Diabetes
Topic: Medicine
 From HandWiki - Reading time: 40 min
From HandWiki - Reading time: 40 min
Diabetes mellitus, commonly known as diabetes, is a group of common endocrine diseases characterized by sustained high blood sugar levels.[1][2] Diabetes is due to either the pancreas not producing enough of the hormone insulin, or the cells of the body becoming unresponsive to insulin's effects.[3] Classic symptoms include the three P's: polydipsia (excessive thirst), polyuria (excessive urination), polyphagia (excessive hunger), weight loss, and blurred vision. If left untreated, the disease can lead to various health complications, including disorders of the cardiovascular system, eye, kidney, and nerves.[4] Diabetes accounts for approximately 4.2 million deaths every year,[5] with an estimated 1.5 million caused by either untreated or poorly treated diabetes.[1]
The major types of diabetes are type 1 and type 2.[6] The most common treatment for type 1 is insulin replacement therapy (insulin injections), while anti-diabetic medications (such as metformin and semaglutide) and lifestyle modifications can be used to manage type 2. Gestational diabetes, a form that sometimes arises during pregnancy, normally resolves shortly after delivery. Type 1 diabetes is an autoimmune condition where the body's immune system attacks the beta cells in the pancreas, preventing the production of insulin. This condition is typically present from birth or develops early in life. Type 2 diabetes occurs when the body becomes resistant to insulin, meaning the cells do not respond effectively to it, and thus, glucose remains in the bloodstream instead of being absorbed by the cells.[7] Additionally, diabetes can also result from other specific causes, such as genetic conditions (monogenic diabetes syndromes like neonatal diabetes and maturity-onset diabetes of the young), diseases affecting the pancreas (such as pancreatitis), or the use of certain medications and chemicals (such as glucocorticoids, other specific drugs and after organ transplantation).[8]
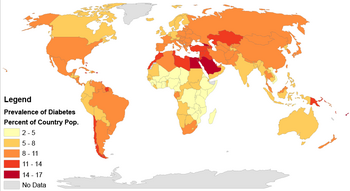
The number of people diagnosed as living with diabetes has increased sharply in recent decades, from 200 million in 1990 to 830 million by 2022.[9][10] It affects one in seven of the adult population, with type 2 diabetes accounting for more than 95% of cases. These numbers have already risen beyond earlier projections of 783 million adults by 2045.[11] The prevalence of the disease continues to increase, most dramatically in low- and middle-income nations.[12] Rates are similar in women and men, with diabetes being the seventh leading cause of death globally.[13][14] The global expenditure on diabetes-related healthcare is an estimated US$760 billion a year.[15]
Signs and symptoms
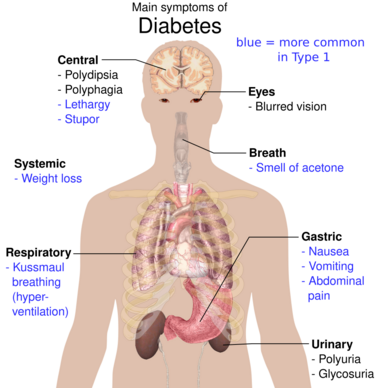

Common symptoms of diabetes include increased thirst, frequent urination, extreme hunger, and unintended weight loss.[16][17] Several other non-specific signs and symptoms may also occur, including fatigue, blurred vision, sweet smelling urine/semen and genital itchiness due to Candida infection.[17] About half of affected individuals may also be asymptomatic.[17] Type 1 presents abruptly following a pre-clinical phase, while type 2 has a more insidious onset; patients may remain asymptomatic for many years.[18]
Diabetic ketoacidosis is a medical emergency that occurs most commonly in type 1, but may also occur in type 2 if it has been longstanding or if the individual has significant β-cell dysfunction.[19] Excessive production of ketone bodies leads to signs and symptoms including nausea, vomiting, abdominal pain, the smell of acetone in the breath, deep breathing known as Kussmaul breathing, and in severe cases decreased level of consciousness.[19] Hyperosmolar hyperglycemic state is another emergency characterized by dehydration secondary to severe hyperglycemia, with resultant hypernatremia leading to an altered mental state and possibly coma.[20]
Hypoglycemia is a recognized complication of insulin treatment used in diabetes.[21] An acute presentation can include mild symptoms such as sweating, trembling, and palpitations, to more serious effects including impaired cognition, confusion, seizures, coma, and rarely death.[21] Recurrent hypoglycemic episodes may lower the glycemic threshold at which symptoms occur, meaning mild symptoms may not appear before cognitive deterioration begins to occur.[21]
Long-term complications
The major long-term complications of diabetes relate to damage to blood vessels at both macrovascular and microvascular levels.[22][23] Diabetes doubles the risk of cardiovascular disease, and about 75% of deaths in people with diabetes are due to coronary artery disease.[24] Other macrovascular morbidities include stroke and peripheral artery disease.[25]
Microvascular disease affects the eyes, kidneys, and nerves.[22] Damage to the retina, known as diabetic retinopathy, is the most common cause of blindness in people of working age.[17] The eyes can also be affected in other ways, including development of cataract and glaucoma.[17] It is recommended that people with diabetes visit an optometrist or ophthalmologist once a year.[26]
Diabetic nephropathy is a major cause of chronic kidney disease, accounting for over 50% of patients on dialysis in the United States.[27] Diabetic neuropathy, damage to nerves, manifests in various ways, including sensory loss, neuropathic pain, and autonomic dysfunction (such as postural hypotension, diarrhoea, and erectile dysfunction).[17] Loss of pain sensation predisposes to trauma that can lead to diabetic foot problems (such as ulceration), the most common cause of non-traumatic lower-limb amputation.[17]
Hearing loss is another long-term complication associated with diabetes.[28]
Based on extensive data and numerous cases of gallstone disease, it appears that a causal link might exist between type 2 diabetes and gallstones. People with diabetes are at a higher risk of developing gallstones compared to those without diabetes.[29]
There is a link between cognitive deficit and diabetes; studies have shown that diabetic individuals are at a greater risk of cognitive decline, and have a greater rate of decline compared to those without the disease.[30] Diabetes increases the risk of dementia, and the earlier that one is diagnosed with diabetes, the higher the risk becomes.[31] The condition also predisposes to falls in the elderly, especially those treated with insulin.[32]
Types
| Feature | Type 1 diabetes | Type 2 diabetes |
|---|---|---|
| Onset | Sudden | Gradual, Insidious |
| Age at onset | Any age; average age at diagnosis being 24.[34] | Mostly in adults |
| Body size | Thin or normal[35] | Often obese |
| Ketoacidosis | Common | Rare |
| Autoantibodies | Usually present | Absent |
| Endogenous insulin | Low or absent | Normal, decreased or increased |
| Heritability | 0.69 to 0.88[36][37][38] | 0.47 to 0.77[39] |
| Prevalence
(age standardized) |
<2 per 1,000[40] | ~6% (men), ~5% (women)[41] |
Diabetes is classified by the World Health Organization into six categories: type 1 diabetes, type 2 diabetes, hybrid forms of diabetes (including slowly evolving, immune-mediated diabetes of adults and ketosis-prone type 2 diabetes), hyperglycemia first detected during pregnancy, "other specific types", and "unclassified diabetes".[42] Diabetes is a more variable disease than once thought, and individuals may have a combination of forms.[43]
Type 1
Type 1 accounts for 5 to 10% of diabetes cases and is the most common type of diabetes diagnosed in patients under 20 years;[44] however, the older term "juvenile-onset diabetes" is no longer used as onset in adulthood is possible.[27] The disease is characterized by loss of the insulin-producing beta cells of the pancreatic islets, leading to severe insulin deficiency, and can be further classified as immune-mediated or idiopathic (without known cause).[44] The majority of cases are immune-mediated, in which a T cell-mediated autoimmune attack causes loss of beta cells and thus insulin deficiency.[45] Patients often have irregular and unpredictable blood sugar levels due to very low insulin and an impaired counter-response to hypoglycemia.[46]

Type 1 diabetes is partly inherited, with multiple genes, including certain HLA genotypes, known to influence the risk of diabetes. In genetically susceptible people, the onset of diabetes can be triggered by one or more environmental factors,[47] such as a viral infection or diet. Several viruses have been implicated, but to date there is no stringent evidence to support this hypothesis in humans.[47][48]
Type 1 diabetes can occur at any age, and a significant proportion is diagnosed during adulthood. Latent autoimmune diabetes of adults (LADA) is the diagnostic term applied when type 1 diabetes develops in adults; it has a slower onset than the same condition in children. Given this difference, some use the unofficial term "type 1.5 diabetes" for this condition.[49] Adults with LADA are frequently initially misdiagnosed as having type 2 diabetes, based on age rather than a cause.[50] LADA leaves adults with higher levels of insulin production than type 1 diabetes, but not enough insulin production for healthy blood sugar levels.[51][52]
Type 2

Type 2 diabetes is characterized by insulin resistance, which may be combined with relatively reduced insulin secretion.[3] The defective responsiveness of body tissues to insulin is believed to involve the insulin receptor.[53] However, the specific defects are not known. Diabetes mellitus cases due to a known defect are classified separately. Type 2 diabetes is the most common type of diabetes mellitus accounting for 95% of diabetes.[54] Many people with type 2 diabetes have evidence of prediabetes (impaired fasting glucose and/or impaired glucose tolerance) before meeting the criteria for type 2 diabetes.[55] The progression of prediabetes to overt type 2 diabetes can be slowed or reversed by lifestyle changes or medications that improve insulin sensitivity or reduce the liver's glucose production.[56]
Type 2 diabetes is primarily due to lifestyle factors and genetics.[57] A number of lifestyle factors are known to be important to the development of type 2 diabetes, including obesity (defined by a body mass index of greater than 30), lack of physical activity, poor diet such as Western Pattern Diet, and stress.[33][58] Excess body fat is associated with 30% of cases in people of Chinese and Japanese descent, 60–80% of cases in those of European and African descent, and 100% of Pima Indians and Pacific Islanders.[3] Even those who are not obese may have a high waist–hip ratio.[3]
Dietary factors such as sugar-sweetened drinks are associated with an increased risk.[59][60][61] The type of fats in the diet is also important, with saturated fat and trans fats increasing the risk and polyunsaturated and monounsaturated fat decreasing the risk.[57] Eating white rice excessively may increase the risk of diabetes, especially in Chinese and Japanese people.[62]
Adverse childhood experiences, including abuse, neglect, and household difficulties, increase the likelihood of type 2 diabetes later in life by 32%, with neglect having the strongest effect.[63]
Antipsychotic medication, SSRI, and SNRI side effects (specifically metabolic abnormalities, dyslipidemia and weight gain) are also potential risk factors.[64]
Gestational diabetes
Gestational diabetes resembles type 2 diabetes in several respects, involving a combination of relatively inadequate insulin secretion and responsiveness. It occurs in about 2–10% of all pregnancies and may improve or disappear after delivery.[65] It is recommended that all pregnant women get tested starting around 24–28 weeks gestation.[66] It is most often diagnosed in the second or third trimester because of the increase in insulin-antagonist hormone levels that occurs at this time.[66] However, after pregnancy approximately 5–10% of women with gestational diabetes are found to have another form of diabetes, most commonly type 2.[65] Gestational diabetes is fully treatable, but requires careful medical supervision throughout the pregnancy. Management may include dietary changes, blood glucose monitoring, and in some cases, insulin may be required.[67]
Though it may be transient, untreated gestational diabetes can damage the health of the fetus or mother. Risks to the baby include macrosomia (high birth weight), congenital heart and central nervous system abnormalities, and skeletal muscle malformations. Increased levels of insulin in a fetus's blood may inhibit fetal surfactant production and cause infant respiratory distress syndrome. A high blood bilirubin level may result from red blood cell destruction. In severe cases, perinatal death may occur, most commonly as a result of poor placental perfusion due to vascular impairment. Labor induction may be indicated with decreased placental function. A caesarean section may be performed if there is marked fetal distress[68] or an increased risk of injury associated with macrosomia, such as shoulder dystocia.[69]
As the risk of developing type 2 diabetes is about 10 times higher in women with a history of gestational diabetes, postpartum screening may involve dietary, lifestyle, and drug interventions to prevent or delay its progression.[70]
Maturity-onset diabetes of the young
Maturity-onset diabetes of the young (MODY) is a rare autosomal dominant inherited form of diabetes, due to one of several single-gene mutations causing defects in insulin production.[71] It is significantly less common than the three main types, constituting 1–2% of all cases. The name of this disease refers to early hypotheses as to its nature. Being due to a defective gene, this disease varies in age at presentation and in severity according to the specific gene defect; thus, there are at least 14 subtypes of MODY.[72] People with MODY often can control it without using insulin.[73]
Malnutrition-related
Malnutrition-related diabetes, also termed Type 5 diabetes, involves decreased insulin production, similar to Type 1 diabetes, but is primarily related to malnutrition rather than autoimmune damage of pancreas beta cells. Unlike in Type 1 diabetes, patients with Type 5 diabetes do not develop ketonuria or ketosis.[74][75] The ICD-10 (1992) diagnostic entity, malnutrition-related diabetes mellitus (ICD-10 code E12), was previously deprecated by the World Health Organization (WHO) when the current taxonomy was introduced in 1999.[76]
Other types
Some cases of diabetes are caused by the body's tissue receptors not responding to insulin (even when insulin levels are normal, which is what separates it from type 2 diabetes); this form is very uncommon. Genetic mutations (autosomal or mitochondrial) can lead to defects in beta cell function. Abnormal insulin action may also have been genetically determined in some cases. Any disease that causes extensive damage to the pancreas may lead to diabetes (for example, chronic pancreatitis and cystic fibrosis). Diseases associated with excessive secretion of insulin-antagonistic hormones can cause diabetes (which is typically resolved once the hormone excess is removed). Many drugs impair insulin secretion and some toxins damage pancreatic beta cells, whereas others increase insulin resistance (especially glucocorticoids which can provoke "steroid diabetes").[77] Yet another form of diabetes that people may develop is double diabetes. This is when a type 1 diabetic becomes insulin resistant, the hallmark for type 2 diabetes or has a family history for type 2 diabetes.[78] It was first discovered in 1990 or 1991.
The following is a list of disorders that may increase the risk of diabetes:[77] Template:Col-float-begin
- Genetic defects of β-cell function
- Maturity onset diabetes of the young
- Mitochondrial DNA mutations
- Genetic defects in insulin processing or insulin action
- Defects in proinsulin conversion
- Insulin gene mutations
- Insulin receptor mutations
- Exocrine pancreatic defects (see Type 3c diabetes, i.e. pancreatogenic diabetes)
- Chronic pancreatitis
- Pancreatectomy
- Pancreatic neoplasia
- Cystic fibrosis
- Hemochromatosis
- Fibrocalculous pancreatopathy
- Endocrinopathies
- Growth hormone excess (acromegaly)
- Cushing syndrome
- Hyperthyroidism
- Hypothyroidism
- Pheochromocytoma
- Glucagonoma
- Infections
- Cytomegalovirus infection
- Coxsackievirus B
- Drugs
- Glucocorticoids
- Thyroid hormone
- β-adrenergic agonists
- Statins[79]
Pathophysiology


Insulin is the principal hormone that regulates the uptake of glucose from the blood into most cells of the body, especially liver, adipose tissue and muscle, except smooth muscle, in which insulin acts via the IGF-1.[80] Therefore, deficiency of insulin or the insensitivity of its receptors play a central role in all forms of diabetes mellitus.[81]
The body obtains glucose from three main sources: the intestinal absorption of food; the breakdown of glycogen (glycogenolysis), the storage form of glucose found in the liver; and gluconeogenesis, the generation of glucose from non-carbohydrate substrates in the body.[82] Insulin plays a critical role in regulating glucose levels in the body. Insulin can inhibit the breakdown of glycogen or the process of gluconeogenesis, it can stimulate the transport of glucose into fat and muscle cells, and it can stimulate the storage of glucose in the form of glycogen.[82]
Insulin is released into the blood by beta cells (β-cells), found in the islets of Langerhans in the pancreas, in response to rising levels of blood glucose, typically after eating. Insulin is used by about two-thirds of the body's cells to absorb glucose from the blood for use as fuel, for conversion to other needed molecules, or for storage. Lower glucose levels result in decreased insulin release from the beta cells and in the breakdown of glycogen to glucose. This process is mainly controlled by the hormone glucagon, which acts in the opposite manner to insulin.[83]
If the amount of insulin available is insufficient, or if cells respond poorly to the effects of insulin (insulin resistance), or if the insulin itself is defective, then glucose is not absorbed properly by the body cells that require it, and is not stored appropriately in the liver and muscles. The net effect is persistently high levels of blood glucose, poor protein synthesis, and other metabolic derangements, such as metabolic acidosis in cases of complete insulin deficiency.[82]
When there is too much glucose in the blood for a long time, the kidneys cannot absorb it all (reach a threshold of reabsorption) and the extra glucose gets passed out of the body through urine (glycosuria).[84] This increases the osmotic pressure of the urine and inhibits reabsorption of water by the kidney, resulting in increased urine production (polyuria) and increased fluid loss. Lost blood volume is replaced osmotically from water in body cells and other body compartments, causing dehydration and increased thirst (polydipsia).[82] In addition, intracellular glucose deficiency stimulates appetite leading to excessive food intake (polyphagia).[85]
Diagnosis
Diabetes mellitus is diagnosed with a test for the glucose content in the blood, and is diagnosed by demonstrating any one of the following:[76]
- Fasting plasma glucose level ≥ 7.0 mmol/L (126 mg/dL). For this test, blood is taken after a period of fasting, i.e. in the morning before breakfast, after the patient had sufficient time to fast overnight or at least 8 hours before the test.
- Plasma glucose ≥ 11.1 mmol/L (200 mg/dL) two hours after a 75 gram oral glucose load as in a glucose tolerance test (OGTT)
- Symptoms of high blood sugar and plasma glucose ≥ 11.1 mmol/L (200 mg/dL) either while fasting or not fasting
- Glycated hemoglobin (HbA1C) ≥ 48 mmol/mol (≥ 6.5 DCCT %).[86]
Template:OGTT A positive result, in the absence of unequivocal high blood sugar, should be confirmed by a repeat of any of the above methods on a different day. It is preferable to measure a fasting glucose level because of the ease of measurement and the considerable time commitment of formal glucose tolerance testing, which takes two hours to complete and offers no prognostic advantage over the fasting test.[87] According to the current definition, two fasting glucose measurements at or above 7.0 mmol/L (126 mg/dL) is considered diagnostic for diabetes mellitus.
Per the WHO, people with fasting glucose levels from 6.1 to 6.9 mmol/L (110 to 125 mg/dL) are considered to have impaired fasting glucose.[88] People with plasma glucose at or above 7.8 mmol/L (140 mg/dL), but not over 11.1 mmol/L (200 mg/dL), two hours after a 75 gram oral glucose load are considered to have impaired glucose tolerance. Of these two prediabetic states, the latter in particular is a major risk factor for progression to full-blown diabetes mellitus, as well as cardiovascular disease.[89] The American Diabetes Association (ADA) since 2003 uses a slightly different range for impaired fasting glucose of 5.6 to 6.9 mmol/L (100 to 125 mg/dL).[90]
Glycated hemoglobin is better than fasting glucose for determining risks of cardiovascular disease and death from any cause.[91]
Prevention
There is no known preventive measure for type 1 diabetes.[54] However, islet autoimmunity and multiple antibodies can be a strong predictor of the onset of type 1 diabetes.[92] Type 2 diabetes—which accounts for 85–90% of all cases worldwide—can often be prevented or delayed[93] by maintaining a normal body weight, engaging in physical activity, and eating a healthy diet.[54] Higher levels of physical activity (more than 90 minutes per day) reduce the risk of diabetes by 28%.[94] Dietary changes known to be effective in helping to prevent diabetes include maintaining a diet rich in whole grains and fiber, and choosing good fats, such as the polyunsaturated fats found in nuts, vegetable oils, and fish.[95] Limiting sugary beverages and eating less red meat and other sources of saturated fat can also help prevent diabetes.[95] Tobacco smoking is also associated with an increased risk of diabetes and its complications, so smoking cessation can be an important preventive measure as well.[96]
The relationship between type 2 diabetes and the main modifiable risk factors (excess weight, unhealthy diet, physical inactivity and tobacco use) is similar in all regions of the world. There is growing evidence that the underlying determinants of diabetes are a reflection of the major forces driving social, economic and cultural change: globalization, urbanization, population aging, and the general health policy environment.[97]
Comorbidity
Diabetes patients' comorbidities have a significant impact on medical expenses and related costs. It has been demonstrated that patients with diabetes are more likely to experience respiratory, urinary tract, and skin infections, develop atherosclerosis, hypertension, and chronic kidney disease, putting them at increased risk of infection and complications that require medical attention.[98] Patients with diabetes mellitus are more likely to experience certain infections, such as COVID-19, with prevalence rates ranging from 5.3 to 35.5%.[99][100] Maintaining adequate glycemic control is the primary goal of diabetes management since it is critical to managing diabetes and preventing or postponing such complications.[101]
People with type 1 diabetes have higher rates of autoimmune disorders than the general population. An analysis of a type 1 diabetes registry found that 27% of the 25,000 participants had other autoimmune disorders.[102] Between 2% and 16% of people with type 1 diabetes also have celiac disease.[102]
Management
Diabetes management concentrates on keeping blood sugar levels close to normal, without causing low blood sugar.[103] This can usually be accomplished with dietary changes,[104] exercise, weight loss, and use of appropriate medications (insulin, oral medications).[103]
Learning about the disease and actively participating in the treatment is important, since complications are far less common and less severe in people who have well-managed blood sugar levels.[103][105] The goal of treatment is an A1C level below 7%.[106][107] Attention is also paid to other health problems that may accelerate the negative effects of diabetes. These include smoking, high blood pressure, metabolic syndrome obesity, and lack of regular exercise.[103][108] Specialized footwear is widely used to reduce the risk of diabetic foot ulcers by relieving the pressure on the foot.[109][110][111] Foot examination for patients living with diabetes should be done annually which includes sensation testing, foot biomechanics, vascular integrity and foot structure.[112]
Concerning those with severe mental illness, the efficacy of type 2 diabetes self-management interventions is still poorly explored, with insufficient scientific evidence to show whether these interventions have similar results to those observed in the general population.[113]
Lifestyle
People with diabetes can benefit from education about the disease and treatment, dietary changes, and exercise, with the goal of keeping both short-term and long-term blood glucose levels within acceptable bounds. In addition, given the associated higher risks of cardiovascular disease, lifestyle modifications are recommended to control blood pressure.[114][115]
Weight loss can prevent progression from prediabetes to diabetes type 2, decrease the risk of cardiovascular disease, or result in a partial remission in people with diabetes.[116][117] No single dietary pattern is best for all people with diabetes.[118] Healthy dietary patterns, such as the Mediterranean diet, low-carbohydrate diet, or DASH diet, are often recommended, although evidence does not support one over the others.[116][117] According to the ADA, "reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia", and for individuals with type 2 diabetes who cannot meet the glycemic targets or where reducing anti-glycemic medications is a priority, low or very-low carbohydrate diets are a viable approach.[117] For overweight people with type 2 diabetes, any diet that achieves weight loss is effective.[118][119]
A 2020 Cochrane systematic review compared several non-nutritive sweeteners to sugar, placebo and a nutritive low-calorie sweetener (tagatose), but the results were unclear for effects on HbA1c, body weight and adverse events.[120] The studies included were mainly of very low-certainty and did not report on health-related quality of life, diabetes complications, all-cause mortality or socioeconomic effects.[120]
In children
While type 1 diabetes is more prevalent in pediatric diabetes, type 2 diabetes has increasing prevalence, accounting for some 33% of new diagnoses.[121][122] Risk factors for type 2 diabetes include ethnicity, family history, sedentary lifestyle, unhealthy diet, a mother with gestational diabetes, female gender, and obesity.[121] Children with type 2 diabetes have increased risk of developing complications, which include insulin resistance, hyperglycemia, polyuria, ketosis, and dehydration.[121] Early recognition, screening, treatment, and education of diabetic children are needed to prevent long-term disease complications.[121][123]
Screening for type 2 diabetes typically starts at 10 years old for obese children and those who have at least two risk factors.[121] Diagnostic criteria include plasma blood glucose of more than 200 mg per deciliter (dl) or a fasting blood glucose above 126 mg per dl in children with overt symptoms. Differentiating type 1 from type 2 diabetes may include assessment of fasting blood insulin or C-peptide, or determination of autoantibodies for type 1 diabetes.[121]
Treatment and management
Adoption of healthy lifestyle practices and metformin medication are recommended as initial treatments.[121][122] Lifestyle changes include daily exercise for at least 60 minutes, reduced screen time, and dietary education.[121][123]
Metformin at 500 mg per day is used upon diagnosis.[121] Insulin is used for children with a blood glucose of more than 250 mg per dl and a hemoglobin A1c greater than 8.5%.[121]
Education
Diabetes management for children requires the integration of the family and health care team to be committed and continuous for promotion of self-management.[123] A health care team may include a pediatric endocrinologist or physician trained in pediatric diabetes, a diabetes specialist nurse, a registered dietitian, a psychologist, a social worker, and child life specialist.[123]
The goal of the health care team and child's family is to empower the child to make informed decisions for health‐promoting lifestyle choices.[123]
Medications
Glucose control
Most medications used to treat diabetes act by lowering blood sugar levels through different mechanisms. There is broad consensus that when people with diabetes maintain tight glucose control – keeping the glucose levels in their blood within normal ranges – they experience fewer complications, such as kidney problems or eye problems.[124][125] There is, however, debate as to whether this is appropriate and cost effective for people later in life in whom the risk of hypoglycemia may be more significant.[126]
There are a number of different classes of anti-diabetic medications. Type 1 diabetes requires treatment with insulin, ideally using a "basal bolus" regimen that most closely matches normal insulin release: long-acting insulin for the basal rate and short-acting insulin with meals.[127] Type 2 diabetes is generally treated with medication that is taken by mouth (e.g. metformin) although some eventually require injectable treatment with insulin or GLP-1 agonists.[128]
Metformin is generally recommended as a first-line treatment for type 2 diabetes, as there is good evidence that it decreases mortality.[129] It works by decreasing the liver's production of glucose, and increasing the amount of glucose stored in peripheral tissue.[130] Several other groups of drugs, mainly oral medication, may also decrease blood sugar in type 2 diabetes. These include agents that increase insulin release (sulfonylureas), agents that decrease absorption of sugar from the intestines (acarbose), agents that inhibit the enzyme dipeptidyl peptidase-4 (DPP-4) that inactivates incretins such as GLP-1 and GIP (sitagliptin), agents that make the body more sensitive to insulin (thiazolidinedione) and agents that increase the excretion of glucose in the urine (SGLT2 inhibitors).[130] When insulin is used in type 2 diabetes, a long-acting formulation is usually added initially, while continuing oral medications.[129]
Some severe cases of type 2 diabetes may also be treated with insulin, which is increased gradually until glucose targets are reached.[129][131]
Blood pressure lowering
Cardiovascular disease is a serious complication associated with diabetes, and many international guidelines recommend blood pressure treatment targets that are lower than 140/90 mmHg for people with diabetes.[132] However, there is only limited evidence regarding what the lower targets should be. A 2016 systematic review found potential harm to treating to targets lower than 140 mmHg,[133] and a subsequent systematic review in 2019 found no evidence of additional benefit from blood pressure lowering to between 130 – 140mmHg, although there was an increased risk of adverse events.[134]
2015 American Diabetes Association recommendations are that people with diabetes and albuminuria should receive an inhibitor of the renin-angiotensin system to reduce the risks of progression to end-stage renal disease, cardiovascular events, and death.[135] There is some evidence that angiotensin converting enzyme inhibitors (ACEIs) are superior to other inhibitors of the renin-angiotensin system such as angiotensin receptor blockers (ARBs),[136] or aliskiren in preventing cardiovascular disease.[137] Although a more recent review found similar effects of ACEIs and ARBs on major cardiovascular and renal outcomes.[138] There is no evidence that combining ACEIs and ARBs provides additional benefits.[138]
Aspirin
The use of aspirin to prevent cardiovascular disease in diabetes is controversial.[135] Aspirin is recommended by some in people at high risk of cardiovascular disease; however, routine use of aspirin has not been found to improve outcomes in uncomplicated diabetes.[139] 2015 American Diabetes Association recommendations for aspirin use (based on expert consensus or clinical experience) are that low-dose aspirin use is reasonable in adults with diabetes who are at intermediate risk of cardiovascular disease (10-year cardiovascular disease risk, 5–10%).[135] National guidelines for England and Wales by the National Institute for Health and Care Excellence (NICE) recommend against the use of aspirin in people with type 1 or type 2 diabetes who do not have confirmed cardiovascular disease.[127][128]
Surgery
Weight loss surgery in those with obesity and type 2 diabetes is often an effective measure.[140] Many are able to maintain normal blood sugar levels with little or no medications following surgery[141] and long-term mortality is decreased.[142] There is, however, a short-term mortality risk of less than 1% from the surgery.[143] The body mass index cutoffs for when surgery is appropriate are not yet clear.[142] It is recommended that this option be considered in those who are unable to get both their weight and blood sugar under control.[144]
A pancreas transplant is occasionally considered for people with type 1 diabetes who have severe complications of their disease, including end stage kidney disease requiring kidney transplantation.[145]
Diabetic peripheral neuropathy (DPN) affects 30% of all diabetes patients.[146] When DPN is superimposed with nerve compression, DPN may be treatable with multiple nerve decompressions.[147][148] The theory is that DPN predisposes peripheral nerves to compression at anatomical sites of narrowing, and that the majority of DPN symptoms are actually attributable to nerve compression, a treatable condition, rather than DPN itself.[149][150] The surgery is associated with lower pain scores, higher two-point discrimination (a measure of sensory improvement), lower rate of ulcerations, fewer falls (in the case of lower extremity decompression), and fewer amputations.[150][151][147][148]
Self-management and support
In countries using a general practitioner system, such as the United Kingdom, care may take place mainly outside hospitals, with hospital-based specialist care used only in case of complications, difficult blood sugar control, or research projects. In other circumstances, general practitioners and specialists share care in a team approach. Evidence has shown that social prescribing led to slight improvements in blood sugar control for people with type 2 diabetes.[152] Home telehealth support can be an effective management technique.[153]
The use of technology to deliver educational programs for adults with type 2 diabetes includes computer-based self-management interventions to collect for tailored responses to facilitate self-management.[154] There is no adequate evidence to support effects on cholesterol, blood pressure, behavioral change (such as physical activity levels and dietary), depression, weight and health-related quality of life, nor in other biological, cognitive or emotional outcomes.[154][155]
Epidemiology

An estimated 382 million people worldwide had diabetes in 2013[156] up from 108 million in 1980.[157] Accounting for the shifting age structure of the global population, the prevalence of diabetes is 8.8% among adults, nearly double the rate of 4.7% in 1980.[158][157] Type 2 makes up about 90% of the cases.[13][33] Some data indicate rates are roughly equal in women and men,[13] but male excess in diabetes has been found in many populations with higher type 2 incidence, possibly due to sex-related differences in insulin sensitivity, consequences of obesity and regional body fat deposition, and other contributing factors such as high blood pressure, tobacco smoking, and alcohol intake.[159][160]
The WHO estimates that diabetes resulted in 1.5 million deaths in 2012, making it the 8th leading cause of death.[161][157] However, another 2.2 million deaths worldwide were attributable to high blood glucose and the increased risks of cardiovascular disease and other associated complications (e.g. kidney failure), which often lead to premature death and are often listed as the underlying cause on death certificates rather than diabetes.[157][162] For example, in 2017, the International Diabetes Federation (IDF) estimated that diabetes resulted in 4.0 million deaths worldwide,[158] using modeling to estimate the total number of deaths that could be directly or indirectly attributed to diabetes.[158]
Diabetes occurs throughout the world but is more common (especially type 2) in more developed countries. The greatest increase in rates has, however, been seen in low- and middle-income countries,[157] where more than 80% of diabetic deaths occur.[163] The fastest prevalence increase is expected to occur in Asia and Africa, where most people with diabetes will probably live in 2030.[164] The increase in rates in developing countries follows the trend of urbanization and lifestyle changes, including increasingly sedentary lifestyles, less physically demanding work and the global nutrition transition, marked by increased intake of foods that are high energy-dense but nutrient-poor (often high in sugar and saturated fats, sometimes referred to as the "Western-style" diet).[157][164] The global number of diabetes cases might increase by 48% between 2017 and 2045.[158]
As of 2020, 38% of all US adults had prediabetes.[165] Prediabetes is an early stage of diabetes.
History
Diabetes was one of the first diseases described,[166] with an Egyptian manuscript from c. 1500 BCE mentioning "too great emptying of the urine."[167] The Ebers papyrus includes a recommendation for a drink to take in such cases.[168] The first described cases are believed to have been type 1 diabetes.[167] Indian physicians around the same time identified the disease and classified it as madhumeha or "honey urine", noting the urine would attract ants.[167][168]
The term "diabetes" or "to pass through" was first used in 230 BCE by the Greek Apollonius of Memphis.[167] The disease was considered rare during the time of the Roman empire, with Galen commenting he had only seen two cases during his career.[167] This is possibly due to the diet and lifestyle of the ancients, or because the clinical symptoms were observed during the advanced stage of the disease. Galen named the disease "diarrhea of the urine" (diarrhea urinosa).[169]
The earliest surviving work with a detailed reference to diabetes is that of Aretaeus of Cappadocia (2nd or early 3rd century CE). He described the symptoms and the course of the disease, which he attributed to the moisture and coldness, reflecting the beliefs of the "Pneumatic School". He hypothesized a correlation between diabetes and other diseases, and he discussed differential diagnosis from the snakebite, which also provokes excessive thirst. His work remained unknown in the West until 1552, when the first Latin edition was published in Venice.[169]
Two types of diabetes were identified as separate conditions for the first time by the Indian physicians Sushruta and Charaka in 400–500 CE with one type being associated with youth and another type with being overweight.[167] Effective treatment was not developed until the early part of the 20th century when Canadians Frederick Banting and Charles Best isolated and purified insulin in 1921 and 1922.[167] This was followed by the development of the long-acting insulin NPH in the 1940s.[167]
Etymology
The word diabetes (/ˌdaɪ.əˈbiːtiːz/ or /ˌdaɪ.əˈbiːtɪs/) comes from Latin diabētēs, which in turn comes from Ancient Greek διαβήτης (diabētēs), which literally means "a passer through; a siphon".[170] Ancient Greek physician Aretaeus of Cappadocia (fl. 2nd century CE) used that word, with the intended meaning "excessive discharge of urine", as the name for the disease.[171][172] Ultimately, the word comes from Greek διαβαίνειν (diabainein), meaning "to pass through",[170] which is composed of δια- (dia-), meaning "through" and βαίνειν (bainein), meaning "to go".[171] The word "diabetes" is first recorded in English, in the form diabete, in a medical text written around 1425.
The word mellitus (/məˈlaɪtəs/ or /ˈmɛlɪtəs/) comes from the classical Latin word mellītus, meaning "mellite"[173] (i.e. sweetened with honey;[173] honey-sweet[174]). The Latin word comes from mell-, which comes from mel, meaning "honey";[173][174] sweetness;[174] pleasant thing,[174] and the suffix -ītus,[173] whose meaning is the same as that of the English suffix "-ite".[175] It was Thomas Willis who in 1675 added "mellitus" to the word "diabetes" as a designation for the disease, when he noticed the urine of a person with diabetes had a sweet taste (glycosuria). This sweet taste had been noticed in urine by the ancient Greeks, Chinese, Egyptians, and Indians.[176]
Society and culture
The 1989 "St. Vincent Declaration"[177][178] was the result of international efforts to improve the care accorded to those with diabetes. Doing so is important not only in terms of quality of life and life expectancy but also economically – expenses due to diabetes have been shown to be a major drain on health – and productivity-related resources for healthcare systems and governments.
Several countries established more and less successful national diabetes programmes to improve treatment of the disease.[179]
Diabetes stigma
Diabetes stigma describes the negative attitudes, judgment, discrimination, or prejudice against people with diabetes. Often, the stigma stems from the idea that diabetes (particularly Type 2 diabetes) resulted from poor lifestyle and unhealthy food choices rather than other causal factors such as genetics and social determinants of health.[180] Manifestation of stigma can be seen throughout different cultures and contexts. Scenarios include diabetes statuses affecting marriage proposals, workplace-employment, and social standing in communities.[181]
Stigma is also seen internally, as people with diabetes can also have negative beliefs about themselves. Often these cases of self-stigma are associated with higher diabetes-specific distress, lower self-efficacy, higher rates of depression, and poorer provider-patient interactions during diabetes care.[182]
Racial and economic inequalities
Racial and ethnic minorities are disproportionately affected with higher prevalence of diabetes compared to non-minority individuals.[183] While US adults overall have a 40% chance of developing type 2 diabetes, Hispanic/Latino adults chance is more than 50%.[184] African Americans also are much more likely to be diagnosed with diabetes compared to White Americans. Asians have increased risk of diabetes as diabetes can develop at lower BMI due to differences in visceral fat compared to other races. For Asians, diabetes can develop at a younger age and lower body fat compared to other groups. Additionally, diabetes is highly underreported in Asian American people, as 1 in 3 cases are undiagnosed compared to the average 1 in 5 for the nation.[185]
People with diabetes who have neuropathic symptoms such as numbness or tingling in feet or hands are twice as likely to be unemployed as those without the symptoms.[186]
In 2010, diabetes-related emergency room (ER) visit rates in the United States were higher among people from the lowest income communities (526 per 10,000 population) than from the highest income communities (236 per 10,000 population). Approximately 9.4% of diabetes-related ER visits were for the uninsured.[187]
Naming
The term "type 1 diabetes" has replaced several former terms, including childhood-onset diabetes, juvenile diabetes, and insulin-dependent diabetes mellitus. Likewise, the term "type 2 diabetes" has replaced several former terms, including adult-onset diabetes, obesity-related diabetes, and noninsulin-dependent diabetes mellitus. Beyond these two types, there is no agreed-upon standard nomenclature.[188]
Diabetes mellitus is also occasionally known as "sugar diabetes" to differentiate it from diabetes insipidus.[189] Diabetes insipidus is an unrelated disease with symptoms that can mimic diabetes mellitus.
Diabetes in other animals
Diabetes can occur in mammals or reptiles.[190][191] Birds do not develop diabetes because of their unusually high tolerance for elevated blood glucose levels.[192] There is some indication that amphibians have the ability to develop diabetes.[193]
In animals, diabetes is most commonly encountered in dogs and cats. Middle-aged animals are most commonly affected. Female dogs are twice as likely to be affected as males, while according to some sources, male cats are more prone than females. In both species, all breeds may be affected, but some small dog breeds are particularly likely to develop diabetes, such as Miniature Poodles.[194]
Feline diabetes is strikingly similar to human type 2 diabetes. The Burmese, Russian Blue, Abyssinian, and Norwegian Forest cat breeds are at higher risk than other breeds. Overweight cats are also at higher risk.[195]
The symptoms may relate to fluid loss and polyuria, but the course may also be insidious. Diabetic animals are more prone to infections. The long-term complications recognized in humans are much rarer in animals. The principles of treatment (weight loss, oral antidiabetics, subcutaneous insulin) and management of emergencies (e.g. ketoacidosis) are similar to those in humans.[194]
See also
References
- ↑ 1.0 1.1 "Diabetes". https://www.who.int/health-topics/diabetes.
- ↑ "Diabetes Mellitus (DM) – Hormonal and Metabolic Disorders". https://www.msdmanuals.com/en-gb/home/hormonal-and-metabolic-disorders/diabetes-mellitus-dm-and-disorders-of-blood-sugar-metabolism/diabetes-mellitus-dm.
- ↑ 3.0 3.1 3.2 3.3 "Chapter 17". Greenspan's basic & clinical endocrinology (9th ed.). New York: McGraw-Hill Medical. 2011. ISBN 978-0-07-162243-1.
- ↑ "Hyperglycemic crises in adult patients with diabetes". Diabetes Care 32 (7): 1335–1343. July 2009. doi:10.2337/dc09-9032. PMID 19564476. PMC 2699725. http://care.diabetesjournals.org/content/32/7/1335.full.
- ↑ Cite error: Invalid
<ref>tag; no text was provided for refs namedIDF2019 - ↑ "Symptoms and Causes of Diabetes". National Institute of Diabetes and Digestive and Kidney Diseases, US National Institutes of Health. 2024. https://www.niddk.nih.gov/health-information/diabetes/overview/symptoms-causes.
- ↑ "Type 1 vs Type 2 Diabetes | UVA Health". https://uvahealth.com/services/diabetes-care/types.
- ↑ American Diabetes Association (2020-12-04). "2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes—2021". Diabetes Care 44 (Supplement_1): S15–S33. doi:10.2337/dc21-S002. ISSN 0149-5992. https://diabetesjournals.org/care/article/44/Supplement_1/S15/30859/2-Classification-and-Diagnosis-of-Diabetes.
- ↑ "Diabetes" (in en). https://www.who.int/news-room/fact-sheets/detail/diabetes.
- ↑ "The top 10 causes of death" (in en). https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- ↑ "Facts & figures". https://idf.org/about-diabetes/facts-figures/.
- ↑ "Inequalities in the prevalence of diabetes mellitus and its risk factors in Sri Lanka: a lower middle income country". International Journal for Equity in Health 17 (1): 45. April 2018. doi:10.1186/s12939-018-0759-3. PMID 29665834.
- ↑ 13.0 13.1 13.2 Vos, T.Expression error: Unrecognized word "et". (December 2012). "Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2163–2196. doi:10.1016/S0140-6736(12)61729-2. PMID 23245607.
- ↑ "The top 10 causes of death". https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death.
- ↑ "Global Economic Burden of Diabetes in Adults: Projections From 2015 to 2030". Diabetes Care 41 (5): 963–970. May 2018. doi:10.2337/dc17-1962. PMID 29475843.
- ↑ "Diabetes". February 17, 2023. https://my.clevelandclinic.org/health/diseases/7104-diabetes.
- ↑ 17.0 17.1 17.2 17.3 17.4 17.5 17.6 Kumar and Clark's Clinical Medicine (10th ed.). Elsevier. 2021. pp. 699–741. ISBN 978-0-7020-7868-2.
- ↑ Goldman-Cecil Medicine (26th ed.). Elsevier. 2020. pp. 1490–1510. ISBN 978-0-323-53266-2.
- ↑ 19.0 19.1 Davidson's Principles and Practice of Medicine (24th ed.). Elsevier. 2023. pp. 703–753. ISBN 978-0-7020-8348-8.
- ↑ "Hyperglycaemic presentations in type 2 diabetes". Australian Journal of General Practice 48 (5): 263–267. May 2019. doi:10.31128/AJGP-12-18-4785. PMID 31129935. https://www1.racgp.org.au/ajgp/2019/may/hyperglycaemic-presentations-in-type-2-diabetes. Retrieved 2023-08-10.
- ↑ 21.0 21.1 21.2 "The consequences of hypoglycaemia". Diabetologia 64 (5): 963–970. May 2021. doi:10.1007/s00125-020-05366-3. PMID 33550443.
- ↑ 22.0 22.1 "Diabetes – long-term effects". Department of Health. http://www.betterhealth.vic.gov.au/health/conditionsandtreatments/diabetes-long-term-effects.
- ↑ "Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies". Lancet 375 (9733): 2215–2222. June 2010. doi:10.1016/S0140-6736(10)60484-9. PMID 20609967.
- ↑ "2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines". Circulation 127 (4): e362–e425. January 2013. doi:10.1161/CIR.0b013e3182742cf6. PMID 23247304.
- ↑ "Complications of Diabetes 2017". Journal of Diabetes Research 2018: 3086167. 11 March 2018. doi:10.1155/2018/3086167. PMID 29713648.
- ↑ "Diabetes eye care". National Library of Medicine. https://medlineplus.gov/ency/patientinstructions/000078.htm.
- ↑ 27.0 27.1 Cecil Essentials of Medicine (10th ed.). Pennsylvania: Elsevier. 2022. pp. 282–297, 662–677. ISBN 978-0-323-72271-1.
- ↑ "A systematic review of the association of Type I diabetes with sensorineural hearing loss". PLOS ONE 19 (2): e0298457. 9 February 2024. doi:10.1371/journal.pone.0298457. PMID 38335215. Bibcode: 2024PLoSO..1998457M.
- ↑ "Obesity, Type 2 Diabetes, Lifestyle Factors, and Risk of Gallstone Disease: A Mendelian Randomization Investigation". Clinical Gastroenterology and Hepatology 20 (3): e529–e537. March 2022. doi:10.1016/j.cgh.2020.12.034. PMID 33418132.
- ↑ "Cognitive decline and dementia in diabetes--systematic overview of prospective observational studies". Diabetologia 48 (12): 2460–2469. December 2005. doi:10.1007/s00125-005-0023-4. PMID 16283246.
- ↑ "What's the relationship between diabetes and dementia?" (in en). 2021-07-12. https://www.health.harvard.edu/blog/whats-the-relationship-between-diabetes-and-dementia-202107122546.
- ↑ "Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis". Age and Ageing 45 (6): 761–767. November 2016. doi:10.1093/ageing/afw140. PMID 27515679.
- ↑ 33.0 33.1 33.2 Williams textbook of endocrinology (12th ed.). Elsevier/Saunders. 2011. pp. 1371–1435. ISBN 978-1-4377-0324-5.
- ↑ "Over a Third of Adults With Type 1 Diabetes Weren't Diagnosed Until After 30". U.S. News & World Report. 28 September 2023. https://www.usnews.com/news/health-news/articles/2023-09-28/over-a-third-of-adults-with-type-1-diabetes-werent-diagnosed-until-after-30.
- ↑ "What is Type 1 Diabetes?". Medicine 30: 1–5. 2002. doi:10.1383/medc.30.1.1.28264.
- ↑ "Co-aggregation and heritability of organ-specific autoimmunity: a population-based twin study". European Journal of Endocrinology 182 (5): 473–480. May 2020. doi:10.1530/EJE-20-0049. PMID 32229696.
- ↑ "Genetic liability of type 1 diabetes and the onset age among 22,650 young Finnish twin pairs: a nationwide follow-up study". Diabetes 52 (4): 1052–1055. April 2003. doi:10.2337/diabetes.52.4.1052. PMID 12663480.
- ↑ "A study of diabetes mellitus within a large sample of Australian twins". Twin Research and Human Genetics 11 (1): 28–40. February 2008. doi:10.1375/twin.11.1.28. PMID 18251672. https://www.pure.ed.ac.uk/ws/files/11913813/study_of_diabetes_mellitus_within_a_large_sample_of_Australian_twins.pdf. Retrieved 2021-12-27.
- ↑ "The Concordance and Heritability of Type 2 Diabetes in 34,166 Twin Pairs From International Twin Registers: The Discordant Twin (DISCOTWIN) Consortium". Twin Research and Human Genetics 18 (6): 762–771. December 2015. doi:10.1017/thg.2015.83. PMID 26678054.
- ↑ "Global, regional, and national burden and trend of diabetes in 195 countries and territories: an analysis from 1990 to 2025". Scientific Reports 10 (1): 14790. September 2020. doi:10.1038/s41598-020-71908-9. PMID 32901098. Bibcode: 2020NatSR..1014790L.
- ↑ "An Update on the Epidemiology of Type 2 Diabetes: A Global Perspective". Endocrinology and Metabolism Clinics of North America 50 (3): 337–355. September 2021. doi:10.1016/j.ecl.2021.05.013. PMID 34399949.
- ↑ Classification of diabetes mellitus 2019 (Report). Geneva: World Health Organisation. 2019. ISBN 978-92-4-151570-2. https://apps.who.int/iris/rest/bitstreams/1233344/retrieve. Retrieved 2023-08-15.
- ↑ "The many faces of diabetes: a disease with increasing heterogeneity". Lancet 383 (9922): 1084–1094. March 2014. doi:10.1016/S0140-6736(13)62219-9. PMID 24315621.
- ↑ 44.0 44.1 Robbins & Cotran Pathologic Basis of Disease (10th ed.). Pennsylvania: Elsevier. 2021. pp. 1065–1132. ISBN 978-0-323-60992-0.
- ↑ "Diabetes treatment--bridging the divide". The New England Journal of Medicine 356 (15): 1499–1501. April 2007. doi:10.1056/NEJMp078030. PMID 17429082.
- ↑ "Diabetes Mellitus (DM)". Merck Publishing. September 2022. https://www.msdmanuals.com/professional/endocrine-and-metabolic-disorders/diabetes-mellitus-and-disorders-of-carbohydrate-metabolism/diabetes-mellitus-dm.
- ↑ 47.0 47.1 "Mechanisms of Beta Cell Dysfunction Associated With Viral Infection". Current Diabetes Reports 15 (10): 73. October 2015. doi:10.1007/s11892-015-0654-x. PMID 26280364. "So far, none of the hypotheses accounting for virus-induced beta cell autoimmunity has been supported by stringent evidence in humans, and the involvement of several mechanisms rather than just one is also plausible.".
- ↑ "Environmental Risk Factors and Type 1 Diabetes: Past, Present, and Future". Canadian Journal of Diabetes 40 (6): 586–593. December 2016. doi:10.1016/j.jcjd.2016.05.002. PMID 27545597.
- ↑ "Latent autoimmune diabetes in adults (LADA): What is it?" (in en). https://www.mayoclinic.org/diseases-conditions/type-1-diabetes/expert-answers/lada-diabetes/faq-20057880.
- ↑ "Latent autoimmune diabetes of the adult: current knowledge and uncertainty". Diabetic Medicine 32 (7): 843–852. July 2015. doi:10.1111/dme.12700. PMID 25601320.
- ↑ "What Is Diabetes?". https://www.diabetesdaily.com/learn-about-diabetes/basics/what-is-diabetes/.
- ↑ "Identification and phenotypic characterization of patients with LADA in a population of southeast Mexico". Scientific Reports 13 (1): 7029. April 2023. doi:10.1038/s41598-023-34171-2. PMID 37120620. Bibcode: 2023NatSR..13.7029N.
- ↑ "Insulin Resistance". StatPearls. Treasure Island (FL): StatPearls Publishing. 2024. http://www.ncbi.nlm.nih.gov/books/NBK507839/. Retrieved 2024-02-13.
- ↑ 54.0 54.1 54.2 Cite error: Invalid
<ref>tag; no text was provided for refs namedWHO2022 - ↑ "2. Classification and Diagnosis of Diabetes". Diabetes Care 40 (Suppl 1): S11–S24. January 2017. doi:10.2337/dc17-S005. PMID 27979889.
- ↑ "Prevention of Diabetes Mellitus in Patients With Prediabetes". The American Journal of Cardiology 123 (3): 507–512. February 2019. doi:10.1016/j.amjcard.2018.10.032. PMID 30528418.
- ↑ 57.0 57.1 "Dietary fats and prevention of type 2 diabetes". Progress in Lipid Research 48 (1): 44–51. January 2009. doi:10.1016/j.plipres.2008.10.002. PMID 19032965.
- ↑ "Risk factors for type 2 diabetes mellitus". The Journal of Cardiovascular Nursing 16 (2): 17–23. January 2002. doi:10.1097/00005082-200201000-00003. PMID 11800065. https://pubmed.ncbi.nlm.nih.gov/11800065. Retrieved 2023-10-12.
- ↑ "Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk". Circulation 121 (11): 1356–1364. March 2010. doi:10.1161/CIRCULATIONAHA.109.876185. PMID 20308626.
- ↑ "Sugar-sweetened beverages and risk of metabolic syndrome and type 2 diabetes: a meta-analysis". Diabetes Care 33 (11): 2477–2483. November 2010. doi:10.2337/dc10-1079. PMID 20693348.
- ↑ "Sugar-sweetened or artificially sweetened beverage consumption, physical activity and risk of type 2 diabetes in US adults". Diabetologia. January 2025. doi:10.1007/s00125-024-06351-w. PMID 39774686.
- ↑ "White rice consumption and risk of type 2 diabetes: meta-analysis and systematic review". BMJ 344: e1454. March 2012. doi:10.1136/bmj.e1454. PMID 22422870.
- ↑ "Adverse childhood experiences and risk of type 2 diabetes: A systematic review and meta-analysis". Metabolism 64 (11): 1408–1418. November 2015. doi:10.1016/j.metabol.2015.08.019. PMID 26404480.
- ↑ "The metabolic side effects of 12 antipsychotic drugs used for the treatment of schizophrenia on glucose: a network meta-analysis". BMC Psychiatry 17 (1): 373. November 2017. doi:10.1186/s12888-017-1539-0. PMID 29162032.
- ↑ 65.0 65.1 "National Diabetes Clearinghouse (NDIC): National Diabetes Statistics 2011". U.S. Department of Health and Human Services. http://diabetes.niddk.nih.gov/dm/pubs/statistics/#Gestational.
- ↑ 66.0 66.1 "Krause's Food & The Nutrition Care Process". Journal of Nutrition Education and Behavior 51 (10): 1225. November 2019. doi:10.1016/j.jneb.2019.06.022. ISSN 1499-4046.
- ↑ "Managing & Treating Gestational Diabetes | NIDDK". https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/gestational/management-treatment.
- ↑ "Intrapartal cardiotocographic patterns and hypoxia-related perinatal outcomes in pregnancies complicated by gestational diabetes mellitus". Acta Diabetologica 58 (11): 1563–1573. November 2021. doi:10.1007/s00592-021-01756-0. PMID 34151398.
- ↑ National Collaborating Centre for Women's and Children's Health (February 2015). "Intrapartum care". Diabetes in Pregnancy: Management of diabetes and its complications from preconception to the postnatal period. National Institute for Health and Care Excellence (UK). https://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0080685/. Retrieved 2018-08-21.
- ↑ "Progression to type 2 diabetes in women with a known history of gestational diabetes: systematic review and meta-analysis". BMJ 369: m1361. May 2020. doi:10.1136/bmj.m1361. PMID 32404325.
- ↑ "Monogenic Forms of Diabetes". US NIH. https://www.niddk.nih.gov/health-information/diabetes/overview/what-is-diabetes/monogenic-neonatal-mellitus-mody#3.
- ↑ "Maturity Onset Diabetes in the Young". StatPearls. Treasure Island (FL): StatPearls Publishing. 2025. https://www.ncbi.nlm.nih.gov/books/NBK532900/. Retrieved 2025-01-27.
- ↑ "Diagnosis and management of maturity onset diabetes of the young (MODY)". BMJ 343 (oct19 3): d6044. October 2011. doi:10.1136/bmj.d6044. PMID 22012810.
- ↑ Sarkar, Alisha Rahaman (April 18, 2025). "What is Type 5 diabetes? New form of disease recognised after decades of debate". The Independent. https://www.independent.co.uk/news/health/diabetes-type-5-signs-symptoms-treatment-malnutrition-b2735523.html.
- ↑ Tucker, Miriam E. (11 April 2025). "Malnutrition-Related Diabetes Officially Named 'Type 5'". Medscape Medical News. https://www.medscape.com/viewarticle/malnutrition-related-diabetes-officially-named-type-5-2025a10008pd?src=mbl_msp_android&ref=share.
- ↑ 76.0 76.1 "Definition, Diagnosis and Classification of Diabetes Mellitus and its Complications". World Health Organization. 1999. http://whqlibdoc.who.int/hq/1999/WHO_NCD_NCS_99.2.pdf.
- ↑ 77.0 77.1 Unless otherwise specified, reference is: Table 20-5 in Robbins Basic Pathology (8th ed.). Philadelphia: Saunders. 2007. ISBN 978-1-4160-2973-1.
- ↑ "Insulin resistance in type 1 diabetes: what is 'double diabetes' and what are the risks?". Diabetologia (National Library of Medicine) 56 (7): 1462–1470. July 2013. doi:10.1007/s00125-013-2904-2. PMID 23613085.
- ↑ "Statins and risk of incident diabetes: a collaborative meta-analysis of randomised statin trials". Lancet 375 (9716): 735–742. February 2010. doi:10.1016/S0140-6736(09)61965-6. PMID 20167359.
- ↑ "Insulin and insulin resistance". The Clinical Biochemist. Reviews 26 (2): 19–39. May 2005. PMID 16278749.
- ↑ "Insulin Basics". American Diabetes Association. https://diabetes.org/healthy-living/medication-treatments/insulin-other-injectables/insulin-basics.
- ↑ 82.0 82.1 82.2 82.3 Greenspan's basic & clinical endocrinology (9th ed.). McGraw-Hill Medical. 2011. ISBN 978-0-07-162243-1.
- ↑ Ganong's review of medical physiology (24th ed.). McGraw-Hill Medical. 2012. ISBN 978-0-07-178003-2.
- ↑ Harper's illustrated biochemistry (29th ed.). McGraw-Hill Medical. 2012. ISBN 978-0-07-176576-3.
- ↑ Juta's Complete Textbook of Medical Surgical Nursing. Cape Town: Juta. 2013. pp. 839.
- ↑ "Summary of revisions for the 2010 Clinical Practice Recommendations". Diabetes Care 33 (Suppl 1): S3. January 2010. doi:10.2337/dc10-S003. PMID 20042773. PMC 2797388. http://care.diabetesjournals.org/content/33/Supplement_1/S3.full. Retrieved 29 January 2010.
- ↑ "Postchallenge hyperglycemia and mortality in a national sample of U.S. adults". Diabetes Care 24 (8): 1397–1402. August 2001. doi:10.2337/diacare.24.8.1397. PMID 11473076.
- ↑ Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation. World Health Organization. 2006. p. 21. ISBN 978-92-4-159493-6. https://www.who.int/diabetes/publications/Definition%20and%20diagnosis%20of%20diabetes_new.pdf.
- ↑ "Diagnosis, prognosis, and treatment of impaired glucose tolerance and impaired fasting glucose". Evidence Report/Technology Assessment (Agency for Healthcare Research and Quality) (128): 1–11. August 2005. PMID 16194123. PMC 4780988. http://www.ahrq.gov/clinic/epcsums/impglusum.htm. Retrieved 20 July 2008.
- ↑ "The oral glucose tolerance test (OGTT) revisited". European Journal of Internal Medicine 22 (1): 8–12. February 2011. doi:10.1016/j.ejim.2010.07.008. PMID 21238885.
- ↑ "Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults". The New England Journal of Medicine 362 (9): 800–811. March 2010. doi:10.1056/NEJMoa0908359. PMID 20200384.
- ↑ "Understanding Pre-Type 1 Diabetes: The Key to Prevention". Frontiers in Endocrinology 9: 70. 2018-03-06. doi:10.3389/fendo.2018.00070. PMID 29559955.
- ↑ "Tackling risk factors for type 2 diabetes in adolescents: PRE-STARt study in Euskadi". Anales de Pediatria (Anales de Pediatría) 95 (3): 186–196. 2020. doi:10.1016/j.anpedi.2020.11.001. PMID 33388268.
- ↑ "Physical activity and risk of breast cancer, colon cancer, diabetes, ischemic heart disease, and ischemic stroke events: systematic review and dose-response meta-analysis for the Global Burden of Disease Study 2013". BMJ 354: i3857. August 2016. doi:10.1136/bmj.i3857. PMID 27510511.
- ↑ 95.0 95.1 "Simple Steps to Preventing Diabetes". Harvard T.H. Chan School of Public Health. 18 September 2012. http://www.hsph.harvard.edu/nutritionsource/preventing-diabetes-full-story/#references.
- ↑ "Active smoking and the risk of type 2 diabetes: a systematic review and meta-analysis". JAMA 298 (22): 2654–2664. December 2007. doi:10.1001/jama.298.22.2654. PMID 18073361.
- ↑ "Chronic diseases and their common risk factors". World Health Organization. 2005. https://www.who.int/chp/chronic_disease_report/media/Factsheet1.pdf.
- ↑ CDC (2023-07-31). "Diabetes and Your Immune System". https://www.cdc.gov/diabetes/library/features/diabetes_immune_system.html.
- ↑ "Diabetes in COVID-19: Prevalence, pathophysiology, prognosis and practical considerations". Diabetes & Metabolic Syndrome 14 (4): 303–310. 2020. doi:10.1016/j.dsx.2020.04.004. PMID 32298981.
- ↑ "Diabetes in COVID-19 pandemic-prevalence, patient characteristics and adverse outcomes". International Journal of Clinical Practice 75 (7): e14112. July 2021. doi:10.1111/ijcp.14112. PMID 33630378.
- ↑ "Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). UK Prospective Diabetes Study (UKPDS) Group". Lancet 352 (9131): 837–853. September 1998. doi:10.1016/S0140-6736(98)07019-6. PMID 9742976.
- ↑ 102.0 102.1 "Type 1 diabetes mellitus". Williams Textbook of Endocrinology. Elsevier. 2020. pp. 1403.
- ↑ 103.0 103.1 103.2 103.3 "Managing diabetes". National Institute of Diabetes and Digestive and Kidney Diseases, US National Institutes of Health. 1 December 2016. https://www.niddk.nih.gov/health-information/diabetes/overview/managing-diabetes.
- ↑ "Effectiveness of plant-based diets in promoting well-being in the management of type 2 diabetes: a systematic review". BMJ Open Diabetes Research & Care 6 (1): e000534. 2018-10-30. doi:10.1136/bmjdrc-2018-000534. PMID 30487971.
- ↑ "The effect of intensive diabetes therapy on the development and progression of neuropathy.". Annals of Internal Medicine 122 (8): 561–568. April 1995. doi:10.7326/0003-4819-122-8-199504150-00001. PMID 7887548.
- ↑ "The A1C test and diabetes". National Institute of Diabetes and Digestive and Kidney Diseases, US National Institutes of Health. 1 April 2018. https://www.niddk.nih.gov/health-information/diagnostic-tests/a1c-test.
- ↑ "Hemoglobin A1c Targets for Glycemic Control With Pharmacologic Therapy for Nonpregnant Adults With Type 2 Diabetes Mellitus: A Guidance Statement Update From the American College of Physicians". Annals of Internal Medicine 168 (8): 569–576. April 2018. doi:10.7326/M17-0939. PMID 29507945.
- ↑ National Institute for Health and Clinical Excellence. Clinical guideline 66: Type 2 diabetes. London, 2008.
- ↑ "Footwear and offloading interventions to prevent and heal foot ulcers and reduce plantar pressure in patients with diabetes: a systematic review". Diabetes/Metabolism Research and Reviews 32 (Suppl 1): 99–118. January 2016. doi:10.1002/dmrr.2702. PMID 26342178.
- ↑ "Effectiveness of offloading methods in preventing primary diabetic foot ulcers in adults with diabetes: a systematic review". JBI Database of Systematic Reviews and Implementation Reports 14 (7): 236–265. July 2016. doi:10.11124/JBISRIR-2016-003013. PMID 27532798.
- ↑ "Prevention of foot ulcers in the at-risk patient with diabetes: a systematic review". Diabetes/Metabolism Research and Reviews 36 (S1 Suppl 1): e3270. March 2020. doi:10.1002/dmrr.3270. PMID 31957213. https://eprints.qut.edu.au/220879/1/Van%2BNetten%2Bet%2Bal%2B-%2B2016%2B-%2BPrevention%2Bof%2Bfoot%2Bulcers%2Bsystematic%2Breview.pdf. Retrieved 2023-01-23.
- ↑ "Preventive foot care in diabetes". Diabetes Care 27 (suppl_1): S63–S64. January 2004. doi:10.2337/diacare.27.2007.S63. PMID 14693928.
- ↑ "Self management interventions for type 2 diabetes in adult people with severe mental illness". The Cochrane Database of Systematic Reviews 2016 (4): CD011361. April 2016. doi:10.1002/14651858.CD011361.pub2. PMID 27120555.
- ↑ "Long-term Sustainability of Diabetes Prevention Approaches: A Systematic Review and Meta-analysis of Randomized Clinical Trials". JAMA Internal Medicine 177 (12): 1808–1817. December 2017. doi:10.1001/jamainternmed.2017.6040. PMID 29114778.
- ↑ "Weight Management in Patients with Type 1 Diabetes and Obesity". Current Diabetes Reports 17 (10): 92. August 2017. doi:10.1007/s11892-017-0918-8. PMID 28836234.
- ↑ 116.0 116.1 American Diabetes Association (January 2019). "5. Lifestyle Management: Standards of Medical Care in Diabetes-2019". Diabetes Care 42 (Suppl 1): S46–S60. doi:10.2337/dc19-S005. PMID 30559231.
- ↑ 117.0 117.1 117.2 "Nutrition Therapy for Adults With Diabetes or Prediabetes: A Consensus Report". Diabetes Care 42 (5): 731–754. May 2019. doi:10.2337/dci19-0014. PMID 31000505.
- ↑ 118.0 118.1 "The effect of macronutrients on glycaemic control: a systematic review of dietary randomised controlled trials in overweight and obese adults with type 2 diabetes in which there was no difference in weight loss between treatment groups". The British Journal of Nutrition 114 (10): 1656–1666. November 2015. doi:10.1017/S0007114515003475. PMID 26411958.
- ↑ "Weight Loss and the Prevention and Treatment of Type 2 Diabetes Using Lifestyle Therapy, Pharmacotherapy, and Bariatric Surgery: Mechanisms of Action". Current Obesity Reports 4 (2): 287–302. June 2015. doi:10.1007/s13679-015-0155-x. PMID 26627223.
- ↑ 120.0 120.1 "Non-nutritive sweeteners for diabetes mellitus". The Cochrane Database of Systematic Reviews 2020 (5): CD012885. May 2020. doi:10.1002/14651858.CD012885.pub2. PMID 32449201.
- ↑ 121.00 121.01 121.02 121.03 121.04 121.05 121.06 121.07 121.08 121.09 "Pediatric type 2 diabetes". StatPearls, US National Library of Medicine. 12 November 2023. https://www.ncbi.nlm.nih.gov/books/NBK431046/.
- ↑ 122.0 122.1 "Global burden of type 2 diabetes in adolescents and young adults, 1990-2019: systematic analysis of the Global Burden of Disease Study 2019". BMJ - Clinical Research 379: e072385. December 2022. doi:10.1136/bmj-2022-072385. PMID 36740855.
- ↑ 123.0 123.1 123.2 123.3 123.4 "ISPAD Clinical Practice Consensus Guidelines 2022: Type 2 diabetes in children and adolescents". Pediatric Diabetes 23 (7): 872–902. November 2022. doi:10.1111/pedi.13409. PMID 36161685.
- ↑ "Diabetic retinopathy: current concepts and emerging therapy". Endocrinology and Metabolism Clinics of North America 42 (4): 721–745. December 2013. doi:10.1016/j.ecl.2013.08.001. PMID 24286948.
- ↑ "Glycemic Control as Primary Prevention for Diabetic Kidney Disease". Advances in Chronic Kidney Disease 25 (2): 141–148. March 2018. doi:10.1053/j.ackd.2017.11.003. PMID 29580578.
- ↑ "One size does not fit all glycemic targets for type 2 diabetes". Journal of Diabetes Investigation 5 (2): 134–141. March 2014. doi:10.1111/jdi.12206. PMID 24843750.
- ↑ 127.0 127.1 "Type 1 diabetes in adults: diagnosis and management". National Institute for Health and Care Excellence. 26 August 2015. https://www.nice.org.uk/guidance/ng17.
- ↑ 128.0 128.1 "Type 2 diabetes in adults: management". National Institute for Health and Care Excellence. 2 December 2015. https://www.nice.org.uk/guidance/ng28.
- ↑ 129.0 129.1 129.2 "Management of blood glucose in type 2 diabetes mellitus". American Family Physician 79 (1): 29–36. January 2009. PMID 19145963. http://www.aafp.org/afp/2009/0101/p29.pdf.
- ↑ 130.0 130.1 "Oral antidiabetic agents: current role in type 2 diabetes mellitus". Drugs 65 (3): 385–411. 2005. doi:10.2165/00003495-200565030-00005. PMID 15669880.
- ↑ Consumer Reports; American College of Physicians (April 2012), "Choosing a type 2 diabetes drug – Why the best first choice is often the oldest drug", High Value Care (Consumer Reports), http://consumerhealthchoices.org/wp-content/uploads/2012/04/High-Value-Care-Diabetes-ACP.pdf, retrieved August 14, 2012
- ↑ "A Roadmap on the Prevention of Cardiovascular Disease Among People Living With Diabetes". Global Heart 14 (3): 215–240. September 2019. doi:10.1016/j.gheart.2019.07.009. PMID 31451236.
- ↑ "Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses". BMJ 352: i717. February 2016. doi:10.1136/bmj.i717. PMID 26920333.
- ↑ "Benefits and harms of lower blood pressure treatment targets: systematic review and meta-analysis of randomised placebo-controlled trials". BMJ Open 9 (9): e026686. September 2019. doi:10.1136/bmjopen-2018-026686. PMID 31575567.
- ↑ 135.0 135.1 135.2 "Update on Prevention of Cardiovascular Disease in Adults With Type 2 Diabetes Mellitus in Light of Recent Evidence: A Scientific Statement From the American Heart Association and the American Diabetes Association". Diabetes Care 38 (9): 1777–1803. September 2015. doi:10.2337/dci15-0012. PMID 26246459.
- ↑ "Effect of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers on all-cause mortality, cardiovascular deaths, and cardiovascular events in patients with diabetes mellitus: a meta-analysis". JAMA Internal Medicine 174 (5): 773–785. May 2014. doi:10.1001/jamainternmed.2014.348. PMID 24687000.
- ↑ "Effects of aliskiren on mortality, cardiovascular outcomes and adverse events in patients with diabetes and cardiovascular disease or risk: A systematic review and meta-analysis of 13,395 patients". Diabetes & Vascular Disease Research 14 (5): 400–406. September 2017. doi:10.1177/1479164117715854. PMID 28844155.
- ↑ 138.0 138.1 "Cardiovascular and Renal Outcomes of Renin-Angiotensin System Blockade in Adult Patients with Diabetes Mellitus: A Systematic Review with Network Meta-Analyses". PLOS Medicine 13 (3): e1001971. March 2016. doi:10.1371/journal.pmed.1001971. PMID 26954482.
- ↑ "Aspirin for primary prevention of cardiovascular events in people with diabetes: a position statement of the American Diabetes Association, a scientific statement of the American Heart Association, and an expert consensus document of the American College of Cardiology Foundation". Diabetes Care 33 (6): 1395–1402. June 2010. doi:10.2337/dc10-0555. PMID 20508233.
- ↑ "The clinical effectiveness and cost-effectiveness of bariatric (weight loss) surgery for obesity: a systematic review and economic evaluation". Health Technology Assessment 13 (41): 1–190, 215–357, iii–iv. September 2009. doi:10.3310/hta13410. PMID 19726018.
- ↑ "Bariatric surgery for diabetes management". Current Opinion in Endocrinology, Diabetes, and Obesity 16 (2): 119–124. April 2009. doi:10.1097/MED.0b013e32832912e7. PMID 19276974.
- ↑ 142.0 142.1 ""Metabolic" surgery for treatment of type 2 diabetes mellitus". Endocrine Practice 15 (6): 624–631. September–October 2009. doi:10.4158/EP09170.RAR. PMID 19625245.
- ↑ "Bariatric surgery in patients with type 2 diabetes: a viable option". Postgraduate Medicine 123 (1): 24–33. January 2011. doi:10.3810/pgm.2011.01.2242. PMID 21293081.
- ↑ "Bariatric surgery for type 2 diabetes". Lancet 379 (9833): 2300–2311. June 2012. doi:10.1016/S0140-6736(12)60401-2. PMID 22683132.
- ↑ "Pancreas Transplantation". American Diabetes Association. http://www.diabetes.org/living-with-diabetes/treatment-and-care/transplantation/pancreas-transplantation.html.
- ↑ "Prevalence of peripheral neuropathy in patients with diabetes: A systematic review and meta-analysis". Primary Care Diabetes 14 (5): 435–444. October 2020. doi:10.1016/j.pcd.2019.12.005. PMID 31917119.
- ↑ 147.0 147.1 "Advances in Interventional Therapies for Painful Diabetic Neuropathy: A Systematic Review". Anesthesia and Analgesia 134 (6): 1215–1228. June 2022. doi:10.1213/ANE.0000000000005860. PMID 35051958.
- ↑ 148.0 148.1 "Surgical Decompression in the Treatment of Diabetic Peripheral Neuropathy: A Systematic Review and Meta-analysis". Journal of Reconstructive Microsurgery 33 (3): 151–157. March 2017. doi:10.1055/s-0036-1594300. PMID 27894152.
- ↑ "A cause for optimism in diabetic neuropathy". Annals of Plastic Surgery 20 (2): 103–105. February 1988. doi:10.1097/00000637-198802000-00001. PMID 3355053.
- ↑ 150.0 150.1 "Biologic Basis of Nerve Decompression Surgery for Focal Entrapments in Diabetic Peripheral Neuropathy". Journal of Diabetes Science and Technology 8 (2): 412–418. March 2014. doi:10.1177/1932296814525030. PMID 24876595.
- ↑ "Lower Extremity Nerve Decompression for Diabetic Peripheral Neuropathy: A Systematic Review and Meta-analysis". Plastic and Reconstructive Surgery. Global Open 10 (8): e4478. August 2022. doi:10.1097/GOX.0000000000004478. PMID 35999882.
- ↑ Can social prescribing improve the health of people with diabetes?. 2024. doi:10.3310/nihrevidence_61876. https://evidence.nihr.ac.uk/alert/can-social-prescribing-improve-the-health-of-people-with-diabetes/. Retrieved 26 January 2024.
- ↑ "Home telehealth for diabetes management: a systematic review and meta-analysis". Diabetes, Obesity & Metabolism 11 (10): 913–930. October 2009. doi:10.1111/j.1463-1326.2009.01057.x. PMID 19531058.
- ↑ 154.0 154.1 "Computer-based diabetes self-management interventions for adults with type 2 diabetes mellitus". The Cochrane Database of Systematic Reviews 2013 (3): CD008776. March 2013. doi:10.1002/14651858.CD008776.pub2. PMID 23543567.
- ↑ "Computer-assisted versus oral-and-written dietary history taking for diabetes mellitus". The Cochrane Database of Systematic Reviews 2011 (12): CD008488. December 2011. doi:10.1002/14651858.CD008488.pub2. PMID 22161430.
- ↑ "The global implications of diabetes and cancer". Lancet 383 (9933): 1947–1948. June 2014. doi:10.1016/S0140-6736(14)60886-2. PMID 24910221.
- ↑ 157.0 157.1 157.2 157.3 157.4 157.5 "Global Report on Diabetes". World Health Organization. 2016. http://apps.who.int/iris/bitstream/handle/10665/204871/9789241565257_eng.pdf.
- ↑ 158.0 158.1 158.2 158.3 Estimated number diabetics worldwide. 10 December 2019. https://www.statista.com/statistics/271442/number-of-diabetics-worldwide/. Retrieved 17 May 2020.
- ↑ "Diabetes and gender". Diabetologia 44 (1): 3–15. January 2001. doi:10.1007/s001250051573. PMID 11206408.
- ↑ "Sex differences in risk factors for incident type 2 diabetes mellitus: the MONICA Augsburg cohort study". Archives of Internal Medicine 162 (1): 82–89. January 2002. doi:10.1001/archinte.162.1.82. PMID 11784224.
- ↑ "The top 10 causes of death Fact sheet N°310". World Health Organization. October 2013. https://www.who.int/mediacentre/factsheets/fs310/en/.
- ↑ Public Health Agency of Canada, Diabetes in Canada: Facts and figures from a public health perspective. Ottawa, 2011.
- ↑ "Projections of global mortality and burden of disease from 2002 to 2030". PLOS Medicine 3 (11): e442. November 2006. doi:10.1371/journal.pmed.0030442. PMID 17132052.
- ↑ 164.0 164.1 "Global prevalence of diabetes: estimates for the year 2000 and projections for 2030". Diabetes Care 27 (5): 1047–1053. May 2004. doi:10.2337/diacare.27.5.1047. PMID 15111519.
- ↑ "Prevalence of Prediabetes Among Adults – Diabetes". 2018-03-13. https://www.cdc.gov/diabetes/data/statistics-report/prevalence-of-prediabetes.html.
- ↑ Exercise and disease management (2nd ed.). Boca Raton: CRC Press. 2011-04-25. p. 25. ISBN 978-1-4398-2759-8. https://books.google.com/books?id=eAn9-bm_pi8C&pg=PA25.
- ↑ 167.0 167.1 167.2 167.3 167.4 167.5 167.6 167.7 Principles of diabetes mellitus (2nd ed.). New York: Springer. 2009. p. 3. ISBN 978-0-387-09840-1. https://books.google.com/books?id=i0qojvF1SpUC&pg=PA3.
- ↑ 168.0 168.1 "Sickening sweet". Distillations 1 (4): 12–15. 2015. https://www.sciencehistory.org/distillations/magazine/sickening-sweet. Retrieved 20 March 2018.
- ↑ 169.0 169.1 "Aretaeus of Cappadocia and the first description of diabetes". Hormones 11 (1): 109–113. 2012. doi:10.1007/BF03401545. PMID 22450352. http://www.hormones.gr/pdf/HORMONES%202012,%20109-113.pdf.
- ↑ 170.0 170.1 Oxford English Dictionary. diabetes. Retrieved 2011-06-10.
- ↑ 171.0 171.1 "Online Etymology Dictionary. diabetes.". 2001–2010. http://www.etymonline.com/index.php?search=diabetes&searchmode=none.
- ↑ Aretaeus, De causis et signis acutorum morborum (lib. 2), Κεφ. β. περὶ Διαβήτεω (Chapter 2, On Diabetes, Greek original) , on Perseus
- ↑ 173.0 173.1 173.2 173.3 Oxford English Dictionary. mellite. Retrieved 2011-06-10.
- ↑ 174.0 174.1 174.2 174.3 "MyEtimology. mellitus.". http://www.myetymology.com/latin/mellitus.html.
- ↑ Oxford English Dictionary. -ite. Retrieved 2011-06-10.
- ↑ "Diabetes urine testing: an historical perspective". The Diabetes Educator 14 (6): 521–526. 1988. doi:10.1177/014572178801400615. PMID 3061764.
- ↑ The New Public Health, Second Edition. New York: Academic Press. 2008. p. 200. ISBN 978-0-12-370890-8.
- ↑ "Monitoring the targets of the St Vincent Declaration and the implementation of quality management in diabetes care: the DIABCARE initiative. The DIABCARE Monitoring Group of the St Vincent Declaration Steering Committee". Diabetic Medicine 10 (4): 371–377. May 1993. doi:10.1111/j.1464-5491.1993.tb00083.x. PMID 8508624.
- ↑ "Type 2 diabetes programmes in Europe". Euro Observer 7 (2): 5–6. 2005. http://www2.lse.ac.uk/LSEHealthAndSocialCare/pdf/euroObserver/Obsvol7no2.pdf.
- ↑ CDC (2022-11-03). "Diabetes Stigma: Learn About It, Recognize It, Reduce It". https://www.cdc.gov/diabetes/library/features/diabetes_stigma.html.
- ↑ "Social stigma in diabetes : a framework to understand a growing problem for an increasing epidemic". The Patient 6 (1): 1–10. 2013-03-01. doi:10.1007/s40271-012-0001-0. PMID 23322536.
- ↑ "Weight stigma and diabetes stigma in U.S. adults with type 2 diabetes: Associations with diabetes self-care behaviors and perceptions of health care". Diabetes Research and Clinical Practice 168: 108387. October 2020. doi:10.1016/j.diabres.2020.108387. PMID 32858100.
- ↑ "Race/ethnic difference in diabetes and diabetic complications". Current Diabetes Reports 13 (6): 814–823. December 2013. doi:10.1007/s11892-013-0421-9. PMID 24037313.
- ↑ CDC (2022-04-04). "Hispanic/Latino Americans and Type 2 Diabetes". https://www.cdc.gov/diabetes/library/features/hispanic-diabetes.html.
- ↑ CDC (2022-11-21). "Diabetes and Asian American People". https://www.cdc.gov/diabetes/library/spotlights/diabetes-asian-americans.html.
- ↑ "Lost productive time and costs due to diabetes and diabetic neuropathic pain in the US workforce". Journal of Occupational and Environmental Medicine 49 (6): 672–679. June 2007. doi:10.1097/JOM.0b013e318065b83a. PMID 17563611.
- ↑ Emergency Department Visits for Adults with Diabetes, 2010. Agency for Healthcare Research and Quality. November 2013. PMID 24455787. http://www.hcup-us.ahrq.gov/reports/statbriefs/sb167.jsp.
- ↑ "Type 1 vs. Type 2 Diabetes Differences: Which One Is Worse?". https://www.medicinenet.com/type_1_vs_type_2_diabetes_similarities_differences/article.htm.
- ↑ Living with diabetes. New York: Facts On File. 2008. p. 143. ISBN 978-1-4381-2108-6. https://archive.org/details/livingwithdiabet0000park.
- ↑ "Comparative occurrence of diabetes in canine, feline, and few wild animals and their association with pancreatic diseases and ketoacidosis with therapeutic approach". Veterinary World 11 (4): 410–422. April 2018. doi:10.14202/vetworld.2018.410-422. PMID 29805204.
- ↑ "Hyperglycemia in Reptiles". Reptile Medicine and Surgery (Second ed.). Saint Louis: W.B. Saunders. 2006-01-01. pp. 822–830. doi:10.1016/b0-72-169327-x/50062-6. ISBN 978-0-7216-9327-9.
- ↑ "Revisiting glucose regulation in birds - A negative model of diabetes complications". Comparative Biochemistry and Physiology. Part B, Biochemistry & Molecular Biology 262: 110778. 8 July 2022. doi:10.1016/j.cbpb.2022.110778. PMID 35817273.
- ↑ "An amphibian high fat diet model confirms that endocrine disruptors can induce a metabolic syndrome in wild green frogs (Pelophylax spp. complex)". Environmental Pollution 311: 120009. October 2022. doi:10.1016/j.envpol.2022.120009. PMID 35998770. Bibcode: 2022EPoll.31120009V.
- ↑ 194.0 194.1 "Diabetes mellitus". 2005. http://www.merckvetmanual.com/mvm/index.jsp?cfile=htm/bc/40302.htm.
- ↑ Feline diabetes mellitus Aspects on epidemiology and pathogenesis. Acta Universitatis agriculturae Sueciae. ISBN 978-91-7760-067-1. https://pub.epsilon.slu.se/14746/1/ohlund_m_171123.pdf. Retrieved 2017-12-18.
External links
- American Diabetes Association
- IDF Diabetes Atlas
- National Diabetes Education Program
- ADA's Standards of Medical Care in Diabetes 2019
- "The past 200 years in diabetes". The New England Journal of Medicine 367 (14): 1332–1340. October 2012. doi:10.1056/NEJMra1110560. PMID 23034021.
- "Diabetes". MedlinePlus. U.S. National Library of Medicine. https://medlineplus.gov/diabetes.html.
| Classification | |
|---|---|
| External resources |
Template:Disease of the pancreas and glucose metabolism
Lua error: Internal error: The interpreter exited with status 1.
 KSF
KSF