Ebola virus disease
Topic: Medicine
 From HandWiki - Reading time: 56 min
From HandWiki - Reading time: 56 min
| Ebola virus disease | |
|---|---|
| Other names | Ebola hemorrhagic fever (EHF), Ebola |
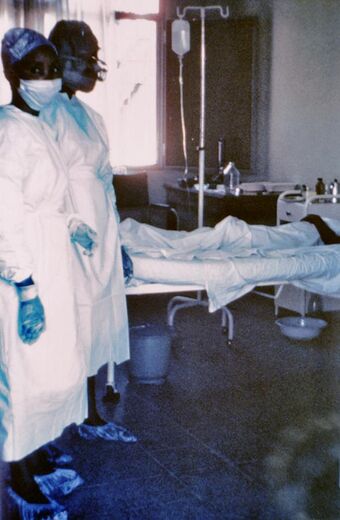 | |
| Two nurses standing near Mayinga N'Seka, a nurse with Ebola virus disease in the 1976 outbreak in Zaire. N'Seka died a few days later. | |
| Specialty | Infectious disease |
| Symptoms | Fever, sore throat, muscular pain, headaches, diarrhea, bleeding[1] |
| Complications | Low blood pressure from fluid loss[2] |
| Usual onset | Two days to three weeks post exposure[1] |
| Causes | Ebolaviruses spread by direct contact[1] |
| Diagnostic method | Finding the virus, viral RNA, or antibodies in blood[1] |
| Differential diagnosis | Malaria, cholera, typhoid fever, meningitis, other viral hemorrhagic fevers[1] |
| Prevention | Coordinated medical services, careful handling of bushmeat[1] |
| Treatment | Supportive care[1] |
| Prognosis | 25–90% mortality[1] |
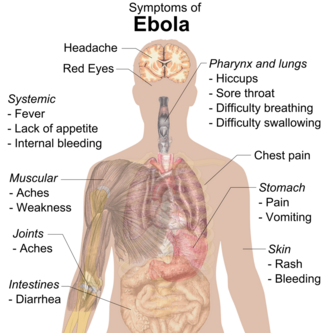
Ebola virus disease (EVD), also known as Ebola hemorrhagic fever (EHF) or simply Ebola, is a viral hemorrhagic fever of humans and other primates caused by ebolaviruses.[1] Signs and symptoms typically start between two days and three weeks after contracting the virus with a fever, sore throat, muscular pain, and headaches.[1] Vomiting, diarrhea and rash usually follow, along with decreased function of the liver and kidneys.[1] At this time, some people begin to bleed both internally and externally.[1] The disease has a high risk of death, killing 25% to 90% of those infected, with an average of about 50%.[1] This is often due to low blood pressure from fluid loss, and typically follows 6 to 16 days after symptoms appear.[2]
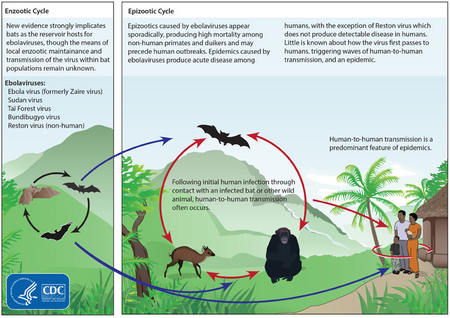
The virus spreads through direct contact with body fluids, such as blood from infected humans or other animals.[1] Spread may also occur from contact with items recently contaminated with bodily fluids.[1] Spread of the disease through the air between primates, including humans, has not been documented in either laboratory or natural conditions.[3] Semen or breast milk of a person after recovery from EVD may carry the virus for several weeks to months.[1][4][5] Fruit bats are believed to be the normal carrier in nature, able to spread the virus without being affected by it.[1] Other diseases such as malaria, cholera, typhoid fever, meningitis and other viral hemorrhagic fevers may resemble EVD.[1] Blood samples are tested for viral RNA, viral antibodies or for the virus itself to confirm the diagnosis.[1][6]
Control of outbreaks requires coordinated medical services and community engagement.[1] This includes rapid detection, contact tracing of those who have been exposed, quick access to laboratory services, care for those infected, and proper disposal of the dead through cremation or burial.[1][7] Samples of body fluids and tissues from people with the disease should be handled with special caution.[1] Prevention includes limiting the spread of disease from infected animals to humans by handling potentially infected bushmeat only while wearing protective clothing, and by thoroughly cooking bushmeat before eating it.[1] It also includes wearing proper protective clothing and washing hands when around a person with the disease.[1] An Ebola vaccine was approved in the United States in December 2019.[8] While there is no approved treatment for Ebola (As of 2019),[9] two treatments (REGN-EB3 and mAb114) are associated with improved outcomes.[10] Supportive efforts, also, improve outcomes.[1] This includes either oral rehydration therapy (drinking slightly sweetened and salty water) or giving intravenous fluids as well as treating symptoms.[1]
The disease was first identified in 1976, in two simultaneous outbreaks: one in Nzara (a town in South Sudan) and the other in Yambuku (Democratic Republic of the Congo), a village near the Ebola River from which the disease takes its name.[11] EVD outbreaks occur intermittently in tropical regions of sub-Saharan Africa.[1] Between 1976 and 2013, the World Health Organization reports 24 outbreaks involving 2,387 cases with 1,590 deaths.[1][12] The largest outbreak to date was the epidemic in West Africa, which occurred from December 2013, to January 2016, with {{#section:Ebola virus epidemic in West Africa|cases}} cases and {{#section:Ebola virus epidemic in West Africa|deaths}} deaths.{{#section:Ebola virus epidemic in West Africa|caserefs}}[13][14] It was declared no longer an emergency on 29 March 2016.[15] Other outbreaks in Africa began in the Democratic Republic of the Congo in May 2017,[16][17] and 2018.[18][19] In July 2019, the World Health Organization declared the Congo Ebola outbreak a world health emergency.[20]
Signs and symptoms
Onset
The length of time between exposure to the virus and the development of symptoms (incubation period) is between 2 and 21 days,[1][21] and usually between 4 and 10 days.[22] However, recent estimates based on mathematical models predict that around 5% of cases may take greater than 21 days to develop.[23]
Symptoms usually begin with a sudden influenza-like stage characterized by feeling tired, fever, weakness, decreased appetite, muscular pain, joint pain, headache, and sore throat.[1][22][24][25] The fever is usually higher than 38.3 °C (101 °F).[26] This is often followed by nausea, vomiting, diarrhea, abdominal pain, and sometimes hiccups.[25][27] The combination of severe vomiting and diarrhea often leads to severe dehydration.[28] Next, shortness of breath and chest pain may occur, along with swelling, headaches, and confusion.[25] In about half of the cases, the skin may develop a maculopapular rash, a flat red area covered with small bumps, five to seven days after symptoms begin.[22][26]
Bleeding
In some cases, internal and external bleeding may occur.[1] This typically begins five to seven days after the first symptoms.[29] All infected people show some decreased blood clotting.[26] Bleeding from mucous membranes or from sites of needle punctures has been reported in 40–50% of cases.[30] This may cause vomiting blood, coughing up of blood, or blood in stool.[31] Bleeding into the skin may create petechiae, purpura, ecchymoses or hematomas (especially around needle injection sites).[32] Bleeding into the whites of the eyes may also occur.[33] Heavy bleeding is uncommon; if it occurs, it is usually in the gastrointestinal tract.[34] The incidence of bleeding into the gastrointestinal tract has decreased since earlier epidemics and is now[when?] estimated to be approximately 10% with improved prevention of disseminated intravascular coagulation.[28]
Recovery and death
Recovery may begin between seven and 14 days after first symptoms.[25] Death, if it occurs, follows typically six to 16 days from first symptoms and is often due to low blood pressure from fluid loss.[2] In general, bleeding often indicates a worse outcome, and blood loss may result in death.[24] People are often in a coma near the end of life.[25]
Those who survive often have ongoing muscular and joint pain, liver inflammation, and decreased hearing, and may have continued tiredness, continued weakness, decreased appetite, and difficulty returning to pre-illness weight.[25][35] Problems with vision may develop.[36]
Survivors develop antibodies against Ebola that last at least 10 years, but it is unclear whether they are immune to additional infections.[37]
Cause
EVD in humans is caused by four of five viruses of the genus Ebolavirus. The four are Bundibugyo virus (BDBV), Sudan virus (SUDV), Taï Forest virus (TAFV) and one simply called Ebola virus (EBOV, formerly Zaire Ebola virus).[38] EBOV, species Zaire ebolavirus, is the most dangerous of the known EVD-causing viruses, and is responsible for the largest number of outbreaks.[39] The fifth virus, Reston virus (RESTV), is not thought to cause disease in humans, but has caused disease in other primates.[40][41] All five viruses are closely related to marburgviruses.[38]
Virology
Ebolaviruses contain single-stranded, non-infectious RNA genomes.[42] Ebolavirus genomes contain seven genes including 3'-UTR-NP-VP35-VP40-GP-VP30-VP24-L-5'-UTR.[32][43] The genomes of the five different ebolaviruses (BDBV, EBOV, RESTV, SUDV and TAFV) differ in sequence and the number and location of gene overlaps. As with all filoviruses, ebolavirus virions are filamentous particles that may appear in the shape of a shepherd's crook, of a "U" or of a "6," and they may be coiled, toroid or branched.[43][44] In general, ebolavirions are 80 nanometers (nm) in width and may be as long as 14,000 nm.[45]
Their life cycle is thought to begin with a virion attaching to specific cell-surface receptors such as C-type lectins, DC-SIGN, or integrins, which is followed by fusion of the viral envelope with cellular membranes.[46] The virions taken up by the cell then travel to acidic endosomes and lysosomes where the viral envelope glycoprotein GP is cleaved.[46] This processing appears to allow the virus to bind to cellular proteins enabling it to fuse with internal cellular membranes and release the viral nucleocapsid.[46] The Ebolavirus structural glycoprotein (known as GP1,2) is responsible for the virus' ability to bind to and infect targeted cells.[47] The viral RNA polymerase, encoded by the L gene, partially uncoats the nucleocapsid and transcribes the genes into positive-strand mRNAs, which are then translated into structural and nonstructural proteins. The most abundant protein produced is the nucleoprotein, whose concentration in the host cell determines when L switches from gene transcription to genome replication. Replication of the viral genome results in full-length, positive-strand antigenomes that are, in turn, transcribed into genome copies of negative-strand virus progeny.[48] Newly synthesized structural proteins and genomes self-assemble and accumulate near the inside of the cell membrane. Virions bud off from the cell, gaining their envelopes from the cellular membrane from which they bud. The mature progeny particles then infect other cells to repeat the cycle. The genetics of the Ebola virus are difficult to study because of EBOV's virulent characteristics.[49]
Transmission
It is believed that between people, Ebola disease spreads only by direct contact with the blood or other body fluids of a person who has developed symptoms of the disease.[50][51][52] Body fluids that may contain Ebola viruses include saliva, mucus, vomit, feces, sweat, tears, breast milk, urine and semen.[4][37] The WHO states that only people who are very sick are able to spread Ebola disease in saliva, and whole virus has not been reported to be transmitted through sweat. Most people spread the virus through blood, feces and vomit.[53] Entry points for the virus include the nose, mouth, eyes, open wounds, cuts and abrasions.[37] Ebola may be spread through large droplets; however, this is believed to occur only when a person is very sick.[54] This contamination can happen if a person is splashed with droplets.[54] Contact with surfaces or objects contaminated by the virus, particularly needles and syringes, may also transmit the infection.[55][56] The virus is able to survive on objects for a few hours in a dried state, and can survive for a few days within body fluids outside of a person.[37][57]
The Ebola virus may be able to persist for more than 3 months in the semen after recovery, which could lead to infections via sexual intercourse.[4][58][59] Virus persistence in semen for over a year has been recorded in a national screening programme.[60] Ebola may also occur in the breast milk of women after recovery, and it is not known when it is safe to breastfeed again.[5] The virus was also found in the eye of one patient in 2014, two months after it was cleared from his blood.[61] Otherwise, people who have recovered are not infectious.[55]
The potential for widespread infections in countries with medical systems capable of observing correct medical isolation procedures is considered low.[62] Usually when someone has symptoms of the disease, they are unable to travel without assistance.[63]
Dead bodies remain infectious; thus, people handling human remains in practices such as traditional burial rituals or more modern processes such as embalming are at risk.[62] 69% of the cases of Ebola infections in Guinea during the 2014 outbreak are believed to have been contracted via unprotected (or unsuitably protected) contact with infected corpses during certain Guinean burial rituals.[64][65]
Health-care workers treating people with Ebola are at greatest risk of infection.[55] The risk increases when they do not have appropriate protective clothing such as masks, gowns, gloves and eye protection; do not wear it properly; or handle contaminated clothing incorrectly.[55] This risk is particularly common in parts of Africa where the disease mostly occurs and health systems function poorly.[66] There has been transmission in hospitals in some African countries that reuse hypodermic needles.[67][68] Some health-care centers caring for people with the disease do not have running water.[69] In the United States the spread to two medical workers treating infected patients prompted criticism of inadequate training and procedures.[70]
Human-to-human transmission of EBOV through the air has not been reported to occur during EVD outbreaks,[3] and airborne transmission has only been demonstrated in very strict laboratory conditions, and then only from pigs to primates, but not from primates to primates.[50][56] Spread of EBOV by water, or food other than bushmeat, has not been observed.[55][56] No spread by mosquitos or other insects has been reported.[55] Other possible methods of transmission are being studied.[57]
Airborne transmission among humans is theoretically possible due to the presence of Ebola virus particles in saliva, which can be discharged into the air with a cough or sneeze, but observational data from previous epidemics suggests the actual risk of airborne transmission is low.[71] A number of studies examining airborne transmission broadly concluded that transmission from pigs to primates could happen without direct contact because, unlike humans and primates, pigs with EVD get very high ebolavirus concentrations in their lungs, and not their bloodstream.[72] Therefore, pigs with EVD can spread the disease through droplets in the air or on the ground when they sneeze or cough.[73] By contrast, humans and other primates accumulate the virus throughout their body and specifically in their blood, but not very much in their lungs.[73] It is believed that this is the reason researchers have observed pig to primate transmission without physical contact, but no evidence has been found of primates being infected without actual contact, even in experiments where infected and uninfected primates shared the same air.[72][73]
Initial case
Although it is not entirely clear how Ebola initially spreads from animals to humans, the spread is believed to involve direct contact with an infected wild animal or fruit bat.[55] Besides bats, other wild animals sometimes infected with EBOV include several monkey species, chimpanzees, gorillas, baboons, and duikers.[77]
Animals may become infected when they eat fruit partially eaten by bats carrying the virus.[78] Fruit production, animal behavior and other factors may trigger outbreaks among animal populations.[78]
Evidence indicates that both domestic dogs and pigs can also be infected with EBOV.[79] Dogs do not appear to develop symptoms when they carry the virus, and pigs appear to be able to transmit the virus to at least some primates.[79] Although some dogs in an area in which a human outbreak occurred had antibodies to EBOV, it is unclear whether they played a role in spreading the disease to people.[79]
Reservoir
The natural reservoir for Ebola has yet to be confirmed; however, bats are considered to be the most likely candidate species.[56] Three types of fruit bats (Hypsignathus monstrosus, Epomops franqueti and Myonycteris torquata) were found to possibly carry the virus without getting sick.[80] (As of 2013), whether other animals are involved in its spread is not known.[79] Plants, arthropods, rodents, and birds have also been considered possible viral reservoirs.[1][28]
Bats were known to roost in the cotton factory in which the first cases of the 1976 and 1979 outbreaks were observed, and they have also been implicated in Marburg virus infections in 1975 and 1980.[81] Of 24 plant and 19 vertebrate species experimentally inoculated with EBOV, only bats became infected.[82] The bats displayed no clinical signs of disease, which is considered evidence that these bats are a reservoir species of EBOV. In a 2002–2003 survey of 1,030 animals including 679 bats from Gabon and the Republic of the Congo, 13 fruit bats were found to contain EBOV RNA.[83] Antibodies against Zaire and Reston viruses have been found in fruit bats in Bangladesh, suggesting that these bats are also potential hosts of the virus and that the filoviruses are present in Asia.[84]
Between 1976 and 1998, in 30,000 mammals, birds, reptiles, amphibians and arthropods sampled from regions of EBOV outbreaks, no Ebola virus was detected apart from some genetic traces found in six rodents (belonging to the species Mus setulosus and Praomys) and one shrew (Sylvisorex ollula) collected from the Central African Republic.[81][85] However, further research efforts have not confirmed rodents as a reservoir.[86] Traces of EBOV were detected in the carcasses of gorillas and chimpanzees during outbreaks in 2001 and 2003, which later became the source of human infections. However, the high rates of death in these species resulting from EBOV infection make it unlikely that these species represent a natural reservoir for the virus.[81]
Deforestation has been mentioned as a possible contributor to recent outbreaks, including the West African Ebola virus epidemic. Index cases of EVD have often been close to recently deforested lands.[87][88]
Pathophysiology
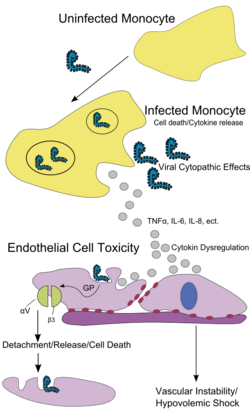
Like other filoviruses, EBOV replicates very efficiently in many cells, producing large amounts of virus in monocytes, macrophages, dendritic cells and other cells including liver cells, fibroblasts, and adrenal gland cells.[89] Viral replication triggers high levels of inflammatory chemical signals and leads to a septic state.[35]
EBOV is thought to infect humans through contact with mucous membranes or skin breaks.[50] After infection, endothelial cells (cells lining the inside of blood vessels), liver cells, and several types of immune cells such as macrophages, monocytes, and dendritic cells are the main targets of attack.[50] Following infection, immune cells carry the virus to nearby lymph nodes where further reproduction of the virus takes place.[50] From there the virus can enter the bloodstream and lymphatic system and spread throughout the body.[50] Macrophages are the first cells infected with the virus, and this infection results in programmed cell death.[45] Other types of white blood cells, such as lymphocytes, also undergo programmed cell death leading to an abnormally low concentration of lymphocytes in the blood.[50] This contributes to the weakened immune response seen in those infected with EBOV.[50]
Endothelial cells may be infected within three days after exposure to the virus.[45] The breakdown of endothelial cells leading to blood vessel injury can be attributed to EBOV glycoproteins. This damage occurs due to the synthesis of Ebola virus glycoprotein (GP), which reduces the availability of specific integrins responsible for cell adhesion to the intercellular structure and causes liver damage, leading to improper clotting. The widespread bleeding that occurs in affected people causes swelling and shock due to loss of blood volume.[90] The dysfunctional bleeding and clotting commonly seen in EVD has been attributed to increased activation of the extrinsic pathway of the coagulation cascade due to excessive tissue factor production by macrophages and monocytes.[22]
After infection, a secreted glycoprotein, small soluble glycoprotein (sGP or GP) is synthesized. EBOV replication overwhelms protein synthesis of infected cells and the host immune defenses. The GP forms a trimeric complex, which tethers the virus to the endothelial cells. The sGP forms a dimeric protein that interferes with the signaling of neutrophils, another type of white blood cell. This enables the virus to evade the immune system by inhibiting early steps of neutrophil activation.
Immune system evasion
Filoviral infection also interferes with proper functioning of the innate immune system.[46][48] EBOV proteins blunt the human immune system's response to viral infections by interfering with the cells' ability to produce and respond to interferon proteins such as interferon-alpha, interferon-beta, and interferon gamma.[47][91]
The VP24 and VP35 structural proteins of EBOV play a key role in this interference. When a cell is infected with EBOV, receptors located in the cell's cytosol (such as RIG-I and MDA5) or outside of the cytosol (such as Toll-like receptor 3 (TLR3), TLR7, TLR8 and TLR9) recognize infectious molecules associated with the virus.[47] On TLR activation, proteins including interferon regulatory factor 3 and interferon regulatory factor 7 trigger a signaling cascade that leads to the expression of type 1 interferons.[47] The type 1 interferons are then released and bind to the IFNAR1 and IFNAR2 receptors expressed on the surface of a neighboring cell.[47] Once interferon has bound to its receptors on the neighboring cell, the signaling proteins STAT1 and STAT2 are activated and move to the cell's nucleus.[47] This triggers the expression of interferon-stimulated genes, which code for proteins with antiviral properties.[47] EBOV's V24 protein blocks the production of these antiviral proteins by preventing the STAT1 signaling protein in the neighboring cell from entering the nucleus.[47] The VP35 protein directly inhibits the production of interferon-beta.[91] By inhibiting these immune responses, EBOV may quickly spread throughout the body.[45]
Diagnosis
When EVD is suspected, travel, work history, and exposure to wildlife are important factors with respect to further diagnostic efforts.
Laboratory testing
Possible non-specific laboratory indicators of EVD include a low platelet count; an initially decreased white blood cell count followed by an increased white blood cell count; elevated levels of the liver enzymes alanine aminotransferase (ALT) and aspartate aminotransferase (AST); and abnormalities in blood clotting often consistent with disseminated intravascular coagulation (DIC) such as a prolonged prothrombin time, partial thromboplastin time, and bleeding time.[92] Filovirions such as EBOV may be identified by their unique filamentous shapes in cell cultures examined with electron microscopy.[93]
The specific diagnosis of EVD is confirmed by isolating the virus, detecting its RNA or proteins, or detecting antibodies against the virus in a person's blood.[94] Isolating the virus by cell culture, detecting the viral RNA by polymerase chain reaction (PCR)[6][22] and detecting proteins by enzyme-linked immunosorbent assay (ELISA) are methods best used in the early stages of the disease and also for detecting the virus in human remains.[6][94] Detecting antibodies against the virus is most reliable in the later stages of the disease and in those who recover.[94] IgM antibodies are detectable two days after symptom onset and IgG antibodies can be detected six to 18 days after symptom onset.[22] During an outbreak, isolation of the virus with cell culture methods is often not feasible. In field or mobile hospitals, the most common and sensitive diagnostic methods are real-time PCR and ELISA.[95] In 2014, with new mobile testing facilities deployed in parts of Liberia, test results were obtained 3–5 hours after sample submission.[96] In 2015, a rapid antigen test which gives results in 15 minutes was approved for use by WHO.[97] It is able to confirm Ebola in 92% of those affected and rule it out in 85% of those not affected.[97]
Differential diagnosis
Early symptoms of EVD may be similar to those of other diseases common in Africa, including malaria and dengue fever.[24] The symptoms are also similar to those of other viral hemorrhagic fevers such as Marburg virus disease, Crimean Congo hemorrhagic fever, and Lassa fever.[98][99]
The complete differential diagnosis is extensive and requires consideration of many other infectious diseases such as typhoid fever, shigellosis, rickettsial diseases, cholera, sepsis, borreliosis, EHEC enteritis, leptospirosis, scrub typhus, plague, Q fever, candidiasis, histoplasmosis, trypanosomiasis, visceral leishmaniasis, measles, and viral hepatitis among others.[100]
Non-infectious diseases that may result in symptoms similar to those of EVD include acute promyelocytic leukemia, hemolytic uremic syndrome, snake envenomation, clotting factor deficiencies/platelet disorders, thrombotic thrombocytopenic purpura, hereditary hemorrhagic telangiectasia, Kawasaki disease, and warfarin poisoning.[95][101][102][103]
Prevention
Vaccines
An Ebola vaccine, rVSV-ZEBOV, was approved in the United States in December 2019.[8] It appears to be fully effective after ten days of being given.[8] It was studied in Guinea between 2014, and 2016.[8] More than 100,000 people have been vaccinated against Ebola (As of 2019).[104]
Infection control
People who care for those infected with Ebola should wear protective clothing including masks, gloves, gowns and goggles.[105] The U.S. Centers for Disease Control (CDC) recommend that the protective gear leaves no skin exposed.[106] These measures are also recommended for those who may handle objects contaminated by an infected person's body fluids.[107] In 2014, the CDC began recommending that medical personnel receive training on the proper suit-up and removal of personal protective equipment (PPE); in addition, a designated person, appropriately trained in biosafety, should be watching each step of these procedures to ensure they are done correctly.[106] In Sierra Leone, the typical training period for the use of such safety equipment lasts approximately 12 days.[108]
The infected person should be in barrier-isolation from other people.[105] All equipment, medical waste, patient waste and surfaces that may have come into contact with body fluids need to be disinfected.[107] During the 2014 outbreak, kits were put together to help families treat Ebola disease in their homes, which included protective clothing as well as chlorine powder and other cleaning supplies.[109] Education of caregivers in these techniques, and providing such barrier-separation supplies has been a priority of Doctors Without Borders.[110]
Ebolaviruses can be eliminated with heat (heating for 30 to 60 minutes at 60 °C or boiling for 5 minutes). To disinfect surfaces, some lipid solvents such as some alcohol-based products, detergents, sodium hypochlorite (bleach) or calcium hypochlorite (bleaching powder), and other suitable disinfectants may be used at appropriate concentrations.[77][111]
Education of the general public about the risk factors for Ebola infection and of the protective measures individuals may take to prevent infection is recommended by the World Health Organization.[1] These measures include avoiding direct contact with infected people and regular hand washing using soap and water.[112]
Bushmeat, an important source of protein in the diet of some Africans, should be handled and prepared with appropriate protective clothing and thoroughly cooked before consumption.[1] Some research suggests that an outbreak of Ebola disease in the wild animals used for consumption may result in a corresponding human outbreak. Since 2003, such animal outbreaks have been monitored to predict and prevent Ebola outbreaks in humans.[113]
If a person with Ebola disease dies, direct contact with the body should be avoided.[105] Certain burial rituals, which may have included making various direct contacts with a dead body, require reformulation so that they consistently maintain a proper protective barrier between the dead body and the living.[114][115][116] Social anthropologists may help find alternatives to traditional rules for burials.[117]
Transportation crews are instructed to follow a certain isolation procedure, should anyone exhibit symptoms resembling EVD.[118] (As of August 2014), the WHO does not consider travel bans to be useful in decreasing spread of the disease.[63] In October 2014, the CDC defined four risk levels used to determine the level of 21-day monitoring for symptoms and restrictions on public activities.[119] In the United States, the CDC recommends that restrictions on public activity, including travel restrictions, are not required for the following defined risk levels:[119]
- having been in a country with widespread Ebola disease transmission and having no known exposure (low risk); or having been in that country more than 21 days ago (no risk)
- encounter with a person showing symptoms; but not within three feet of the person with Ebola without wearing PPE; and no direct contact with body fluids
- having had brief skin contact with a person showing symptoms of Ebola disease when the person was believed to be not very contagious (low risk)
- in countries without widespread Ebola disease transmission: direct contact with a person showing symptoms of the disease while wearing PPE (low risk)
- contact with a person with Ebola disease before the person was showing symptoms (no risk).
The CDC recommends monitoring for the symptoms of Ebola disease for those both at "low risk" and at higher risk.[119]
In laboratories where diagnostic testing is carried out, biosafety level 4-equivalent containment is required.[120] Laboratory researchers must be properly trained in BSL-4 practices and wear proper PPE.[120]
Putting on protective equipment
Isolation
Isolation refers to separating those who are sick from those who are not. Quarantine refers to separating those who may have been exposed to a disease until they either show signs of the disease or are no longer at risk.[121] Quarantine, also known as enforced isolation, is usually effective in decreasing spread.[122][123] Governments often quarantine areas where the disease is occurring or individuals who may transmit the disease outside of an initial area.[124] In the United States, the law allows quarantine of those infected with ebolaviruses.[125][126]
Contact tracing
Contact tracing is considered important to contain an outbreak. It involves finding everyone who had close contact with infected individuals and monitoring them for signs of illness for 21 days. If any of these contacts comes down with the disease, they should be isolated, tested and treated. Then the process is repeated, tracing the contacts' contacts.[127][128]
Management
While there is no approved[by whom?] treatment for Ebola (As of 2019),[9] two treatments (REGN-EB3 and mAb114) are associated with improved outcomes.[10] The U.S. Food and Drug Administration (FDA) advises people to be careful of advertisements making unverified or fraudulent claims of benefits supposedly gained from various anti-Ebola products.[129][130]
Standard support
Treatment is primarily supportive in nature.[131] Early supportive care with rehydration and symptomatic treatment improves survival.[1] Rehydration may be via the oral or intravenous route.[131] These measures may include pain management, and treatment for nausea, fever, and anxiety.[131] The World Health Organization (WHO) recommends avoiding aspirin or ibuprofen for pain management, due to the risk of bleeding associated with these medications.[132]
Blood products such as packed red blood cells, platelets, or fresh frozen plasma may also be used.[131] Other regulators of coagulation have also been tried including heparin in an effort to prevent disseminated intravascular coagulation and clotting factors to decrease bleeding.[131] Antimalarial medications and antibiotics are often used before the diagnosis is confirmed,[131] though there is no evidence to suggest such treatment helps. Several experimental treatments are being studied.[citation needed]
Where hospital care is not possible, the WHO's guidelines for home care have been relatively successful. Recommendations include using towels soaked in a bleach solution when moving infected people or bodies and also applying bleach on stains. It is also recommended that the caregivers wash hands with bleach solutions and cover their mouth and nose with a cloth.[133]
Intensive care
Intensive care is often used in the developed world.[32] This may include maintaining blood volume and electrolytes (salts) balance as well as treating any bacterial infections that may develop.[32] Dialysis may be needed for kidney failure, and extracorporeal membrane oxygenation may be used for lung dysfunction.[32]
Prognosis
EVD has a risk of death in those infected, between 25% and 90%.[1][134] (As of September 2014), the average risk of death among those infected is 50%.[1] The highest risk of death was 90% in the 2002–2003 Republic of the Congo outbreak.[135]
Death, if it occurs, follows typically six to sixteen days after symptoms appear and is often due to low blood pressure from fluid loss.[2] Early supportive care to prevent dehydration may reduce the risk of death.
If an infected person survives, recovery may be quick and complete. Prolonged cases are often complicated by the occurrence of long-term problems, such as inflammation of the testicles, joint pains, fatigue, hearing loss, mood and sleep disturbances, muscular pain, abdominal pain, menstrual abnormalities, miscarriages, skin peeling, or hair loss.[22][136] Inflammation and swelling of the uveal layer of the eye is the most common eye complication in survivors of Ebola virus disease.[136] Eye symptoms, such as light sensitivity, excess tearing, and vision loss have been described.[137]
Ebola can stay in some body parts like the eyes,[138] breasts, and testicles after infection.[4][139] Sexual transmission after recovery has been suspected.[140][141] If sexual transmission occurs following recovery it is believed to be a rare event.[142] One case of a condition similar to meningitis has been reported many months after recovery, (As of October 2015).[143]
A study of 44 survivors of the Ebola virus in Sierra Leone reported musculoskeletal pain in 70%, headache in 48%, and eye problems in 14%.[144]
Epidemiology
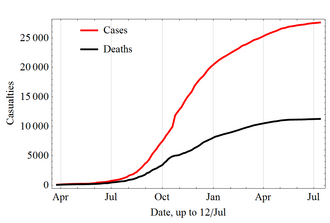
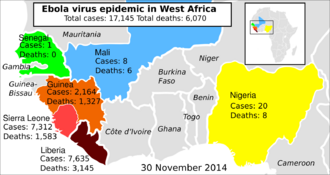
The disease typically occurs in outbreaks in tropical regions of Sub-Saharan Africa.[1] From 1976 (when it was first identified) through 2013, the WHO reported 2,387 confirmed cases with 1,590 overall fatalities.[1][12] The largest outbreak to date was the Ebola virus epidemic in West Africa, which caused a large number of deaths in Guinea, Sierra Leone, and Liberia.[13][14]
1976
Sudan
The first known outbreak of EVD was identified only after the fact. It occurred between June and November 1976, in Nzara, South Sudan[38][145] (then part of Sudan), and was caused by Sudan virus (SUDV). The Sudan outbreak infected 284 people and killed 151. The first identifiable case in Sudan occurred on 27 June in a storekeeper in a cotton factory in Nzara, who was hospitalized on 30 June and died on 6 July.[32][146] Although the WHO medical staff involved in the Sudan outbreak knew that they were dealing with a heretofore unknown disease, the actual "positive identification" process and the naming of the virus did not occur until some months later in Zaire.[146]
Zaire
On 26 August 1976, a second outbreak of EVD began in Yambuku, a small rural village in Mongala District in northern Zaire (now known as the Democratic Republic of the Congo).[147][148] This outbreak was caused by EBOV, formerly designated Zaire ebolavirus, a different member of the genus Ebolavirus than in the first Sudan outbreak. The first person infected with the disease was the village school's headmaster Mabalo Lokela, who began displaying symptoms on 26 August 1976.[149] Lokela had returned from a trip to Northern Zaire near the border of the Central African Republic, after visiting the Ebola River between 12 and 22 August. He was originally believed to have malaria and given quinine. However, his symptoms continued to worsen, and he was admitted to Yambuku Mission Hospital on 5 September. Lokela died on 8 September, 14 days after he began displaying symptoms.[150][151]
Soon after Lokela's death, others who had been in contact with him also died, and people in Yambuku began to panic. The country's Minister of Health and Zaire President Mobutu Sese Seko declared the entire region, including Yambuku and the country's capital, Kinshasa, a quarantine zone. No-one was permitted to enter or leave the area, and roads, waterways, and airfields were placed under martial law. Schools, businesses and social organizations were closed.[152] The initial response was led by Congolese doctors, including Jean-Jacques Muyembe-Tamfum, one of the discoverers of Ebola. Muyembe took a blood sample from a Belgian nun; this sample would eventually be used by Peter Piot to identify the previously unknown Ebola virus.[153] Muyembe was also the first scientist to come into direct contact with the disease and survive.[154] Researchers from the Centers for Disease Control and Prevention (CDC), including Piot, co-discoverer of Ebola, later arrived to assess the effects of the outbreak, observing that "the whole region was in panic."[155][156][157]
Piot concluded that Belgian nuns had inadvertently started the epidemic by giving unnecessary vitamin injections to pregnant women without sterilizing the syringes and needles. The outbreak lasted 26 days and the quarantine lasted two weeks. Researchers speculated that the disease disappeared due to the precautions taken by locals, the quarantine of the area, and discontinuing the injections.[152]
During this outbreak, Ngoy Mushola recorded the first clinical description of EVD in Yambuku, where he wrote the following in his daily log: "The illness is characterized with a high temperature of about 39 °C (102 °F), hematemesis, diarrhea with blood, retrosternal abdominal pain, prostration with 'heavy' articulations, and rapid evolution death after a mean of three days."[158]
The virus responsible for the initial outbreak, first thought to be Marburg virus, was later identified as a new type of virus related to marburgviruses. Virus strain samples isolated from both outbreaks were named "Ebola virus" after the Ebola River, near the first-identified viral outbreak site in Zaire.[32] Reports conflict about who initially coined the name: either Karl Johnson of the American CDC team[159] or Belgian researchers.[160] Subsequently, a number of other cases were reported, almost all centered on the Yambuku mission hospital or close contacts of another case.[149] In all, 318 cases and 280 deaths (an 88% fatality rate) occurred in Zaire.[161] Although the two outbreaks were at first believed connected, scientists later realized that they were caused by two distinct ebolaviruses, SUDV and EBOV.[148] The Zaire outbreak was contained with the help of the World Health Organization and transport from the Congolese air force, by quarantining villagers, sterilizing medical equipment, and providing protective clothing.[citation needed]
1995–2014
The second major outbreak occurred in Zaire (now the Democratic Republic of the Congo, DRC), in 1995, affecting 315 and killing 254.[1]
In 2000, Uganda had an outbreak infecting 425 and killing 224; in this case, the Sudan virus was found to be the Ebola species responsible for the outbreak.[1]
In 2003, an outbreak in the DRC infected 143 and killed 128, a 90% death rate, the highest of a genus Ebolavirus outbreak to date.[162]
In 2004, a Russian scientist died from Ebola after sticking herself with an infected needle.[163]
Between April and August 2007, a fever epidemic[164] in a four-village region[165] of the DRC was confirmed in September to have been cases of Ebola.[166] Many people who attended the recent funeral of a local village chief died.[165] The 2007 outbreak eventually infected 264 individuals and killed 187.[1]
On 30 November 2007, the Uganda Ministry of Health confirmed an outbreak of Ebola in the Bundibugyo District in Western Uganda. After confirming samples tested by the United States National Reference Laboratories and the Centers for Disease Control, the World Health Organization (WHO) confirmed the presence of a new species of genus Ebolavirus, which was tentatively named Bundibugyo.[167] The WHO reported 149 cases of this new strain and 37 of those led to deaths.[1]
The WHO confirmed two small outbreaks in Uganda in 2012, both caused by the Sudan variant. The first outbreak affected 7 people, killing 4, and the second affected 24, killing 17.[1]
On 17 August 2012, the Ministry of Health of the DRC reported an outbreak of the Ebola-Bundibugyo variant[168] in the eastern region.[169][170] Other than its discovery in 2007, this was the only time that this variant has been identified as responsible for an outbreak. The WHO revealed that the virus had sickened 57 people and killed 29. The probable cause of the outbreak was tainted bush meat hunted by local villagers around the towns of Isiro and Viadana.[1][171]
In 2014, an outbreak occurred in the DRC. Genome-sequencing showed that this outbreak was not related to the 2014–15 West Africa Ebola virus outbreak, but was the same EBOV species, the Zaire species.[172] It began in August 2014, and was declared over in November with 66 cases and 49 deaths.[173] This was the 7th outbreak in the DRC, three of which occurred during the period when the country was known as Zaire.[174]
2013–2016 West Africa
In March 2014, the World Health Organization (WHO) reported a major Ebola outbreak in Guinea, a West African nation.[175] Researchers traced the outbreak to a one-year-old child who died December 2013.[176][177] The disease rapidly spread to the neighboring countries of Liberia and Sierra Leone. It was the largest Ebola outbreak ever documented, and the first recorded in the region.[175] On 8 August 2014, the WHO declared the epidemic an international public health emergency. Urging the world to offer aid to the affected regions, its Director-General said, "Countries affected to date simply do not have the capacity to manage an outbreak of this size and complexity on their own. I urge the international community to provide this support on the most urgent basis possible."[178] By mid-August 2014, Doctors Without Borders reported the situation in Liberia's capital, Monrovia, was "catastrophic" and "deteriorating daily". They reported that fears of Ebola among staff members and patients had shut down much of the city's health system, leaving many people without medical treatment for other conditions.[179] In a 26 September statement, WHO said, "The Ebola epidemic ravaging parts of West Africa is the most severe acute public health emergency seen in modern times. Never before in recorded history has a biosafety level four pathogen infected so many people so quickly, over such a broad geographical area, for so long."[180]
Intense contact tracing and strict isolation largely prevented further spread of the disease in the countries that had imported cases. {{#section:Ebola virus epidemic in West Africa|casesasof}}, {{#section:Ebola virus epidemic in West Africa|cases}} suspected cases and {{#section:Ebola virus epidemic in West Africa|deaths}} deaths were reported;{{#section:Ebola virus epidemic in West Africa|caserefs}}[181] however, the WHO said that these numbers may be underestimated.[182] Because they work closely with the body fluids of infected patients, healthcare workers were especially vulnerable to infection ; in August 2014, the WHO reported that 10% of the dead were healthcare workers.[183]
In September 2014, it was estimated that the countries' capacity for treating Ebola patients was insufficient by the equivalent of 2,122 beds; by December there were a sufficient number of beds to treat and isolate all reported Ebola cases, although the uneven distribution of cases was causing serious shortfalls in some areas.[184] On 28 January 2015, the WHO reported that for the first time since the week ending 29 June 2014, there had been fewer than 100 new confirmed cases reported in a week in the three most-affected countries. The response to the epidemic then moved to a second phase, as the focus shifted from slowing transmission to ending the epidemic.[185] On 8 April 2015, the WHO reported only 30 confirmed cases, the lowest weekly total since the third week of May 2014.[186]
On 29 December 2015, 42 days after the last person tested negative for a second time, Guinea was declared free of Ebola transmission.[187] At that time, a 90-day period of heightened surveillance was announced by that agency. "This is the first time that all three countries – Guinea, Liberia and Sierra Leone – have stopped the original chains of transmission ...", the organization stated in a news release.[188] A new case was detected in Sierra Leone on 14 January 2016.[189] However, the outbreak was declared no longer an emergency on 29 March 2016.[15]
2014 spread outside West Africa
On 19 September, Eric Duncan flew from his native Liberia to Texas; 5 days later he began showing symptoms and visited a hospital but was sent home. His condition worsened and he returned to the hospital on 28 September, where he died on 8 October. Health officials confirmed a diagnosis of Ebola on 30 September – the first case in the United States.[190]
In early October, Teresa Romero, a 44-year-old Spanish nurse, contracted Ebola after caring for a priest who had been repatriated from West Africa. This was the first transmission of the virus to occur outside Africa.[191] Romero tested negative for the disease on 20 October, suggesting that she may have recovered from Ebola infection.[192]
On 12 October, the Centers for Disease Control and Prevention (CDC) confirmed that a nurse in Texas, Nina Pham, who had treated Duncan tested positive for the Ebola virus, the first known case of transmission in the United States.[193] On 15 October, a second Texas health-care worker who had treated Duncan was confirmed to have the virus.[70][194] Both of these people recovered.[195] An unrelated case involved a doctor in New York City, who returned to the United States from Guinea after working with Doctors Without Borders and tested positive for Ebola on 23 October.[196] The person recovered and was discharged from Bellevue Hospital Center on 11 November.[195] On 24 December 2014, a laboratory in Atlanta, Georgia reported that a technician had been exposed to Ebola.[197]
On 29 December 2014, Pauline Cafferkey, a British nurse who had just returned to Glasgow from Sierra Leone, was diagnosed with Ebola at Glasgow's Gartnavel General Hospital.[198] After initial treatment in Glasgow, she was transferred by air to RAF Northolt, then to the specialist high-level isolation unit at the Royal Free Hospital in London for longer-term treatment.[199]
2017 Democratic Republic of the Congo
On 11 May 2017, the DRC Ministry of Public Health notified the WHO about an outbreak of Ebola. Four people died, and four people survived; five of these eight cases were laboratory-confirmed. A total of 583 contacts were monitored. On 2 July 2017, the WHO declared the end of the outbreak.[citation needed]
2018 Équateur province
On 14 May 2018, the World Health Organization reported that "the Democratic Republic of Congo reported 39 suspected, probable or confirmed cases of Ebola between 4 April and 13 May, including 19 deaths."[200] Some 393 people identified as contacts of Ebola patients were being followed up. The outbreak centered on the Bikoro, Iboko, and Wangata areas in Equateur province,[200] including in the large city of Mbandaka. The DRC Ministry of Public Health approved the use of an experimental vaccine.[201][202][203] On 13 May 2018, WHO Director-General Tedros Adhanom Ghebreyesus visited Bikoro.[204] Reports emerged that maps of the area were inaccurate, not so much hampering medical providers as epidemiologists and officials trying to assess the outbreak and containment efforts.[205] The 2018 outbreak in the DRC was declared over on 24 July 2018.[19]
2018–20 Kivu
On 1 August 2018, the world’s 10th Ebola outbreak was declared in North Kivu province of the Democratic Republic of the Congo. It was the first Ebola outbreak in a military conflict zone, with thousands of refugees in the area.[206][207] By November 2018, nearly 200 Congolese had died of Ebola, about half of them from the city of Beni, where armed groups are fighting over the region's mineral wealth, impeding medical relief efforts.[208]
By March 2019, this became the second largest Ebola outbreak ever recorded, with more than 1,000 cases and insecurity continuing to being the major resistance to providing an adequate response.[209][210] (As of June 2019), the WHO reported 2025 confirmed and probable cases with 1357 deaths.[211] In June 2019, two people died of Ebola in neighbouring Uganda.[212]
In July 2019, an infected man travelled to Goma, home to more than 2 million people.[213] One week later, on 17 July 2019, the WHO declared the Ebola outbreak a global health emergency, the fifth time such a declaration has been made by the organization.[214] A government spokesman said that half of the Ebola cases are unidentified, and he added that the current outbreak could last up to three years.[215]
Society and culture
Weaponization
Ebolavirus is classified as a biosafety level 4 agent, as well as a Category A bioterrorism agent by the Centers for Disease Control and Prevention.[89][216] It has the potential to be weaponized for use in biological warfare,[217][218] and was investigated by Biopreparat for such use, but might be difficult to prepare as a weapon of mass destruction because the virus becomes ineffective quickly in open air.[219] Fake emails pretending to be Ebola information from the WHO or the Mexican Government have, in 2014, been misused to spread computer malware.[220] The BBC reported in 2015, that, "North Korean state media has suggested the disease was created by the U.S. military as a biological weapon."[221]
Literature
Richard Preston's 1995 best-selling book, The Hot Zone, dramatized the Ebola outbreak in Reston, Virginia.[222][223][224]
William Close's 1995 Ebola: A Documentary Novel of Its First Explosion[225][226] and 2002 Ebola: Through the Eyes of the People focused on individuals' reactions to the 1976 Ebola outbreak in Zaire.[227][228]
Tom Clancy's 1996 novel, Executive Orders, involves a Middle Eastern terrorist attack on the United States using an airborne form of a deadly Ebola virus strain named "Ebola Mayinga" (see Mayinga N'Seka).[229][230]
As the Ebola virus epidemic in West Africa developed in 2014, a number of popular self-published and well-reviewed books containing sensational and misleading information about the disease appeared in electronic and printed formats. The authors of some such books admitted that they lacked medical credentials and were not technically qualified to give medical advice. The World Health Organization and the United Nations stated that such misinformation had contributed to the spread of the disease.[231]
Other animals
Wild animals
Ebola has a high mortality rate among primates.[232] Frequent outbreaks of Ebola may have resulted in the deaths of 5,000 gorillas.[233] Outbreaks of Ebola may have been responsible for an 88% decline in tracking indices of observed chimpanzee populations in the 420 km2 Lossi Sanctuary between 2002 and 2003.[234] Transmission among chimpanzees through meat consumption constitutes a significant risk factor, whereas contact between the animals, such as touching dead bodies and grooming, is not.[235]
Recovered gorilla carcasses have contained multiple Ebola virus strains, suggesting multiple introductions of the virus. Bodies decompose quickly and carcasses are not infectious after 3 to 4 days. Contact between gorilla groups is rare, suggesting that transmission among gorilla groups is unlikely, and that outbreaks result from transmission between viral reservoirs and animal populations.[234]
Domestic animals
In 2012, it was demonstrated that the virus can travel without contact from pigs to nonhuman primates, although the same study failed to achieve transmission in that manner between primates.[79][236]
Dogs may become infected with EBOV but not develop symptoms. Dogs in some parts of Africa scavenge for food, and they sometimes eat EBOV-infected animals and also the corpses of humans. A 2005 survey of dogs during an EBOV outbreak found that although they remain asymptomatic, about 32 percent of dogs closest to an outbreak showed a seroprevalence for EBOV versus 9 percent of those farther away.[237] The authors concluded that there were "potential implications for preventing and controlling human outbreaks."
Reston virus
In late 1989, Hazelton Research Products' Reston Quarantine Unit in Reston, Virginia, suffered an outbreak of fatal illness amongst certain lab monkeys. This lab outbreak was initially diagnosed as simian hemorrhagic fever virus (SHFV) and occurred amongst a shipment of crab-eating macaque monkeys imported from the Philippines. Hazelton's veterinary pathologist sent tissue samples from dead animals to the United States Army Medical Research Institute of Infectious Diseases (USAMRIID) at Fort Detrick, Maryland, where an ELISA test indicated the antibodies present in the tissue were a response to Ebola virus and not SHFV.[238] An electron microscopist from USAMRIID discovered filoviruses similar in appearance to Ebola in the tissue samples sent from Hazelton Research Products' Reston Quarantine Unit.[239]
A US Army team headquartered at USAMRIID euthanized the surviving monkeys, and brought all the monkeys to Ft. Detrick for study by the Army's veterinary pathologists and virologists, and eventual disposal under safe conditions.[238] Blood samples were taken from 178 animal handlers during the incident.[240] Of those, six animal handlers eventually seroconverted, including one who had cut himself with a bloody scalpel.[90][241] Despite its status as a Level‑4 organism and its apparent pathogenicity in monkeys, when the handlers did not become ill, the CDC concluded that the virus had a very low pathogenicity to humans.[241][242]
The Philippines and the United States had no previous cases of Ebola infection, and upon further isolation, researchers concluded it was another strain of Ebola, or a new filovirus of Asian origin, which they named Reston ebolavirus (RESTV) after the location of the incident.[238] Reston virus (RESTV) can be transmitted to pigs.[79] Since the initial outbreak it has since been found in nonhuman primates in Pennsylvania, Texas, and Italy,[243] where the virus had infected pigs.[244] According to the WHO, routine cleaning and disinfection of pig (or monkey) farms with sodium hypochlorite or detergents should be effective in inactivating the Reston ebolavirus. Pigs that have been infected with RESTV tend to show symptoms of the disease.
Research
Treatments
(As of July 2015), no medication has been proven safe and effective for treating Ebola. By the time the Ebola virus epidemic in West Africa began in 2013, there were at least nine different candidate treatments. Several trials were conducted in late 2014, and early 2015, but some were abandoned due to lack of efficacy or lack of people to study.[245]
(As of August 2019), two experimental treatments known as REGN-EB3 and mAb114 were found to be 90% effective.[246][247][248]
Diagnostic tests
The diagnostic tests currently available require specialized equipment and highly trained personnel. Since there are few suitable testing centers in West Africa, this leads to delay in diagnosis.[249]
On 29 November 2014, a new 15-minute Ebola test was reported that if successful, "not only gives patients a better chance of survival, but it prevents transmission of the virus to other people." The new equipment, about the size of a laptop and solar-powered, allows testing to be done in remote areas.[250]
On 29 December 2014, the U.S. Food and Drug Administration (FDA) approved the LightMix Ebola Zaire rRT-PCR test for patients with symptoms of Ebola.[251]
Disease models
Animal models and in particular non-human primates are being used to study different aspects of Ebola virus disease. Developments in organ-on-a-chip technology have led to a chip-based model for Ebola hemorrhagic syndrome.[252]
References
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 1.13 1.14 1.15 1.16 1.17 1.18 1.19 1.20 1.21 1.22 1.23 1.24 1.25 1.26 1.27 1.28 1.29 1.30 1.31 1.32 1.33 1.34 1.35 1.36 1.37 1.38 1.39 1.40 1.41 1.42 1.43 1.44 "Ebola virus disease" (Press release). World Health Organization (WHO). 12 February 2018.
- ↑ 2.0 2.1 2.2 2.3 Singh, Sunit K.; Ruzek, Daniel, eds (2014). Viral hemorrhagic fevers. Boca Raton: CRC Press, Taylor & Francis Group. p. 444. ISBN 9781439884294. https://books.google.com/books?id=l5MtJdDhie0C&pg=PA444.
- ↑ 3.0 3.1 "2014 Ebola Virus Disease (EVD) outbreak in West Africa". World Health Organization (WHO). 21 April 2014. Archived from the original on 29 July 2014. https://web.archive.org/web/20140729034008/http://www.who.int/ith/updates/20140421/en/. Retrieved 3 August 2014.
- ↑ 4.0 4.1 4.2 4.3 "Preliminary study finds that Ebola virus fragments can persist in the semen of some survivors for at least nine months". Centers for Disease Control and Prevention (CDC). 14 October 2015. Archived from the original on 24 August 2017. https://web.archive.org/web/20170824104650/https://www.cdc.gov/media/releases/2015/p1014-ebola-virus.html.
- ↑ 5.0 5.1 "Recommendations for Breastfeeding/Infant Feeding in the Context of Ebola". Centers for Disease Control and Prevention (CDC). 19 September 2014. Archived from the original on 24 October 2014. https://web.archive.org/web/20141024235607/http://www.cdc.gov/vhf/ebola/hcp/recommendations-breastfeeding-infant-feeding-ebola.html. Retrieved 26 October 2014.
- ↑ 6.0 6.1 6.2 "Diagnosis of Ebola Virus Disease: Past, Present, and Future". Clinical Microbiology Reviews (American Society for Microbiology) 29 (4): 773–793. 13 July 2016. doi:10.1128/cmr.00003-16. ISSN 0893-8512. OCLC 38839512. PMID 27413095.
- ↑ "Guidance for Safe Handling of Human Remains of Ebola Patients in U. S. Hospitals and Mortuaries". Centers for Disease Control and Prevention (CDC). Archived from the original on 9 October 2014. https://web.archive.org/web/20141009172209/http://www.cdc.gov/vhf/ebola/hcp/guidance-safe-handling-human-remains-ebola-patients-us-hospitals-mortuaries.html. Retrieved 10 October 2014.
- ↑ 8.0 8.1 8.2 8.3 "First FDA-approved vaccine for the prevention of Ebola virus disease, marking a critical milestone in public health preparedness and response". U.S. Food and Drug Administration (FDA) (Press release). 20 December 2019. Retrieved 22 December 2019.
- ↑ 9.0 9.1 "Ebola Treatment Research". https://www.niaid.nih.gov/diseases-conditions/ebola-treatment. Retrieved 20 August 2019.
- ↑ 10.0 10.1 "Independent Monitoring Board Recommends Early Termination of Ebola Therapeutics Trial in DRC Because of Favorable Results with Two of Four Candidates". https://www.niaid.nih.gov/news-events/independent-monitoring-board-recommends-early-termination-ebola-therapeutics-trial-drc. Retrieved 20 August 2019.
- ↑ "Ebola virus disease, Fact sheet N°103, Updated September 2014". World Health Organization (WHO). September 2014. Archived from the original on 14 December 2014. https://web.archive.org/web/20141214011751/http://www.who.int/mediacentre/factsheets/fs103/en/. Retrieved 15 December 2014.
- ↑ 12.0 12.1 "Ebola Viral Disease Outbreak – West Africa, 2014". Centers for Disease Control and Prevention (CDC). 27 June 2014. Archived from the original on 30 June 2014. https://web.archive.org/web/20140630115747/http://www.cdc.gov/mmwr/preview/mmwrhtml/mm6325a4.htm?s_cid=mm6325a4_w. Retrieved 26 June 2014.
- ↑ 13.0 13.1 "CDC urges all US residents to avoid nonessential travel to Liberia, Guinea and Sierra Leone because of an unprecedented outbreak of Ebola". Centers for Disease Control and Prevention (CDC). 31 July 2014. Archived from the original on 9 August 2014. https://web.archive.org/web/20140809181737/http://wwwnc.cdc.gov/travel/notices/warning/ebola-liberia. Retrieved 2 August 2014.
- ↑ 14.0 14.1 "2014 Ebola Outbreak in West Africa". Centers for Disease Control and Prevention (CDC). 4 August 2014. Archived from the original on 2 October 2014. https://web.archive.org/web/20141002134254/http://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/. Retrieved 5 August 2014.
- ↑ 15.0 15.1 "Statement on the 9th meeting of the IHR Emergency Committee regarding the Ebola outbreak in West Africa". World Health Organization (WHO). 29 March 2016. Archived from the original on 31 March 2016. https://web.archive.org/web/20160331231040/http://www.who.int/mediacentre/news/statements/2016/end-of-ebola-pheic/en/. Retrieved 30 March 2016.
- ↑ "Statement on Ebola in the Democratic Republic of the Congo". World Health Organization (WHO). Archived from the original on 12 May 2017. https://web.archive.org/web/20170512203522/http://www.who.int/mediacentre/news/statements/2017/ebola-drc/en/. Retrieved 12 May 2017.
- ↑ Hodal, Kate (12 May 2017). "Ebola outbreak declared in Democratic Republic of the Congo after three die". The Guardian (United Kingdom: Guardian Media Group). ISSN 1756-3224. OCLC 60623878. Archived from the original on 12 May 2017. https://web.archive.org/web/20170512161809/https://www.theguardian.com/world/2017/may/12/ebola-outbreak-declared-democratic-republic-of-congo-after-three-die. Retrieved 12 May 2017.
- ↑ Scutti, Susan; Goldschmidt, Debra. "Ebola outbreak declared in Democratic Republic of Congo". CNN. https://www.cnn.com/2018/05/08/health/ebola-outbreak-who-bn/index.html. Retrieved 9 May 2018.
- ↑ 19.0 19.1 "Ebola outbreak in DRC ends: WHO calls for international efforts to stop other deadly outbreaks in the country". World Health Organization (WHO). http://www.who.int/news-room/detail/24-07-2018-ebola-outbreak-in-drc-ends-who-calls-for-international-efforts-to-stop-other-deadly-outbreaks-in-the-country. Retrieved 26 July 2018.
- ↑ Grady, Denise (17 July 2019). "Congo's Ebola Outbreak Is Declared a Global Health Emergency". The New York Times. ISSN 1553-8095. OCLC 1645522. https://www.nytimes.com/2019/07/17/health/ebola-congo-who-emergency.html. Retrieved 17 July 2019.
- ↑ 21.0 21.1 "Ebola Hemorrhagic Fever Signs and Symptoms". Centers for Disease Control and Prevention (CDC). 28 January 2014. Archived from the original on 1 August 2014. https://web.archive.org/web/20140801015854/http://www.cdc.gov/vhf/ebola/symptoms/index.html. Retrieved 2 August 2014.
- ↑ 22.0 22.1 22.2 22.3 22.4 22.5 22.6 "Ebola virus disease: a review on epidemiology, symptoms, treatment and pathogenesis". Neth J Med 72 (9): 442–48. November 2014. PMID 25387613. Archived from the original on 29 November 2014. https://web.archive.org/web/20141129144852/http://www.njmonline.nl/getpdf.php?t=a&id=10001148.
- ↑ "On the Quarantine Period for Ebola Virus". PLOS Currents Outbreaks 6. 14 October 2014. doi:10.1371/currents.outbreaks.2ab4b76ba7263ff0f084766e43abbd89. PMID 25642371.
- ↑ 24.0 24.1 24.2 "The 2014 Ebola virus disease outbreak in West Africa". J Gen Virol 95 (Pt 8): 1619–24. August 2014. doi:10.1099/vir.0.067199-0. PMID 24795448.
- ↑ 25.0 25.1 25.2 25.3 25.4 25.5 Magill, Alan (2013). Hunter's tropical medicine and emerging infectious diseases (9th ed.). New York: Saunders. p. 332. ISBN 9781416043904. https://books.google.com/books?id=UgvdM8WRld4C&pg=PA332.
- ↑ 26.0 26.1 26.2 "Ebola virus: unravelling pathogenesis to combat a deadly disease". Trends in Molecular Medicine 12 (5): 206–15. May 2006. doi:10.1016/j.molmed.2006.03.006. PMID 16616875.
- ↑ "Ebola Virus Disease: An Update on Epidemiology, Symptoms, Laboratory Findings, Diagnostic Issues, and Infection Prevention and Control Issues for Laboratory Professionals". Clinical Laboratory Medicine 37 (2): 269–84. June 2017. doi:10.1016/j.cll.2017.01.003. PMID 28457350.
- ↑ 28.0 28.1 28.2 "Gastrointestinal and Hepatic Manifestations of Ebola Virus Infection". Digestive Diseases and Sciences 60 (9): 2590–603. September 2015. doi:10.1007/s10620-015-3691-z. PMID 25972150.
- ↑ "Marburg and Ebola virus infections: a guide for their diagnosis, management, and control". WHO Offset Publication No. 36: 10f. 1977. Archived from the original on 21 October 2014. https://web.archive.org/web/20141021090422/http://whqlibdoc.who.int/offset/WHO_OFFSET_36.pdf.
- ↑ "Ebola Virus, Clinical Presentation". Medscape. Archived from the original on 1 January 2012. https://web.archive.org/web/20120101205843/http://emedicine.medscape.com/article/216288-clinical#showall. Retrieved 30 July 2012.
- ↑ "Appendix A: Disease-Specific Chapters — Chapter: Hemorrhagic fevers caused by: i) Ebola virus and ii) Marburg virus and iii) Other viral causes including bunyaviruses, arenaviruses, and flaviviruses". Ministry of Health and Long-Term Care. Archived from the original on 15 October 2014. https://web.archive.org/web/20141015081924/http://www.health.gov.on.ca/en/pro/programs/publichealth/oph_standards/docs/hemorrhagic_fevers_chapter.pdf. Retrieved 9 October 2014.
- ↑ 32.0 32.1 32.2 32.3 32.4 32.5 32.6 "Ebola haemorrhagic fever". Lancet 377 (9768): 849–62. March 2011. doi:10.1016/S0140-6736(10)60667-8. PMID 21084112.
- ↑ "Ebola virus disease and the eye". Current Opinion in Ophthalmology 27 (6): 538–44. November 2016. doi:10.1097/ICU.0000000000000313. PMID 27585217.
- ↑ "Clinical presentation and management of severe Ebola virus disease". Annals of the American Thoracic Society 11 (9): 1341–50. November 2014. doi:10.1513/AnnalsATS.201410-481PS. PMID 25369317.
- ↑ 35.0 35.1 "What Clinicians Should Know About the 2014 Ebola Outbreak". Mayo Clin Proc 89 (12): 1710–17. December 2014. doi:10.1016/j.mayocp.2014.10.010. PMID 25467644.
- ↑ "An emergency within an emergency: caring for Ebola survivors". World Health Organization (WHO). 7 August 2015. Archived from the original on 13 August 2015. https://web.archive.org/web/20150813163313/http://www.afro.who.int/en/sierra-leone/press-materials/item/7908-an-emergency-within-an-emergency-caring-for-ebola-survivors.html. Retrieved 12 August 2015.
- ↑ 37.0 37.1 37.2 37.3 "Q&A on Transmission, Ebola". Centers for Disease Control and Prevention (CDC). September 2014. Archived from the original on 2 October 2014. https://web.archive.org/web/20141002210702/http://www.cdc.gov/vhf/ebola/transmission/qas.html. Retrieved 3 October 2014.
- ↑ 38.0 38.1 38.2 "Current Ebola vaccines". Expert Opin Biol Ther 12 (7): 859–72. July 2012. doi:10.1517/14712598.2012.685152. PMID 22559078.
- ↑ "Proposal for a revised taxonomy of the family Filoviridae: Classification, names of taxa and viruses, and virus abbreviations". Archives of Virology 155 (12): 2083–103. December 2010. doi:10.1007/s00705-010-0814-x. PMID 21046175.
- ↑ Spickler, Anna. "Ebolavirus and Marburgvirus Infections". Archived from the original on 30 April 2015. https://web.archive.org/web/20150430165458/http://www.cfsph.iastate.edu/Factsheets/pdfs/viral_hemorrhagic_fever_filovirus.pdf.
- ↑ "About Ebola Virus Disease". Centers for Disease Control and Prevention (CDC). Archived from the original on 16 October 2014. https://web.archive.org/web/20141016080233/http://www.cdc.gov/vhf/ebola/about.html. Retrieved 18 October 2014.
- ↑ Pringle, C. R. (2005). "Order Mononegavirales". in Fauquet, C. M.; Mayo, M. A.; Maniloff, J. et al.. Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, U.S.: Elsevier/Academic Press. pp. 609–14. ISBN 978-0-12-370200-5.
- ↑ 43.0 43.1 "Membrane binding and bending in Ebola VP40 assembly and egress". Front Microbiol 5: 300. June 2014. doi:10.3389/fmicb.2014.00300. PMID 24995005.
- ↑ "Ebolavirus and Marburgvirus: insight the Filoviridae family". Mol Aspects Med 29 (3): 151–85. June 2008. doi:10.1016/j.mam.2007.09.005. PMID 18063023. https://air.unimi.it/retrieve/handle/2434/53604/1077822/Ebola_2008%29_Proofs.pdf.
- ↑ 45.0 45.1 45.2 45.3 "Outbreaks of Ebola virus disease in Africa: the beginnings of a tragic saga". J Venom Anim Toxins Incl Trop Dis 20 (1): 44. October 2014. doi:10.1186/1678-9199-20-44. PMID 25320574.
- ↑ 46.0 46.1 46.2 46.3 "Camouflage and Misdirection: The Full-On Assault of Ebola Virus Disease". Cell 159 (3): 477–86. October 2014. doi:10.1016/j.cell.2014.10.006. PMID 25417101.
- ↑ 47.0 47.1 47.2 47.3 47.4 47.5 47.6 47.7 "How Ebola virus counters the interferon system". Zoonoses Public Health 59 (Supplement 2): 116–31. September 2012. doi:10.1111/j.1863-2378.2012.01454.x. PMID 22958256.
- ↑ 48.0 48.1 "Intracellular events and cell fate in filovirus infection". Viruses 3 (8): 1501–31. August 2011. doi:10.3390/v3081501. PMID 21927676.
- ↑ Feldmann, H.; Geisbert, T. W.; Jahrling, P. B.; Klenk, H.-D.; Netesov, S. V.; Peters, C. J.; Sanchez, A.; Swanepoel, R. et al. (2005). "Family Filoviridae". in Fauquet, C. M.; Mayo, M. A.; Maniloff, J. et al.. Virus Taxonomy – Eighth Report of the International Committee on Taxonomy of Viruses. San Diego, U.S.: Elsevier/Academic Press. pp. 645–53. ISBN 978-0-12-370200-5.
- ↑ 50.0 50.1 50.2 50.3 50.4 50.5 50.6 50.7 "Ebola virus disease: an update for anesthesiologists and intensivists". Can J Anaesth 62 (1): 80–91. November 2014. doi:10.1007/s12630-014-0257-z. PMID 25373801.
- ↑ "Ebola (Ebola Virus Disease) Transmission". Centers for Disease Control and Prevention (CDC). 5 November 2014. Archived from the original on 6 November 2014. https://web.archive.org/web/20141106022141/http://www.cdc.gov/vhf/ebola/transmission/index.html. Retrieved 7 November 2014.
- ↑ "Ebola and quarantine". N Engl J Med 371 (21): 2029–30. November 2014. doi:10.1056/NEJMe1413139. PMID 25347231.
- ↑ McNeil Jr., Donald G. (3 October 2014). "Ask Well: How Does Ebola Spread? How Long Can the Virus Survive?". The New York Times. Archived from the original on 24 October 2014. https://web.archive.org/web/20141024061521/http://well.blogs.nytimes.com/2014/10/03/ebola-ask-well-spread-public-transit/. Retrieved 24 October 2014.
- ↑ 54.0 54.1 "How Ebola Is Spread". Centers for Disease Control and Prevention (CDC). 1 November 2014. Archived from the original on 8 July 2017. https://web.archive.org/web/20170708092027/https://www.cdc.gov/vhf/ebola/pdf/infections-spread-by-air-or-droplets.pdf.
- ↑ 55.0 55.1 55.2 55.3 55.4 55.5 55.6 "Transmission". Centers for Disease Control and Prevention (CDC). 17 October 2014. Archived from the original on 19 October 2014. https://web.archive.org/web/20141019024316/http://www.cdc.gov/vhf/ebola/transmission/. Retrieved 18 October 2014.
- ↑ 56.0 56.1 56.2 56.3 "Transmission dynamics and control of Ebola virus disease (EVD): a review". BMC Med 12 (1): 196. October 2014. doi:10.1186/s12916-014-0196-0. PMID 25300956.
- ↑ 57.0 57.1 "Transmission of Ebola viruses: what we know and what we do not know". mBio 6 (2): e00137. 19 February 2015. doi:10.1128/mBio.00137-15. PMID 25698835.
- ↑ "Sexual transmission of the Ebola Virus : evidence and knowledge gaps". World Health Organization (WHO). 4 April 2015. Archived from the original on 14 April 2015. https://web.archive.org/web/20150414084657/http://www.who.int/reproductivehealth/topics/rtis/ebola-virus-semen/en/. Retrieved 16 April 2015.
- ↑ Wu, Brian (2 May 2015). "Ebola Can Be Transmitted Through Sex". Science Times. Archived from the original on 2 May 2015. https://web.archive.org/web/20150502222419/http://www.sciencetimes.com/articles/6000/20150502/ebola-transmitted-through-sex.htm. Retrieved 3 May 2015.
- ↑ "Prevention of sexual transmission of Ebola in Liberia through a national semen testing and counselling programme for survivors: an analysis of Ebola virus RNA results and behavioural data". Lancet Global Health 4 (10): e736–e743. 2016. doi:10.1016/S2214-109X(16)30175-9. PMID 27596037. http://www.thelancet.com/journals/langlo/article/PIIS2214-109X(16)30175-9/fulltext.
- ↑ "Persistence of Ebola Virus in Ocular Fluid during Convalescence". The New England Journal of Medicine 372 (25): 2423–27. 7 May 2015. doi:10.1056/NEJMoa1500306. PMID 25950269.
- ↑ 62.0 62.1 "CDC Telebriefing on Ebola outbreak in West Africa". Centers for Disease Control and Prevention (CDC). 28 July 2014. Archived from the original on 2 August 2014. https://web.archive.org/web/20140802025607/http://www.cdc.gov/media/releases/2014/t0728-ebola.html. Retrieved 3 August 2014.
- ↑ 63.0 63.1 "Air travel is low-risk for Ebola transmission". World Health Organization (WHO). 14 August 2014. Archived from the original on 19 January 2015. https://web.archive.org/web/20150119231747/http://www.who.int/mediacentre/news/notes/2014/ebola-travel/en/.
- ↑ "Ebola virus disease in West Africa – no early end to the outbreak". N Engl J Med 371 (13): 1183–85. September 2014. doi:10.1056/NEJMp1409859. PMID 25140856.
- ↑ "Sierra Leone: a traditional healer and a funeral". World Health Organization (WHO). Archived from the original on 6 October 2014. https://web.archive.org/web/20141006082559/http://www.who.int/csr/disease/ebola/ebola-6-months/sierra-leone/en/. Retrieved 6 October 2014.
- ↑ "The 2014 Ebola Outbreak: International and U.S. Responses". 26 August 2014. Archived from the original on 3 September 2014. https://web.archive.org/web/20140903122230/http://fas.org/sgp/crs/row/R43697.pdf. Retrieved 9 September 2014.
- ↑ Lashley, Felissa R.; Durham, Jerry D., eds (2007). Emerging infectious diseases trends and issues (2nd ed.). New York: Springer. p. 141. ISBN 9780826103505. https://books.google.com/books?id=fsaWlKQ4OjcC&pg=PA141.
- ↑ Alan J. Magill, ed (2013). Hunter's tropical medicine and emerging infectious disease (9th ed.). London, New York: Elsevier. pp. 170–72. ISBN 978-1455740437. OCLC 822525408. https://books.google.com/books?id=x15umovaD08C&pg=PA170.
- ↑ "Questions and Answers on Ebola Hemorrhagic Fever". Centers for Disease Control and Prevention (CDC). 2018-05-22. Archived from the original on 28 July 2017. https://web.archive.org/web/20170728032458/https://www.cdc.gov/vhf/ebola/outbreaks/guinea/qa.html.
- ↑ 70.0 70.1 "Ebola in Texas: Second Health Care Worker Tests Positive". 15 October 2014. Archived from the original on 15 October 2014. https://web.archive.org/web/20141015211852/http://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161.
- ↑ "Aerosol transmission of infectious disease". Journal of Occupational and Environmental Medicine 57 (5): 501–8. May 2015. doi:10.1097/JOM.0000000000000448. PMID 25816216.
- ↑ 72.0 72.1 "Transmission of Ebola virus". 27 September 2014. Archived from the original on 29 January 2016. https://web.archive.org/web/20160129111738/http://www.virology.ws/2014/09/27/transmission-of-ebola-virus/. Retrieved 22 January 2016.
- ↑ 73.0 73.1 73.2 "Transmission of Ebola virus from pigs to non-human primates". Scientific Reports 2: 811. 2012. doi:10.1038/srep00811. PMID 23155478. Bibcode: 2012NatSR...2E.811W.
- ↑ "Risk of Exposure". Centers for Disease Control and Prevention (CDC). 12 October 2014. Archived from the original on 16 October 2014. https://web.archive.org/web/20141016205158/http://www.cdc.gov/vhf/ebola/exposure/index.html. Retrieved 18 October 2014.
- ↑ "FAO warns of fruit bat risk in West African Ebola epidemic". 21 July 2014. Archived from the original on 13 October 2014. https://web.archive.org/web/20141013151812/http://www.fao.org/news/story/en/item/239123/icode/. Retrieved 22 October 2014.
- ↑ Williams, Evan. "African monkey meat that could be behind the next HIV". The Independent. Archived from the original on 22 June 2017. https://web.archive.org/web/20170622133307/http://www.independent.co.uk/life-style/health-and-families/health-news/african-monkey-meat-that-could-be-behind-the-next-hiv-7786152.html. "25 people in Bakaklion, Cameroon killed due to eating of ape"
- ↑ 77.0 77.1 "Ebolavirus – Pathogen Safety Data Sheets". Public Health Agency of Canada. 2001-09-17. Archived from the original on 20 August 2014. https://web.archive.org/web/20140820211755/http://www.phac-aspc.gc.ca/lab-bio/res/psds-ftss/ebola-eng.php. Retrieved 22 August 2014.
- ↑ 78.0 78.1 Wildlife and Emerging Zoonotic Diseases: The Biology, Circumstances and Consequences of Cross-Species Transmission. Ebolavirus and other filoviruses. 315. 2007. 363–87. doi:10.1007/978-3-540-70962-6_15. ISBN 978-3-540-70961-9.
- ↑ 79.0 79.1 79.2 79.3 79.4 79.5 Review of Ebola virus infections in domestic animals. Developments in Biologicals. 135. May 2013. 211–18. doi:10.1159/000178495. ISBN 978-3-318-02365-7. https://semanticscholar.org/paper/e90b6779b4a09d3bb85a80f6f335d6991999c8b9.
- ↑ "Ebola virus disease". Can J Infect Dis Med Microbiol 25 (3): 128–29. May 2014. doi:10.1155/2014/527378. PMID 25285105.
- ↑ 81.0 81.1 81.2 "The natural history of Ebola virus in Africa". Microbes Infect 7 (7–8): 1005–14. June 2005. doi:10.1016/j.micinf.2005.04.006. PMID 16002313.
- ↑ "Experimental inoculation of plants and animals with Ebola virus". Emerg. Infect. Dis. 2 (4): 321–25. October 1996. doi:10.3201/eid0204.960407. ISSN 1080-6040. PMID 8969248.
- ↑ "Fruit bats as reservoirs of Ebola virus". Nature 438 (7068): 575–76. December 2005. doi:10.1038/438575a. PMID 16319873. Bibcode: 2005Natur.438..575L.
- ↑ "Ebola virus antibodies in fruit bats, Bangladesh". Emerg. Infect. Dis. 19 (2): 270–73. February 2013. doi:10.3201/eid1902.120524. PMID 23343532.
- ↑ "Identification of Ebola virus sequences present as RNA or DNA in organs of terrestrial small mammals of the Central African Republic". Microbes and Infection 1 (14): 1193–201. December 1999. doi:10.1016/S1286-4579(99)00242-7. PMID 10580275.
- ↑ "The ecology of Ebola virus". Trends Microbiol 15 (9): 408–16. September 2007. doi:10.1016/j.tim.2007.08.001. PMID 17698361.
- ↑ "Did deforestation cause the Ebola outbreak?". 10 April 2018. https://newint.org/features/web-exclusive/2018/04/10/deforestation-ebola-outbreak. Retrieved 10 July 2018.
- ↑ "Recent loss of closed forests is associated with Ebola virus disease outbreaks". Scientific Reports 7 (1): 14291. 30 October 2017. doi:10.1038/s41598-017-14727-9. ISSN 2045-2322. PMID 29085050. Bibcode: 2017NatSR...714291O.
- ↑ 89.0 89.1 "Clinical features and pathobiology of Ebolavirus infection". J Autoimmun 55: 1–9. September 2014. doi:10.1016/j.jaut.2014.09.001. PMID 25260583.
- ↑ 90.0 90.1 Smith, Tara (2005). Ebola (Deadly Diseases and Epidemics). Chelsea House Publications. ISBN 978-0-7910-8505-9. https://archive.org/details/ebola0000smit.
- ↑ 91.0 91.1 "Filoviral immune evasion mechanisms". Viruses 3 (9): 1634–49. September 2011. doi:10.3390/v3091634. PMID 21994800.
- ↑ "Basic clinical and laboratory features of filoviral hemorrhagic fever". J Infect Dis 204 (Supplement 3): S810–16. November 2011. doi:10.1093/infdis/jir299. PMID 21987756.
- ↑ "Modern uses of electron microscopy for detection of viruses". Clinical Microbiology Reviews 22 (4): 552–63. October 2009. doi:10.1128/CMR.00027-09. PMID 19822888.
- ↑ 94.0 94.1 94.2 "Ebola Hemorrhagic Fever Diagnosis". Centers for Disease Control and Prevention (CDC). 28 January 2014. Archived from the original on 24 September 2014. https://web.archive.org/web/20140924150049/http://www.cdc.gov/vhf/ebola/diagnosis/index.html. Retrieved 3 August 2014.
- ↑ 95.0 95.1 "Laboratory diagnosis of Ebola and Marburg hemorrhagic fever". Bull Soc Pathol Exot 98 (3): 205–09. September 2005. PMID 16267962.
- ↑ "Liberia: New Ebola mobile lab speeds up diagnosis and improves care". World Health Organization (WHO). October 2014. Archived from the original on 24 October 2014. https://web.archive.org/web/20141024235048/http://who.int/features/2014/liberia-mobile-ebola-lab/en/. Retrieved 26 October 2014.
- ↑ 97.0 97.1 "First Antigen Rapid Test for Ebola through Emergency Assessment and Eligible for Procurement". World Health Organization (WHO). Archived from the original on 20 February 2015. https://web.archive.org/web/20150220203131/http://www.who.int/medicines/ebola-treatment/1st_antigen_RT_Ebola/en/. Retrieved 20 February 2015.
- ↑ Longo, DL, ed (2011). "Chapter 197". Harrison's Principles of Internal Medicine (18th ed.). McGraw-Hill. ISBN 978-0-07-174889-6.
- ↑ "Ebola Virus Disease". BMJ 10 (349): g7438. December 2014. doi:10.1136/bmj.g7348. PMID 25497512.
- ↑ "Viral Hemorrhagic Fever" (PDF). S.F. Dept Public Health – Infectious Disease Emergencies. July 2008. Archived from the original on 20 April 2013. https://web.archive.org/web/20130420174306/http://www.sfcdcp.org/document.html?id=316. Retrieved 17 August 2014.
- ↑ "Clinical aspects of African viral hemorrhagic fevers". Rev Infect Dis 11 (Supplement 4): S777–82. May–June 1989. doi:10.1093/clinids/11.supplement_4.s777. PMID 2665013.
- ↑ "A consideration of the diagnosis of dangerous infectious fevers in South Africa". South African Medical Journal 53 (7): 235–37. February 1978. PMID 565951.
- ↑ "Differential diagnosis of infectious diseases with hemorrhagic syndrome". Terapevticheskii Arkhiv 70 (4): 63–68. 1998. PMID 9612907.
- ↑ "Congo Ebola deaths surpass 1,000 as attacks on treatment centers go on". Reuters. 3 May 2019. https://www.reuters.com/article/us-health-ebola-who/congo-ebola-death-toll-to-hit-1000-new-vaccine-planned-who-idUSKCN1S9161. Retrieved 8 May 2019.
- ↑ 105.0 105.1 105.2 "Ebola Hemorrhagic Fever Prevention". Centers for Disease Control and Prevention (CDC). 31 July 2014. Archived from the original on 4 September 2014. https://web.archive.org/web/20140904125431/http://www.cdc.gov/vhf/ebola/prevention/index.html. Retrieved 2 August 2014.
- ↑ 106.0 106.1 "Guidance on Personal Protective Equipment To Be Used by Healthcare Workers During Management of Patients with Ebola Virus Disease in U.S. Hospitals, Including Procedures for Putting On (Donning) and Removing (Doffing)". Centers for Disease Control and Prevention (CDC). 20 October 2014. Archived from the original on 22 October 2014. https://web.archive.org/web/20141022024557/http://www.cdc.gov/vhf/ebola/hcp/procedures-for-ppe.html. Retrieved 22 October 2014.
- ↑ 107.0 107.1 Peters, C. J. (December 1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf.
- ↑ Ebola medics 'better trained in Sierra Leone than Spain' The Telegraph, by Fiona Govan, 11 October 2014
- ↑ This Is How Ebola Patients Are Equipping Their Homes Time magazine, by Alexandra Sifferlin, 9 October 2014
- ↑ Fink, Sheri; Adam Nossiter; James Kanter (10 October 2014). "Doctors Without Borders Evolves as It Forms the Vanguard in Ebola Fight". The New York Times. Archived from the original on 14 October 2014. https://web.archive.org/web/20141014172320/http://www.nytimes.com/2014/10/11/world/africa/doctors-without-borders-evolves-as-it-forms-the-vanguard-in-ebola-fight-.html?_r=0. Retrieved 12 October 2014.
- ↑ "Infection Prevention and Control Guidance for Care of Patients with Suspected or Confirmed Filovirus Haemorrhagic Fever in Health-care Settings with Focus on Ebola". World Health Organization (WHO). August 2014. Archived from the original on 21 August 2014. https://web.archive.org/web/20140821182137/http://apps.who.int/iris/bitstream/10665/130596/1/WHO_HIS_SDS_2014.4_eng.pdf?ua=1&ua=1. Retrieved 21 August 2014.
- ↑ "Ebola – 5 tips to avoid the deadly disease". Plan International. 6 September 2014. Archived from the original on 24 March 2015. https://web.archive.org/web/20150324061050/http://plan-international.org/about-plan/resources/news/ebola-outbreak-5-tips-to-avoid-the-deadly-disease/.
- ↑ "Wild animal mortality monitoring and human Ebola outbreaks, Gabon and Republic of Congo, 2001–2003". Emerg. Infect. Dis. 11 (2): 283–90. February 2005. doi:10.3201/eid1102.040533. ISSN 1080-6040. PMID 15752448.
- ↑ Centers for Disease Control and Prevention and World Health Organization (1998). Infection Control for Viral Haemorrhagic Fevers in the African Health Care Setting. Centers for Disease Control and Prevention (CDC). https://www.cdc.gov/vhf/abroad/pdf/african-healthcare-setting-vhf.pdf. Retrieved 8 February 2013.
- ↑ "Section 7: Use Safe Burial Practices". World Health Organization (WHO). 1 June 2014. Archived from the original on 26 February 2015. https://web.archive.org/web/20150226091100/http://www.who.int/csr/resources/publications/ebola/whoemcesr982sec7-9.pdf.
- ↑ Harden, Blaine (24 December 2000). "Ebola's Shadow". The New York Times. Archived from the original on 20 October 2014. https://web.archive.org/web/20141020200433/http://partners.nytimes.com/library/magazine/home/20001224mag-ebola.html. Retrieved 12 October 2014.
- ↑ Fassassi, Amzath (September 2014). "How anthropologists help medics fight Ebola in Guinea". SciDev.Net. Archived from the original on 6 October 2014. https://web.archive.org/web/20141006112752/http://www.scidev.net/global/cooperation/feature/anthropologists-medics-ebola-guinea.html. Retrieved 3 October 2014.
- ↑ "West Africa – Ebola virus disease Update: Travel and transport". World Health Organization (WHO). Archived from the original on 29 July 2014. https://web.archive.org/web/20140729034008/http://www.who.int/ith/updates/20140421/en/.
- ↑ 119.0 119.1 119.2 "Monitoring Symptoms and Controlling Movement to Stop Spread of Ebola". Centers for Disease Control and Prevention (CDC). 27 October 2014. Archived from the original on 8 July 2017. https://web.archive.org/web/20170708091445/https://www.cdc.gov/media/releases/2014/fs1027-monitoring-symptoms-controlling-movement.html.
- ↑ 120.0 120.1 "Ebola: Control and Prevention". Occupational Safety and Health Administration (OSHA). Archived from the original on 9 November 2014. https://web.archive.org/web/20141109145135/https://www.osha.gov/SLTC/ebola/control_prevention.html. Retrieved 9 November 2014.
- ↑ "About Quarantine and Isolation". Centers for Disease Control and Prevention (CDC). 28 August 2014. Archived from the original on 20 October 2014. https://web.archive.org/web/20141020041517/http://www.cdc.gov/quarantine/quarantineisolation.html. Retrieved 26 October 2014.
- ↑ Sompayrac, Lauren (2002). How pathogenic viruses work (3 ed.). Boston: Jones and Bartlett Publishers. p. 87. ISBN 9780763720827. https://books.google.com/books?id=PrOHLe35qNEC&pg=PA87.
- ↑ "[Ebola and Marburg viruses: the humans strike back"] (in French). Med Sci (Paris) 22 (4): 405–10. April 2006. doi:10.1051/medsci/2006224405. PMID 16597410. https://www.medecinesciences.org/articles/medsci/pdf/2006/05/medsci2006224p405.pdf.
- ↑ "Ebola virus disease update – west Africa". World Health Organization (WHO). 19 August 2014. Archived from the original on 22 October 2014. https://web.archive.org/web/20141022110953/http://www.who.int/csr/don/2014_08_19_ebola/en/. Retrieved 26 October 2014.
- ↑ Koenig, Kristi; Schultz, Carl, eds (2009). Koenig and Schultz's disaster medicine : comprehensive principles and practices. Cambridge: Cambridge University Press. p. 209. ISBN 9780521873673. https://books.google.com/books?id=IfpOtV-FAl4C&pg=PA209.
- ↑ "Control of Communicable Diseases". Federal Register. 19 January 2017. https://www.federalregister.gov/documents/2017/01/19/2017-00615/control-of-communicable-diseases.
- ↑ "Ebola 2014 – New Challenges, New Global Response and Responsibility". New England Journal of Medicine 371 (13): 1177–1180. 25 September 2014. doi:10.1056/NEJMp1409903. PMID 25140858.
- ↑ "What is Contact Tracing?". Centers for Disease Control and Prevention (CDC). Archived from the original on 12 September 2014. https://web.archive.org/web/20140912114723/http://www.cdc.gov/vhf/ebola/pdf/contact-tracing.pdf. Retrieved 15 September 2014.
- ↑ "FDA warns consumers about fraudulent Ebola treatment products" (Press release). Archived from the original on 11 January 2017. Retrieved 20 August 2014.
- ↑ "Natural Solutions Foundation Warning Letter". U.S. Food and Drug Administration (FDA). 22 September 2014. Archived from the original on 8 October 2014. https://web.archive.org/web/20141008213137/https://www.fda.gov/ICECI/EnforcementActions/WarningLetters/2014/ucm416051.htm. Retrieved 9 October 2014.
- ↑ 131.0 131.1 131.2 131.3 131.4 131.5 "Clinical management of filovirus-infected patients". Viruses 4 (9): 1668–86. September 2012. doi:10.3390/v4091668. PMID 23170178.
- ↑ "Ebola messages for the general public". World Health Organization (WHO). Archived from the original on 25 October 2014. https://web.archive.org/web/20141025120028/http://www.who.int/csr/disease/ebola/messages/en/. Retrieved 26 October 2014.
- ↑ "Annex 18. Transmission risk reduction of filoviruses in home-care settings". World Health Organization (WHO). Archived from the original on 26 October 2014. https://web.archive.org/web/20141026092619/http://www.who.int/csr/disease/ebola/Annex_18_risk_reduction_home_care.pdf?ua=1. Retrieved 26 October 2014.
- ↑ C.M. Fauquet (2005). Virus taxonomy classification and nomenclature of viruses; 8th report of the International Committee on Taxonomy of Viruses. Oxford: Elsevier/Academic Press. p. 648. ISBN 9780080575483. https://books.google.com/books?id=9Wy7Jgy5RWYC&pg=PA648.
- ↑ "More or Less behind the stats Ebola". BBC World Service. Archived from the original on 3 September 2014. https://web.archive.org/web/20140903044359/http://www.bbc.co.uk/programmes/p0244jdt. Retrieved 8 October 2014.
- ↑ 136.0 136.1 "An update on ocular complications of Ebola virus disease". Current Opinion in Ophthalmology 28 (6): 600–06. November 2017. doi:10.1097/ICU.0000000000000426. PMID 28872492.
- ↑ "Ocular problem in Ebola virus infection: A short review". Saudi Journal of Ophthalmology 29 (3): 225–26. 2015. doi:10.1016/j.sjopt.2015.02.006. PMID 26155084.
- ↑ "Persistence of Ebola Virus in Ocular Fluid during Convalescence". New England Journal of Medicine 372 (25): 2423–27. 2015. doi:10.1056/NEJMoa1500306. ISSN 0028-4793. PMID 25950269.
- ↑ "Ebola virus in the semen of convalescent men". The Lancet Infectious Diseases 15 (2): 149–50. 2015. doi:10.1016/S1473-3099(14)71033-3. ISSN 1473-3099. PMID 25467652.
- ↑ "Ebola virus as a sexually transmitted infection". Current Opinion in Infectious Diseases 28 (1): 83–85. February 2015. doi:10.1097/qco.0000000000000135. PMID 25501666.
- ↑ "Possible sexual transmission of Ebola virus – Liberia, 2015". MMWR. Morbidity and Mortality Weekly Report 64 (17): 479–81. 8 May 2015. PMID 25950255.
- ↑ "Handle Survivors with Care". The New England Journal of Medicine 377 (15): 1480–1482. 14 October 2015. doi:10.1056/NEJMe1512928. PMID 26465064.
- ↑ "Neuro complications cited in UK nurse's Ebola case". Archived from the original on 17 October 2015. https://web.archive.org/web/20151017211314/http://www.cidrap.umn.edu/news-perspective/2015/10/neuro-complications-cited-uk-nurses-ebola-case. Retrieved 19 October 2015.
- ↑ "Post-Ebola Syndrome, Sierra Leone". Emerg. Infect. Dis. 22 (4): 641–46. April 2016. doi:10.3201/eid2204.151302. PMID 26983037.
- ↑ "Ecologic and Geographic Distribution of Filovirus Disease". Emerg. Infect. Dis. 10 (1): 40–47. 2004. doi:10.3201/eid1001.030125. PMID 15078595.
- ↑ 146.0 146.1 "Ebola haemorrhagic fever in Sudan, 1976". Archived from the original on 13 October 2014. https://web.archive.org/web/20141013194802/http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56(2)_247-270.pdf. Retrieved 8 October 2014.
- ↑ Hewlett, Barry; Hewlett, Bonnie (2007). Ebola, Culture and Politics: The Anthropology of an Emerging Disease. Cengage Learning. p. 103. ISBN 978-1111797317. https://books.google.com/?id=aboFAAAAQBAJ&pg=PA103. Retrieved 31 July 2014.
- ↑ 148.0 148.1 "Ebola virus: from discovery to vaccine". Nature Reviews Immunology 3 (8): 677–85. August 2003. doi:10.1038/nri1154. PMID 12974482.
- ↑ 149.0 149.1 "Ebola haemorrhagic fever in Zaire, 1976". Bull. World Health Organ. 56 (2): 271–93. 1978. PMID 307456. PMC 2395567. Archived from the original on 8 August 2014. https://web.archive.org/web/20140808213715/http://whqlibdoc.who.int/bulletin/1978/Vol56-No2/bulletin_1978_56%282%29_271-293.pdf. Retrieved 14 August 2014.
- ↑ Centers for Disease Control Prevention (CDC) (1995). "Outbreak of Ebola Viral Hemorrhagic Fever – Zaire, 1995". Morbidity and Mortality Weekly Report 44 (19): 381–2. PMID 7739512. Archived from the original on 25 June 2017. https://web.archive.org/web/20170625191457/https://www.cdc.gov/mmwr/preview/mmwrhtml/00037078.htm.
- ↑ Elezra M. "Ebola: The Truth Behind The Outbreak (Video) l". http://politicalmoll.com/tag/mabalo-lokela/.
- ↑ 152.0 152.1 Stimola, Aubrey (2011). Ebola (1st ed.). New York: Rosen Pub.. pp. 31, 52. ISBN 978-1435894334. https://archive.org/details/ebola0000stim/page/31.
- ↑ "This Congolese Doctor Discovered Ebola But Never Got Credit For It — Until Now". https://www.npr.org/sections/goatsandsoda/2019/11/04/774863495/this-congolese-doctor-discovered-ebola-but-never-got-credit-for-it-until-now.
- ↑ McNeish, Hannah (2017-03-24). "He Treated The Very First Ebola Cases 40 Years Ago. Then He Watched The World Forget.". https://www.huffpost.com/entry/ebola-neglected-tropical-diseases_n_58d2ac02e4b0f838c62e9e0d.
- ↑ No time to lose: a life in pursuit of deadly viruses (1st ed.). New York: W.W. Norton & Co.. 2012. pp. 30, 90. ISBN 978-0393063165.
- ↑ Piot, Peter (11 August 2014). "Part one: A virologist's tale of Africa's first encounter with Ebola". ScienceInsider. Archived from the original on 9 October 2014. https://web.archive.org/web/20141009050901/http://news.sciencemag.org/africa/2014/08/part-one-virologists-tale-africas-first-encounter-ebola.
- ↑ Piot, Peter (13 August 2014). "Part two: A virologist's tale of Africa's first encounter with Ebola". ScienceInsider. Archived from the original on 16 November 2014. https://web.archive.org/web/20141116233325/http://news.sciencemag.org/africa/2014/08/part-two-virologists-tale-africas-first-encounter-ebola.
- ↑ Bardi, Jason Socrates. "Death Called a River". Archived from the original on 2 August 2014. https://web.archive.org/web/20140802170848/http://www.scripps.edu/newsandviews/e_20020114/ebola1.html. Retrieved 9 October 2014.
- ↑ Preston, Richard (20 July 1995). The Hot Zone. Anchor Books (Random House ). p. 117. "Karl Johnson named it Ebola"
- ↑ Bredow, Rafaela von; Hackenbroch, Veronika (4 October 2014). "In 1976 I Discovered Ebola – Now I Fear an Unimaginable Tragedy". Archived from the original on 3 January 2017. https://web.archive.org/web/20170103105318/https://www.theguardian.com/world/2014/oct/04/ebola-zaire-peter-piot-outbreak.
- ↑ King, John W. (2 April 2008). "Ebola Virus". WebMD. Archived from the original on 28 September 2008. https://web.archive.org/web/20080928063653/http://www.emedicine.com/med/TOPIC626.HTM. Retrieved 6 October 2008.
- ↑ "[Outbreak of Ebola hemorrhagic fever in the Republic of the Congo, 2003: a new strategy?]" (in French). Med Trop (Mars) 63 (3): 291–95. 2003. PMID 14579469.
- ↑ Miller, Judith (25 May 2004). "Russian Scientist Dies in Ebola Accident at Former Weapons Lab". The New York Times. Archived from the original on 17 October 2014. https://web.archive.org/web/20141017035417/http://www.nytimes.com/2004/05/25/world/russian-scientist-dies-in-ebola-accident-at-former-weapons-lab.html. Retrieved 12 October 2014.
- ↑ "Ebola outbreak in Congo". CBC News. 12 September 2007. Archived from the original on 19 November 2014. https://web.archive.org/web/20141119105248/http://www.cbc.ca/news/world/ebola-outbreak-in-congo-1.648593.
- ↑ 165.0 165.1 "Mystery DR Congo fever kills 100". BBC News Online. 31 August 2007. Archived from the original on 11 November 2007. https://web.archive.org/web/20071111024636/http://news.bbc.co.uk/2/hi/africa/6973013.stm.
- ↑ "Ebola Outbreak Confirmed in Congo". 11 September 2007. Archived from the original on 18 June 2015. https://web.archive.org/web/20150618230241/http://www.newscientist.com/article/dn12624-ebola-outbreak-confirmed-in-congo.html.
- ↑ "Uganda: Deadly Ebola Outbreak Confirmed – UN". UN News Service. 30 November 2007. Archived from the original on 3 March 2008. https://web.archive.org/web/20080303200540/http://allafrica.com/stories/200711301070.html. Retrieved 25 February 2008.
- ↑ "DRC Confirms Ebola Outbreak". Voanews.com. Archived from the original on 15 September 2012. https://web.archive.org/web/20120915235056/http://www.voanews.com/content/Ebola-drc-outbreak/1492233.html. Retrieved 15 April 2013.
- ↑ "WHO – Ebola outbreak in Democratic Republic of Congo". World Health Organization (WHO). 17 August 2012. Archived from the original on 27 October 2013. https://web.archive.org/web/20131027035536/http://www.who.int/csr/don/2012_08_18/en/index.html. Retrieved 15 April 2013.
- ↑ "WHO – Ebola outbreak in Democratic Republic of Congo – update". World Health Organization (WHO). 21 August 2012. Archived from the original on 16 December 2012. https://web.archive.org/web/20121216144914/http://www.who.int/csr/don/2012_08_21/en/index.html. Retrieved 15 April 2013.
- ↑ Castillo, Michelle (2012). "Ebola virus claims 31 lives in Democratic Republic of the Congo". CBS News (United States). Archived from the original on 14 September 2012. https://web.archive.org/web/20120914015301/http://www.cbsnews.com/8301-504763_162-57512216-10391704/ebola-virus-claims-31-lives-in-democratic-republic-of-the-congo/. Retrieved 14 September 2012.
- ↑ "Virological Analysis: no link between Ebola outbreaks in west Africa and Democratic Republic of Congo". World Health Organization (WHO). 2 September 2014. Archived from the original on 21 November 2014. https://web.archive.org/web/20141121121328/http://www.who.int/mediacentre/news/ebola/2-september-2014/en/.
- ↑ "Congo declares its Ebola outbreak over". Reuters. 15 November 2014. Archived from the original on 29 November 2014. https://web.archive.org/web/20141129065140/http://uk.reuters.com/article/2014/11/15/health-ebola-congodemocratic-idUKL6N0T50F720141115. Retrieved 15 November 2014.
- ↑ "Democratic Republic of the Congo: The country that knows how to beat Ebola". World Health Organization (WHO). December 2014. Archived from the original on 26 February 2015. https://web.archive.org/web/20150226005300/http://www.who.int/features/2014/drc-beats-ebola/en/. Retrieved 26 February 2015.
- ↑ 175.0 175.1 "Guidelines for Evaluation of US Patients Suspected of Having Ebola Virus Disease". Centers for Disease Control and Prevention (CDC). 1 August 2014. Archived from the original on 8 August 2014. https://web.archive.org/web/20140808075214/http://emergency.cdc.gov/han/han00364.asp. Retrieved 5 August 2014.
- ↑ "Emergence of Zaire Ebola Virus Disease in Guinea". New England Journal of Medicine 371 (15): 1418–25. October 2014. doi:10.1056/NEJMoa1404505. PMID 24738640. https://semanticscholar.org/paper/29bafbdb9b461edc7f705777a6672000570b896c.
- ↑ "The first cases of this Ebola outbreak traced by WHO" (png). World Health Organization (WHO). 2014. Archived from the original on 6 October 2014. https://web.archive.org/web/20141006092047/http://who.int/csr/disease/ebola/ebola-6-months/guinea-chart-big.png?ua=1.
- ↑ "WHO raises global alarm over Ebola outbreak". CBS News. Archived from the original on 8 August 2014. https://web.archive.org/web/20140808095616/http://www.cbsnews.com/news/ebola-outbreak-international-public-health-emergency-who/. Retrieved 2 August 2014.
- ↑ Fulton, Deirdre (18 August 2014). "In Liberia's Ebola-Stricken Villages, Residents Face 'Stark' Choices". Common Dreams. Archived from the original on 20 August 2014. https://web.archive.org/web/20140820041111/http://www.commondreams.org/news/2014/08/18/liberias-ebola-stricken-villages-residents-face-stark-choices. Retrieved 20 August 2014.
- ↑ "Experimental therapies: growing interest in the use of whole blood or plasma from recovered Ebola patients (convalescent therapies)" (Press release). World Health Organization (WHO). 26 September 2014. Archived from the original on 28 September 2014. Retrieved 28 September 2014.
- ↑ "2014 Ebola Outbreak in West Africa – Case Counts". Centers for Disease Control and Prevention (CDC). 2014. Archived from the original on 6 August 2017. https://web.archive.org/web/20170806135144/https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/index.html.
- ↑ "Ebola Response Roadmap Situation Report". World Health Organization (WHO). 1 October 2014. Archived from the original on 2 October 2014. https://web.archive.org/web/20141002142707/http://apps.who.int/iris/bitstream/10665/135600/1/roadmapsitrep_1Oct2014_eng.pdf?ua=1.
- ↑ "Unprecedented number of medical staff infected with Ebola". World Health Organization (WHO). 25 August 2014. Archived from the original on 28 August 2014. https://web.archive.org/web/20140828123825/http://www.who.int/mediacentre/news/ebola/25-august-2014/en/. Retrieved 29 August 2014.
- ↑ "Ebola response roadmap - Situation report" (PDF). World Health Organization (WHO). 10 December 2014. Archived from the original on 10 December 2014. https://web.archive.org/web/20141210214551/http://apps.who.int/iris/bitstream/10665/145198/1/roadmapsitrep_10Dec2014_eng.pdf?ua=1. Retrieved 11 December 2014.
- ↑ "Ebola Situation Report". World Health Organization (WHO). 28 January 2015. Archived from the original on 3 February 2015. https://web.archive.org/web/20150203214717/http://apps.who.int/ebola/en/ebola-situation-report/situation-reports/ebola-situation-report-28-january-2015. Retrieved 5 February 2015.
- ↑ "Ebola Situation Report". World Health Organization (WHO). 8 April 2015. Archived from the original on 14 April 2015. https://web.archive.org/web/20150414170339/http://apps.who.int/iris/bitstream/10665/161244/1/roadmapsitrep_8Apr2015_eng.pdf?ua=1&ua=1. Retrieved 14 April 2015.
- ↑ "Ebola gone from Guinea". Thomson Reuters. CBC News. 29 December 2015. Archived from the original on 30 December 2015. https://web.archive.org/web/20151230001240/http://www.cbc.ca/news/health/ebola-guinea-1.3382945. Retrieved 30 December 2015.
- ↑ "UN declares end to Ebola virus transmission in Guinea; first time all three host countries free" (Press release). United Nations. Archived from the original on 1 January 2016. Retrieved 30 December 2015.
- ↑ "New Ebola case in Sierra Leone. WHO continues to stress risk of more flare-ups". World Health Organization (WHO). 15 January 2016. Archived from the original on 27 January 2016. https://web.archive.org/web/20160127143222/http://www.who.int/mediacentre/news/statements/2016/new-ebola-case/en/. Retrieved 25 January 2016.
- ↑ Botelho, Greg; Jacque Wilson (8 October 2014). "Thomas Eric Duncan: First Ebola death in U.S.". CNN. Archived from the original on 29 May 2016. https://web.archive.org/web/20160529040652/http://edition.cnn.com/2014/10/08/health/thomas-eric-duncan-ebola/index.html. Retrieved 8 August 2017.
- ↑ "Second US Ebola diagnosis 'deeply concerning', admits CDC chief". Archived from the original on 14 October 2014. https://web.archive.org/web/20141014175544/http://www.msn.com/en-us/news/us/second-us-ebola-diagnosis-deeply-concerning-admits-cdc-chief/ar-BB8UFz0.archiveurl=https://web.archive.org/web/20141014175544/http://www.msn.com/en-us/news/us/second-us-ebola-diagnosis-deeply-concerning-admits-cdc-chief/ar-BB8UFz0%7Carchivedate%3D14 October 2013
- ↑ "Ebola crisis: Tests show Spanish nurse Teresa Romero no longer has the virus". ABC News. 20 October 2014. Archived from the original on 29 October 2014. https://web.archive.org/web/20141029201132/http://www.abc.net.au/news/2014-10-20/spanish-nurse-infected-with-ebola-no-longer-has-virus/5825720.
- ↑ Fernandez, Manny (12 October 2014). "Texas Health Worker Tests Positive for Ebola". The New York Times. Archived from the original on 12 October 2014. https://web.archive.org/web/20141012162113/http://www.nytimes.com/2014/10/13/us/texas-health-worker-tests-positive-for-ebola.html. Retrieved 12 October 2014.
- ↑ "Ebola in Texas: Second Health Care Worker Tests Positive". Archived from the original on 15 October 2014. https://web.archive.org/web/20141015211852/http://www.nbcnews.com/storyline/ebola-virus-outbreak/ebola-texas-second-health-care-worker-tests-positive-n226161.
- ↑ 195.0 195.1 "Cases of Ebola Diagnosed in the United States". 2018-05-22. Archived from the original on 26 February 2017. https://web.archive.org/web/20170226055827/https://www.cdc.gov/vhf/ebola/outbreaks/2014-west-africa/united-states-imported-case.html.
- ↑ Sanchez, Ray; Prokupecz, Shimon (23 October 2014). "N.Y. doctor positive for Ebola had no symptoms until Thursday, officials say". CNN. Archived from the original on 24 October 2014. https://web.archive.org/web/20141024022702/http://www.cnn.com/2014/10/23/health/new-york-possible-ebola-case/index.html?hpt=hp_t1. Retrieved 23 October 2014.
- ↑ Sun, Lena H.; Achenbach, Joel (24 December 2014). "CDC reports potential Ebola exposure in Atlanta lab". The Washington Post. Archived from the original on 25 December 2014. https://web.archive.org/web/20141225002131/http://www.washingtonpost.com/national/health-science/cdc-reports-potential-ebola-exposure-in-atlanta-lab/2014/12/24/f1a9f26c-8b8e-11e4-8ff4-fb93129c9c8b_story.html. Retrieved 25 December 2014.
- ↑ "Ebola case confirmed in Glasgow hospital". BBC News Online. 29 December 2014. Archived from the original on 29 December 2014. https://web.archive.org/web/20141229191607/http://www.bbc.co.uk/news/uk-scotland-30628349.
- ↑ "Ebola nurse Pauline Cafferkey transferred to London unit". BBC News Online. 30 December 2014. Archived from the original on 30 December 2014. https://web.archive.org/web/20141230120858/http://www.bbc.com/news/uk-scotland-30629397.
- ↑ 200.0 200.1 "WHO says 19 dead, 39 infected so far in Congo Ebola outbreak". MSN. http://www.msn.com/en-us/health/medical/who-says-19-dead-39-infected-so-far-in-congo-ebola-outbreak/ar-AAxfhX9?ocid=ientp. Retrieved 2018-05-14.
- ↑ "WHO planning for 'worst case scenario' over DRC Ebola outbreak". Al Jazeera. https://www.aljazeera.com/news/2018/05/planning-worst-case-scenario-drc-ebola-outbreak-180511153458973.html. Retrieved 2018-05-14.
- ↑ "19 dead in latest Congo Ebola outbreak: WHO". https://www.reuters.com/video/2018/05/14/19-dead-in-latest-congo-ebola-outbreak-w?videoId=426863714&videoChannel=118261. Retrieved 2018-05-14.
- ↑ Editorial, Reuters (2018-05-14). "UPDATE 1-WHO gets approval to use Ebola vaccine in Democratic…". Reuters. https://www.reuters.com/article/health-ebola-who/update-1-who-gets-approval-to-use-ebola-vaccine-in-democratic-republic-of-congo-idUSL5N1SL554. Retrieved 5 August 2018.
- ↑ "WHO Director General visits Ebola-affected areas in DR Congo". World Health Organization (WHO). http://www.who.int/news-room/detail/13-05-2018-who-director-general-visits-ebola-affected-areas-in-dr-congo. Retrieved 2018-05-14.
- ↑ Yong, Ed (21 May 2018). "Most Maps of the New Ebola Outbreak Are Wrong: Villages, and sometimes whole regions of the Congo, are misplaced—but the ministry of health and a team of cartographers are racing to get better data". The Atlantic. https://www.theatlantic.com/health/archive/2018/05/most-maps-of-the-new-ebola-outbreak-are-wrong/560777/.
- ↑ "Ebola In A Conflict Zone". National Public Radio (NPR). https://www.npr.org/sections/goatsandsoda/2018/08/02/635016034/ebola-in-a-conflict-zone. Retrieved 5 August 2018.
- ↑ Specia, Megan (2018-08-02). "The Latest Ebola Outbreak Is Centered in a War Zone". The New York Times. https://www.nytimes.com/2018/08/02/world/africa/ebola-outbreak-congo-war-zone.html. Retrieved 5 August 2018.
- ↑ "DRC: Ebola Outbreak Worst in Country's History, Kills Almost 200". Democracy Now. 13 November 2018. https://www.democracynow.org/2018/11/13/headlines/drc_ebola_outbreak_worst_in_countrys_history_kills_almost_200. Retrieved 14 November 2018.
- ↑ "Ebola outbreak in eastern Democratic Republic of Congo tops 1,000 cases" (Press release). Centers for Disease Control and Prevention (CDC). 29 March 2019. Retrieved 12 May 2019.
- ↑ "Ebola virus disease – Democratic Republic of the Congo". World Health Organization (WHO). http://www.who.int/csr/don/02-may-2019-ebola-drc/en/. Retrieved 12 May 2019.
- ↑ "Ebola virus disease – Democratic Republic of the Congo - Disease outbreak news: Update 6 June 2019". World Health Organization (WHO). 2019-06-06. Archived from the original on 2019-06-07. https://web.archive.org/web/20190607113738/https://www.who.int/csr/don/06-june-2019-ebola-drc/en/. Retrieved 2019-06-07.
- ↑ "Ebola outbreak: Grandmother dies in Uganda". BBC News Online. 2019-06-13. https://www.bbc.co.uk/news/world-africa-48622635. Retrieved 2019-06-15.
- ↑ Larson, Krista (2019-07-15). "Congo tracing contacts of first Ebola case in eastern city". https://apnews.com/7ae99b8b4e414467b9139abde98684ee. Retrieved 2019-07-17.
- ↑ Cheng, Maria; Keaten, Jamey (2019-07-17). "Ebola outbreak in Congo declared a global health emergency". https://apnews.com/204fc739fc5846cdba4093ee65c4f7db. Retrieved 2019-07-17.
- ↑ "Half of Ebola cases in DR Congo 'unidentified'". BBC News Online. 2019-08-02. https://www.bbc.com/news/world-africa-49212116. Retrieved 2019-08-03.
- ↑ "Ebola and Marburg hemorrhagic fevers: neglected tropical diseases?". PLoS Negl Trop Dis 6 (6): e1546. June 2012. doi:10.1371/journal.pntd.0001546. PMID 22761967.
- ↑ "Hemorrhagic fever viruses as biological weapons: medical and public health management". Journal of the American Medical Association 287 (18): 2391–405. May 2002. doi:10.1001/jama.287.18.2391. PMID 11988060.
- ↑ "Other viral bioweapons: Ebola and Marburg hemorrhagic fever". Dermatologic Clinics 22 (3): 291–302, vi. July 2004. doi:10.1016/j.det.2004.03.003. PMID 15207310.
- ↑ Zubray, Geoffrey (2013). Agents of Bioterrorism: Pathogens and Their Weaponization. New York, NY, USA: Columbia University Press. pp. 73–74. ISBN 9780231518130. https://books.google.com/books?id=AwkVgNPRnKoC&pg=PA73.
- ↑ "Malicious Ebola-Themed Emails Are on the Rise". 24 October 2014. Archived from the original on 7 July 2017. https://web.archive.org/web/20170707125209/https://bits.blogs.nytimes.com/2014/10/24/malicious-ebola-themed-emails-are-on-the-rise/?action=click&contentCollection=US%20Open®ion=Article&module=Promotron. Retrieved 26 October 2014.
- ↑ "North Korea bans foreigners from Pyongyang marathon over Ebola". BBC News Online. 23 February 2015. Archived from the original on 24 February 2015. https://web.archive.org/web/20150224061401/http://www.bbc.com/news/world-asia-31581935. Retrieved 23 February 2015.
- ↑ Preston, Richard (1995). The Hot Zone, A Terrifying True Story. Anchor Books. ISBN 978-0-385-47956-1. OCLC 32052009. https://books.google.com/books?id=E6BKpf2tSkoC.
- ↑ "Best Sellers: 4 June 1995". The New York Times Book Review. 4 June 1995. https://query.nytimes.com/gst/fullpage.html?res=9C06E3DA1E39F937A35755C0A963958260. Retrieved 10 September 2014.
- ↑ "About The Hot Zone". Random House. Archived from the original on 7 October 2014. https://web.archive.org/web/20141007011934/http://www.randomhouse.com/features/richardpreston/bookshelf/hz.html. Retrieved 10 September 2014.archiveurl=https://web.archive.org/web/20141006105554/ http://www.randomhouse.com/features/richardpreston/bookshelf/hz.html%7Carchivedate=6 October 2014
- ↑ Close, William T. (1995). Ebola: A Documentary Novel of Its First Explosion. New York: Ivy Books. ISBN 978-0804114325. OCLC 32753758. https://books.google.com/books?id=1IvgAAAAMAAJ.
- ↑ Grove, Ryan (2 June 2006). "More about the people than the virus". Archived from the original on 21 October 2014. https://web.archive.org/web/20141021075254/http://www.amazon.com/Ebola-documentary-novel-first-explosion/dp/B007HEJSE6. Retrieved 17 September 2014.
- ↑ Close, William T. (2002). Ebola: Through the Eyes of the People. Marbleton, Wyoming: Meadowlark Springs Productions. ISBN 978-0970337115. OCLC 49193962. https://books.google.com/books?id=BX0gAQAAIAAJ.
- ↑ Pink, Brenda (24 June 2008). "A fascinating perspective". Archived from the original on 21 October 2014. https://web.archive.org/web/20141021075312/http://www.amazon.com/Ebola-Through-William-T-Close/product-reviews/0970337116. Retrieved 17 September 2014.
- ↑ Clancy, Tom (1996). Executive Orders. New York: Putnam. ISBN 978-0399142185. OCLC 34878804. https://books.google.com/books?id=m1Cny9KFm_wC.
- ↑ Stone, Oliver (2 September 1996). "Who's That in the Oval Office?". The New York Times. Archived from the original on 10 April 2009. https://web.archive.org/web/20090410091107/http://www.nytimes.com/books/97/08/17/bsp/20141.html. Retrieved 10 September 2014.
- ↑ Dewey, Caitlin (2 October 2014). "Popular on Amazon: Wildly misleading self-published books about Ebola, by random people without medical degrees". The Washington Post. Archived from the original on 22 October 2014. https://web.archive.org/web/20141022174054/http://www.washingtonpost.com/news/the-intersect/wp/2014/10/02/popular-on-amazon-wildly-misleading-self-published-books-about-ebola-by-random-people-without-medical-degrees/. Retrieved 27 October 2014.
- ↑ "Emerging targets and novel approaches to Ebola virus prophylaxis and treatment". BioDrugs 27 (6): 565–83. December 2013. doi:10.1007/s40259-013-0046-1. PMID 23813435.
- ↑ "Ebola 'kills over 5,000 gorillas'". BBC News Online. 8 December 2006. Archived from the original on 29 March 2009. https://web.archive.org/web/20090329013552/http://news.bbc.co.uk/2/hi/science/nature/6220122.stm. Retrieved 31 May 2009.
- ↑ 234.0 234.1 "Multiple Ebola virus transmission events and rapid decline of central African wildlife". Science 303 (5656): 387–90. January 2004. doi:10.1126/science.1092528. PMID 14726594. Bibcode: 2004Sci...303..387L.
- ↑ "Ebola virus outbreak among wild chimpanzees living in a rain forest of Côte d'Ivoire". The Journal of Infectious Diseases. 179 Suppl 1 (s1): S120–S126. February 1999. doi:10.1086/514296. PMID 9988175.
- ↑ "Transmission of Ebola virus from pigs to non-human primates". Sci Rep 2: 811. November 2012. doi:10.1038/srep00811. PMID 23155478. Bibcode: 2012NatSR...2E.811W.
- ↑ "Ebola virus antibody prevalence in dogs and human risk". Emerg. Infect. Dis. 11 (3): 385–90. March 2005. doi:10.3201/eid1103.040981. PMID 15757552.
- ↑ 238.0 238.1 238.2 Preston, Richard (1994). The Hot Zone. New York: Random House. p. 300. ISBN 978-0679437840. https://archive.org/details/hotzone00pres.
- ↑ McCormick & Fisher-Hoch 1999, pp. 277–79
- ↑ Waterman, Tara (1999). Ebola Reston Outbreaks. Stanford University. http://www.stanford.edu/group/virus/filo/ebor.html. Retrieved 2 August 2008.
- ↑ 241.0 241.1 McCormick & Fisher-Hoch 1999, pp. 298–99
- ↑ McCormick & Fisher-Hoch 1999, p. 300
- ↑ "Outbreaks Chronology: Ebola Virus Disease". Centers for Disease Control and Prevention (CDC).gov. Archived from the original on 26 October 2014. https://web.archive.org/web/20141026230925/http://origin.glb.cdc.gov/vhf/ebola/outbreaks/history/chronology.html. Retrieved 26 October 2014.
- ↑ McNeil Jr, Donald G. (24 January 2009). "Pig-to-Human Ebola Case Suspected in Philippines". The New York Times. Archived from the original on 10 March 2009. https://web.archive.org/web/20090310113731/http://www.nytimes.com/2009/01/24/health/24ebola.html. Retrieved 26 January 2009.
- ↑ "Final trial results confirm Ebola vaccine provides high protection against disease". World Health Organization (WHO). Archived from the original on 1 April 2017. https://web.archive.org/web/20170401042946/http://who.int/mediacentre/news/releases/2016/ebola-vaccine-results/en/. Retrieved 2017-03-29.
- ↑ "Two Ebola drugs show promise amid ongoing outbreak". Nature. 12 August 2019. doi:10.1038/d41586-019-02442-6. ISSN 0028-0836.
- ↑ "Therapeutic strategies to target the Ebola virus life cycle". Nature Reviews. Microbiology 17 (10): 593–606. 24 July 2019. doi:10.1038/s41579-019-0233-2. ISSN 1740-1526. PMID 31341272.
- ↑ "Investigational Monoclonal Antibody to Treat Ebola Is Safe in Adults" (Press release). National Institute of Allergy and Infectious Diseases (NIAID). 24 January 2019. Retrieved 12 August 2019.
- ↑ Butler, Declan. "Ebola Experts Seek to Expand Testing". Scientific American. Archived from the original on 13 December 2014. https://web.archive.org/web/20141213012943/http://www.scientificamerican.com/article/ebola-experts-seek-to-expand-testing/. Retrieved 11 December 2014.
- ↑ Buchanan, Rose Troup (29 November 2014). "Ebola outbreak: New 15-minute test offers hope for thousands". The Independent. Archived from the original on 1 December 2014. https://web.archive.org/web/20141201003020/http://www.independent.co.uk/news/world/africa/ebola-outbreak-new-15minute-test-trialled-in-guinea-offers-hope-for-thousands-9892543.html. Retrieved 1 December 2014.
- ↑ Falconi, Marta (29 December 2014). "Roche Secures Emergency Approval by U.S. Regulators for Ebola Test". The Wall Street Journal. Archived from the original on 29 December 2014. https://web.archive.org/web/20141229163045/http://www.wsj.com/articles/roche-secures-emergency-approval-by-u-s-regulators-for-ebola-test-1419840858. Retrieved 29 December 2014.
- ↑ Junaid, Abidemi; Tang, Huaqi; van Reeuwijk, Anne; Abouleila, Yasmine; Wuelfroth, Petra; van Duinen, Vincent; Stam, Wendy; Jan van Zonneveld, Anton et al. (12 December 2019). "Ebola hemorrhagic shock syndrome-on-a-chip". pp. 100765. doi:10.1016/j.isci.2019.100765. https://www.sciencedirect.com/science/article/pii/S2589004219305103. Retrieved 21 December 2019.
- The article uses public domain text from the CDC as cited.
Bibliography
- Center For Disease Control; Francois Wilson (2014). CDC Guidance on Ebola Virus (EVD): 2014 Edition. International Publications Media Group. ISBN 978-1-63267-011-3. https://books.google.com/books?id=yMQNBQAAQBAJ&pg=PP1.
- Ebola Virus: New Insights for the Healthcare Professional: 2011 Edition: ScholarlyPaper. Scholarly Editions. 2012. ISBN 978-1-4649-1493-5. https://books.google.com/books?id=nLA4W5IjJpwC&pg=PP1.
- Klenk, Hans-Dieter (January 1999). Marburg and Ebola Viruses. Current Topics in Microbiology and Immunology 235. Berlin: Springer-Verlag Telos. ISBN 978-3-540-64729-4.
- Klenk, Hans-Dieter; Feldmann, Heinz (2004) (Limited preview). Ebola and Marburg viruses: molecular and cellular biology. Wymondham, Norfolk, UK: Horizon Bioscience. ISBN 978-0-9545232-3-7. https://books.google.com/?id=EV_mFgnyPoMC.
- Kuhn, Jens H. (2008) (Limited preview). Filoviruses: A Compendium of 40 Years of Epidemiological, Clinical, and Laboratory Studies. Archives of Virology Supplement, vol. 20. Vienna: SpringerWienNewYork. ISBN 978-3-211-20670-6. https://books.google.com/?id=LaOue0F9Ns4C.
- McCormick, Joseph; Fisher-Hoch, Susan (June 1999) [1996] (Limited preview). Level 4: Virus Hunters of the CDC. Horvitz, Leslie Alan (Updated [3rd] ed.). Barnes & Noble. ISBN 978-0-7607-1208-5. https://books.google.com/?id=QEvR3aJX2m0C.
- Pattyn, S. R. (1978) (Full free text). Ebola Virus Haemorrhagic Fever (1st ed.). Amsterdam: Elsevier/North-Holland Biomedical Press. ISBN 978-0-444-80060-2. http://www.itg.be/ebola/.
- Ryabchikova, Elena I.; Price, Barbara B. (2004). Ebola and Marburg Viruses: A View of Infection Using Electron Microscopy. Columbus, Ohio: Battelle Press. ISBN 978-1-57477-131-2.
External links
- Ebola (Ebola Virus Disease) – Centers for Disease Control and Prevention, Viral Special Pathogens Branch
- Health topics: Ebola virus disease – World Health Organization
- Fact Sheet 103 Ebola Virus Disease – World Health Organization, updated 30 May 2019
- Videos: Ebola outbreak response – World Health Organization
- Ebola: What You Need to Know – Scientific American articles related to Ebola; note these are general reading articles, they are not scientific peer-reviewed research articles.
| Classification | |
|---|---|
| External resources |
so:Ebola virus disease
 KSF
KSF