Concussions in rugby union
Topic: Medicine
 From HandWiki - Reading time: 7 min
From HandWiki - Reading time: 7 min
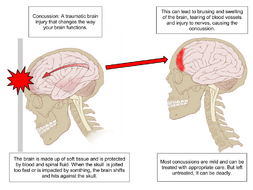
Concussions in England's professional rugby union are the most common injury received.[1] Concussion can occur where an individual experiences an impact to the head. Commonly occurring in high contact sporting activities; American football, boxing, and rugby. It can also occur in recreational activities like horse riding, jumping, cycling, and skiing. The reason being that it doesn't have to be something to strike you in the proximity of your brain, but can also be caused by rapid change of movement, giving the skull not enough time to move with your body, causing your brain to press against your skull.[2] With rugby being such a contact and fast moving sport, it is no wonder why there is concussion and other head injuries occurring. With the development of equipment and training methods, these will help benefit the players on the field know what could happen and how they can help with preventing it.
History of concussions
A concussion, which is known as a subset of traumatic brain injury (TBI), is when a force comes in contact with the head, neck or face, or fast movement of the head, causing a functional injury to the brain.[3] Depending on where the location of impact, depends on the severity of the injury. It is short-lived impairment of neurological function, the brains ability to process information, which can be resolved in seven to ten days.[1] Not all concussion involves the loss of consciousness, with it occurring in less than 10% of concussions.[3] Second-impact syndrome is when a player has obtained a second concussion when you either return to field the same day, or return to play before a complete recovery from a previous concussion. This is a result from brain swelling, from vascular congestion and increased intracranial pressure, this can be fatal to a player as it is a very difficult medical injury to control.[4] The brain is surrounded by cerebrospinal fluid, which protects it from light trauma. More severe impacts, or the forces associated with rapid acceleration, may not be absorbed by this cushion. Concussion may be caused by impact forces, in which the head strikes or is struck by something, or impulsive forces, in which the head moves without itself being subject to blunt trauma (for example, when the chest hits something and the head snaps forward). Chronic traumatic encephalopathy, or "CTE", is an example of the cumulative damage that can occur as the result of multiple concussions or less severe blows to the head. The condition was previously referred to as "dementia pugilistica", or "punch drunk" syndrome, as it was first noted in boxers. The disease can lead to cognitive and physical handicaps such as parkinsonism, speech and memory problems, slowed mental processing, tremor, depression, and inappropriate behavior. It shares features with Alzheimer's disease. Lamont sai od th PSCA after his incident::
| “ | The problem with the PSCA is a concussed player can pass the assessment. I know from first hand experience it can be quite ineffective in deciding if a player is concussed. It is argued that allowing the five-minutes assessment is better than zero minutes but it is not as clear cut as one might hope. Concussion symptoms regularly take 10 minutes or longer to actually present. Consequently the five-minute PSCA may be giving concussed players a license to return to the field.[5] | ” |
Connection with rugby union

Rugby union has been played since the early eighteen hundreds. Being a high contact sport it has the highest announced rates of concussion.[6] Research finding that during match play, concussion was reported at a higher level, and during training at a lower level, but still at a higher level than most players of another sport to receive.[6] With the game being both physically and mentally demanding, it varies from being at high intensities of sprinting, tackling and rucking, with small intensities of jogging and walking. The position of the forwards consists of them having to have a lot of physical strength to get the ball from the other team, or create gaps for their team to run through. Where as the backs are the players that make the play happen, making runs with the ball, with the protection of the forwards stopping attacks, the backs still do get tackled like any other player on the field, so they have to have physical strength as much as a forward. The Concussion bin was replaced by the head bin in 2012 with the players assessment taking 10 minutes.[7]
Causes and likelihood of concussion
Concussion was the most commonly reported Premiership Rugby match injury in 2015-16 (for the 5th consecutive season), constituting appropriately 25% of all match injuries, and the RFU medical officer said that the tackle is where the overwhelming majority of concussions occur.[8] A study found that playing more than 25 matches in the 2015/2016 season meant that sustaining concussion was more likely than not sustaining concussion.[9]
Signs of Concussion
Some of the effects that concussion can cause to an individuals mind set can vary, depending on the circumstances and the severity of the impact. The common signs of concussion can be; blank look, slow to get up off of the ground, unsteady on their feet, grabbing their head, confused in where they are or what they are doing, and obviously if they are unconscious.[10] These are the things that a spectator, coach and medical assistant will notice in a player. Sometimes concussion can go unrecognised, so from a players point there can be these symptoms; continual headaches, dizziness, visual problems, feeling of fatigue and drowsiness.[10] These all can occur post game, so a player needs to have knowledge of what these signs could mean.
Treatment of the injury

Once taken off the field of play due to possible concussion, being unconscious, or showing the symptoms post game, getting medical advice as soon as possible is recommended. At the hospital or medical practice, the player will be under observation, if they are experiencing a headache, mild pain killers will be given. The medical professional will request that no food or drink is to be consumed until advised.[11] They will then assess whether the player needs an x-ray, to check for any possible cervical vertebrae damage, or a computerised axial tomography (CT Scan) to check for any brain or cranium damage.[11] With a mild head injury being sent home to take care and doing activities slower than usual, and maintaining painkillers. If symptoms of concussion don't disappear in the average of seven to ten days, then seek medical advice again as injury could be worse. In post-concussion syndrome, symptoms do not resolve for weeks, months, or years after a concussion, and may occasionally be permanent. About 10% to 20% of people have post concussion syndrome for more than a month.
Controlling concussions
In order to minimise the risk of concussion and repetitive head trauma, the method of the 6 R's is used.[10] Firstly Recognising and Removing a suspected player of concussion, to stop the injury from getting worse. Secondly Refer, whether the player is either recognised or suspected with concussion they must see a medical doctor as soon as possible. 90.8% of players knew they should not continue playing when concussed. 75% of players would continue an important game even if concussed. Of those concussed, 39.1% have tried to influence medical assessment with 78.2% stating it is possible or quite easy to do so. If the player is diagnosed with concussion, they then must Rest, until all signs of concussion are gone. The player must then Recover by just returning to general activities in life, then progressing back to playing. Returning to play, must follow the Graduated Return to Play (GRTP) protocol, by having clearance from a medical professional, and no symptoms of concussion.[10] Despite good knowledge of concussion complications, management players engage in unsafe behaviour with little difference between gender and competition grades. Information regarding symptoms and management should be available to all players, coaches, and parents. On-going education is needed to assist coaches in identifying concussion signs and symptoms. Provision of medical care should be mandatory at every level of competition.
Effect of concussions on brain functioning in later life
A 2017 study found that past participation in rugby or a history of concussion were associated with small to moderate neurocognitive deficits after retirement from competitive sport.[12]
See also
- Head injury
- Rugby union
- Concussions in sport
References
- ↑ 1.0 1.1 Kirkwood, Graham; Parekh, Nikesh; Ofori-Asenso, Richard; Pollock, Allyson M (2015). "Concussion in youth rugby union and rugby league: A systematic review". British Journal of Sports Medicine 49 (8): 506–510. doi:10.1136/bjsports-2014-093774. PMID 25586912.
- ↑ "Concussion". http://brainfoundation.org.au/disorders/concussion. Retrieved 2 September 2015.
- ↑ 3.0 3.1 "World Rugby Player Welfare – Putting Players First : World Rugby Concussion Guidance for the General Public". http://playerwelfare.worldrugby.org/?documentid=133. Retrieved 2 September 2015.
- ↑ "Brain Injury in Sports". http://www.headinjury.com/sports.htm. Retrieved 2 September 2015.
- ↑ Lamont, Rory (19 December 2013). "Players are deliberately cheating concussion tests". ESPN Scrum. http://www.espnscrum.com/scrum/rugby/story/208943.html. Retrieved 26 December 2013.
- ↑ 6.0 6.1 Gardner, Andrew J; Iverson, Grant L; Williams, W. Huw; Baker, Stephanie; Stanwell, Peter (2014). "A Systematic Review and Meta-Analysis of Concussion in Rugby Union". Sports Medicine 44 (12): 1717–1731. doi:10.1007/s40279-014-0233-3. PMID 25138311.
- ↑ "Rugby is still holding the concussion bomb with tongs in spite of warnings". Irish Independent. http://m.independent.ie/opinion/columnists/vincent-hogan/rugby-is-still-holding-the-concussion-bomb-with-tongs-in-spite-of-warnings-30952483.html. Retrieved 13 September 2016.
- ↑ https://www.premiershiprugby.com/news/rugbys-most-comprehensive-injury-study-published/[full citation needed]
- ↑ Rafferty, James; Ranson, Craig; Oatley, Giles; Mostafa, Mohamed; Mathema, Prabhat; Crick, Tom; Moore, Isabel S (2018). "On average, a professional rugby union player is more likely than not to sustain a concussion after 25 matches". British Journal of Sports Medicine: bjsports-2017-098417. doi:10.1136/bjsports-2017-098417. PMID 29530941.
- ↑ 10.0 10.1 10.2 10.3 "Concussion Guidelines". http://www.rugby.com.au/tryrugby/administration/ConcussionGuidelines.aspx. Retrieved 2 September 2015.
- ↑ 11.0 11.1 "Head injury – home care tips – Better Health Channel". http://www.betterhealth.vic.gov.au/bhcv2/bhcarticles.nsf/pages/Head_injury_home_care_tips. Retrieved 2 September 2015.
- ↑ Hume, Patria A; Theadom, Alice; Lewis, Gwyn N; Quarrie, Kenneth L; Brown, Scott R; Hill, Rosamund; Marshall, Stephen W (2016). "A Comparison of Cognitive Function in Former Rugby Union Players Compared with Former Non-Contact-Sport Players and the Impact of Concussion History". Sports Medicine 47 (6): 1209–1220. doi:10.1007/s40279-016-0608-8. PMID 27558141.
 KSF
KSF