Cyanide poisoning
Topic: Medicine
 From HandWiki - Reading time: 21 min
From HandWiki - Reading time: 21 min
| Cyanide poison | |
|---|---|
| Other names | Cyanide toxicity, hydrocyanic acid poison[1] |
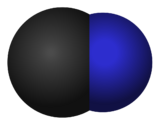 | |
| Cyanide ion | |
| Specialty | Toxicology, critical care medicine |
| Symptoms | Early: headache, dizziness, fast heart rate, shortness of breath, vomiting[2] Later: seizures, slow heart rate, low blood pressure, loss of consciousness, cardiac arrest[2] |
| Usual onset | Few minutes[2][3] |
| Causes | Cyanide compounds[4] |
| Risk factors | House fire, metal polishing, certain insecticides, eating seeds such as from almonds[2][3][5] |
| Diagnostic method | Based on symptoms, high blood lactate[2] |
| Treatment | Decontamination, supportive care (100% oxygen), hydroxocobalamin[2][3][6] |
Cyanide poisoning is poisoning that results from exposure to any of a number of forms of cyanide.[4] Early symptoms include headache, dizziness, fast heart rate, shortness of breath, and vomiting.[2] This phase may then be followed by seizures, slow heart rate, low blood pressure, loss of consciousness, and cardiac arrest.[2] Onset of symptoms usually occurs within a few minutes.[2][3] Some survivors have long-term neurological problems.[2]
Toxic cyanide-containing compounds include hydrogen cyanide gas and a number of cyanide salts.[2] Poisoning is relatively common following breathing in smoke from a house fire.[2] Other potential routes of exposure include workplaces involved in metal polishing, certain insecticides, the medication sodium nitroprusside, and certain seeds such as those of apples and apricots.[3][7][8] Liquid forms of cyanide can be absorbed through the skin.[9] Cyanide ions interfere with cellular respiration, resulting in the body's tissues being unable to use oxygen.[2]
Diagnosis is often difficult.[2] It may be suspected in a person following a house fire who has a decreased level of consciousness, low blood pressure, or high lactic acid.[2] Blood levels of cyanide can be measured but take time.[2] Levels of 0.5–1 mg/L are mild, 1–2 mg/L are moderate, 2–3 mg/L are severe, and greater than 3 mg/L generally result in death.[2]
If exposure is suspected, the person should be removed from the source of the exposure and decontaminated.[3] Treatment involves supportive care and giving the person 100% oxygen.[2][3] Hydroxocobalamin (vitamin B12a) appears to be useful as an antidote and is generally first-line.[2][6] Sodium thiosulphate may also be given.[2] Historically, cyanide has been used for mass suicide and it was used for genocide by the Nazis.[3][10]
Signs and symptoms
Acute exposure
If hydrogen cyanide is inhaled, it can cause a coma with seizures, apnea, and cardiac arrest, with death following in a matter of seconds. At lower doses, loss of consciousness may be preceded by general weakness, dizziness, headaches, vertigo, confusion, and perceived difficulty in breathing. At the first stages of unconsciousness, breathing is often sufficient or even rapid, although the state of the person progresses towards a deep coma, sometimes accompanied by pulmonary edema, and finally cardiac arrest. A cherry red skin color that darkens may be present as the result of increased venous hemoglobin oxygen saturation. Despite the similar name, cyanide does not directly cause cyanosis.[11] A fatal dose for humans can be as low as 1.5 mg/kg body weight.[12] Other sources claim a lethal dose is 1–3 mg per kg body weight for vertebrates.[13]
Chronic exposure
Exposure to lower levels of cyanide over a long period (e.g., after use of improperly processed cassava roots; cassava is a staple food in various parts of West Africa) results in increased blood cyanide levels, which can result in weakness and a variety of symptoms, including permanent paralysis, nervous lesions,[14][15][16] hypothyroidism,[15] and miscarriages.[17][18] Other effects include mild liver and kidney damage.[19][20]
Causes
Cyanide poisoning can result from the ingestion of cyanide salts; imbibing pure liquid prussic acid; skin absorption of prussic acid; intravenous infusion of nitroprusside for hypertensive crisis;[8] or the inhalation of hydrogen cyanide gas. The last typically occurs through one of three mechanisms:
- The gas is directly released from canisters (e.g., as part of a pesticide, insecticide, or Zyklon B).
- It is generated on site by reacting potassium cyanide or sodium cyanide with sulfuric acid (e.g., in a modern American gas chamber).
- Fumes arise during a building fire or any similar scenario involving the burning of polyurethane,[21] vinyl[22] or other polymer products that required nitriles in their production.
As potential contributing factors, cyanide is present in:
- Tobacco smoke.
- Many seeds or kernels such as those of almonds, apricots, apples, oranges, and flaxseed.[23]
- Foods including cassava (also known as tapioca, yuca or manioc) and bamboo shoots.
As a potential harm-reduction factor, Vitamin B12, in the form of hydroxocobalamin (also spelled hydroxycobalamin), might reduce the negative effects of chronic exposure; whereas, a deficiency might worsen negative health effects following exposure to cyanide.[24]
Mechanism
Cyanide is a potent cytochrome c oxidase (COX, a.k.a. Complex IV) inhibitor. As such, cyanide poisoning is a form of histotoxic hypoxia, because it interferes with oxidative phosphorylation.[25]:1475
Specifically, cyanide binds to the heme a3-CuB binuclear center of COX[26] (and thus is a non-competitive inhibitor of it). This prevents electrons passing through COX from being transferred to O2, which not only blocks the mitochondrial electron transport chain, it also interferes with the pumping of a proton out of the mitochondrial matrix which would otherwise occur at this stage. Therefore, cyanide interferes not only with aerobic respiration but also with the ATP synthesis pathway it facilitates, owing to the close relationship between those two processes.[27]:705
One antidote for cyanide poisoning, nitrite (i.e., via amyl nitrite), works by converting ferrohemoglobin to ferrihemoglobin, which can then compete with COX for free cyanide (as the cyanide will bind to the iron in its heme groups instead). Ferrihemoglobin cannot carry oxygen, but the amount of ferrihemoglobin that can be formed without impairing oxygen transport is much greater than the amount of COX in the body.[25]:1475
Cyanide is a broad-spectrum poison because the reaction it inhibits is essential to aerobic metabolism; COX is found in many forms of life.[28] However, susceptibility to cyanide is far from uniform across affected species; for instance, plants have an alternative electron transfer pathway available that passes electrons directly from ubiquinone to O2, which confers cyanide resistance by bypassing COX.[27]:704
Diagnosis
Lactate is produced by anaerobic glycolysis when oxygen concentration becomes too low for the normal aerobic respiration pathway. Cyanide poisoning inhibits aerobic respiration and therefore increases anaerobic glycolysis which causes a rise of lactate in the plasma. A lactate concentration above 10 mmol per liter is an indicator of cyanide poisoning, as defined by the presence of a blood cyanide concentration above 40 µmol per liter. Lactate levels greater than 6 mmol/L after reported or strongly suspected pure cyanide poisoning, such as cyanide-containing smoke exposure, suggests significant cyanide exposure.[29] However, lactate alone is not diagnostic of cyanide poisoning because lactosis is also triggered by many other things, including mitochondrial dysfunction.
Methods of detection include colorimetric assays such as the Prussian blue test, the pyridine-barbiturate assay, also known as the "Conway diffusion method"[30] and the taurine fluorescence-HPLC but like all colorimetric assays these are prone to false positives. Lipid peroxidation resulting in "TBARS", an artifact of heart attack produces dialdehydes that cross-react with the pyridine-barbiturate assay. Meanwhile, the taurine-fluorescence-HPLC assay used for cyanide detection is identical to the assay used to detect glutathione in spinal fluid.
Cyanide and thiocyanate assays have been run with mass spectrometry (LC/MS/MS), which are considered specific tests. Since cyanide has a short half-life, the main metabolite, thiocyanate is typically measured to determine exposure.
Treatment
Decontamination
Decontamination of people exposed to hydrogen cyanide gas only requires removal of the outer clothing and the washing of their hair.[9] Those exposed to liquids or powders generally require full decontamination.[9]
Antidote
The International Programme on Chemical Safety issued a survey (IPCS/CEC Evaluation of Antidotes Series) that lists the following antidotal agents and their effects: oxygen, sodium thiosulfate, amyl nitrite, sodium nitrite, 4-dimethylaminophenol, hydroxocobalamin, and dicobalt edetate ('Kelocyanor'), as well as several others.[31] Other commonly-recommended antidotes are 'solutions A and B' (a solution of ferrous sulfate in aqueous citric acid, and aqueous sodium carbonate, respectively) and amyl nitrite.
The United States standard cyanide antidote kit first uses a small inhaled dose of amyl nitrite, followed by intravenous sodium nitrite, followed by intravenous sodium thiosulfate.[32] Hydroxocobalamin was approved for use in the US in late 2006[33] and is available in Cyanokit antidote kits.[34] Sulfanegen TEA, which could be delivered to the body through an intra-muscular (IM) injection, detoxifies cyanide and converts the cyanide into thiocyanate, a less toxic substance.[35] Alternative methods of treating cyanide intoxication are used in other countries.
The Irish Health Service Executive (HSE) has recommended against the use of solutions A and B because of their limited shelf life, potential to cause iron poisoning, and limited applicability (effective only in cases of cyanide ingestion, whereas the main modes of poisoning are inhalation and skin contact). The HSE has also questioned the usefulness of amyl nitrite due to storage/availability problems, risk of abuse, and lack of evidence of significant benefits. It also states that the availability of kelocyanor at the workplace may mislead doctors into treating a patient for cyanide poisoning when this is an erroneous diagnosis. The HSE no longer recommends a particular cyanide antidote.[36]
| Agent | Description |
|---|---|
| Nitrites | The nitrites oxidize some of the hemoglobin's iron from the ferrous state to the ferric state, converting the hemoglobin into methemoglobin.
Cyanide binds avidly to methemoglobin, forming cyanmethemoglobin, thus releasing cyanide from cytochrome oxidase.[37] Treatment with nitrites is not innocuous as methemoglobin cannot carry oxygen, and severe methemoglobinemia may need to be treated in turn with methylene blue.[note 1] |
| Thiosulfate | The evidence for sodium thiosulfate's use is based on animal studies and case reports: the small quantities of cyanide present in dietary sources and in cigarette smoke are normally metabolized to relatively harmless thiocyanate by the mitochondrial enzyme rhodanese (thiosulfate cyanide sulfurtransferase), which uses thiosulfate as a substrate. However, this reaction occurs too slowly in the body for thiosulfate to be adequate by itself in acute cyanide poisoning. Thiosulfate must therefore be used in combination with nitrites.[37] |
| Hydroxocobalamin | Hydroxocobalamin, a form (or vitamer) of vitamin B12 made by bacteria, and sometimes denoted vitamin B12a, is used to bind cyanide to form the harmless cyanocobalamin form of vitamin B12. |
| 4-Dimethylaminophenol | 4-Dimethylaminophenol (4-DMAP) has been proposed[by whom?] in Germany as a more rapid antidote than nitrites with (reportedly) lower toxicity. 4-DMAP is used currently by the German military and by the civilian population. In humans, intravenous injection of 3 mg/kg of 4-DMAP produces 35 percent methemoglobin levels within 1 minute. Reportedly, 4-DMAP is part of the US Cyanokit, while it is not part of the German Cyanokit due to side effects (e. g. hemolysis). |
| Dicobalt edetate | Cobalt ions, being chemically similar to iron ions, can also bind cyanide. One current cobalt-based antidote available in Europe is dicobalt edetate or dicobalt-EDTA, sold as Kelocyanor. This agent chelates cyanide as the cobalticyanide. This drug provides an antidote effect more quickly than formation of methemoglobin, but a clear superiority to methemoglobin formation has not been demonstrated. Cobalt complexes are quite toxic, and there have been accidents reported in the UK where patients have been given dicobalt-EDTA by mistake based on a false diagnosis of cyanide poisoning. Because of its side effects, it should be reserved only for patients with the most severe degree of exposure to cyanide; otherwise, nitrite/thiosulfate is preferred.[40] |
| Glucose | Evidence from animal experiments suggests that coadministration of glucose protects against cobalt toxicity associated with the antidote agent dicobalt edetate. For this reason, glucose is often administered alongside this agent (e.g. in the formulation 'Kelocyanor'). It has also been anecdotally suggested that glucose is itself an effective counteragent to cyanide, reacting with it to form less toxic compounds that can be eliminated by the body. One theory on the apparent immunity of Grigori Rasputin to cyanide was that his killers put the poison in sweet pastries and madeira wine, both of which are rich in sugar; thus, Rasputin would have been administered the poison together with massive quantities of antidote. One study found a reduction in cyanide toxicity in mice when the cyanide was first mixed with glucose.[41] However, as yet glucose on its own is not an officially acknowledged antidote to cyanide poisoning. |
| 3-Mercaptopyruvate prodrugs | The most widely studied cyanide-metabolizing pathway involves utilization of thiosulfate by the enzyme rhodanese, as stated above. In humans, however, rhodanese is concentrated in the kidneys (0.96 units/mg protein) and liver (0.15 u/mg), with concentrations in lung, brain, muscle and stomach not exceeding 0.03 U/ml.[42] In all these tissues, it is found in the mitochondrial matrix, a site of low accessibility for ionized, inorganic species, such as thiosulfate. This compartmentalization of rhodanese in mammalian tissues leaves major targets of cyanide lethality, namely, the heart and central nervous system, unprotected. Rhodanese is also found in red blood cells, but its relative importance has not been clarified.[43][44])
A different cyanide-metabolizing pathway, 3-mercaptopyruvate sulfurtransferase (3-MPST, EC 2.8.1.2), which is more widely distributed in mammalian tissues than rhodanese, is being explored. 3-MPST converts cyanide to thiocyanate, using the cysteine catabolite, 3-mercaptopyruvate (3-MP). However, 3-MP is extremely unstable chemically. Therefore, a prodrug, sulfanegen sodium (2, 5-dihydroxy-1,4-dithiane-2,5-dicarboxylic acid disodium salt), which hydrolyzes into 2 molecules of 3-MP after being administered orally or parenterally, is being evaluated in animal models.[45][46] |
| Oxygen therapy | Oxygen therapy is not a cure in its own right. However, the human liver is capable of metabolizing cyanide quickly in low doses (smokers breathe in hydrogen cyanide, but it is such a small amount and metabolized so fast that it does not accumulate). |
- ↑ Methylene blue has historically been used as an antidote to cyanide poisoning,[38] but is not a preferred therapy due to its theoretical risk of worsening of cyanide symptoms by displacement of cyanide from methemoglobin, allowing the toxin to bind to tissue electron transport chains.[39]
History
Fires
The República Cromañón nightclub fire broke out in Buenos Aires, Argentina on 30 December 2004, killing 194 people and leaving at least 1,492 injured. Most of the victims died from inhaling poisonous gases, including carbon monoxide. After the fire, the technical institution INTI found that the level of toxicity due to the materials and volume of the building was 225 ppm of cyanide in the air. A lethal dose for rats is between 150 ppm and 220 ppm, meaning the air in the building was highly toxic.
On 27 January 2013, a fire at the Kiss nightclub in the city of Santa Maria, in the south of Brazil , caused the poisoning of hundreds of young people by cyanide released by the combustion of soundproofing foam made with polyurethane. By March 2013, 245 fatalities were confirmed.[47][48]
[when?]
Gas chambers
Research of hydrogen cyanide by chemists Carl Wilhelm Scheele and Claude Bernard would become central to understanding the lethality of future gas chambers.[49] In early 1942, Zyklon B, which contains hydrogen cyanide, emerged as the preferred killing tool of Nazi Germany for use in extermination camps during the Holocaust.[50] The chemical was used to murder roughly one million people in gas chambers installed in extermination camps at Auschwitz-Birkenau, Majdanek, and elsewhere.[51] Most of the people who were murdered were Jews, and by far the majority of these murders took place at Auschwitz.[52][53][lower-alpha 1] The constituents of Zyklon B were manufactured by several companies under licenses for Degesch, a corporation co-owned by IG Farben, Degussa and Th. Goldschmidt AG. It was sold to the German Army and the Schutzstaffel (SS) by the distributors Heli and Testa, with Heli supplying it to concentration camps at Mauthausen, Dachau, and Buchenwald and Testa to Auschwitz and Majdanek.[55] Camps also occasionally bought Zyklon B directly from the manufacturers.[56] Of the 729 tonnes of Zyklon B sold in Germany in 1942–44, 56 tonnes (about eight percent of domestic sales) were sold to concentration camps.[57] Auschwitz received 23.8 tonnes, of which six tonnes were used for fumigation. The remainder was used in the gas chambers or lost to spoilage (the product had a stated shelf life of only three months).[58] Tests conducted fumigations for the Wehrmacht and supplied them with Zyklon B. They also offered courses to the SS in the safe handling and use of the material for fumigation purposes.[59] In April 1941, the German agriculture and interior ministries designated the SS as an authorized applier of the chemical, and thus they were able to use it without any further training or governmental oversight.[60]
Hydrogen cyanide gas has been used for judicial execution in some states of the United States, where cyanide was generated by reaction between potassium cyanide (or sodium cyanide[61][62]) dropped into a compartment containing sulfuric acid, directly below the chair in the gas chamber.[63]
Suicide
Cyanide salts are sometimes used as fast-acting suicide devices. Cyanide reacts at a higher level with high stomach acidity.
- On 26 January 1904, company promoter and swindler Whitaker Wright died by suicide by ingesting cyanide in a court anteroom immediately after being convicted of fraud.
- In February 1937, the Uruguayan short story writer Horacio Quiroga died by suicide by drinking cyanide at a hospital in Buenos Aires.
- In 1937, polymer chemist Wallace Carothers died by suicide by cyanide.
- In the 1943 Operation Gunnerside to destroy the Vemork Heavy Water Plant in World War II (an attempt to stop or slow German atomic bomb progress), the commandos were given cyanide tablets (cyanide enclosed in rubber) kept in the mouth and were instructed to bite into them in case of German capture. The tablets ensured death within three minutes.[64]
- Cyanide, in the form of pure liquid prussic acid (a historical name for hydrogen cyanide), was the favored suicide agent of Nazi Germany. Erwin Rommel (1944), Adolf Hitler's wife, Eva Braun (1945),[65] and Nazi leaders Heinrich Himmler (1945), possibly Martin Bormann (1945), and Hermann Göring (1946) all died by suicide by ingesting it.
- It is speculated that, in 1954, Alan Turing used an apple that had been injected with a solution of cyanide to die by suicide after being convicted of having a homosexual relationship, which was illegal at the time in the United Kingdom, and forced to undergo hormonal castration to avoid prison. An inquest determined that Turing's death from cyanide poisoning was a suicide, although this has been disputed.
- Members of the Sri Lankan Tamil (or Eelam Tamil) LTTE (Liberation Tigers of Tamil Eelam, whose insurgency lasted from 1983 to 2009), used to wear cyanide vials around their necks with the intention of dying by suicide if captured by the government forces.
- On 22 June 1977, Moscow, Aleksandr Dmitrievich Ogorodnik, a Soviet diplomat accused of spying on behalf of the Colombian Intelligence Agency and the US Central Intelligence Agency, was arrested. During the interrogations, Ogorodnik offered to write a full confession and asked for his pen. Inside the pen cap was a cleverly hidden cyanide pill, which when bitten on, caused Ogorodnik to die before he hit the floor, according to the Soviets.[66]
- On 18 November 1978, Jonestown. A total of 909 individuals died in Jonestown, many from apparent cyanide poisoning, in an event termed "revolutionary suicide" by Jones and some members on an audio tape of the event and in prior discussions. The poisonings in Jonestown followed the murder of five others by Temple members at Port Kaituma, including United States Congressman Leo Ryan, an act that Jones ordered. Four other Temple members died by murder-suicide in Georgetown at Jones' command.
- On 6 June 1985, serial killer Leonard Lake died in custody after having ingested cyanide pills he had sewn into his clothes.
- On 28 June 2012, Wall Street trader Michael Marin ingested a cyanide pill seconds after a guilty verdict was read in his arson trial in Phoenix, Arizona; he died minutes after.[67]
- On 22 June 2015, John B. McLemore, a horologist and the central figure of the podcast S-Town, died after ingesting cyanide.[68]
- On 29 November 2017, Slobodan Praljak died from drinking potassium cyanide, after being convicted of war crimes by the International Criminal Tribunal for the former Yugoslavia.[69]
Mining and industrial
- In 1993, an illegal spill resulted in the death of seven people in Avellaneda, Argentina .[70] In their memory, the National Environmental Conscious Day (Día Nacional de la Conciencia Ambiental) was established.[71]
- In 2000, a spill at Baia Mare, Romania, resulted in the worst environmental disaster in Europe since Chernobyl.[72]
- In 2000, Allen Elias, CEO of Evergreen Resources was convicted of knowing endangerment for his role in the cyanide poisoning of employee Scott Dominguez.[73][74] This was one of the first successful criminal prosecutions of a corporate executive by the Environmental Protection Agency.
Murder
- John Tawell, a murderer who in 1845 became the first person to be arrested as the result of telecommunications technology.
- Grigori Rasputin (1916; attempted, later killed by gunshot)
- The Goebbels children (1945)
- Stepan Bandera (1959)
- Jonestown, Guyana, was the site of a large mass murder–suicide,[75] in which over 900 members of the Peoples Temple drank potassium cyanide–laced Flavor Aid in 1978.
- Chicago Tylenol murders (1982)
- Timothy Marc O'Bryan (1966–1974) died on October 31, 1974, by ingesting potassium cyanide placed into a giant Pixy Stix. His father, Ronald Clark O'Bryan, was [76] convicted of Tim's murder plus four counts of attempted murder. O'Bryan put potassium cyanide into five giant Pixy Stix that he gave to his son and daughter along with three other children. Only Timothy ate the poisoned candy and died.
- Bruce Nickell and Sue Snow (5 June 1986) Murdered by Stella Nickell who poisoned bottles of Excedrin.
- Richard Kuklinski (1935–2006)
- Janet Overton (1942–1988) Her husband, Richard Overton, was convicted of poisoning her,[77] but Janet's symptoms did not match those of classic cyanide poisoning, the timeline was inconsistent with cyanide poisoning, and the amount found was just a trace. The diagnostic method used was prone to false positives. Richard Overton died in prison in 2009.
- Urooj Khan (1966–2012), won the lottery and was found dead a few days later.[78] A blood diagnostic reported a lethal level of cyanide in his blood, but the body did not display any classic symptoms of cyanide poisoning, and no link to cyanide could be found in Urooj's social circle. The diagnostic method used was the Conway diffusion method, prone to false positives with artifacts of heart attack and kidney failure. The chemistry of this and other false positives could be linked to the TBARS response following heart failure.
- Autumn Marie Klein (20 April 2013), a prominent 41-year-old neuroscientist and physician, died from cyanide poisoning.[79] Klein's husband, Robert J. Ferrante, also a prominent neuroscientist who used cyanide in his research, was convicted of murder and sentenced to life in prison for her death. Robert Ferrante is appealing his conviction, claiming the cyanide was a false positive.[80]
- Mirna Salihin died in hospital on 6 January 2016, after drinking a Vietnamese iced coffee at a cafe in a shopping mall in Jakarta. Police reports claim that cyanide poisoning was the most likely cause of her death.
- Jolly Thomas of Kozhikode, Kerala, India , was arrested in 2019 for the murder of 6 family members. Murders took place over a 14-year period, and each victim ate a meal prepared by the killer. The murders were allegedly motivated by wanting control of the family finances and property.[81]
- Mei Xiang Li of Brooklyn, New York, collapsed and died in April 2017, with cyanide later reported to be in her blood.[82] However, Mei never exhibited symptoms of cyanide poisoning and no link to cyanide could be found in her life. Another likely false positive.
- Sararath "Am" Rangsiwutthiporn, who became quickly known as "Am Cyanide" in Thai media, was arrested by the Thai police for allegedly poisoning 11 of her friends and acquaintances, spanning 2020 to 2023, with 10 deaths and 1 surviving supposed victim.[83] According to an ongoing investigation, the number of victims is currently at 20-30 persons, mostly dead with several survived.
Warfare or terrorism
- In 1988, between 3,200 and 5,000 people died in the Halabja massacre owing to unknown chemical nerve agents. Hydrogen cyanide gas was strongly suspected.[84][85]
- In 1995, a device was discovered in a restroom in the Kayabachō Tokyo subway station, consisting of bags of sodium cyanide and sulfuric acid with a remote controlled motor to rupture them, in what was believed to be an attempt by the Aum Shinrikyo cult to produce toxic amounts of hydrogen cyanide gas.[86]
- In 2003, Al Qaeda reportedly planned to release cyanide gas into the New York City Subway system. The attack was supposedly aborted because there would not be enough casualties.[87]
Research
Cobinamide is the final compound in the biosynthesis of cobalamin. It has greater affinity for the cyanide than cobalamin itself, which suggests that it could be a better option for emergency treatment.[88]
See also
- Anaerobic glycolysis
- Lactic acidosis
- List of poisonings
- Konzo
References
Explanatory notes
Citations
- ↑ Waters, Brenda L. (2010). Handbook of Autopsy Practice (4 ed.). Springer Science & Business Media. p. 427. ISBN 978-1597451277. https://books.google.com/books?id=JN4DJu_pzoMC&pg=PA427. Retrieved 26 August 2017.
- ↑ 2.00 2.01 2.02 2.03 2.04 2.05 2.06 2.07 2.08 2.09 2.10 2.11 2.12 2.13 2.14 2.15 2.16 2.17 2.18 2.19 Anseeuw, K; Delvau, N; Burillo-Putze, G; De Iaco, F; Geldner, G; Holmström, P; Lambert, Y; Sabbe, M (February 2013). "Cyanide poisoning by fire smoke inhalation: a European expert consensus.". European Journal of Emergency Medicine 20 (1): 2–9. doi:10.1097/mej.0b013e328357170b. PMID 22828651.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 Hamel, J (February 2011). "A review of acute cyanide poisoning with a treatment update.". Critical Care Nurse 31 (1): 72–81; quiz 82. doi:10.4037/ccn2011799. PMID 21285466.
- ↑ 4.0 4.1 Dorland's Illustrated Medical Dictionary (32 ed.). Elsevier Health Sciences. 2011. p. 1481. ISBN 978-1455709854. https://books.google.com/books?id=mNACisYwbZoC&pg=PA1481. Retrieved 26 August 2017.
- ↑ Ballhorn, Daniel J. (2011). "Cyanogenic Glycosides in Nuts and Seeds". Nuts and Seeds in Health and Disease Prevention. Elsevier. pp. 129–136. doi:10.1016/b978-0-12-375688-6.10014-3. ISBN 978-0123756886.
- ↑ 6.0 6.1 Thompson, JP; Marrs, TC (December 2012). "Hydroxocobalamin in cyanide poisoning.". Clinical Toxicology 50 (10): 875–885. doi:10.3109/15563650.2012.742197. PMID 23163594.
- ↑ Hevesi, Dennis (26 March 1993). "Imported Bitter Apricot Pits Recalled as Cyanide Hazard". The New York Times. https://www.nytimes.com/1993/03/26/nyregion/imported-bitter-apricot-pits-recalled-as-cyanide-hazard.html.
- ↑ 8.0 8.1 "Sodium Nitroprusside". The American Society of Health-System Pharmacists. https://www.drugs.com/monograph/sodium-nitroprusside.html.
- ↑ 9.0 9.1 9.2 "Hydrogen Cyanide – Emergency Department/Hospital Management". 14 January 2015. https://chemm.nlm.nih.gov/cyanide_hospital_mmg.htm.
- ↑ Longerich 2010, pp. 281–282.
- ↑ Bhagavan, N. V.; Ha, Chung-Eun Ha (2015). Essentials of Medical Biochemistry (Second ed.). https://www.sciencedirect.com/topics/neuroscience/cyanide-poisoning. Retrieved 10 November 2022.
- ↑ "Cyanide [Technical document – Chemical/Physical Parameters"]. Health Canada. 6 October 2008. https://www.hc-sc.gc.ca/ewh-semt/pubs/water-eau/cyanide-cyanure/index-eng.php.
- ↑ Oke, O. L. (1969). "The role of hydrocyanic acid in nutrition". World Review of Nutrition and Dietetics 11: 170–98. doi:10.1159/000387578. ISBN 978-3-8055-0662-5. PMID 4313082.
- ↑ "Effects of long-term low-dose cyanide administration to rats". Ecotoxicology and Environmental Safety 53 (1): 37–41. 2002. doi:10.1006/eesa.2002.2189. PMID 12481854.
- ↑ 15.0 15.1 "Comparative effects of prolonged administration of cyanide, thiocyanate and chokecherry (Prunus virginiana) to goats". Journal of Applied Toxicology 28 (3): 356–63. 2008. doi:10.1002/jat.1286. PMID 17631662. https://naldc-legacy.nal.usda.gov/naldc/download.xhtml?id=15073&content=PDF. Retrieved 29 December 2018.
- ↑ "Neuropathologic study of long term cyanide administration to goats". Food and Chemical Toxicology 40 (11): 1693–1698. 2002. doi:10.1016/S0278-6915(02)00151-5. PMID 12176095.
- ↑ "Prenatal toxicity of cyanide in goats—a model for teratological studies in ruminants". Theriogenology 62 (6): 1012–26. 2004. doi:10.1016/j.theriogenology.2003.12.023. PMID 15289044.
- ↑ Soto-Blanco B, Pereira, Verechia FT (2009). "Fetal and maternal lesions of cyanide dosing to pregnant goats". Small Ruminant Research 87 (1–3): 76–80. doi:10.1016/j.smallrumres.2009.09.029.
- ↑ "Does prolonged oral exposure to cyanide promote hepatotoxicity and nephrotoxicity?". Toxicology 174 (2): 87–95. 2002. doi:10.1016/S0300-483X(02)00041-0. PMID 11985886.
- ↑ "Effects of long-term cyanide ingestion by pigs". Veterinary Research Communications 31 (1): 93–104. 2007. doi:10.1007/s11259-006-3361-x. PMID 17180454.
- ↑ McKenna, Sean Thomas; Hull, Terence Richard (2016). "The fire toxicity of polyurethane foams". Fire Science Reviews 5 (1). doi:10.1186/s40038-016-0012-3.
- ↑ David M. Cline, ed (2012). Tintinalli's emergency medicine manual (7th ed.). New York: McGraw-Hill Medical. p. 604. ISBN 978-0071781848.
- ↑ ((EFSA Panel on Contaminants in the Food Chain)) (2019). "Evaluation of the health risks related to the presence of cyanogenic glycosides in foods other than raw apricot kernels". European Food Safety Authority Journal 17 (4): e05662. doi:10.2903/j.efsa.2019.5662. PMID 32626287.
- ↑ "Effects of low cobalamin diet and chronic cyanide toxicity in baboons". Toxicology 12 (3): 221–234. 1979. doi:10.1016/0300-483X(79)90068-4. PMID 494304.
- ↑ 25.0 25.1 Berg, Jeremy M.; Tymoczko, John L.; Stryer, Lubert (2002). Biochemistry (5th ed.). New York: W. H. Freeman. ISBN 0716730510.
- ↑ Leavesley, Heather B.; Li, Li; Prabhakaran, Krishnan; Borowitz, Joseph L.; Isom, Gary E. (January 2008). "Interaction of Cyanide and Nitric Oxide with Cytochrome c Oxidase: Implications for Acute Cyanide Toxicity". Toxicological Sciences 101 (1): 101–111. doi:10.1093/toxsci/kfm254. PMID 17906319. https://academic.oup.com/toxsci/article/101/1/101/1657982. Retrieved 9 February 2021.
- ↑ 27.0 27.1 Nelson, David L.; Cox, Michael M. (2004). Lehninger Principles of Biochemistry (4th ed.). New York: W. H. Freeman. ISBN 978-0716762652.
- ↑ "Evolution of cytochrome oxidase, an enzyme older than atmospheric oxygen" (in en). The EMBO Journal 13 (11): 2516–2525. June 1994. doi:10.1002/j.1460-2075.1994.tb06541.x. PMID 8013452.
- ↑ Leybell, Inna. "Cyanide Toxicity Workup". https://emedicine.medscape.com/article/814287-workup.
- ↑ Forensic Toxicology: Principles and Concepts By Nicholas T Lappas, Courtney M Lappas, Chapter 10.
- ↑ "Antidotes for Poisoning by Cyanide: 6. myl Nitrite". IPCS/CEC Evaluation of Antidotes Series; Volume 2. https://www.inchem.org/documents/antidote/antidote/ant02.htm#PartNumber:6.
- ↑ Toxicity, Cyanide~overview at eMedicine
- ↑ "Drug Approval Package: Cyanokit (hydroxocobalamin for injection) NDA #022041". https://www.accessdata.fda.gov/drugsatfda_docs/nda/2006/022041_cyanokit_toc.cfm.
- ↑ Toxicity, Cyanide~treatment at eMedicine
- ↑ "New Antidote for Cyanide Found". February 2013. https://news.yahoo.com/antidote-cyanide-found-132827160.html.[full citation needed]
- ↑ "Cyanide poisoning – New recommendations on first aid treatment". Health and Safety Executive. https://www.hse.gov.uk/pubns/misc076.htm.
- ↑ 37.0 37.1 Leybell, Inna (12 November 2019). "Cyanide Toxicity". https://emedicine.medscape.com/article/814287-overview.
- ↑ Hanzlik, PJ (4 February 1933). "Methylene blue as an antidote for cyanide poisoning". JAMA 100 (5): 357. doi:10.1001/jama.1933.02740050053028.
- ↑ Dart, Richard, ed (2004). Medical Toxicology (Third ed.). Lippincott Williams & Wilkins. p. 221. ISBN 978-0781728454. https://books.google.com/books?id=BfdighlyGiwC&q=cyanide+methylene+blue&pg=PA221.
- ↑ Nagler, J; Provoost, RA; Parizel, G (1978). "Hydrogen cyanide poisoning: Treatment with cobalt EDTA". Journal of Occupational Medicine 20 (6): 414–416. PMID 209160.
- ↑ Gerardo, I; Ilsen, R; Ernesto, I; Egar, S; Magaly, T; Marcelo, G (2005). "Valoración de la glucosa como antídoto en la intoxicación por cianuro" (in es). Retel (7). https://www.sertox.com.ar/modules.php?name=Content&pa=showpage&pid=120.
- ↑ Aminlari, Mahmoud; Malekhusseini, Ali; Akrami, Fatemeh; Ebrahimnejad, Hadi (2006). "Cyanide-metabolizing enzyme rhodanese in human tissues: Comparison with domestic animals". Comparative Clinical Pathology 16: 47–51. doi:10.1007/s00580-006-0647-x.
- ↑ "The antidotal action of sodium nitrite and sodium thiosulfate against cyanide poisoning". J Clin Pharmacol 32 (4): 368–375. 1992. doi:10.1002/j.1552-4604.1992.tb03849.x. PMID 1569239.
- ↑ "The inactivation of rhodanese by nitrite and inhibition by other anions in vitro". J. Biochem. Toxicol. 4 (1): 29–33. 1989. doi:10.1002/jbt.2570040106. PMID 2769694.
- ↑ "A novel paradigm for assessing efficacies of potential antidotes against neurotoxins in mice". Toxicol. Lett. 175 (1–3): 111–117. December 2007. doi:10.1016/j.toxlet.2007.10.001. PMID 18024011.
- ↑ "Novel, orally effective cyanide antidotes". J. Med. Chem. 50 (26): 6462–6464. December 2007. doi:10.1021/jm7011497. PMID 18038966.
- ↑ "Número de pessoas mortas em incêndio em boate em Santa Maria, no RS, é revisado para 232" (in pt). 27 January 2013. https://noticias.r7.com/cidades/autoridades-confirmam-245-pessoas-mortas-em-incendio-em-casa-noturna-de-santa-maria-rs-27012013.
- ↑ Haynes and Prada (2 February 2013). "U.S. rushing treatment for Brazil fire victims". Reuters. https://www.reuters.com/article/us-brazil-nightclub-deaths-idUSBRE9100ZF20130202.
- ↑ Christianson, S. (2010). The Last Gasp: The Rise and Fall of the American Gas Chamber. University of California Press. p. 24. ISBN 978-0-520-25562-3. https://books.google.com/books?id=AIzaoHoggUwC&pg=PA24. Retrieved 2023-06-17.
- ↑ Longerich 2010, pp. 281–282.
- ↑ Hayes 2004, pp. 2, 272.
- ↑ Piper 1994, p. 161.
- ↑ Hayes 2004, p. 272.
- ↑ Steinbacher (2005). Auschwitz: A History. Penguin. pp. 132–133. https://www.amazon.com/Auschwitz-History-Sybille-Steinbacher-2005-01-17/dp/B017MYHO5U. Retrieved 27 February 2021.
- ↑ Christianson, Scott (2010). The last gasp: the rise and fall of the American gas chamber. Berkeley, Calif.: University of California Press. pp. 166. ISBN 978-0-520-25562-3.
- ↑ Hayes 2004, pp. 288–289.
- ↑ Hayes 2004, p. 296.
- ↑ Hayes 2004, pp. 294–297, chpt. "Degesch and Zyklon B.". "The SS learned in 1944 that the expiration dates on the Zyklon tins were not hard and fast. All in all, it seems reasonable to assume that the SS over- rather than underdosed ..." —Peter Hayes
- ↑ Hayes 2004, p. 283.
- ↑ Hayes 2004, p. 284.
- ↑ "Gas chamber | execution device". https://www.britannica.com/topic/gas-chamber. second paragraph
- ↑ "Execution by gas in Md. To end next week Killer Hunt's death will be last by method". https://articles.baltimoresun.com/1997-06-22/news/1997173051_1_gas-chamber-hunt-lethal-injection.
- ↑ "Gas Chamber Executions". About.com. https://civilliberty.about.com/od/capitalpunishment/ig/Types-of-Executions/Gas-Chamber-Executions.htm.
- ↑ "Operation Gunnerside" in the book Bomb: The Race to Build – and Steal – the World's Most Dangerous Weapon
- ↑ Linge, Heinz (2009) (in en). With Hitler to the End. Frontline Books–Skyhorse Publishing. ISBN 978-1-60239-804-7. https://archive.org/details/withhitlertoendm00ling.
- ↑ Former CIA Chief of Disguise Breaks Down Cold War Spy Gadgets | Wired
- ↑ "Michael Marin, former Wall Street trader, took cyanide after arson conviction, says autopsy". CBS News. https://www.cbsnews.com/8301-504083_162-57481400-504083/michael-marin-former-wall-street-trader-took-cyanide-after-arson-conviction-says-autopsy/.
- ↑ "Who is John B. McLemore, figure in new 'S-Town' podcast? (spoilers)". Alabama Local News. https://www.al.com/entertainment/index.ssf/2017/03/who_is_john_b_mclemore_figure.html/.
- ↑ "Preliminary results autopsy Slobodan Praljak". Openbaar Ministerie. https://www.om.nl/@101281/preliminary-results/.
- ↑ "Recordando: "A tres años de la muerte de 7 personas por un escape de gas tóxico no hay culpables" (artículo del 28/09/1996)" (in es). 2018-04-20. https://redproteger.com.ar/safetyblog/recordando-a-tres-anos-de-la-muerte-de-7-personas-por-un-escape-de-gas-toxico-no-hay-culpables-articulo-del-28-09-1996/.
- ↑ "InfoLeg - Información Legislativa". https://servicios.infoleg.gob.ar/infolegInternet/verNorma.do?id=32306.
- ↑ "Death of a river" , BBC, 15 February 2000
- ↑ Kenworthy, Tom (13 December 1999). "A Life 'Trashed' in Cyanide Tank Long Prison Term Predicted in Environmental Crime". The Washington Post. https://www.washingtonpost.com/wp-srv/WPcap/1999-12/13/011r-121399-idx.html.
- ↑ Dugoni, Robert; Hilldorfer, Joseph (2004). The Cyanide Canary. Simon & Schuster. pp. 1–352. ISBN 978-0743246521. https://archive.org/details/cyanidecanary00hill/page/1.
- ↑ "Was It Murder or Suicide: A Forum". https://jonestown.sdsu.edu/?page_id=31981.
- ↑ "Ronald Clark O'Bryan, Appellant, v. The State of Texas, Appellee". https://law.justia.com/cases/texas/court-of-criminal-appeals/1979/59731-3.html.
- ↑ "Overton Found Guilty of Wife's Cyanide Murder". 9 May 1995. https://www.latimes.com/archives/la-xpm-1995-05-09-mn-64088-story.html.
- ↑ Gorner, Jeremy (25 July 2017). "Lottery winner's cyanide poisoning death remains unsolved five years later". Chicago Tribune. https://www.chicagotribune.com/news/breaking/ct-cyanide-poisoning-death-lottery-winner-met-20170725-story.html.
- ↑ Reed Ward, Paula. "The Ferrante trial: A look inside the cyanide poisoning case". Pittsburgh Post-Gazette. https://www.post-gazette.com/local/city/2014/10/19/The-Ferrante-trial-Inside-the-Autumn-Marie-Klein-cyanide-poisoning-case-in-Pittsburgh/stories/201410190091.
- ↑ "Pittsburgh researcher convicted of poisoning wife with cyanide". 7 November 2014. https://www.cbsnews.com/news/jury-pittsburgh-researcher-robert-ferrante-poisoned-his-wife-autumn-klein/.
- ↑ Dhillon, Amrit (7 October 2019). "Woman in India admits poisoning six family members with cyanide". The Guardian. https://www.theguardian.com/world/2019/oct/07/woman-in-india-admits-poisoning-six-family-members-with-cyanide.
- ↑ Parascandola, Kerry Burke, Rocco. "Sunset Park family reeling after they learn their matriarch had high levels of cyanide in her blood when she died – NY Daily News". nydailynews.com. https://www.nydailynews.com/new-york/brooklyn/son-reels-learns-mom-died-cyanide-poisoning-article-1.3075881.
- ↑ Rebecca Ratcliffe, Navaon Siradapuvadol. "Thai police investigate 10 deaths as woman accused of poisoning friend". https://www.theguardian.com/world/2023/apr/25/thai-police-investigate-other-deaths-as-woman-accused-of-poisoning-friend.
- ↑ Centers for Disease Control and Prevention (April 4, 2018). "Facts About Cyanide". https://emergency.cdc.gov/agent/cyanide/basics/facts.asp.
- ↑ Eric Croddy with Clarisa Perez-Armendariz & John Hart, Chemical and Biological Warfare: A Comprehensive Survey for the Concerned Citizen (Spring Science+Business Media, 2002), p. 164.
- ↑ "Chronology of Aum Shinrikyo's CBW Activities". Monterey Institute of International Studies. 2001. https://cns.miis.edu/reports/pdfs/aum_chrn.pdf.
- ↑ Suskind, Ron (19 June 2006). "The Untold Story of al-Qaeda's Plot to Attack the Subway". Time (magazine) magazine. https://www.time.com/time/magazine/article/0,9171,1205478,00.html. Retrieved 20 January 2007.
- ↑ Suman, Sigridur G.; Gretarsdottir, Johanna M.; Sigel, Astrid; Freisinger, Eva; Sigel, Roland K. O.; Carver, Peggy L. (2019). "Chapter 14. Chemical and Clinical Aspects of Metal-Containing Antidotes for Poisoning by Cyanide". Essential Metals in Medicine: Therapeutic Use and Toxicity of Metal Ions in the Clinic. Metal Ions in Life Sciences, vol. 19. 19. Berlin: de Gruyter. pp. 359–391. doi:10.1515/9783110527872-020. ISBN 978-3110526912.
Sources
- Longerich, Peter (2010). Holocaust: The Nazi Persecution and Murder of the Jews. Oxford; New York: Oxford University Press. ISBN 978-0192804365.
- Hayes, Peter (2004). From Cooperation to Complicity: Degussa in the Third Reich. Cambridge; New York; Melbourne: Cambridge University Press. ISBN 978-0521782272.
- Piper, Franciszek (1994). "Gas Chambers and Crematoria". in Gutman, Yisrael; Berenbaum, Michael. Anatomy of the Auschwitz Death Camp. Bloomington: Indiana University Press. pp. 157–182. ISBN 978-0253326843. https://archive.org/details/anatomyofauschwi00yisr.
| Classification | |
|---|---|
| External resources |
 |
 KSF
KSF

