Infection
Topic: Medicine
 From HandWiki - Reading time: 46 min
From HandWiki - Reading time: 46 min
| Infection | |
|---|---|
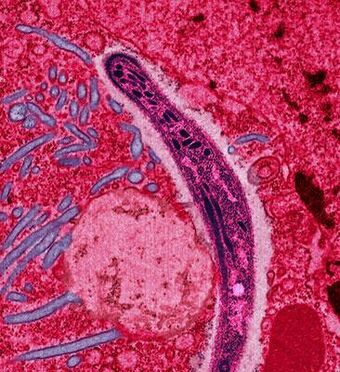 | |
| False-colored electron micrograph showing a malaria sporozoite migrating through the midgut epithelium of a rat | |
| Specialty | Infectious diseases |
| Causes | bacterial, viral, parasitic, fungal, prion |
An infection is the invasion of tissues by pathogens, their multiplication, and the reaction of host tissues to the infectious agent and the toxins they produce.[1] An infectious disease, also known as a transmissible disease or communicable disease, is an illness resulting from an infection.
Infections can be caused by a wide range of pathogens, most prominently bacteria and viruses.[2] Hosts can fight infections using their immune systems. Mammalian hosts react to infections with an innate response, often involving inflammation, followed by an adaptive response.
Specific medications used to treat infections include antibiotics, antivirals, antifungals, antiprotozoals,[3] and antihelminthics. Infectious diseases resulted in 9.2 million deaths in 2013 (about 17% of all deaths).[4] The branch of medicine that focuses on infections is referred to as infectious diseases.[5]
Types
Infections are caused by infectious agents (pathogens) including:
- Bacteria (e.g. Mycobacterium tuberculosis, Staphylococcus aureus, Escherichia coli, Clostridium botulinum, and Salmonella spp.)
- Viruses and related agents such as viroids. (E.g. HIV, Rhinovirus, Lyssaviruses such as Rabies virus, Ebolavirus and Severe acute respiratory syndrome coronavirus 2)
- Fungi, further subclassified into:
- Ascomycota, including yeasts such as Candida (the most common fungal infection); filamentous fungi such as Aspergillus; Pneumocystis species; and dermatophytes, a group of organisms causing infection of skin and other superficial structures in humans.[6]
- Basidiomycota, including the human-pathogenic genus Cryptococcus.[7]
- Parasites, which are usually divided into:[8]
- Unicellular organisms (e.g. malaria, Toxoplasma, Babesia)
- Macroparasites[9] (worms or helminths) including nematodes such as parasitic roundworms and pinworms, tapeworms (cestodes), and flukes (trematodes, such as schistosomes). Diseases caused by helminths are sometimes termed infestations, but are sometimes called infections.
- Arthropods such as ticks, mites, fleas, and lice, can also cause human disease, which conceptually are similar to infections, but invasion of a human or animal body by these macroparasites is usually termed infestation.
- Prions (although they do not secrete toxins)
Signs and symptoms
The signs and symptoms of an infection depend on the type of disease. Some signs of infection affect the whole body generally, such as fatigue, loss of appetite, weight loss, fevers, night sweats, chills, aches and pains. Others are specific to individual body parts, such as skin rashes, coughing, or a runny nose.[10]
In certain cases, infectious diseases may be asymptomatic for much or even all of their course in a given host. In the latter case, the disease may only be defined as a "disease" (which by definition means an illness) in hosts who secondarily become ill after contact with an asymptomatic carrier. An infection is not synonymous with an infectious disease, as some infections do not cause illness in a host.[11]
Bacterial or viral
As bacterial and viral infections can both cause the same kinds of symptoms, it can be difficult to distinguish which is the cause of a specific infection.[12] Distinguishing the two is important, since viral infections cannot be cured by antibiotics whereas bacterial infections can.[13]
| Characteristic | Viral infection | Bacterial infection |
|---|---|---|
| Typical symptoms | In general, viral infections are systemic. This means they involve many different parts of the body or more than one body system at the same time; i.e. a runny nose, sinus congestion, cough, body aches etc. They can be local at times as in viral conjunctivitis or "pink eye" and herpes. Only a few viral infections are painful, like herpes. The pain of viral infections is often described as itchy or burning.[12] | The classic symptoms of a bacterial infection are localized redness, heat, swelling and pain. One of the hallmarks of a bacterial infection is local pain, pain that is in a specific part of the body. For example, if a cut occurs and is infected with bacteria, pain occurs at the site of the infection. Bacterial throat pain is often characterized by more pain on one side of the throat. An ear infection is more likely to be diagnosed as bacterial if the pain occurs in only one ear.[12] A cut that produces pus and milky-colored liquid is most likely infected.[14] |
| Cause | Pathogenic viruses | Pathogenic bacteria |
Pathophysiology
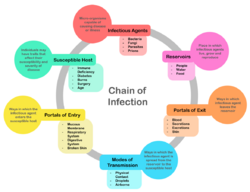
There is a general chain of events that applies to infections, sometimes called the chain of infection[15] or transmission chain. The chain of events involves several steps – which include the infectious agent, reservoir, entering a susceptible host, exit and transmission to new hosts. Each of the links must be present in a chronological order for an infection to develop. Understanding these steps helps health care workers target the infection and prevent it from occurring in the first place.[16]
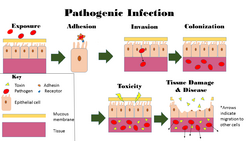
Colonization

Infection begins when an organism successfully enters the body, grows and multiplies. This is referred to as colonization. Most humans are not easily infected. Those with compromised or weakened immune systems have an increased susceptibility to chronic or persistent infections. Individuals who have a suppressed immune system are particularly susceptible to opportunistic infections. Entrance to the host at host–pathogen interface, generally occurs through the mucosa in orifices like the oral cavity, nose, eyes, genitalia, anus, or the microbe can enter through open wounds. While a few organisms can grow at the initial site of entry, many migrate and cause systemic infection in different organs. Some pathogens grow within the host cells (intracellular) whereas others grow freely in bodily fluids.[17]
Wound colonization refers to non-replicating microorganisms within the wound, while in infected wounds, replicating organisms exist and tissue is injured.[18] All multicellular organisms are colonized to some degree by extrinsic organisms, and the vast majority of these exist in either a mutualistic or commensal relationship with the host. An example of the former is the anaerobic bacteria species, which colonizes the mammalian colon, and an example of the latter are the various species of staphylococcus that exist on human skin. Neither of these colonizations are considered infections. The difference between an infection and a colonization is often only a matter of circumstance. Non-pathogenic organisms can become pathogenic given specific conditions, and even the most virulent organism requires certain circumstances to cause a compromising infection. Some colonizing bacteria, such as Corynebacteria sp. and Viridans streptococci, prevent the adhesion and colonization of pathogenic bacteria and thus have a symbiotic relationship with the host, preventing infection and speeding wound healing.
The variables involved in the outcome of a host becoming inoculated by a pathogen and the ultimate outcome include:
- the route of entry of the pathogen and the access to host regions that it gains
- the intrinsic virulence of the particular organism
- the quantity or load of the initial inoculant
- the immune status of the host being colonized
As an example, several staphylococcal species remain harmless on the skin, but, when present in a normally sterile space, such as in the capsule of a joint or the peritoneum, multiply without resistance and cause harm.[22]
An interesting fact that gas chromatography–mass spectrometry, 16S ribosomal RNA analysis, omics, and other advanced technologies have made more apparent to humans in recent decades is that microbial colonization is very common even in environments that humans think of as being nearly sterile. Because it is normal to have bacterial colonization, it is difficult to know which chronic wounds can be classified as infected and how much risk of progression exists. Despite the huge number of wounds seen in clinical practice, there are limited quality data for evaluated symptoms and signs. A review of chronic wounds in the Journal of the American Medical Association's "Rational Clinical Examination Series" quantified the importance of increased pain as an indicator of infection.[23] The review showed that the most useful finding is an increase in the level of pain [likelihood ratio (LR) range, 11–20] makes infection much more likely, but the absence of pain (negative likelihood ratio range, 0.64–0.88) does not rule out infection (summary LR 0.64–0.88).
Disease
Disease can arise if the host's protective immune mechanisms are compromised and the organism inflicts damage on the host. Microorganisms can cause tissue damage by releasing a variety of toxins or destructive enzymes. For example, Clostridium tetani releases a toxin that paralyzes muscles, and staphylococcus releases toxins that produce shock and sepsis. Not all infectious agents cause disease in all hosts. For example, less than 5% of individuals infected with polio develop disease.[24] On the other hand, some infectious agents are highly virulent. The prion causing mad cow disease and Creutzfeldt–Jakob disease invariably kills all animals and people that are infected.[25]
Persistent infections occur because the body is unable to clear the organism after the initial infection. Persistent infections are characterized by the continual presence of the infectious organism, often as latent infection with occasional recurrent relapses of active infection. There are some viruses that can maintain a persistent infection by infecting different cells of the body. Some viruses once acquired never leave the body. A typical example is the herpes virus, which tends to hide in nerves and become reactivated when specific circumstances arise.[26]
Persistent infections cause millions of deaths globally each year.[27] Chronic infections by parasites account for a high morbidity and mortality in many underdeveloped countries.[28][29]
Transmission

For infecting organisms to survive and repeat the infection cycle in other hosts, they (or their progeny) must leave an existing reservoir and cause infection elsewhere. Infection transmission can take place via many potential routes:[30]
- Droplet contact, also known as the respiratory route, and the resultant infection can be termed airborne disease. If an infected person coughs or sneezes on another person the microorganisms, suspended in warm, moist droplets, may enter the body through the nose, mouth or eye surfaces.
- Fecal-oral transmission, wherein foodstuffs or water become contaminated (by people not washing their hands before preparing food, or untreated sewage being released into a drinking water supply) and the people who eat and drink them become infected. Common fecal-oral transmitted pathogens include Vibrio cholerae, Giardia species, rotaviruses, Entamoeba histolytica, Escherichia coli, and tape worms.[31] Most of these pathogens cause gastroenteritis.
- Sexual transmission, with the result being called sexually transmitted infection.
- Oral transmission, diseases that are transmitted primarily by oral means may be caught through direct oral contact such as kissing, or by indirect contact such as by sharing a drinking glass or a cigarette.
- Transmission by direct contact, Some diseases that are transmissible by direct contact include athlete's foot, impetigo and warts.
- Vehicle transmission, transmission by an inanimate reservoir (food, water, soil).[32]
- Vertical transmission, directly from the mother to an embryo, fetus or baby during pregnancy or childbirth. It can occur as a result of a pre-existing infection or one acquired during pregnancy.
- Iatrogenic transmission, due to medical procedures such as injection or transplantation of infected material.
- Vector-borne transmission, transmitted by a vector, which is an organism that does not cause disease itself but that transmits infection by conveying pathogens from one host to another.[33]
The relationship between virulence versus transmissibility is complex; with studies have shown that there were no clear relationship between the two.[34][35] There is still a small number of evidence that partially suggests a link between virulence and transmissibility.[36][37][38]
Diagnosis
Diagnosis of infectious disease sometimes involves identifying an infectious agent either directly or indirectly.[39] In practice most minor infectious diseases such as warts, cutaneous abscesses, respiratory system infections and diarrheal diseases are diagnosed by their clinical presentation and treated without knowledge of the specific causative agent. Conclusions about the cause of the disease are based upon the likelihood that a patient came in contact with a particular agent, the presence of a microbe in a community, and other epidemiological considerations. Given sufficient effort, all known infectious agents can be specifically identified.[40]
Diagnosis of infectious disease is nearly always initiated by medical history and physical examination. More detailed identification techniques involve the culture of infectious agents isolated from a patient. Culture allows identification of infectious organisms by examining their microscopic features, by detecting the presence of substances produced by pathogens, and by directly identifying an organism by its genotype.[40]
Many infectious organisms are identified without culture and microscopy. This is especially true for viruses, which cannot grow in culture. For some suspected pathogens, doctors may conduct tests that examine a patient's blood or other body fluids for antigens or antibodies that indicate presence of a specific pathogen that the doctor suspects.[40]
Other techniques (such as X-rays, CAT scans, PET scans or NMR) are used to produce images of internal abnormalities resulting from the growth of an infectious agent. The images are useful in detection of, for example, a bone abscess or a spongiform encephalopathy produced by a prion.[41]
The benefits of identification, however, are often greatly outweighed by the cost, as often there is no specific treatment, the cause is obvious, or the outcome of an infection is likely to be benign.[42]
Symptomatic diagnostics
The diagnosis is aided by the presenting symptoms in any individual with an infectious disease, yet it usually needs additional diagnostic techniques to confirm the suspicion. Some signs are specifically characteristic and indicative of a disease and are called pathognomonic signs; but these are rare. Not all infections are symptomatic.[43]
In children the presence of cyanosis, rapid breathing, poor peripheral perfusion, or a petechial rash increases the risk of a serious infection by greater than 5 fold.[44] Other important indicators include parental concern, clinical instinct, and temperature greater than 40 °C.[44]
Microbial culture

Many diagnostic approaches depend on microbiological culture to isolate a pathogen from the appropriate clinical specimen.[45] In a microbial culture, a growth medium is provided for a specific agent. A sample taken from potentially diseased tissue or fluid is then tested for the presence of an infectious agent able to grow within that medium. Many pathogenic bacteria are easily grown on nutrient agar, a form of solid medium that supplies carbohydrates and proteins necessary for growth, along with copious amounts of water. A single bacterium will grow into a visible mound on the surface of the plate called a colony, which may be separated from other colonies or melded together into a "lawn". The size, color, shape and form of a colony is characteristic of the bacterial species, its specific genetic makeup (its strain), and the environment that supports its growth. Other ingredients are often added to the plate to aid in identification. Plates may contain substances that permit the growth of some bacteria and not others, or that change color in response to certain bacteria and not others. Bacteriological plates such as these are commonly used in the clinical identification of infectious bacterium. Microbial culture may also be used in the identification of viruses: the medium, in this case, being cells grown in culture that the virus can infect, and then alter or kill. In the case of viral identification, a region of dead cells results from viral growth, and is called a "plaque". Eukaryotic parasites may also be grown in culture as a means of identifying a particular agent.[46]
In the absence of suitable plate culture techniques, some microbes require culture within live animals. Bacteria such as Mycobacterium leprae and Treponema pallidum can be grown in animals, although serological and microscopic techniques make the use of live animals unnecessary. Viruses are also usually identified using alternatives to growth in culture or animals. Some viruses may be grown in embryonated eggs. Another useful identification method is Xenodiagnosis, or the use of a vector to support the growth of an infectious agent. Chagas disease is the most significant example, because it is difficult to directly demonstrate the presence of the causative agent, Trypanosoma cruzi in a patient, which therefore makes it difficult to definitively make a diagnosis. In this case, xenodiagnosis involves the use of the vector of the Chagas agent T. cruzi, an uninfected triatomine bug, which takes a blood meal from a person suspected of having been infected. The bug is later inspected for growth of T. cruzi within its gut.[47]
Microscopy
Another principal tool in the diagnosis of infectious disease is microscopy.[48] Virtually all of the culture techniques discussed above rely, at some point, on microscopic examination for definitive identification of the infectious agent. Microscopy may be carried out with simple instruments, such as the compound light microscope, or with instruments as complex as an electron microscope. Samples obtained from patients may be viewed directly under the light microscope, and can often rapidly lead to identification. Microscopy is often also used in conjunction with biochemical staining techniques, and can be made exquisitely specific when used in combination with antibody based techniques. For example, the use of antibodies made artificially fluorescent (fluorescently labeled antibodies) can be directed to bind to and identify a specific antigens present on a pathogen. A fluorescence microscope is then used to detect fluorescently labeled antibodies bound to internalized antigens within clinical samples or cultured cells. This technique is especially useful in the diagnosis of viral diseases, where the light microscope is incapable of identifying a virus directly.[49]
Other microscopic procedures may also aid in identifying infectious agents. Almost all cells readily stain with a number of basic dyes due to the electrostatic attraction between negatively charged cellular molecules and the positive charge on the dye. A cell is normally transparent under a microscope, and using a stain increases the contrast of a cell with its background. Staining a cell with a dye such as Giemsa stain or crystal violet allows a microscopist to describe its size, shape, internal and external components and its associations with other cells. The response of bacteria to different staining procedures is used in the taxonomic classification of microbes as well. Two methods, the Gram stain and the acid-fast stain, are the standard approaches used to classify bacteria and to diagnosis of disease. The Gram stain identifies the bacterial groups Bacillota and Actinomycetota, both of which contain many significant human pathogens. The acid-fast staining procedure identifies the Actinomycetota genera Mycobacterium and Nocardia.[50]
Biochemical tests
Biochemical tests used in the identification of infectious agents include the detection of metabolic or enzymatic products characteristic of a particular infectious agent. Since bacteria ferment carbohydrates in patterns characteristic of their genus and species, the detection of fermentation products is commonly used in bacterial identification. Acids, alcohols and gases are usually detected in these tests when bacteria are grown in selective liquid or solid media.[51]
The isolation of enzymes from infected tissue can also provide the basis of a biochemical diagnosis of an infectious disease. For example, humans can make neither RNA replicases nor reverse transcriptase, and the presence of these enzymes are characteristic., of specific types of viral infections. The ability of the viral protein hemagglutinin to bind red blood cells together into a detectable matrix may also be characterized as a biochemical test for viral infection, although strictly speaking hemagglutinin is not an enzyme and has no metabolic function.[52]
Serological methods are highly sensitive, specific and often extremely rapid tests used to identify microorganisms. These tests are based upon the ability of an antibody to bind specifically to an antigen. The antigen, usually a protein or carbohydrate made by an infectious agent, is bound by the antibody. This binding then sets off a chain of events that can be visibly obvious in various ways, dependent upon the test. For example, "Strep throat" is often diagnosed within minutes, and is based on the appearance of antigens made by the causative agent, S. pyogenes, that is retrieved from a patient's throat with a cotton swab. Serological tests, if available, are usually the preferred route of identification, however the tests are costly to develop and the reagents used in the test often require refrigeration. Some serological methods are extremely costly, although when commonly used, such as with the "strep test", they can be inexpensive.[11]
Complex serological techniques have been developed into what are known as immunoassays. Immunoassays can use the basic antibody – antigen binding as the basis to produce an electro-magnetic or particle radiation signal, which can be detected by some form of instrumentation. Signal of unknowns can be compared to that of standards allowing quantitation of the target antigen. To aid in the diagnosis of infectious diseases, immunoassays can detect or measure antigens from either infectious agents or proteins generated by an infected organism in response to a foreign agent. For example, immunoassay A may detect the presence of a surface protein from a virus particle. Immunoassay B on the other hand may detect or measure antibodies produced by an organism's immune system that are made to neutralize and allow the destruction of the virus.
Instrumentation can be used to read extremely small signals created by secondary reactions linked to the antibody – antigen binding. Instrumentation can control sampling, reagent use, reaction times, signal detection, calculation of results, and data management to yield a cost-effective automated process for diagnosis of infectious disease.
PCR-based diagnostics

Technologies based upon the polymerase chain reaction (PCR) method will become nearly ubiquitous gold standards of diagnostics of the near future, for several reasons. First, the catalog of infectious agents has grown to the point that virtually all of the significant infectious agents of the human population have been identified. Second, an infectious agent must grow within the human body to cause disease; essentially it must amplify its own nucleic acids in order to cause a disease. This amplification of nucleic acid in infected tissue offers an opportunity to detect the infectious agent by using PCR. Third, the essential tools for directing PCR, primers, are derived from the genomes of infectious agents, and with time those genomes will be known, if they are not already.[53]
Thus, the technological ability to detect any infectious agent rapidly and specifically are currently available. The only remaining blockades to the use of PCR as a standard tool of diagnosis are in its cost and application, neither of which is insurmountable. The diagnosis of a few diseases will not benefit from the development of PCR methods, such as some of the clostridial diseases (tetanus and botulism). These diseases are fundamentally biological poisonings by relatively small numbers of infectious bacteria that produce extremely potent neurotoxins. A significant proliferation of the infectious agent does not occur, this limits the ability of PCR to detect the presence of any bacteria.[53]
Metagenomic sequencing
Given the wide range of bacterial, viral, fungal, protozoal, and helminthic pathogens that cause debilitating and life-threatening illnesses, the ability to quickly identify the cause of infection is important yet often challenging. For example, more than half of cases of encephalitis, a severe illness affecting the brain, remain undiagnosed, despite extensive testing using the standard of care (microbiological culture) and state-of-the-art clinical laboratory methods. Metagenomic sequencing-based diagnostic tests are currently being developed for clinical use and show promise as a sensitive, specific, and rapid way to diagnose infection using a single all-encompassing test. This test is similar to current PCR tests; however, an untargeted whole genome amplification is used rather than primers for a specific infectious agent. This amplification step is followed by next-generation sequencing or third-generation sequencing, alignment comparisons, and taxonomic classification using large databases of thousands of pathogen and commensal reference genomes. Simultaneously, antimicrobial resistance genes within pathogen and plasmid genomes are sequenced and aligned to the taxonomically classified pathogen genomes to generate an antimicrobial resistance profile – analogous to antibiotic sensitivity testing – to facilitate antimicrobial stewardship and allow for the optimization of treatment using the most effective drugs for a patient's infection.
Metagenomic sequencing could prove especially useful for diagnosis when the patient is immunocompromised. An ever-wider array of infectious agents can cause serious harm to individuals with immunosuppression, so clinical screening must often be broader. Additionally, the expression of symptoms is often atypical, making a clinical diagnosis based on presentation more difficult. Thirdly, diagnostic methods that rely on the detection of antibodies are more likely to fail. A rapid, sensitive, specific, and untargeted test for all known human pathogens that detects the presence of the organism's DNA rather than antibodies is therefore highly desirable.
Indication of tests

There is usually an indication for a specific identification of an infectious agent only when such identification can aid in the treatment or prevention of the disease, or to advance knowledge of the course of an illness prior to the development of effective therapeutic or preventative measures. For example, in the early 1980s, prior to the appearance of AZT for the treatment of AIDS, the course of the disease was closely followed by monitoring the composition of patient blood samples, even though the outcome would not offer the patient any further treatment options. In part, these studies on the appearance of HIV in specific communities permitted the advancement of hypotheses as to the route of transmission of the virus. By understanding how the disease was transmitted, resources could be targeted to the communities at greatest risk in campaigns aimed at reducing the number of new infections. The specific serological diagnostic identification, and later genotypic or molecular identification, of HIV also enabled the development of hypotheses as to the temporal and geographical origins of the virus, as well as a myriad of other hypothesis.[11] The development of molecular diagnostic tools have enabled physicians and researchers to monitor the efficacy of treatment with anti-retroviral drugs. Molecular diagnostics are now commonly used to identify HIV in healthy people long before the onset of illness and have been used to demonstrate the existence of people who are genetically resistant to HIV infection. Thus, while there still is no cure for AIDS, there is great therapeutic and predictive benefit to identifying the virus and monitoring the virus levels within the blood of infected individuals, both for the patient and for the community at large.
Classification
Subclinical versus clinical (latent versus apparent)
Symptomatic infections are apparent and clinical, whereas an infection that is active but does not produce noticeable symptoms may be called inapparent, silent, subclinical, or occult. An infection that is inactive or dormant is called a latent infection.[54] An example of a latent bacterial infection is latent tuberculosis. Some viral infections can also be latent, examples of latent viral infections are any of those from the Herpesviridae family.[55]
The word infection can denote any presence of a particular pathogen at all (no matter how little) but also is often used in a sense implying a clinically apparent infection (in other words, a case of infectious disease). This fact occasionally creates some ambiguity or prompts some usage discussion; to get around this it is common for health professionals to speak of colonization (rather than infection) when they mean that some of the pathogens are present but that no clinically apparent infection (no disease) is present.[56]
Course of infection
Different terms are used to describe how and where infections present over time. In an acute infection, symptoms develop rapidly; its course can either be rapid or protracted. In chronic infection, symptoms usually develop gradually over weeks or months and are slow to resolve.[57] In subacute infections, symptoms take longer to develop than in acute infections but arise more quickly than those of chronic infections. A focal infection is an initial site of infection from which organisms travel via the bloodstream to another area of the body.[58]
Primary versus opportunistic
Among the many varieties of microorganisms, relatively few cause disease in otherwise healthy individuals.[59] Infectious disease results from the interplay between those few pathogens and the defenses of the hosts they infect. The appearance and severity of disease resulting from any pathogen depend upon the ability of that pathogen to damage the host as well as the ability of the host to resist the pathogen. However, a host's immune system can also cause damage to the host itself in an attempt to control the infection. Clinicians, therefore, classify infectious microorganisms or microbes according to the status of host defenses – either as primary pathogens or as opportunistic pathogens.[60]
Primary pathogens
Primary pathogens cause disease as a result of their presence or activity within the normal, healthy host, and their intrinsic virulence (the severity of the disease they cause) is, in part, a necessary consequence of their need to reproduce and spread. Many of the most common primary pathogens of humans only infect humans, however, many serious diseases are caused by organisms acquired from the environment or that infect non-human hosts.[61]
Opportunistic pathogens
Opportunistic pathogens can cause an infectious disease in a host with depressed resistance (immunodeficiency) or if they have unusual access to the inside of the body (for example, via trauma). Opportunistic infection may be caused by microbes ordinarily in contact with the host, such as pathogenic bacteria or fungi in the gastrointestinal or the upper respiratory tract, and they may also result from (otherwise innocuous) microbes acquired from other hosts (as in Clostridium difficile colitis) or from the environment as a result of traumatic introduction (as in surgical wound infections or compound fractures). An opportunistic disease requires impairment of host defenses, which may occur as a result of genetic defects (such as chronic granulomatous disease), exposure to antimicrobial drugs or immunosuppressive chemicals (as might occur following poisoning or cancer chemotherapy), exposure to ionizing radiation, or as a result of an infectious disease with immunosuppressive activity (such as with measles, malaria or HIV disease). Primary pathogens may also cause more severe disease in a host with depressed resistance than would normally occur in an immunosufficient host.[11]
Secondary infection
While a primary infection can practically be viewed as the root cause of an individual's current health problem, a secondary infection is a sequela or complication of that root cause. For example, an infection due to a burn or penetrating trauma (the root cause) is a secondary infection. Primary pathogens often cause primary infection and often cause secondary infection. Usually, opportunistic infections are viewed as secondary infections (because immunodeficiency or injury was the predisposing factor).[60]
Other types of infection
Other types of infection consist of mixed, iatrogenic, nosocomial, and community-acquired infection. A mixed infection is an infection that is caused by two or more pathogens. An example of this is appendicitis, which is caused by Bacteroides fragilis and Escherichia coli. The second is an iatrogenic infection. This type of infection is one that is transmitted from a health care worker to a patient. A nosocomial infection is also one that occurs in a health care setting. Nosocomial infections are those that are acquired during a hospital stay. Lastly, a community-acquired infection is one in which the infection is acquired from a whole community.[58]
Infectious or not
One manner of proving that a given disease is infectious, is to satisfy Koch's postulates (first proposed by Robert Koch), which require that first, the infectious agent be identifiable only in patients who have the disease, and not in healthy controls, and second, that patients who contract the infectious agent also develop the disease. These postulates were first used in the discovery that Mycobacteria species cause tuberculosis.[62]
However, Koch's postulates cannot usually be tested in modern practice for ethical reasons. Proving them would require experimental infection of a healthy individual with a pathogen produced as a pure culture. Conversely, even clearly infectious diseases do not always meet the infectious criteria; for example, Treponema pallidum, the causative spirochete of syphilis, cannot be cultured in vitro – however the organism can be cultured in rabbit testes. It is less clear that a pure culture comes from an animal source serving as host than it is when derived from microbes derived from plate culture.[63]
Epidemiology, or the study and analysis of who, why and where disease occurs, and what determines whether various populations have a disease, is another important tool used to understand infectious disease. Epidemiologists may determine differences among groups within a population, such as whether certain age groups have a greater or lesser rate of infection; whether groups living in different neighborhoods are more likely to be infected; and by other factors, such as gender and race. Researchers also may assess whether a disease outbreak is sporadic, or just an occasional occurrence; endemic, with a steady level of regular cases occurring in a region; epidemic, with a fast arising, and unusually high number of cases in a region; or pandemic, which is a global epidemic. If the cause of the infectious disease is unknown, epidemiology can be used to assist with tracking down the sources of infection.[64]
Contagiousness
Infectious diseases are sometimes called contagious diseases when they are easily transmitted by contact with an ill person or their secretions (e.g., influenza). Thus, a contagious disease is a subset of infectious disease that is especially infective or easily transmitted. Other types of infectious, transmissible, or communicable diseases with more specialized routes of infection, such as vector transmission or sexual transmission, are usually not regarded as "contagious", and often do not require medical isolation (sometimes loosely called quarantine) of those affected. However, this specialized connotation of the word "contagious" and "contagious disease" (easy transmissibility) is not always respected in popular use. Infectious diseases are commonly transmitted from person to person through direct contact. The types of contact are through person to person and droplet spread. Indirect contact such as airborne transmission, contaminated objects, food and drinking water, animal person contact, animal reservoirs, insect bites, and environmental reservoirs are another way infectious diseases are transmitted.[65]
By anatomic location
Infections can be classified by the anatomic location or organ system infected, including:[citation needed]
- Urinary tract infection
- Skin infection
- Respiratory tract infection
- Odontogenic infection (an infection that originates within a tooth or in the closely surrounding tissues)
- Vaginal infections
- Intra-amniotic infection
In addition, locations of inflammation where infection is the most common cause include pneumonia, meningitis and salpingitis.[citation needed]
Prevention

Techniques like hand washing, wearing gowns, and wearing face masks can help prevent infections from being passed from one person to another. Aseptic technique was introduced in medicine and surgery in the late 19th century and greatly reduced the incidence of infections caused by surgery. Frequent hand washing remains the most important defense against the spread of unwanted organisms.[67] There are other forms of prevention such as avoiding the use of illicit drugs, using a condom, wearing gloves, and having a healthy lifestyle with a balanced diet and regular exercise. Cooking foods well and avoiding foods that have been left outside for a long time is also important.[citation needed]
Antimicrobial substances used to prevent transmission of infections include:[citation needed]
- antiseptics, which are applied to living tissue/skin
- disinfectants, which destroy microorganisms found on non-living objects.
- antibiotics, called prophylactic when given as prevention rather as treatment of infection. However, long term use of antibiotics leads to resistance of bacteria. While humans do not become immune to antibiotics, the bacteria does. Thus, avoiding using antibiotics longer than necessary helps preventing bacteria from forming mutations that aide in antibiotic resistance.
One of the ways to prevent or slow down the transmission of infectious diseases is to recognize the different characteristics of various diseases.[68] Some critical disease characteristics that should be evaluated include virulence, distance traveled by those affected, and level of contagiousness. The human strains of Ebola virus, for example, incapacitate those infected extremely quickly and kill them soon after. As a result, those affected by this disease do not have the opportunity to travel very far from the initial infection zone.[69] Also, this virus must spread through skin lesions or permeable membranes such as the eye. Thus, the initial stage of Ebola is not very contagious since its victims experience only internal hemorrhaging. As a result of the above features, the spread of Ebola is very rapid and usually stays within a relatively confined geographical area. In contrast, the human immunodeficiency virus (HIV) kills its victims very slowly by attacking their immune system.[11] As a result, many of its victims transmit the virus to other individuals before even realizing that they are carrying the disease. Also, the relatively low virulence allows its victims to travel long distances, increasing the likelihood of an epidemic.[citation needed]
Another effective way to decrease the transmission rate of infectious diseases is to recognize the effects of small-world networks.[68] In epidemics, there are often extensive interactions within hubs or groups of infected individuals and other interactions within discrete hubs of susceptible individuals. Despite the low interaction between discrete hubs, the disease can jump and spread in a susceptible hub via a single or few interactions with an infected hub. Thus, infection rates in small-world networks can be reduced somewhat if interactions between individuals within infected hubs are eliminated (Figure 1). However, infection rates can be drastically reduced if the main focus is on the prevention of transmission jumps between hubs. The use of needle exchange programs in areas with a high density of drug users with HIV is an example of the successful implementation of this treatment method.[70] Another example is the use of ring culling or vaccination of potentially susceptible livestock in adjacent farms to prevent the spread of the foot-and-mouth virus in 2001.[71]
A general method to prevent transmission of vector-borne pathogens is pest control.
In cases where infection is merely suspected, individuals may be quarantined until the incubation period has passed and the disease manifests itself or the person remains healthy. Groups may undergo quarantine, or in the case of communities, a cordon sanitaire may be imposed to prevent infection from spreading beyond the community, or in the case of protective sequestration, into a community. Public health authorities may implement other forms of social distancing, such as school closings, lockdowns or temporary restrictions (e.g. circuit breakers)[72] to control an epidemic.
Immunity

Infection with most pathogens does not result in death of the host and the offending organism is ultimately cleared after the symptoms of the disease have waned.[59] This process requires immune mechanisms to kill or inactivate the inoculum of the pathogen. Specific acquired immunity against infectious diseases may be mediated by antibodies and/or T lymphocytes. Immunity mediated by these two factors may be manifested by:
- a direct effect upon a pathogen, such as antibody-initiated complement-dependent bacteriolysis, opsonoization, phagocytosis and killing, as occurs for some bacteria,
- neutralization of viruses so that these organisms cannot enter cells,
- or by T lymphocytes, which will kill a cell parasitized by a microorganism.
The immune system response to a microorganism often causes symptoms such as a high fever and inflammation, and has the potential to be more devastating than direct damage caused by a microbe.[11]
Resistance to infection (immunity) may be acquired following a disease, by asymptomatic carriage of the pathogen, by harboring an organism with a similar structure (crossreacting), or by vaccination. Knowledge of the protective antigens and specific acquired host immune factors is more complete for primary pathogens than for opportunistic pathogens. There is also the phenomenon of herd immunity which offers a measure of protection to those otherwise vulnerable people when a large enough proportion of the population has acquired immunity from certain infections.[73]
Immune resistance to an infectious disease requires a critical level of either antigen-specific antibodies and/or T cells when the host encounters the pathogen. Some individuals develop natural serum antibodies to the surface polysaccharides of some agents although they have had little or no contact with the agent, these natural antibodies confer specific protection to adults and are passively transmitted to newborns.
Host genetic factors
The organism that is the target of an infecting action of a specific infectious agent is called the host. The host harbouring an agent that is in a mature or sexually active stage phase is called the definitive host. The intermediate host comes in contact during the larvae stage. A host can be anything living and can attain to asexual and sexual reproduction.[74] The clearance of the pathogens, either treatment-induced or spontaneous, it can be influenced by the genetic variants carried by the individual patients. For instance, for genotype 1 hepatitis C treated with Pegylated interferon-alpha-2a or Pegylated interferon-alpha-2b (brand names Pegasys or PEG-Intron) combined with ribavirin, it has been shown that genetic polymorphisms near the human IL28B gene, encoding interferon lambda 3, are associated with significant differences in the treatment-induced clearance of the virus. This finding, originally reported in Nature,[75] showed that genotype 1 hepatitis C patients carrying certain genetic variant alleles near the IL28B gene are more possibly to achieve sustained virological response after the treatment than others. Later report from Nature[76] demonstrated that the same genetic variants are also associated with the natural clearance of the genotype 1 hepatitis C virus.
Treatments
When infection attacks the body, anti-infective drugs can suppress the infection. Several broad types of anti-infective drugs exist, depending on the type of organism targeted; they include antibacterial (antibiotic; including antitubercular), antiviral, antifungal and antiparasitic (including antiprotozoal and antihelminthic) agents. Depending on the severity and the type of infection, the antibiotic may be given by mouth or by injection, or may be applied topically. Severe infections of the brain are usually treated with intravenous antibiotics. Sometimes, multiple antibiotics are used in case there is resistance to one antibiotic. Antibiotics only work for bacteria and do not affect viruses. Antibiotics work by slowing down the multiplication of bacteria or killing the bacteria. The most common classes of antibiotics used in medicine include penicillin, cephalosporins, aminoglycosides, macrolides, quinolones and tetracyclines.[77][78]
Not all infections require treatment, and for many self-limiting infections the treatment may cause more side-effects than benefits. Antimicrobial stewardship is the concept that healthcare providers should treat an infection with an antimicrobial that specifically works well for the target pathogen for the shortest amount of time and to only treat when there is a known or highly suspected pathogen that will respond to the medication.[79]
Susceptibility to infection
Pandemics such as COVID-19 show that people dramatically differ in their susceptibility to infection. This may be because of general health, age, or their immune status, e.g. when they have been infected previously. However, it also has become clear that there are genetic factor which determine susceptibility to infection. For instance, up to 40% of SARS-CoV-2 infections may be asymptomatic, suggesting that many people are naturally protected from disease.[80] Large genetic studies have defined risk factors for severe SARS-CoV-2 infections, and genome sequences from 659 patients with severe COVID-19 revealed genetic variants that appear to be associated with life-threatening disease. One gene identified in these studies is type I interferon (IFN). Autoantibodies against type I IFNs were found in up to 13.7% of patients with life-threatening COVID-19, indicating that a complex interaction between genetics and the immune system is important for natural resistance to Covid.[81]
Similarly, mutations in the ERAP2 gene, encoding endoplasmic reticulum aminopeptidase 2, seem to increase the susceptibility to the plague, the disease caused by an infection with the bacteria Yersinia pestis. People who inherited two copies of a complete variant of the gene were twice as likely to have survived the plague as those who inherited two copies of a truncated variant.[82]
Susceptibility also determined the epidemiology of infection, given that different populations have different genetic and environmental conditions that affect infections.
Epidemiology
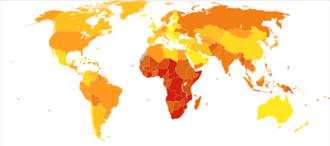
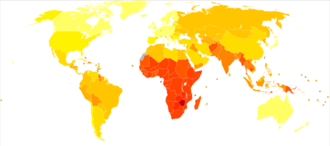
- no data
- ≤250
- 250–500
- 500–1000
- 1000–2000
- 2000–3000
- 3000–4000
- 4000–5000
- 5000–6250
- 6250–12,500
- 12,500–25,000
- 25,000–50,000
- ≥50,000
In 2010, about 10 million people died of infectious diseases.[84]
The World Health Organization collects information on global deaths by International Classification of Disease (ICD) code categories. The following table lists the top infectious disease by number of deaths in 2002. 1993 data is included for comparison.
| Rank | Cause of death | Deaths 2002 (in millions) |
Percentage of all deaths |
Deaths 1993 (in millions) |
1993 Rank |
|---|---|---|---|---|---|
| N/A | All infectious diseases | 14.7 | 25.9% | 16.4 | 32.2% |
| 1 | Lower respiratory infections[87] | 3.9 | 6.9% | 4.1 | 1 |
| 2 | HIV/AIDS | 2.8 | 4.9% | 0.7 | 7 |
| 3 | Diarrheal diseases[88] | 1.8 | 3.2% | 3.0 | 2 |
| 4 | Tuberculosis (TB) | 1.6 | 2.7% | 2.7 | 3 |
| 5 | Malaria | 1.3 | 2.2% | 2.0 | 4 |
| 6 | Measles | 0.6 | 1.1% | 1.1 | 5 |
| 7 | Pertussis | 0.29 | 0.5% | 0.36 | 7 |
| 8 | Tetanus | 0.21 | 0.4% | 0.15 | 12 |
| 9 | Meningitis | 0.17 | 0.3% | 0.25 | 8 |
| 10 | Syphilis | 0.16 | 0.3% | 0.19 | 11 |
| 11 | Hepatitis B | 0.10 | 0.2% | 0.93 | 6 |
| 12–17 | Tropical diseases (6)[89] | 0.13 | 0.2% | 0.53 | 9, 10, 16–18 |
| Note: Other causes of death include maternal and perinatal conditions (5.2%), nutritional deficiencies (0.9%), noncommunicable conditions (58.8%), and injuries (9.1%). | |||||
The top three single agent/disease killers are HIV/AIDS, TB and malaria. While the number of deaths due to nearly every disease have decreased, deaths due to HIV/AIDS have increased fourfold. Childhood diseases include pertussis, poliomyelitis, diphtheria, measles and tetanus. Children also make up a large percentage of lower respiratory and diarrheal deaths. In 2012, approximately 3.1 million people have died due to lower respiratory infections, making it the number 4 leading cause of death in the world.[90]
Historic pandemics
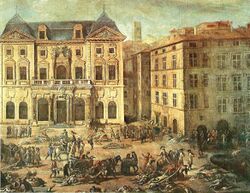
With their potential for unpredictable and explosive impacts, infectious diseases have been major actors in human history.[91] A pandemic (or global epidemic) is a disease that affects people over an extensive geographical area. For example:
- Plague of Justinian, from 541 to 542, killed between 50% and 60% of Europe's population.[92]
- The Black Death of 1347 to 1352 killed 25 million in Europe over five years. The plague reduced the old world population from an estimated 450 million to between 350 and 375 million in the 14th century.
- The introduction of smallpox, measles, and typhus to the areas of Central and South America by European explorers during the 15th and 16th centuries caused pandemics among the native inhabitants. Between 1518 and 1568 disease pandemics are said to have caused the population of Mexico to fall from 20 million to 3 million.[93]
- The first European influenza epidemic occurred between 1556 and 1560, with an estimated mortality rate of 20%.[93]
- Smallpox killed an estimated 60 million Europeans during the 18th century[94] (approximately 400,000 per year).[95] Up to 30% of those infected, including 80% of the children under 5 years of age, died from the disease, and one-third of the survivors went blind.[96]
- In the 19th century, tuberculosis killed an estimated one-quarter of the adult population of Europe;[97] by 1918 one in six deaths in France were still caused by TB.
- The Influenza Pandemic of 1918 (or the Spanish flu) killed 25–50 million people (about 2% of world population of 1.7 billion).[98] Today Influenza kills about 250,000 to 500,000 worldwide each year.
Emerging diseases
In most cases, microorganisms live in harmony with their hosts via mutual or commensal interactions. Diseases can emerge when existing parasites become pathogenic or when new pathogenic parasites enter a new host.
- Coevolution between parasite and host can lead to hosts becoming resistant to the parasites or the parasites may evolve greater virulence, leading to immunopathological disease.
- Human activity is involved with many emerging infectious diseases, such as environmental change enabling a parasite to occupy new niches. When that happens, a pathogen that had been confined to a remote habitat has a wider distribution and possibly a new host organism. Parasites jumping from nonhuman to human hosts are known as zoonoses. Under disease invasion, when a parasite invades a new host species, it may become pathogenic in the new host.[99]
Several human activities have led to the emergence of zoonotic human pathogens, including viruses, bacteria, protozoa, and rickettsia,[100] and spread of vector-borne diseases,[99] see also globalization and disease and wildlife disease:
- Encroachment on wildlife habitats. The construction of new villages and housing developments in rural areas force animals to live in dense populations, creating opportunities for microbes to mutate and emerge.[101]
- Changes in agriculture. The introduction of new crops attracts new crop pests and the microbes they carry to farming communities, exposing people to unfamiliar diseases.
- The destruction of rain forests. As countries make use of their rain forests, by building roads through forests and clearing areas for settlement or commercial ventures, people encounter insects and other animals harboring previously unknown microorganisms.
- Uncontrolled urbanization. The rapid growth of cities in many developing countries tends to concentrate large numbers of people into crowded areas with poor sanitation. These conditions foster transmission of contagious diseases.
- Modern transport. Ships and other cargo carriers often harbor unintended "passengers", that can spread diseases to faraway destinations. While with international jet-airplane travel, people infected with a disease can carry it to distant lands, or home to their families, before their first symptoms appear.
Germ theory of disease
In Antiquity, the Ancient Greece historian Thucydides (c. 460 – c. 400 BCE) was the first person to write, in his account of the plague of Athens, that diseases could spread from an infected person to others.[102][103] In his On the Different Types of Fever (c. 175 AD), the Greco-Roman physician Galen speculated that plagues were spread by "certain seeds of plague", which were present in the air.[104] In the Sushruta Samhita, the ancient Indian physician Sushruta theorized: "Leprosy, fever, consumption, diseases of the eye, and other infectious diseases spread from one person to another by sexual union, physical contact, eating together, sleeping together, sitting together, and the use of same clothes, garlands and pastes."[105][106] This book has been dated to about the sixth century BC.[107]
A basic form of contagion theory was proposed by Persian physician Ibn Sina (known as Avicenna in Europe) in The Canon of Medicine (1025), which later became the most authoritative medical textbook in Europe up until the 16th century. In Book IV of the Canon, Ibn Sina discussed epidemics, outlining the classical miasma theory and attempting to blend it with his own early contagion theory. He mentioned that people can transmit disease to others by breath, noted contagion with tuberculosis, and discussed the transmission of disease through water and dirt.[108] The concept of invisible contagion was later discussed by several Islamic scholars in the Ayyubid Sultanate who referred to them as najasat ("impure substances"). The fiqh scholar Ibn al-Haj al-Abdari (c. 1250–1336), while discussing Islamic diet and hygiene, gave warnings about how contagion can contaminate water, food, and garments, and could spread through the water supply, and may have implied contagion to be unseen particles.[109]
When the Black Death bubonic plague reached Al-Andalus in the 14th century, the Arab physicians Ibn Khatima (c. 1369) and Ibn al-Khatib (1313–1374) hypothesised that infectious diseases were caused by "minute bodies" and described how they can be transmitted through garments, vessels and earrings.[110] Ideas of contagion became more popular in Europe during the Renaissance, particularly through the writing of the Italian physician Girolamo Fracastoro.[111] Anton van Leeuwenhoek (1632–1723) advanced the science of microscopy by being the first to observe microorganisms, allowing for easy visualization of bacteria.
In the mid-19th century John Snow and William Budd did important work demonstrating the contagiousness of typhoid and cholera through contaminated water. Both are credited with decreasing epidemics of cholera in their towns by implementing measures to prevent contamination of water.[112] Louis Pasteur proved beyond doubt that certain diseases are caused by infectious agents, and developed a vaccine for rabies. Robert Koch provided the study of infectious diseases with a scientific basis known as Koch's postulates. Edward Jenner, Jonas Salk and Albert Sabin developed effective vaccines for smallpox and polio, which would later result in the eradication and near-eradication of these diseases, respectively. Alexander Fleming discovered the world's first antibiotic, penicillin, which Florey and Chain then developed. Gerhard Domagk developed sulphonamides, the first broad spectrum synthetic antibacterial drugs.[citation needed]
Medical specialists
The medical treatment of infectious diseases falls into the medical field of Infectious Disease and in some cases the study of propagation pertains to the field of Epidemiology. Generally, infections are initially diagnosed by primary care physicians or internal medicine specialists. For example, an "uncomplicated" pneumonia will generally be treated by the internist or the pulmonologist (lung physician). The work of the infectious diseases specialist therefore entails working with both patients and general practitioners, as well as laboratory scientists, immunologists, bacteriologists and other specialists.[citation needed]
An infectious disease team may be alerted when:[citation needed]
- The disease has not been definitively diagnosed after an initial workup
- The patient is immunocompromised (for example, in AIDS or after chemotherapy);
- The infectious agent is of an uncommon nature (e.g. tropical diseases);
- The disease has not responded to first line antibiotics;
- The disease might be dangerous to other patients, and the patient might have to be isolated
Society and culture
Several studies have reported associations between pathogen load in an area and human behavior. Higher pathogen load is associated with decreased size of ethnic and religious groups in an area. This may be due high pathogen load favoring avoidance of other groups, which may reduce pathogen transmission, or a high pathogen load preventing the creation of large settlements and armies that enforce a common culture. Higher pathogen load is also associated with more restricted sexual behavior, which may reduce pathogen transmission. It also associated with higher preferences for health and attractiveness in mates. Higher fertility rates and shorter or less parental care per child is another association that may be a compensation for the higher mortality rate. There is also an association with polygyny which may be due to higher pathogen load, making selecting males with a high genetic resistance increasingly important. Higher pathogen load is also associated with more collectivism and less individualism, which may limit contacts with outside groups and infections. There are alternative explanations for at least some of the associations although some of these explanations may in turn ultimately be due to pathogen load. Thus, polygyny may also be due to a lower male: female ratio in these areas but this may ultimately be due to male infants having increased mortality from infectious diseases. Another example is that poor socioeconomic factors may ultimately in part be due to high pathogen load preventing economic development.[113]
Fossil record

Evidence of infection in fossil remains is a subject of interest for paleopathologists, scientists who study occurrences of injuries and illness in extinct life forms. Signs of infection have been discovered in the bones of carnivorous dinosaurs. When present, however, these infections seem to tend to be confined to only small regions of the body. A skull attributed to the early carnivorous dinosaur Herrerasaurus ischigualastensis exhibits pit-like wounds surrounded by swollen and porous bone. The unusual texture of the bone around the wounds suggests they were affected by a short-lived, non-lethal infection. Scientists who studied the skull speculated that the bite marks were received in a fight with another Herrerasaurus. Other carnivorous dinosaurs with documented evidence of infection include Acrocanthosaurus, Allosaurus, Tyrannosaurus and a tyrannosaur from the Kirtland Formation. The infections from both tyrannosaurs were received by being bitten during a fight, like the Herrerasaurus specimen.[114]
Outer space
A 2006 Space Shuttle experiment found that Salmonella typhimurium, a bacterium that can cause food poisoning, became more virulent when cultivated in space.[115] On April 29, 2013, scientists in Rensselaer Polytechnic Institute, funded by NASA, reported that, during spaceflight on the International Space Station, microbes seem to adapt to the space environment in ways "not observed on Earth" and in ways that "can lead to increases in growth and virulence".[116] More recently, in 2017, bacteria were found to be more resistant to antibiotics and to thrive in the near-weightlessness of space.[117] Microorganisms have been observed to survive the vacuum of outer space.[118][119]
See also
- Biological hazard
- Blood-borne disease
- Coinfection
- Copenhagen Consensus
- Cordon sanitaire
- Epidemiological transition
- Foodborne illness
- Hospital-acquired infection
- Eradication of infectious diseases
- Infection control
- Isolation (health care)
- List of causes of death by rate
- List of diseases caused by insects
- List of infectious diseases
- Mathematical modelling of infectious disease
- Multiplicity of infection
- Neglected tropical diseases
- Sentinel surveillance
- Spillover infection
- Threshold host density
- Transmission
- Vaccine-preventable diseases
- Waterborne diseases
References
- ↑ "infection", The Free Dictionary, https://medical-dictionary.thefreedictionary.com/infection, retrieved 2023-11-17
- ↑ Sehgal, Mukul; Ladd, Hugh J.; Totapally, Balagangadhar (2020-12-01). "Trends in Epidemiology and Microbiology of Severe Sepsis and Septic Shock in Children" (in en). Hospital Pediatrics 10 (12): 1021–1030. doi:10.1542/hpeds.2020-0174. ISSN 2154-1663. PMID 33208389. https://hosppeds.aappublications.org/content/10/12/1021. Retrieved 2021-03-26.
- ↑ "Antiprotozoal Drugs". https://medical-dictionary.thefreedictionary.com/Antiprotozoal+Drugs.
- ↑ ((GBD 2013 Mortality and Causes of Death Collaborators)) (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study". Lancet 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMID 25530442.
- ↑ "Infectious Disease, Internal Medicine". Association of American Medical Colleges. https://www.aamc.org/cim/specialty/list/us/339608/infectious_disease_-internal_medicine.html. "Infectious disease is the subspecialty of internal medicine dealing with the diagnosis and treatment of communicable diseases of all types, in all organs, and in all ages of patients."
- ↑ "Types of Fungal Diseases" (in en-us). 2019-06-27. https://www.cdc.gov/fungal/diseases/index.html.
- ↑ Mada, Pradeep Kumar; Jamil, Radia T.; Alam, Mohammed U. (2019), "Cryptococcus (Cryptococcosis)", StatPearls (StatPearls Publishing), PMID 28613714, http://www.ncbi.nlm.nih.gov/books/NBK431060/, retrieved 2019-12-09
- ↑ "About Parasites" (in en-us). 2019-02-25. https://www.cdc.gov/parasites/about.html.
- ↑ Brown, Peter J. (1987). "Microparasites and Macroparasites". Cultural Anthropology 2 (1): 155–71. doi:10.1525/can.1987.2.1.02a00120.
- ↑ "Runny Nose: Symptoms, Causes & Treatment". https://my.clevelandclinic.org/health/symptoms/17660-runny-nose.
- ↑ 11.0 11.1 11.2 11.3 11.4 11.5 Sherris Medical Microbiology (4th ed.). McGraw Hill. 2004. ISBN 978-0-8385-8529-0.
- ↑ 12.0 12.1 12.2 "NIPA - Bacteria - Bacterial vs. Viral infections". http://www.antibiotics-info.org/bact02.html.
- ↑ Robert N. Golden; Fred Peterson (2009). The Truth About Illness and Disease. Infobase Publishing. p. 181. ISBN 978-1438126371.
- ↑ "Infection". Rencare. http://www.rencareltd.com/conditions/infections/.
- ↑ "Infection Cycle Symptoms and Treatment" (in en-US). https://infectioncycle.com/.
- ↑ ((National Institutes of Health (US))); Study, Biological Sciences Curriculum (2007), "Understanding Emerging and Re-emerging Infectious Diseases" (in en), NIH Curriculum Supplement Series [Internet] (National Institutes of Health (US)), https://www.ncbi.nlm.nih.gov/books/NBK20370/, retrieved 2023-11-17
- ↑ Peterson, Johnny W. (1996) (in en). Bacterial Pathogenesis. University of Texas Medical Branch at Galveston. ISBN 9780963117212. https://www.ncbi.nlm.nih.gov/books/NBK8526/. Retrieved 2022-10-20.
- ↑ Negut, Irina; Grumezescu, Valentina; Grumezescu, Alexandru Mihai (2018-09-18). "Treatment Strategies for Infected Wounds". Molecules 23 (9): 2392. doi:10.3390/molecules23092392. ISSN 1420-3049. PMID 30231567.
- ↑ Duerkop, Breck A; Hooper, Lora V (2013-07-01). "Resident viruses and their interactions with the immune system" (in en). Nature Immunology 14 (7): 654–59. doi:10.1038/ni.2614. PMID 23778792.
- ↑ "Bacterial Pathogenesis at Washington University". St. Louis. https://www.studyblue.com/notes/note/n/bacterial-pathogenesis/deck/11094651.
- ↑ "Print Friendly". http://www.lifeextension.com/magazine/2014/6/the-dangers-of-using-antibiotics-to-prevent-urinary-tract-infections/page-01?p=1.
- ↑ Tong, Steven Y. C.; Davis, Joshua S.; Eichenberger, Emily; Holland, Thomas L.; Fowler, Vance G. (2015). "Staphylococcus aureus Infections: Epidemiology, Pathophysiology, Clinical Manifestations, and Management". Clinical Microbiology Reviews 28 (3): 603–661. doi:10.1128/CMR.00134-14. ISSN 0893-8512. PMID 26016486.
- ↑ "Does this patient have an infection of a chronic wound?". JAMA 307 (6): 605–11. Feb 2012. doi:10.1001/jama.2012.98. PMID 22318282.
- ↑ "Polio: Questions and Answers". http://www.immunize.org/catg.d/p4215.pdf.
- ↑ Trent, Ronald J (2005). "Infectious Diseases". Molecular Medicine: 193–220. doi:10.1016/B978-012699057-7/50008-4. ISBN 9780126990577.
- ↑ Rouse, Barry T.; Sehrawat, Sharvan (2010). "Immunity and immunopathology to viruses: what decides the outcome?" (in en). Nature Reviews Immunology 10 (7): 514–526. doi:10.1038/nri2802. ISSN 1474-1741. PMID 20577268.
- ↑ "Chronic Infection Information". http://www.persistentinfection.net/.
- ↑ Torgerson, Paul R.; Devleesschauwer, Brecht; Praet, Nicolas; Speybroeck, Niko; Willingham, Arve Lee; Kasuga, Fumiko; Rokni, Mohammad B.; Zhou, Xiao-Nong et al. (2015-12-03). "World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis". PLOS Medicine 12 (12): e1001920. doi:10.1371/journal.pmed.1001920. ISSN 1549-1277. PMID 26633705.
- ↑ Hotez, Peter J.; Bundy, Donald A. P.; Beegle, Kathleen; Brooker, Simon; Drake, Lesley; de Silva, Nilanthi; Montresor, Antonio; Engels, Dirk et al. (2006), Jamison, Dean T.; Breman, Joel G.; Measham, Anthony R. et al., eds., "Helminth Infections: Soil-transmitted Helminth Infections and Schistosomiasis", Disease Control Priorities in Developing Countries (Washington (DC): World Bank), ISBN 978-0-8213-6179-5, PMID 21250326, http://www.ncbi.nlm.nih.gov/books/NBK11748/, retrieved 2021-08-13
- ↑ "How Infections Spread". 1 January 2016. https://www.cdc.gov/infectioncontrol/spread/index.html.
- ↑ Intestinal Parasites and Infection fungusfocus.com – Retrieved on 2010-01-21
- ↑ "Clinical Infectious Disease – Introduction". http://www.microbiologybook.org/Infectious%20Disease/Infectious%20Disease%20Introduction.htm.
- ↑ Pathogens and vectors . MetaPathogen.com.
- ↑ Hector, Tobias E.; Booksmythe, Isobel (April 2019). "Digest: Little evidence exists for a virulence-transmission trade-off*". Evolution 73 (4): 858–859. doi:10.1111/evo.13724. PMID 30900249.
- ↑ Acevedo, Miguel A.; Dillemuth, Forrest P.; Flick, Andrew J.; Faldyn, Matthew J.; Elderd, Bret D. (April 2019). "Virulence-driven trade-offs in disease transmission: A meta-analysis*". Evolution 73 (4): 636–647. doi:10.1111/evo.13692. PMID 30734920. https://digitalcommons.lsu.edu/biosci_pubs/1193. Retrieved 2022-06-28.
- ↑ Ericson, L.; Burdon, J. J.; Müller, W. J. (August 1999). "Spatial and temporal dynamics of epidemics of the rust fungus Uromyces valerianae on populations of its host Valeriana salina". Journal of Ecology 87 (4): 649–658. doi:10.1046/j.1365-2745.1999.00384.x. Bibcode: 1999JEcol..87..649E.
- ↑ Mideo, N; Alizon, S; Day, T (September 2008). "Linking within- and between-host dynamics in the evolutionary epidemiology of infectious diseases". Trends in Ecology & Evolution 23 (9): 511–517. doi:10.1016/j.tree.2008.05.009. PMID 18657880.
- ↑ Mordecai, Erin A.; Cohen, Jeremy M.; Evans, Michelle V.; Gudapati, Prithvi; Johnson, Leah R.; Lippi, Catherine A.; Miazgowicz, Kerri; Murdock, Courtney C. et al. (27 April 2017). "Detecting the impact of temperature on transmission of Zika, dengue, and chikungunya using mechanistic models". PLOS Neglected Tropical Diseases 11 (4): e0005568. doi:10.1371/journal.pntd.0005568. PMID 28448507.
- ↑ "Principles of Infectious Diseases: Transmission, Diagnosis, Prevention, and Control". International Encyclopedia of Public Health: 22–39. October 2016. doi:10.1016/B978-0-12-803678-5.00516-6. ISBN 9780128037089.
- ↑ 40.0 40.1 40.2 Vazquez-Pertejo, Maria T. (October 2022). "Diagnosis of Infectious Disease - Infections" (in English). https://www.merckmanuals.com/home/infections/diagnosis-of-infectious-disease/diagnosis-of-infectious-disease.
- ↑ Weaver, Jennifer S.; Omar, Imran M.; Mar, Winnie A.; Klauser, Andrea S.; Winegar, Blair A.; Mlady, Gary W.; McCurdy, Wendy E.; Taljanovic, Mihra S. (2022-03-05). "Magnetic resonance imaging of musculoskeletal infections". Polish Journal of Radiology 87: e141–e162. doi:10.5114/pjr.2022.113825. ISSN 1733-134X. PMID 35505859.
- ↑ Pinsky, B. A.; Hayden, R. T. (2019-08-26). "Cost-Effective Respiratory Virus Testing". Journal of Clinical Microbiology 57 (9): e00373–19. doi:10.1128/JCM.00373-19. ISSN 0095-1137. PMID 31142607.
- ↑ Ljubin-Sternak, Suncanica; Mestrovic, Tomislav (2014). "Review: Chlamydia trachonmatis and Genital Mycoplasmias: Pathogens with an Impact on Human Reproductive Health". Journal of Pathogens 2014 (183167): 3. doi:10.1155/2014/183167. PMID 25614838.
- ↑ 44.0 44.1 "Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review". Lancet 375 (9717): 834–45. March 2010. doi:10.1016/S0140-6736(09)62000-6. PMID 20132979.
- ↑ Murray, Patrick R. (2021). "Laboratory Diagnosis of Bacterial Diseases". Medical Microbiology (9th ed.). Philadelphia: Elsevier. ISBN 978-0-323-67450-8.
- ↑ Joyce, Bradley R.; Queener, Sherry F.; Wek, Ronald C.; Sullivan, William J. (2010-10-05). "Phosphorylation of eukaryotic initiation factor-2α promotes the extracellular survival of obligate intracellular parasite Toxoplasma gondii". Proceedings of the National Academy of Sciences of the United States of America 107 (40): 17200–17205. doi:10.1073/pnas.1007610107. ISSN 0027-8424. PMID 20855600. Bibcode: 2010PNAS..10717200J.
- ↑ Elliot, Simon L.; Rodrigues, Juliana de O.; Lorenzo, Marcelo G.; Martins-Filho, Olindo A.; Guarneri, Alessandra A. (2015). "Trypanosoma cruzi, etiological agent of Chagas disease, is virulent to its triatomine vector Rhodnius prolixus in a temperature-dependent manner". PLOS Neglected Tropical Diseases 9 (3): e0003646. doi:10.1371/journal.pntd.0003646. ISSN 1935-2735. PMID 25793495.
- ↑ Murray, Patrick R. (2021). "Microscopy and In Vitro Culture". Medical Microbiology (9th ed.). Philadelphia: Elsevier. ISBN 978-0-323-67450-8.
- ↑ Parveen, Nagma; Borrenberghs, Doortje; Rocha, Susana; Hendrix, Jelle (2018-05-10). "Single Viruses on the Fluorescence Microscope: Imaging Molecular Mobility, Interactions and Structure Sheds New Light on Viral Replication". Viruses 10 (5): 250. doi:10.3390/v10050250. ISSN 1999-4915. PMID 29748498.
- ↑ Saubolle, Michael A.; Sussland, Den (2003). "Nocardiosis". Journal of Clinical Microbiology 41 (10): 4497–4501. doi:10.1128/JCM.41.10.4497-4501.2003. ISSN 0095-1137. PMID 14532173.
- ↑ Flint, Harry J.; Scott, Karen P.; Duncan, Sylvia H.; Louis, Petra; Forano, Evelyne (2012-07-01). "Microbial degradation of complex carbohydrates in the gut". Gut Microbes 3 (4): 289–306. doi:10.4161/gmic.19897. ISSN 1949-0976. PMID 22572875.
- ↑ Makkoch, Jarika; Prachayangprecha, Slinporn; Payungporn, Sunchai; Chieochansin, Thaweesak; Songserm, Thaweesak; Amonsin, Alongkorn; Poovorawan, Yong (2012). "Erythrocyte Binding Preference of Human Pandemic Influenza Virus A and Its Effect on Antibody Response Detection". Annals of Laboratory Medicine 32 (4): 276–282. doi:10.3343/alm.2012.32.4.276. ISSN 2234-3806. PMID 22779069.
- ↑ 53.0 53.1 Kozera, Bartłomiej; Rapacz, Marcin (2013). "Reference genes in real-time PCR". Journal of Applied Genetics 54 (4): 391–406. doi:10.1007/s13353-013-0173-x. ISSN 1234-1983. PMID 24078518.
- ↑ Kayser, Fritz H; Kurt A Bienz; Johannes Eckert; Rolf M Zinkernagel (2005). Medical microbiology. Stuttgart: Georg Thieme Verlag. p. 398. ISBN 978-3-13-131991-3.
- ↑ Grinde, Bjørn (2013-10-25). "Herpesviruses: latency and reactivation – viral strategies and host response". Journal of Oral Microbiology 5: 22766. doi:10.3402/jom.v5i0.22766. ISSN 0901-8328. PMID 24167660.
- ↑ Dani, Arpad (2014). "Colonization and infection". Central European Journal of Urology 67 (1): 86–87. doi:10.5173/ceju.2014.01.art19. ISSN 2080-4806. PMID 24982790.
- ↑ Boldogh, Istvan; Albrecht, Thomas; Porter, David D. (1996), Baron, Samuel, ed., "Persistent Viral Infections", Medical Microbiology (University of Texas Medical Branch at Galveston), ISBN 978-0-9631172-1-2, PMID 21413348, http://www.ncbi.nlm.nih.gov/books/NBK8538/, retrieved 2020-01-23
- ↑ 58.0 58.1 Foster, John (2018). Microbiology. New York: Norton. pp. 39. ISBN 978-0-393-60257-9.
- ↑ 59.0 59.1 This section incorporates public domain materials included in the text: Medical Microbiology Fourth Edition: Chapter 8 (1996). Baron, Samuel MD. The University of Texas Medical Branch at Galveston. Baron, S. (1996). Medical Microbiology. University of Texas Medical Branch at Galveston. ISBN 9780963117212. https://www.ncbi.nlm.nih.gov/books/bv.fcgi?rid=mmed. Retrieved 2013-11-27.
- ↑ 60.0 60.1 "Targeting Immune Cell Checkpoints during Sepsis". International Journal of Molecular Sciences 18 (11): 2413. November 2017. doi:10.3390/ijms18112413. PMID 29135922.
- ↑ "Emerging Infectious Diseases". The Nursing Clinics of North America 54 (2): 297–311. June 2019. doi:10.1016/j.cnur.2019.02.006. PMID 31027668.
- ↑ "The history of tuberculosis: from the first historical records to the isolation of Koch's bacillus". Journal of Preventive Medicine and Hygiene 58 (1): E9–E12. March 2017. PMID 28515626.
- ↑ "The necessity to revise Koch's postulates and its application to infectious and non-infectious diseases: a mini-review". European Journal of Clinical Microbiology & Infectious Diseases 39 (2): 215–218. February 2020. doi:10.1007/s10096-019-03681-1. PMID 31440916.
- ↑ "Differentiating Epidemic from Endemic or Sporadic Infectious Disease Occurrence". Microbiology Spectrum 7 (4). July 2019. doi:10.1128/microbiolspec.AME-0007-2019. PMID 31325286.
- ↑ Higurea & Pietrangelo 2016 [page needed]
- ↑ "The effectiveness of hand hygiene procedures including hand-washing and alcohol-based hand sanitizers in reducing the risks of infections in home and community settings". American Journal of Infection Control 35 (10): S27–S64. 2007. doi:10.1016/j.ajic.2007.07.001. PMC 7115270. http://www.ajicjournal.org/article/S0196-6553(07)00595-0/fulltext. Retrieved 2017-03-26.
- ↑ ""Generalized Infectious Cycle" Diagram Illustration". http://science.education.nih.gov/supplements/nih1/diseases/guide/fig4-longdesc.htm.
- ↑ 68.0 68.1 Watts, Duncan (2003). Six degrees: the science of a connected age. London: William Heinemann. ISBN 978-0-393-04142-2. https://archive.org/details/sixdegrees00dunc.
- ↑ Preston, Richard (1995). The hot zone. Garden City, N.Y.: Anchor Books. ISBN 978-0-385-49522-6.
- ↑ Programs, National Research Council (US) and Institute of Medicine (US) Panel on Needle Exchange and Bleach Distribution; Normand, Jacques; Vlahov, David; Moses, Lincoln E. (1995) (in en). The Effects of Needle Exchange Programs. National Academies Press (US). https://www.ncbi.nlm.nih.gov/books/NBK232343/. Retrieved 2022-10-20.
- ↑ "The foot-and-mouth epidemic in Great Britain: pattern of spread and impact of interventions". Science 292 (5519): 1155–60. May 2001. doi:10.1126/science.1061020. PMID 11303090. Bibcode: 2001Sci...292.1155F.
- ↑ von Csefalvay, Chris (2023), "Modeling the control of infectious disease" (in en), Computational Modeling of Infectious Disease (Elsevier): pp. 173–215, doi:10.1016/b978-0-32-395389-4.00015-3, ISBN 978-0-323-95389-4, https://linkinghub.elsevier.com/retrieve/pii/B9780323953894000153, retrieved 2023-03-02
- ↑ "Herd Immunity". Oxford Vaccine Group, University of Oxford. http://vk.ovg.ox.ac.uk/herd-immunity.
- ↑ "Infectious diseases epidemiology". Journal of Epidemiology and Community Health 60 (3): 192–95. 2006. doi:10.1136/jech.2003.011593. PMID 16476746.
- ↑ "Genetic variation in IL28B predicts hepatitis C treatment-induced viral clearance". Nature 461 (7262): 399–401. 2009. doi:10.1038/nature08309. PMID 19684573. Bibcode: 2009Natur.461..399G.
- ↑ "Genetic variation in IL28B and spontaneous clearance of hepatitis C virus". Nature 461 (7265): 798–801. 2009. doi:10.1038/nature08463. PMID 19759533. Bibcode: 2009Natur.461..798T.
- ↑ "Antibiotics and Bacterial Resistance in the 21st Century". Perspectives in Medicinal Chemistry 6: 25–64. 2014. doi:10.4137/PMC.S14459. PMID 25232278.
- ↑ "Antibiotics: List of Common Antibiotics & Types" (in en). https://www.drugs.com/article/antibiotics.html.
- ↑ O'Brien, Deirdre J.; Gould, Ian M. (August 2013). "Maximizing the impact of antimicrobial stewardship". Current Opinion in Infectious Diseases 26 (4): 352–58. doi:10.1097/QCO.0b013e3283631046. PMID 23806898.
- ↑ Oran, Daniel P.; Topol, Eric J. (2020-09-01). "Prevalence of Asymptomatic SARS-CoV-2 Infection : A Narrative Review". Annals of Internal Medicine 173 (5): 362–367. doi:10.7326/M20-3012. ISSN 1539-3704. PMID 32491919.
- ↑ Beck, David B.; Aksentijevich, Ivona (2020-10-23). "Susceptibility to severe COVID-19" (in en). Science 370 (6515): 404–405. doi:10.1126/science.abe7591. ISSN 0036-8075. PMID 33093097.
- ↑ Klunk, Jennifer; Vilgalys, Tauras P.; Demeure, Christian E.; Cheng, Xiaoheng; Shiratori, Mari; Madej, Julien; Beau, Rémi; Elli, Derek et al. (November 2022). "Evolution of immune genes is associated with the Black Death". Nature 611 (7935): 312–319. doi:10.1038/s41586-022-05349-x. ISSN 1476-4687. PMID 36261521. Bibcode: 2022Natur.611..312K.
- ↑ World Health Organization (February 2009). "Age-standardized DALYs per 100,000 by cause, and Member State, 2004". https://www.who.int/entity/healthinfo/global_burden_disease/gbddeathdalycountryestimates2004.xls.
- ↑ "Could Ebola rank among the deadliest communicable diseases?". CBC News. 20 October 2014. http://www.cbc.ca/news/1.2802071.
- ↑ "The World Health Report (Annex Table 2)". 2004. https://www.who.int/whr/2004/annex/topic/en/annex_2_en.pdf.
- ↑ "Table 5". 1995. https://www.who.int/whr/1995/en/whr95_ch1_en.pdf.
- ↑ Lower respiratory infections include various pneumonias, influenzas and acute bronchitis.
- ↑ Diarrheal diseases are caused by many different organisms, including cholera, botulism, and E. coli to name a few. See also: Intestinal infectious diseases
- ↑ Tropical diseases include Chagas disease, dengue fever, lymphatic filariasis, leishmaniasis, onchocerciasis, schistosomiasis and trypanosomiasis.
- ↑ "WHO | The top 10 causes of death". WHO. https://www.who.int/mediacentre/factsheets/fs310/en/.
- ↑ "The perpetual challenge of infectious diseases". New England Journal of Medicine 366 (5): 454–61. 2012. doi:10.1056/NEJMra1108296. PMID 22296079.
- ↑ "Infectious and Epidemic Disease in History"
- ↑ 93.0 93.1 "Infectious Diseases and Human Population History". BioScience 46 (2): 115–26. 1996. doi:10.2307/1312814. http://www.erin.utoronto.ca/~w3gwynne/BIO418/Dobson1996.pdf. Retrieved 2013-11-27.
- ↑ "NCpedia | NCpedia". https://www.ncpedia.org/anchor/smallpox.
- ↑ Smallpox and Vaccinia. National Center for Biotechnology Information.
- ↑ Barquet, Nicolau (15 October 1997). "Smallpox: The Triumph over the Most Terrible of the Ministers of Death". Annals of Internal Medicine 127 (8_Part_1): 635–42. doi:10.7326/0003-4819-127-8_Part_1-199710150-00010. PMID 9341063.
- ↑ Multidrug-Resistant "Tuberculosis". Centers for Disease Control and Prevention.
- ↑ "Influenza of 1918 (Spanish Flu) and the US Navy". 20 February 2006. http://www.history.navy.mil/library/online/influenza_main.htm.
- ↑ 99.0 99.1 Krauss H; Weber A; Appel M (2003). Zoonoses: Infectious Diseases Transmissible from Animals to Humans (3rd ed.). Washington, D.C.: ASM Press. ISBN 978-1-55581-236-2.
- ↑ Potter P (July 2013). "Summer buzz". Emerg Infect Dis 19 (3): 1184. doi:10.3201/eid1907.AC1907.
- ↑ Peter Daszak; Andrew A. Cunningham; Alex D. Hyatt (27 January 2000). "Emerging Infectious Diseases of Wildlife – Threats to Biodiversity and Human Health". Science 287 (5452): 443–49. doi:10.1126/science.287.5452.443. PMID 10642539. Bibcode: 2000Sci...287..443D.
- ↑ "Annals of medical history. v.1 1917." (in en). p. 14. https://hdl.handle.net/2027/mdp.39015016778261?urlappend=%3Bseq=28.
- ↑ Thucydides; Crawley, Richard (1914). History of the Peloponnesian War, done into English by Richard Crawley. Robarts - University of Toronto. London Dent. pp. 131–132. http://archive.org/details/pelocrawleyr00thucuoft.
- ↑ Nutton, V (January 1983). "The seeds of disease: an explanation of contagion and infection from the Greeks to the Renaissance.". Medical History 27 (1): 1–34. doi:10.1017/s0025727300042241. ISSN 0025-7273. PMID 6339840.
- ↑ Rastogi, Nalin; Rastogi, R (1985-01-01). "Leprosy in ancient India". International Journal of Leprosy and Other Mycobacterial Diseases 52 (4): 541–43. PMID 6399073. https://www.researchgate.net/publication/16797371.
- ↑ Susruta; Bhishagratna, Kunja Lal (1907–1916). An English translation of the Sushruta samhita, based on original Sanskrit text. Edited and published by Kaviraj Kunja Lal Bhishagratna. With a full and comprehensive introd., translation of different readings, notes, comparative views, index, glossary and plates. Gerstein – University of Toronto. Calcutta. http://archive.org/details/englishtranslati00susruoft.
- ↑ Hoernle, A. F. Rudolf (August Friedrich Rudolf) (1907). Studies in the medicine of ancient India. Gerstein – University of Toronto. Oxford : At the Clarendon Press. http://archive.org/details/studiesinmedicin01hoeruoft.
- ↑ Byrne, Joseph Patrick (2012). Encyclopedia of the Black Death. ABC-CLIO. p. 29. ISBN 978-1598842531. https://books.google.com/books?id=5KtDfvlSrDAC&pg=PA29.
- ↑ Reid, Megan H. (2013). Law and Piety in Medieval Islam. Cambridge University Press. pp. 106, 114, 189–90. ISBN 978-1107067110. https://books.google.com/books?id=5fJ4AAAAQBAJ.
- ↑ Majeed, Azeem (22 December 2005). "How Islam changed medicine". BMJ 331 (7531): 1486–87. doi:10.1136/bmj.331.7531.1486. ISSN 0959-8138. PMID 16373721.
- ↑ Beretta M (2003). "The revival of Lucretian atomism and contagious diseases during the renaissance". Medicina Nei Secoli 15 (2): 129–54. PMID 15309812.
- ↑ Moorhead Robert (November 2002). "William Budd and typhoid fever". J R Soc Med 95 (11): 561–64. doi:10.1177/014107680209501115. PMID 12411628.
- ↑ Nettle D (2009). "Ecological influences on human behavioural diversity: a review of recent findings". Trends Ecol. Evol. 24 (11): 618–24. doi:10.1016/j.tree.2009.05.013. PMID 19683831.
- ↑ Molnar, R. E., 2001, "Theropod paleopathology: a literature survey": In: Mesozoic Vertebrate Life, edited by Tanke, D. H., and Carpenter, K., Indiana University Press, pp. 337–63.
- ↑ Caspermeyer, Joe (23 September 2007). "Space flight shown to alter ability of bacteria to cause disease". https://biodesign.asu.edu/news/space-flight-shown-alter-ability-bacteria-cause-disease.
- ↑ "Spaceflight Promotes Biofilm Formation by Pseudomonas aeruginosa". PLOS ONE 8 (4): e6237. April 29, 2013. doi:10.1371/journal.pone.0062437. PMID 23658630. Bibcode: 2013PLoSO...862437K.
- ↑ Dvorsky, George (13 September 2017). "Alarming Study Indicates Why Certain Bacteria Are More Resistant to Drugs in Space". https://gizmodo.com/alarming-study-indicates-why-certain-bacteria-are-more-1805666249.
- ↑ Dose, K.; Bieger-Dose, A.; Dillmann, R.; Gill, M.; Kerz, O.; Klein, A.; Meinert, H.; Nawroth, T. et al. (1995). "ERA-experiment "space biochemistry"". Advances in Space Research 16 (8): 119–29. doi:10.1016/0273-1177(95)00280-R. PMID 11542696. Bibcode: 1995AdSpR..16h.119D. http://publications.ub.uni-mainz.de/opus/volltexte/2008/11364/pdf/11364.pdf.[yes|permanent dead link|dead link}}]
- ↑ Horneck G.; Eschweiler, U.; Reitz, G.; Wehner, J.; Willimek, R.; Strauch, K. (1995). "Biological responses to space: results of the experiment "Exobiological Unit" of ERA on EURECA I". Adv. Space Res. 16 (8): 105–18. doi:10.1016/0273-1177(95)00279-N. PMID 11542695. Bibcode: 1995AdSpR..16h.105H.
External links
| Classification |
|---|
- European Center for Disease Prevention and Control
- U.S. Centers for Disease Control and Prevention,
- Infectious Disease Society of America (IDSA)
- Vaccine Research Center Information concerning vaccine research clinical trials for Emerging and re-Emerging Infectious Diseases.
- Microbes & Infection (journal)
 |
 KSF
KSF