–83. doi:10.1016/j.eurpsy.2018.10.010. PMID 30599336.
- ↑ Leichsenring, Falk; Heim, Nikolas; Leweke, Frank; Spitzer, Carsten; Steinert, Christiane; Kernberg, Otto F. (28 February 2023). "Borderline Personality Disorder: A Review". JAMA 329 (8): 670–679. doi:10.1001/jama.2023.0589. PMID 36853245. "An observational study of 290 patients with BPD reported that over a 10-year period, [...] 93% of BPD patients attained [symptomatic] remission from BPD lasting 2 years and 86% attained remission lasting 4 years. Excellent recovery, defined as remission of BPD or other personality disorders and good social and full-time vocational functioning, occurred in 39% of patients with BPD compared with 73% of patients with other personality disorders.".
- ↑ "The relationship between agreeableness and the development of the working alliance in patients with borderline personality disorder". Journal of Personality Disorders 26 (4): 616–627. August 2012. doi:10.1521/pedi.2012.26.4.616. PMID 22867511.
- ↑ "Psychosocial functioning of borderline patients and axis II comparison subjects followed prospectively for six years". Journal of Personality Disorders 19 (1): 19–29. February 2005. doi:10.1521/pedi.19.1.19.62178. PMID 15899718.
- ↑ 202.0 202.1 202.2 "Borderline personality disorder: Epidemiology, pathogenesis, clinical features, course, assessment, and diagnosis". UpToDate. Wolters Kluwer. https://www.uptodate.com/contents/borderline-personality-disorder-epidemiology-pathogenesis-clinical-features-course-assessment-and-diagnosis. Retrieved 13 March 2024.
- ↑ "NIMH " Personality Disorders". https://www.nimh.nih.gov/health/statistics/personality-disorders.
- ↑ "Borderline personality disorder in primary care". Archives of Internal Medicine 162 (1): 53–60. January 2002. doi:10.1001/archinte.162.1.53. PMID 11784220.
- ↑ "The prevalence of DSM-IV personality disorders in psychiatric outpatients". The American Journal of Psychiatry 162 (10): 1911–1918. October 2005. doi:10.1176/appi.ajp.162.10.1911. PMID 16199838.
- ↑ American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders (DSM-IV).
- ↑ "DSM-IV personality disorders in the National Comorbidity Survey Replication". Biological Psychiatry 62 (6): 553–564. September 2007. doi:10.1016/j.biopsych.2006.09.019. PMID 17217923.
- ↑ "BPD Fact Sheet". National Educational Alliance for Borderline Personality Disorder. 2013. http://www.borderlinepersonalitydisorder.com/understading-bpd/bpd-fact-sheet/.
- ↑ Treatment of Borderline Personality Disorder: A Guide to Evidence-Based Practice. The Guilford Press. 2008. p. 21.
- ↑ Sometimes I Act Crazy. Living With Borderline Personality Disorder. Wiley & Sons. 2004. p. 206. ISBN 978-0-471-22286-6. https://archive.org/details/sometimesiactcra00jero.
- ↑ 211.0 211.1 211.2 "Gender patterns in borderline personality disorder". Innovations in Clinical Neuroscience 8 (5): 16–20. May 2011. PMID 21686143. "Men with borderline personality disorder are more likely to demonstrate an explosive temperament and higher levels of novelty seeking. For Axis I comorbidity, men are more likely to evidence substance use disorders, whereas women with BPD are more likely to evidence eating, mood, anxiety, and posttraumatic stress disorders. Concerning Axis II comorbidity, men are more likely than women to evidence antisocial personality disorder. Finally, in terms of treatment utilization, men are more likely to have treatment histories relating to substance use disorders. Women are more likely to have treatment histories characterized by more pharmacotherapy and psychotherapy.".
- ↑ Edvard Munch: the life of a person with borderline personality as seen through his art. Denmark: Lundbeck Pharma A/S. 1990. pp. 34–35. ISBN 978-87-983524-1-9.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedauto - ↑ Edvard Munch: the life of a person with borderline personality as seen through his art. Denmark: Lundbeck Pharma A/S. 1990. ISBN 978-87-983524-1-9.
- ↑ Millon, Grossman & Meagher 2004, p. 172
- ↑ "Borderline psychiatric records – prodromal symptoms of psychical impairments". Alienists & Neurology 5: 85–90. 1884. OCLC 773814725.
- ↑ 217.0 217.1 Millon 1996, pp. 645–690
- ↑ "A history of borderline: disorder at the heart of psychiatry". Journal of Psychosocial Studies 16 (2): 117–134. 1 August 2023. doi:10.1332/147867323X16871713092130. https://oro.open.ac.uk/90946/1/90946.pdf. Retrieved 25 September 2023.
- ↑ "Psychoanalytic investigation of and therapy in the borderline group of neuroses". Psychoanalytic Quarterly 7 (4): 467–489. 1938. doi:10.1080/21674086.1938.11925367.
- ↑ "Adolph Stern, father of term 'borderline personality'". Minerva Psichiatrica 56 (2): 95. 2015.
- ↑ 221.0 221.1 "Historical perspectives on the borderline concept: a review and critique". Psychiatry 48 (3): 209–222. August 1985. doi:10.1080/00332747.1985.11024282. PMID 3898174.
- ↑ "The diagnostic interview for borderline patients". The American Journal of Psychiatry 138 (7): 896–903. July 1981. doi:10.1176/ajp.138.7.896. PMID 7258348.
- ↑ "Borderline Personality Disorder: History of the Concept". Borderline personality disorder. Boca Raton, Florida: Taylor & Francis. 2005. pp. 1–18. ISBN 978-0-8247-2928-8.
- ↑ Gunderson, John G.; Lyons-Ruth, Karlen (February 2008). "BPD's interpersonal hypersensitivity phenotype: a gene-environment-developmental model". Journal of Personality Disorders 22 (1): 22–41. doi:10.1521/pedi.2008.22.1.22. ISSN 0885-579X. PMID 18312121.
- ↑ Kernberg, Otto F.; Michels, Robert (May 2009). "Borderline Personality Disorder". American Journal of Psychiatry 166 (5): 505–508. doi:10.1176/appi.ajp.2009.09020263. ISSN 0002-953X. PMID 19411373. https://psychiatryonline.org/doi/10.1176/appi.ajp.2009.09020263.
- ↑ Adler, G.; Buie, D. H. (1979). "Aloneness and borderline psychopathology: the possible relevance of child development issues". The International Journal of Psycho-Analysis 60 (1): 83–96. ISSN 0020-7578. PMID 457345.
- ↑ LENZENWEGER, MARK F. (October 2001). "The Personality Disorders: A New Look at the Developmental Self and Object Relations Approach". American Journal of Psychiatry 158 (10): 1755–a. doi:10.1176/appi.ajp.158.10.1755-a. ISSN 0002-953X. https://psychiatryonline.org/doi/10.1176/appi.ajp.158.10.1755-a.
- ↑ Ruffalo, Mark L. (2025). "Heads I win, tails you lose: Interpersonal aspects of borderline personality disorder". Bulletin of the Menninger Clinic 89 (1): 52–69. doi:10.1521/bumc.2025.89.1.52. ISSN 1943-2828. PMID 40063356.
- ↑ Mental Health Primer. CreateSpace Independent Publishing Platform. 29 May 2018. p. 43. ISBN 978-1-7205-1057-4.
- ↑ Psychopharmacology Bulletin. The Clearinghouse. 1966. p. 555. https://books.google.com/books?id=_kOnSecueiYC&pg=PA555. Retrieved 5 June 2020.
- ↑ "Crossing the border into borderline personality and borderline schizophrenia. The development of criteria". Archives of General Psychiatry 36 (1): 17–24. January 1979. doi:10.1001/archpsyc.1979.01780010023001. PMID 760694.
- ↑ Harold Merskey, Psychiatric Illness: Diagnosis, Management and Treatment for General Practitioners and Students, Baillière Tindall (1980), p. 415. "Borderline personality disorder is a very controversial and confusing American term, best avoided.
- ↑ "Borderline personality disorder: gender stereotypes, stigma, and limited system of care". Issues in Mental Health Nursing 19 (2): 97–112. 1998. doi:10.1080/016128498249105. PMID 9601307.
- ↑ Shimo, Alexandra (2019-03-27). "Are sexual abuse victims being diagnosed with a mental disorder they don't have?" (in en-GB). The Guardian. ISSN 0261-3077. https://www.theguardian.com/lifeandstyle/2019/mar/27/are-sexual-abuse-victims-being-diagnosed-with-a-mental-disorder-they-dont-have.
- ↑ May, Natasha (2024-05-11). "Is this actually PTSD? Clinicians divided over redefining borderline personality disorder" (in en-GB). The Guardian. ISSN 0261-3077. https://www.theguardian.com/society/article/2024/may/12/is-this-actually-ptsd-clinicians-divided-over-redefining-borderline-personality-disorder.
- ↑ "When she was bad: borderline personality disorder in a posttraumatic age". The American Journal of Orthopsychiatry 70 (4): 422–432. October 2000. doi:10.1037/h0087769. PMID 11086521.
- ↑ "Borderline personality disorder: the voice of patients". Research in Nursing & Health 22 (4): 285–293. August 1999. doi:10.1002/(SICI)1098-240X(199908)22:4<285::AID-NUR3>3.0.CO;2-R. PMID 10435546.
- ↑ 238.0 238.1 238.2 Chapman & Gratz 2007, p. 31
- ↑ 239.0 239.1 239.2 239.3 Chapman & Gratz 2007, p. 32
- ↑ 240.0 240.1 "Elucidating the relationship between borderline personality disorder and intimate partner violence". Personality and Mental Health 14 (3): 284–303. August 2020. doi:10.1002/pmh.1480. PMID 32162499.
- ↑ "Chapter 1: Credibility problems in multiple personality disorder patients and abused children". Childhood antecedents of multiple personality. American Psychiatric Press. 1985. ISBN 978-0-88048-082-6. https://archive.org/details/childhoodanteced00kluf.
- ↑ "Pathological lying revisited". The Journal of the American Academy of Psychiatry and the Law 33 (3): 342–349. 2005. PMID 16186198. https://citeseerx.ist.psu.edu/document?repid=rep1&type=pdf&doi=43902f103c5ab7f664c1fdfe6b2bcb7743f9bcdb. Retrieved 10 January 2023.
- ↑ 243.0 243.1 "Borderline Personality Disorder Label Creates Stigma". http://www.borderlinepersonalitytoday.com/main/label.htm.
- ↑ "Understanding Borderline Personality Disorder". Treatment and Research Advancements Association for Personality Disorder. 2004. http://www.tara4bpd.org/dyn/index.php?option=content&task=view&id=12.
- ↑ Understanding and Treating Borderline Personality Disorder A Guide for Professionals and Families. Arlington, Virginia: American Psychiatric Publishing. 2005. ISBN 978-1-58562-135-4. https://archive.org/details/understandingtre00john.
- ↑ Chapman & Gratz 2007, p. 52
- ↑ American Psychiatric Association 2013, pp. 663–666
- ↑ "The Depiction of Trauma and its Effect on Character Development in the Brontë Fiction". Brontë Studies 38 (2): 157–168. 1 April 2013. doi:10.1179/1474893213Z.00000000062.
- ↑ "Personality Disorder of Character Smerdyakov in Novel the Brother Karamazov Bu [sic] Fyodor Dostovesky (Translated by Constance Clara Garnett)". Skripsi 1 (321412044). 26 October 2019. https://repository.ung.ac.id/skripsi/show/321412044/personality-disorder-of-character-smerdyakov-in-novel-the-brother-karamazov-bu-fyodor-dostovesky-translated-by-constance-clara-garnett.html. Retrieved 22 May 2022.
- ↑ Transpersonal Psychotherapy. SAGE. 1 January 2000. ISBN 978-1-4129-0802-3. https://books.google.com/books?id=RXa0uEkiNbQC&q=borderline+personality+disorder+%22steppenwolf%22&pg=PA74. Retrieved 22 May 2022.
- ↑ The Field Guide to Personality Disorders. Rapid Psychler Press. 1999. p. 113. ISBN 978-0-9680324-6-6.
- ↑ "Kristen Wiig earns awkward laughs and silence in 'Welcome to Me'". The Washington Post. 7 May 2015. https://www.washingtonpost.com/goingoutguide/movies/kristen-wiig-earns-awkward-laughs-and-silence-in-welcome-to-me/2015/05/06/c26d9b78-ef6d-11e4-8abc-d6aa3bad79dd_story.html.
- ↑ "Toronto Film Review: 'Welcome to Me': Kristen Wiig plays a woman with borderline personality disorder in this startlingly inspired comedy from Shira Piven". Variety. 11 September 2014. https://variety.com/2014/film/festivals/toronto-film-review-welcome-to-me-1201304067/.
- ↑ "Use Your Movie Time To Get Help With Mental Health Issues". 9 November 2021. https://www.femina.in/wellness/mental-health/use-your-movie-time-to-get-help-with-mental-health-issues-211072.html.
- ↑ "Early Sea Changes in Borderline Personality Disorder". Current Psychiatry Reports 8 (1): 1–4. 2006. doi:10.1007/s11920-006-0071-6. PMID 16513034. http://www.nami.org/Template.cfm?Section=By_Illness&template=%2FContentManagement%2FContentDisplay.cfm&ContentID=43145. Retrieved 17 April 2009.
- ↑ 256.0 256.1 Reel Psychiatry: Movie Portrayals of Psychiatric Conditions. Port Huron, Michigan: Rapid Psychler Press. 2003. p. 234. ISBN 978-1-894328-07-4.
- ↑ Movies and Mental Illness: Using Films to Understand Psychopathology. Cambridge, Massachusetts: Hogrefe. 2005. p. 59. ISBN 978-0-88937-292-4.
- ↑ "Long-term Memories: The Good, the Bad, and the Ugly". Cerebrum: The Dana Forum on Brain Science 2010: 21. 29 October 2010. ISSN 1524-6205. PMID 23447766.
- ↑ Psychology at the Movies. 14 March 2012. doi:10.1002/9781119941149. ISBN 978-1-119-94114-9.
- ↑ "Shame and A Dangerous Method reviews". The Art of Psychiatry. 16 April 2012. http://www.artofpsychiatry.co.uk/shame-and-a-dangerous-method-reviews/.
- ↑ "Netflix's 'Maniac' Is A Trippy Ride with a Lot To Say About Mental Illness". 26 September 2018. https://www.bustle.com/p/how-netflixs-maniac-uses-mental-illness-to-interrogate-what-it-means-to-be-normal-12019062.
- ↑ "A Therapist Explains Why Everyone on 'Game of Thrones' Has Serious Issues: Westeros is Basically A Living, Breathing Manual for Mental Illness". MTV News. 30 April 2015. http://www.mtv.com/news/2146368/game-of-thrones-mental-illness/.
- ↑ This Thing of Ours: Investigating the Sopranos. Wallflower Press. 2002. p. 118.
- ↑ "Titans Gives Bruce Wayne a Psychological Diagnosis". 26 August 2021. https://www.cbr.com/titans-bruce-wayne-borderline-personality-disorder/.
- ↑ Alvernaz, Adam (2019-01-29). "The Depressing Themes Hiding in Bojack Horseman's Closet". https://www.highlandernews.org/34540/depressing-themes-hiding-bojack-horsemans-closet/.
- ↑ "BPD Awareness Month – Congressional History". BPD Today (Mental Health Today). http://www.borderlinepersonalitydisorder.com/awareness/awareness-files/background.shtml.
- ↑ "선미 고백한 '경계선 인격장애' 뭐길래?" (in Korean). Naver TV. 16 December 2020. https://entertain.naver.com/ranking/read?oid=082&aid=0001052070.
General bibliography
- American Psychiatric Association (2000). Diagnostic and Statistical Manual of Mental Disorders (4th ed.). American Psychiatric Association. ISBN 978-0-89042-025-6.
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). American Psychiatric Publishing. ISBN 978-0-89042-555-8.
- The Borderline Personality Disorder Survival Guide: Everything You Need to Know About Living with BPD. Oakland, Calif.: New Harbinger Publications. 2007. ISBN 978-1-57224-507-5.
- "Two-year randomized controlled trial and follow-up of dialectical behavior therapy vs therapy by experts for suicidal behaviors and borderline personality disorder". Archives of General Psychiatry 63 (7): 757–66. July 2006. doi:10.1001/archpsyc.63.7.757. PMID 16818865.
- Cognitive-behavioral treatment of borderline personality disorder. New York: Guilford Press. 1993. ISBN 978-0-89862-183-9.
- Loving Someone with Borderline Personality Disorder. The Guilford Press. 2011. ISBN 978-1-59385-607-6.
- Disorders of Personality: DSM-IV-TM and Beyond. New York: John Wiley & Sons. 1996. ISBN 978-0-471-01186-6.
- Personality Disorders in Modern Life. Wiley. 2004. ISBN 978-0-471-32355-6.
- Masters of the mind: exploring the story of mental illness from ancient times to the new millennium. John Wiley & Sons. 2004. ISBN 978-0-471-46985-8.
- "Personality Subtypes". Dicandrien, Inc.. 2006. http://millon.net/taxonomy/summary.htm.
External links
- "Borderline personality disorder". National Institute of Mental Health. https://www.nimh.nih.gov/health/topics/borderline-personality-disorder.
- APA DSM 5 Definition of Borderline personality disorder
- APA Division 12 treatment page for Borderline personality disorder
- ICD-11 definition of Personality disorder, Borderline pattern by the World Health Organization
- NHS
- "Borderline Support UK". https://borderlinesupport.org.uk.
| Classification | |
|---|---|
| External resources |
 |
 KSF
KSF