Medical cannabis
Topic: Medicine
 From HandWiki - Reading time: 34 min
From HandWiki - Reading time: 34 min
Medical cannabis, or medical marijuana (MMJ), is cannabis and cannabinoids that are prescribed by physicians for their patients.[1][2] The use of cannabis as medicine has not been rigorously tested due to production and governmental restrictions, resulting in limited clinical research to define the safety and efficacy of using cannabis to treat diseases.[3]
Preliminary evidence has indicated that cannabis might reduce nausea and vomiting during chemotherapy and reduce chronic pain and muscle spasms.[4][5] Regarding non-inhaled cannabis or cannabinoids, a 2021 review found that it provided little relief against chronic pain and sleep disturbance, and caused several transient adverse effects, such as cognitive impairment, nausea, and drowsiness.[6]
Short-term use increases the risk of minor and major adverse effects.[5] Common side effects include dizziness, feeling tired, vomiting, and hallucinations.[5] Long-term effects of cannabis are not clear.[5] Concerns include memory and cognition problems, risk of addiction, schizophrenia in young people, and the risk of children taking it by accident.[4]
Many cultures have used cannabis for therapeutic purposes for thousands of years.[7] Some American medical organizations have requested removal of cannabis from the list of Schedule I controlled substances maintained by the United States federal government, followed by regulatory and scientific review.[8][9] Others oppose its legalization, such as the American Academy of Pediatrics.[10]
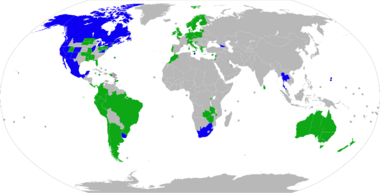
Medical cannabis can be administered through various methods, including capsules, lozenges, tinctures, dermal patches, oral or dermal sprays, cannabis edibles, and vaporizing or smoking dried buds. Synthetic cannabinoids are available for prescription use in some countries, such as dronabinol and nabilone. Countries that allow the medical use of whole-plant cannabis include Argentina, Australia, Canada, Chile, Colombia, Germany, Greece, Israel, Italy, the Netherlands, Peru, Poland, Portugal, Spain, and Uruguay. In the United States, 38 states and the District of Columbia have legalized cannabis for medical purposes, beginning with the passage of California's Proposition 215 in 1996.[11] Although cannabis remains prohibited for any use at the federal level, the Rohrabacher–Farr amendment was enacted in December 2014, limiting the ability of federal law to be enforced in states where medical cannabis has been legalized.
Classification
The National Institute on Drug Abuse defines medical cannabis as "using the whole, unprocessed marijuana plant or its basic extracts to treat symptoms of illness and other conditions".[12]
A cannabis plant includes more than 400 different chemicals, of which about 70 are cannabinoids.[13] In comparison, typical government-approved medications contain only one or two chemicals.[13] The number of active chemicals in cannabis is one reason why treatment with cannabis is difficult to classify and study.[13]
A 2014 review stated that the variations in ratio of CBD-to-THC in botanical and pharmaceutical preparations determines the therapeutic vs psychoactive effects (CBD attenuates THC's psychoactive effects[14]) of cannabis products.[15]
Medical uses
Overall, research into the health effects of medical cannabis has been of low quality and it is not clear whether it is a useful treatment for any condition, or whether harms outweigh any benefit.[16] There is no consistent evidence that it helps with chronic pain and muscle spasms.[16]
Low quality evidence suggests its use for reducing nausea during chemotherapy, improving appetite in HIV/AIDS, improving sleep, and improving tics in Tourette syndrome.[5] When usual treatments are ineffective, cannabinoids have also been recommended for anorexia, arthritis, glaucoma,[17] and migraine.[18]
It is unclear whether American states might be able to mitigate the adverse effects of the opioid epidemic by prescribing medical cannabis as an alternative pain management drug.[19]
Cannabis should not be used in pregnancy.[20]
Nausea and vomiting
Medical cannabis is somewhat effective in chemotherapy-induced nausea and vomiting (CINV)[4][17] and may be a reasonable option in those who do not improve following preferential treatment.[21] Comparative studies have found cannabinoids to be more effective than some conventional antiemetics such as prochlorperazine, promethazine, and metoclopramide in controlling CINV,[22] but these are used less frequently because of side effects including dizziness, dysphoria, and hallucinations.[23][24] Long-term cannabis use may cause nausea and vomiting, a condition known as cannabinoid hyperemesis syndrome (CHS).[25]
A 2016 Cochrane review said that cannabinoids were "probably effective" in treating chemotherapy-induced nausea in children, but with a high side-effect profile (mainly drowsiness, dizziness, altered moods, and increased appetite). Less common side effects were "ocular problems, orthostatic hypotension, muscle twitching, pruritus, vagueness, hallucinations, lightheadedness and dry mouth".[26]
HIV/AIDS
Evidence is lacking for both efficacy and safety of cannabis and cannabinoids in treating patients with HIV/AIDS or for anorexia associated with AIDS. As of 2013, current studies suffer from the effects of bias, small sample size, and lack of long-term data.[27]
Pain
A 2021 review found little effect of using non-inhaled cannabis to relieve chronic pain.[6] According to a 2019 systematic review, there have been inconsistent results of using cannabis for neuropathic pain, spasms associated with multiple sclerosis and pain from rheumatic disorders, but was not effective treating chronic cancer pain. The authors state that additional randomized controlled trials of different cannabis products are necessary to make conclusive recommendations.[16]
When cannabis is inhaled to relieve pain, blood levels of cannabinoids rise faster than when oral products are used, peaking within three minutes and attaining an analgesic effect in seven minutes.[28]
A 2011 review considered cannabis to be generally safe,[29] and it appears safer than opioids in palliative care.[30]
A 2022 review concluded the pain relief experienced after using medical cannabis is due to the placebo effect, especially given widespread media attention that sets the expectation for pain relief.[31]
Neurological conditions
Cannabis' efficacy is not clear in treating neurological problems, including multiple sclerosis (MS) and movement problems.[15] Evidence also suggests that oral cannabis extract is effective for reducing patient-centered measures of spasticity.[15] A trial of cannabis is deemed to be a reasonable option if other treatments have not been effective.[4][by whom?] Its use for MS is approved in ten countries.[4][32]Template:COI source A 2012 review found no problems with tolerance, abuse, or addiction.[33] In the United States, cannabidiol, one of the cannabinoids found in the marijuana plant, has been approved for treating two severe forms of epilepsy, Lennox-Gastaut syndrome and Dravet syndrome.[34]
Mental disorders
A 2019 systematic review found that there is a lack of evidence that cannabinoids are effective in treating depressive or anxiety disorders, attention-deficit hyperactivity disorder (ADHD), Tourette syndrome, post-traumatic stress disorder, or psychosis.[35]
Adverse effects

Medical use
There is insufficient data to draw strong conclusions about the safety of medical cannabis.[36] Typically, adverse effects of medical cannabis use are not serious;[4] they include tiredness, dizziness, increased appetite, and cardiovascular and psychoactive effects. Other effects can include impaired short-term memory; impaired motor coordination; altered judgment; and paranoia or psychosis at high doses.[37] Tolerance to these effects develops over a period of days or weeks. The amount of cannabis normally used for medicinal purposes is not believed to cause any permanent cognitive impairment in adults, though long-term treatment in adolescents should be weighed carefully as they are more susceptible to these impairments. Withdrawal symptoms are rarely a problem with controlled medical administration of cannabinoids. The ability to drive vehicles or to operate machinery may be impaired until a tolerance is developed.[21] Although supporters of medical cannabis say that it is safe,[36] further research is required to assess the long-term safety of its use.[23][38]
Cognitive effects
Recreational use of cannabis is associated with cognitive deficits, especially for those who begin to use cannabis in adolescence. As of 2021[update] there is a lack of research into long-term cognitive effects of medical use of cannabis, but one 12-month observational study reported that "MC patients demonstrated significant improvements on measures of executive function and clinical state over the course of 12 months".[39]
Impact on psychosis
Exposure to THC can cause acute transient psychotic symptoms in healthy individuals and people with schizophrenia.[14]
A 2007 meta analysis concluded that cannabis use reduced the average age of onset of psychosis by 2.7 years relative to non-cannabis use.[40] A 2005 meta analysis concluded that adolescent use of cannabis increases the risk of psychosis, and that the risk is dose-related.[41] A 2004 literature review on the subject concluded that cannabis use is associated with a two-fold increase in the risk of psychosis, but that cannabis use is "neither necessary nor sufficient" to cause psychosis.[42] A French review from 2009 came to a conclusion that cannabis use, particularly that before age 15, was a factor in the development of schizophrenic disorders.[43]
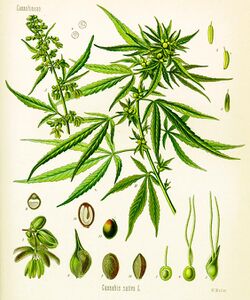
Pharmacology
The genus Cannabis contains two species which produce useful amounts of psychoactive cannabinoids: Cannabis indica and Cannabis sativa, which are listed as Schedule I medicinal plants in the US;[4] a third species, Cannabis ruderalis, has few psychogenic properties.[4] Cannabis contains more than 460 compounds;[7] at least 80 of these are cannabinoids[44][45] – chemical compounds that interact with cannabinoid receptors in the brain.[4] As of 2012, more than 20 cannabinoids were being studied by the U.S. FDA.[46]
The most psychoactive cannabinoid found in the cannabis plant is tetrahydrocannabinol (or delta-9-tetrahydrocannabinol, commonly known as THC).[7] Other cannabinoids include delta-8-tetrahydrocannabinol, cannabidiol (CBD), cannabinol (CBN), cannabicyclol (CBL), cannabichromene (CBC) and cannabigerol (CBG); they have less psychotropic effects than THC, but may play a role in the overall effect of cannabis.[7] The most studied are THC, CBD and CBN.[47]
CB1 and CB2 are the primary cannabinoid receptors responsible for several of the effects of cannabinoids, although other receptors may play a role as well. Both belong to a group of receptors called G protein-coupled receptors (GPCRs). CB1 receptors are found in very high levels in the brain and are thought to be responsible for psychoactive effects.[48] CB2 receptors are found peripherally throughout the body and are thought to modulate pain and inflammation.[49]
Absorption
Cannabinoid absorption is dependent on its route of administration.
Inhaled and vaporized THC have similar absorption profiles to smoked THC, with a bioavailability ranging from 10 to 35%. Oral administration has the lowest bioavailability of approximately 6%, variable absorption depending on the vehicle used, and the longest time to peak plasma levels (2 to 6 hours) compared to smoked or vaporized THC.[50]
Similar to THC, CBD has poor oral bioavailability, approximately 6%. The low bioavailability is largely attributed to significant first-pass metabolism in the liver and erratic absorption from the gastrointestinal tract. However, oral administration of CBD has a faster time to peak concentrations (2 hours) than THC.[50]
Due to the poor bioavailability of oral preparations, alternative routes of administration have been studied, including sublingual and rectal. These alternative formulations maximize bioavailability and reduce first-pass metabolism. Sublingual administration in rabbits yielded bioavailability of 16% and time to peak concentration of 4 hours.[51] Rectal administration in monkeys doubled bioavailability to 13.5% and achieved peak blood concentrations within 1 to 8 hours after administration.[52]
Distribution
Like cannabinoid absorption, distribution is also dependent on route of administration. Smoking and inhalation of vaporized cannabis have better absorption than do other routes of administration, and therefore also have more predictable distribution.[52][53] THC is highly protein bound once absorbed, with only 3% found unbound in the plasma. It distributes rapidly to highly vascularized organs such as the heart, lungs, liver, spleen, and kidneys, as well as to various glands. Low levels can be detected in the brain, testes, and unborn fetuses, all of which are protected from systemic circulation via barriers.[54] THC further distributes into fatty tissues a few days after administration due to its high lipophilicity, and is found deposited in the spleen and fat after redistribution.[53][55][56]
Metabolism
Delta-9-THC is the primary molecule responsible for the effects of cannabis. Delta-9-THC is metabolized in the liver and turns into 11-OH-THC.[57] 11-OH-THC is the first metabolic product in this pathway. Both Delta-9-THC and 11-OH-THC are psychoactive. The metabolism of THC into 11-OH-THC plays a part in the heightened psychoactive effects of edible cannabis.[58]
Next, 11-OH-THC is metabolized in the liver into 11-COOH-THC, which is the second metabolic product of THC.[59] 11-COOH-THC is not psychoactive.[57]
Ingestion of edible cannabis products lead to a slower onset of effect than the inhalation of it because the THC travels to the liver first through the blood before it travels to the rest of the body. Inhaled cannabis can result in THC going directly to the brain, where it then travels from the brain back to the liver in recirculation for metabolism.[57] Eventually, both routes of metabolism result in the metabolism of psychoactive THC to inactive 11-COOH-THC.
Excretion
Due to substantial metabolism of THC and CBD, their metabolites are excreted mostly via feces, rather than by urine.[50][60] After delta-9-THC is hydroxylated into 11-OH-THC via CYP2C9, CYP2C19, and CYP3A4, it undergoes phase II metabolism into more than 30 metabolites, a majority of which are products of glucuronidation. Approximately 65% of THC is excreted in feces and 25% in the urine, while the remaining 10% is excreted by other means.[50] The terminal half-life of THC is 25 to 36 hours,[61] whereas for CBD it is 18 to 32 hours.[60]
CBD is hydroxylated by P450 liver enzymes into 7-OH-CBD. Its metabolites are products of primarily CYP2C19 and CYP3A4 activity, with potential activity of CYP1A1, CYP1A2, CYP2C9, and CYP2D6.[62] Similar to delta-9-THC, a majority of CBD is excreted in feces and some in the urine.[50] The terminal half-life is approximately 18–32 hours.[63]
Administration
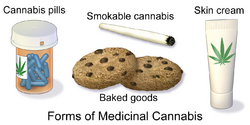
Smoking has been the means of administration of cannabis for many users, but it is not suitable for the use of cannabis as a medicine.[64] It was the most common method of medical cannabis consumption in the US as of 2013[update].[4] It is difficult to predict the pharmacological response to cannabis because concentration of cannabinoids varies widely, as there are different ways of preparing it for consumption (smoked, applied as oils, eaten, infused into other foods, or drunk) and a lack of production controls.[4] The potential for adverse effects from smoke inhalation makes smoking a less viable option than oral preparations.[64] Cannabis vaporizers have gained popularity because of a perception among users that fewer harmful chemicals are ingested when components are inhaled via aerosol rather than smoke.[4] Cannabinoid medicines are available in pill form (dronabinol and nabilone) and liquid extracts formulated into an oromucosal spray (nabiximols).[4] Oral preparations are "problematic due to the uptake of cannabinoids into fatty tissue, from which they are released slowly, and the significant first-pass liver metabolism, which breaks down Δ9THC and contributes further to the variability of plasma concentrations".[64]
The US Food and Drug Administration (FDA) has not approved smoked cannabis for any condition or disease, as it deems that evidence is lacking concerning safety and efficacy.[65] The FDA issued a 2006 advisory against smoked medical cannabis stating: "marijuana has a high potential for abuse, has no currently accepted medical use in treatment in the United States, and has a lack of accepted safety for use under medical supervision."[65]
History
Ancient
Cannabis, called má 麻 (meaning "hemp; cannabis; numbness") or dàmá 大麻 (with "big; great") in Chinese, was used in Taiwan for fiber starting about 10,000 years ago.[66] The botanist Hui-lin Li wrote that in China, "The use of Cannabis in medicine was probably a very early development. Since ancient humans used hemp seed as food, it was quite natural for them to also discover the medicinal properties of the plant."[67] Emperor Shen-Nung, who was also a pharmacologist, wrote a book on treatment methods in 2737 BCE that included the medical benefits of cannabis. He recommended the substance for many ailments, including constipation, gout, rheumatism, and absent-mindedness.[68] Cannabis is one of the 50 "fundamental" herbs in traditional Chinese medicine.[69]
The Ebers Papyrus (c. 1550 BCE) from Ancient Egypt describes medical cannabis.[70] The ancient Egyptians used hemp (cannabis) in suppositories for relieving the pain of hemorrhoids.[71]
Surviving texts from ancient India confirm that cannabis' psychoactive properties were recognized, and doctors used it for treating a variety of illnesses and ailments, including insomnia, headaches, gastrointestinal disorders, and pain, including during childbirth.[72]
The Ancient Greeks used cannabis to dress wounds and sores on their horses,[73] and in humans, dried leaves of cannabis were used to treat nose bleeds, and cannabis seeds were used to expel tapeworms.[73]
In the medieval Islamic world, Arabic physicians made use of the diuretic, antiemetic, antiepileptic, anti-inflammatory, analgesic and antipyretic properties of Cannabis sativa, and used it extensively as medication from the 8th to 18th centuries.[74]
Landrace strains

Cannabis seeds may have been used for food, rituals or religious practices in ancient Europe and China.[75]: 19–22 Harvesting the plant led to the spread of cannabis throughout Eurasia about 10,000 to 5,000 years ago, with further distribution to the Middle East and Africa about 2,000 to 500 years ago.[75]: 18–19 A landrace strain of cannabis developed over centuries.[76] They are cultivars of the plant that originated in one specific region.
Widely cultivated strains of cannabis, such as "Afghani" or "Hindu Kush", are indigenous to the Pakistan and Afghanistan regions, while "Durban Poison" is native to Africa.[75]: 45–48 There are approximately 16 landrace strains of cannabis identified from Pakistan, Jamaica, Africa, Mexico, Central America and Asia.[77]
Modern
An Irish physician, William Brooke O'Shaughnessy, is credited with introducing cannabis to Western medicine.[78] O'Shaughnessy discovered cannabis in the 1830s while living abroad in India , where he conducted numerous experiments investigating the drug's medical utility (noting in particular its analgesic and anticonvulsant effects).[79] He returned to England with a supply of cannabis in 1842, after which its use spread through Europe and the United States.[80] In 1845 French physician Jacques-Joseph Moreau published a book about the use of cannabis in psychiatry.[81] In 1850 cannabis was entered into the United States Pharmacopeia.[79] An anecdotal report of Cannabis indica as a treatment for tetanus appeared in Scientific American in 1880.[82]
The use of cannabis in medicine began to decline by the end of the 19th century, due to difficulty in controlling dosages and the rise in popularity of synthetic and opium-derived drugs.[80] Also, the advent of the hypodermic syringe allowed these drugs to be injected for immediate effect, in contrast to cannabis which is not water-soluble and therefore cannot be injected.[80]
In the United States, the medical use of cannabis further declined with the passage of the Marihuana Tax Act of 1937, which imposed new regulations and fees on physicians prescribing cannabis.[83] Cannabis was removed from the U.S. Pharmacopeia in 1941, and officially banned for any use with the passage of the Controlled Substances Act of 1970.[80]
Cannabis began to attract renewed interest as medicine in the 1970s and 1980s, in particular due to its use by cancer and AIDS patients who reported relief from the effects of chemotherapy and wasting syndrome.[84] In 1996, California became the first U.S. state to legalize medical cannabis in defiance of federal law.[85] In 2001, Canada became the first country to adopt a system regulating the medical use of cannabis.[86]
-
The use of cannabis, at least as fiber, has been shown to go back at least 10,000 years in Taiwan. "Dà má" (Pinyin pronunciation) is the Chinese expression for cannabis, the first character meaning "big" and the second character meaning "hemp".
-
Cannabis indica fluid extract, American Druggists Syndicate, pre-1937
-
An advertisement for cannabis americana distributed by a pharmacist in New York in 1917
-
The Ebers Papyrus (c. 1550 BCE) from Ancient Egypt has a prescription for medical marijuana applied directly for inflammation.
Society and culture
Legal status
See also countries that have decriminalized or where enforcement is limited.
Countries that have legalized the medical use of cannabis include Argentina ,[87] Australia ,[88] Brazil ,[89] Canada ,[90] Chile ,[90] Colombia,[90] Costa Rica,[91] Croatia,[92] Cyprus,[93] Czech Republic,[90] Finland ,[94] Germany ,[95] Greece,[96] Israel,[97] Italy,[98] Jamaica,[99] Lebanon,[100] Luxembourg,[101] Malta,[102] Morocco,[103] the Netherlands,[90] New Zealand,[104] North Macedonia,[105] Panama,[106] Peru,[107] Poland ,[108] Portugal,[109] Rwanda,[110] Spain ,[111] Sri Lanka,[112] Switzerland ,[113] Thailand,[114] the United Kingdom ,[115] and Uruguay.[90] Other countries have more restrictive laws that allow only the use of isolated cannabinoid drugs such as Sativex or Epidiolex.[116][117] Countries with the most relaxed policies include Canada,[118] the Netherlands,[90] Thailand,[119] and Uruguay,[90] where cannabis can be purchased without need for a prescription. In Mexico, THC content of medical cannabis is limited to one percent.[120] In the United States , the legality of medical cannabis varies by state.[11]
Cannabis and its derivatives are subject to regulation under three United Nations treaties: the 1961 Single Convention on Narcotic Drugs, the 1971 Convention on Psychotropic Substances, and the 1988 Convention Against Illicit Traffic in Narcotic Drugs and Psychotropic Substances.[121] Cannabis is classified as a Schedule I drug under the Single Convention treaty, meaning that medical use is allowed but that it is considered to be an addictive drug with a serious risk of abuse – along with other drugs such as opium and cocaine.[122] Prior to December 2020 it was also included in Schedule IV, a subset of Schedule I, which is for only the most dangerous drugs such as heroin and fentanyl.[123] Member nations of the UN Commission on Narcotic Drugs voted 27–25 to remove it from Schedule IV on 2 December 2020,[124] following a World Health Organization recommendation for removal in January 2019.[125][126]
United States
In the United States, the use of cannabis for medical purposes is legal in 38 states, four out of five permanently inhabited U.S. territories, and the District of Columbia.[11] An additional 10 states have more restrictive laws allowing the use of low-THC products.[11] Cannabis remains illegal at the federal level under the Controlled Substances Act, which classifies it as a Schedule I drug with a high potential for abuse and no accepted medical use. In December 2014, however, the Rohrabacher–Farr amendment was signed into law, prohibiting the Justice Department from prosecuting individuals acting in accordance with state medical cannabis laws.[127]
Economics
Distribution

The method of obtaining medical cannabis varies by region and by legislation. In the US, most consumers grow their own or buy it from cannabis dispensaries in states where it is legal.[4][128] Marijuana vending machines for selling or dispensing cannabis are in use in the United States and are planned to be used in Canada.[129] In 2014, the startup Meadow began offering on-demand delivery of medical marijuana in the San Francisco Bay Area, through their mobile app.[130]
Almost 70% of medical cannabis is exported from the United Kingdom, according to a 2017 United Nations report, with much of the remaining amount coming from Canada and the Netherlands.[131]
Insurance
In the United States, health insurance companies may not pay for a medical marijuana prescription as the Food and Drug Administration must approve any substance for medicinal purposes. Before this can happen, the FDA must first permit the study of the medical benefits and drawbacks of the substance, which it has not done since it was placed on Schedule I of the Controlled Substances Act in 1970. Therefore, all expenses incurred fulfilling a medical marijuana prescription will possibly be incurred as out-of-pocket.[132] However, the New Mexico Court of Appeals has ruled that workers' compensation insurance must pay for prescribed marijuana as part of the state's Medical Cannabis Program.[133]
Positions of medical organizations
Medical organizations that have issued statements in support of allowing access to medical cannabis include the American Nurses Association,[8] American Public Health Association,[134] American Medical Student Association,[135] National Multiple Sclerosis Society,[136] Epilepsy Foundation,[137] and Leukemia & Lymphoma Society.[138]
Organizations that oppose the legalization of medical cannabis include the American Academy of Pediatrics[10] and American Psychiatric Association.[139] However, the AAP also supports rescheduling for the purpose of facilitating research.[10]
The American Medical Association[140] and American College of Physicians[141] do not take a position on the legalization of medical cannabis, but have called for the Schedule I classification to be reviewed. The American Academy of Family Physicians[9] and American Society of Addiction Medicine[142] also do not take a position, but do support rescheduling to better facilitate research. The American Heart Association says that "many of the concerning health implications of cannabis include cardiovascular diseases" but that it supports rescheduling to allow "more nuanced ... marijuana legislation and regulation" and to "reflect the existing science behind cannabis".[143] The American Cancer Society[144] and American Psychological Association[145] have noted the obstacles that exist for conducting research on cannabis, and have called on the federal government to better enable scientific study of the drug.
Cancer Research UK say that while cannabis is being studied for therapeutic potential, "claims that there is solid "proof" that cannabis or cannabinoids can cure cancer is highly misleading to patients and their families, and builds a false picture of the state of progress in this area".[146]
Brand names
In the US, the FDA has approved two oral cannabinoids for use as medicine: dronabinol and nabilone.[4] Dronabinol, synthetic THC, is listed as Schedule II.[147] Nabilone, a synthetic cannabinoid, is also Schedule II, indicating high potential for side effects and addiction.[46] Both received approval for sale in the US in 1985, under the brand names Marinol and Cesamet.[148] Nabiximols, an oromucosal spray derived from two strains of Cannabis sativa and containing THC and CBD,[46] is not approved in the United States, but is approved in several European countries, Canada, and New Zealand as of 2013.[4] As of 2018, medical marijuana in Canada is being legally distributed to registered patients in bud, drops and capsule forms by such companies as Canopy Growth Corp. and Aurora Cannabis.
| Generic medication |
Brand name(s) |
Country | Licensed indications |
|---|---|---|---|
| Nabilone | Cesamet | U.S., Canada | Antiemetic (treatment of nausea or vomiting) associated with chemotherapy that has failed to respond adequately to conventional therapy[4] |
| Dronabinol | Marinol | ||
| Syndros | U.S. | Anorexia associated with AIDS–related weight loss[4] | |
| Nabiximols | Sativex | Canada, New Zealand, majority of the EU[149] |
Limited treatment for spasticity and neuropathic pain associated with multiple sclerosis and intractable cancer pain.[4] |
As an antiemetic, these medications are usually used when conventional treatment for nausea and vomiting associated with cancer chemotherapy fail to work.[4]
Nabiximols is used for treatment of spasticity associated with MS when other therapies have not worked, and when an initial trial demonstrates "meaningful improvement".[4] Trials for FDA approval in the US are underway.[4] It is also approved in several European countries for overactive bladder and vomiting.[46] When sold under the trade name Sativex as a mouth spray, the prescribed daily dose in Sweden delivers a maximum of 32.4 mg of THC and 30 mg of CBD; mild to moderate dizziness is common during the first few weeks.[150]
Relative to inhaled consumption, peak concentration of oral THC is delayed, and it may be difficult to determine optimal dosage because of variability in patient absorption.[4]
In 1964, Albert Lockhart and Manley West began studying the health effects of traditional cannabis use in Jamaican communities. They developed, and in 1987 gained permission to market, the pharmaceutical "Canasol", one of the first cannabis extracts.[151]
Research
Medical cannabis research includes any medical research on using cannabis as a treatment for any medical condition. For reasons including increased popular support of cannabis use, a trend of cannabis legalization, and the perception of medical usefulness, more scientists are doing medical cannabis research. Medical cannabis is broad for many conditions, each of which has its own state of research.
A 2022 review concluded that "oral, synthetic cannabis products with high THC-to-CBD ratios and sublingual, extracted cannabis products with comparable THC-to-CBD ratios may be associated with short-term improvements in chronic pain and increased risk for dizziness and sedation."[152]
See also
- Charlotte's Web (cannabis)
- Chinese herbology
- Tilden's Extract
References
- ↑ "Medicinal cannabis". Australian Prescriber 38 (6): 212–15. December 2015. doi:10.18773/austprescr.2015.072. PMID 26843715.
- ↑ "What is medical marijuana?". July 2015. https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine. "The term medical marijuana refers to using the whole unprocessed marijuana plant or its basic extracts to treat a disease or symptom."
- ↑ "Release the strains". Nature Medicine 21 (9): 963. September 2015. doi:10.1038/nm.3946. PMID 26340110.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 4.11 4.12 4.13 4.14 4.15 4.16 4.17 4.18 4.19 4.20 4.21 4.22 "The pharmacologic and clinical effects of medical cannabis". Pharmacotherapy 33 (2): 195–209. February 2013. doi:10.1002/phar.1187. PMID 23386598. https://wsma.org/doc_library/LegalResourceCenter/MedicalCannabis/Med%20Mar%20-%20Pharmacologic%20and%20Clinical%20Effects.pdf. Retrieved 11 November 2017.
- ↑ 5.0 5.1 5.2 5.3 5.4 "Cannabinoids for Medical Use: A Systematic Review and Meta-analysis". JAMA 313 (24): 2456–73. 23 June 2015. doi:10.1001/jama.2015.6358. PMID 26103030.
- ↑ 6.0 6.1 Wang, Li; Hong, Patrick J; May, Curtis; Rehman, Yasir; Oparin, Yvgeniy; Hong, Chris J; Hong, Brian Y; AminiLari, Mahmood et al. (2021-09-09). "Medical cannabis or cannabinoids for chronic non-cancer and cancer related pain: a systematic review and meta-analysis of randomised clinical trials". BMJ 374: n1034. doi:10.1136/bmj.n1034. ISSN 1756-1833. PMID 34497047. https://www.bmj.com/content/374/bmj.n1034. Retrieved 9 September 2021.
- ↑ 7.0 7.1 7.2 7.3 "Cannabinoids in medicine: A review of their therapeutic potential". Journal of Ethnopharmacology 105 (1–2): 1–25. April 2006. doi:10.1016/j.jep.2006.02.001. PMID 16540272.
- ↑ 8.0 8.1 Therapeutic Use of Marijuana and Related Cannabinoids, American Nurses Association, 2016, https://www.nursingworld.org/~4ad4a8/globalassets/docs/ana/therapeutic-use-of-marijuana-and-related-cannabinoids.pdf, retrieved 13 May 2018
- ↑ 9.0 9.1 "AAFP Releases Marijuana, Cannabinoids Position Paper". American Academy of Family Physicians. 20 September 2019. https://www.aafp.org/news/health-of-the-public/20190920cannabispaper.html.
- ↑ 10.0 10.1 10.2 American Academy of Pediatrics Reaffirms Opposition to Legalizing Marijuana for Recreational or Medical Use, American Academy of Pediatrics, 26 January 2015, https://www.aap.org/en-us/about-the-aap/aap-press-room/Pages/American-Academy-of-Pediatrics-Reaffirms-Opposition-to-Legalizing-Marijuana-for-Recreational-or-Medical-Use.aspx, retrieved 30 July 2017
- ↑ 11.0 11.1 11.2 11.3 "State Medical Marijuana Laws". 12 September 2022. http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx.
- ↑ "Marijuana as Medicine". National Institute on Drug Abuse. July 2019. https://www.drugabuse.gov/publications/drugfacts/marijuana-medicine.
- ↑ 13.0 13.1 13.2 "Up in Smoke: Does Medical Marijuana Work?". 28 April 2016. http://www.consumerreports.org/medical-marijuana/does-medical-marijuana-work/.
- ↑ 14.0 14.1 "Cannabidiol as a potential treatment for psychosis". European Neuropsychopharmacology 24 (1): 51–64. January 2014. doi:10.1016/j.euroneuro.2013.11.002. PMID 24309088. http://cannabisclinicians.org/wp-content/uploads/2013/12/CBD-psychosis-2013.pdf. Retrieved 9 July 2016.
- ↑ 15.0 15.1 15.2 "Systematic review: efficacy and safety of medical marijuana in selected neurologic disorders: report of the Guideline Development Subcommittee of the American Academy of Neurology". Neurology 82 (17): 1556–1563. April 2014. doi:10.1212/WNL.0000000000000363. PMID 24778283.
- ↑ 16.0 16.1 16.2 "Benefits and harms of medical cannabis: a scoping review of systematic reviews". Syst Rev 8 (1): 320. December 2019. doi:10.1186/s13643-019-1243-x. PMID 31823819.
- ↑ 17.0 17.1 "Safety and Toxicology of Cannabinoids". Neurotherapeutics 12 (4): 735–46. October 2015. doi:10.1007/s13311-015-0380-8. PMID 26269228.
- ↑ "Sex(ism), Drugs, and Migraines: Distillations Podcast and Transcript, Episode 237". Science History Institute. 15 January 2019. https://www.sciencehistory.org/distillations/podcast/sexism-drugs-and-migraines.
- ↑ Gilson, Aaron M.; LeBaron, Virginia T.; Vyas, Marianne Beare (1 January 2018). "The use of cannabis in response to the opioid crisis: A review of the literature". Nursing Outlook 66 (1): 56–65. doi:10.1016/j.outlook.2017.08.012. ISSN 0029-6554. PMID 28993073.
- ↑ American College of Obstetricians Gynecologists Committee on Obstetric Practice (July 2015). "Committee Opinion No. 637: Marijuana Use During Pregnancy and Lactation". Obstetrics and Gynecology 126 (1): 234–38. doi:10.1097/01.AOG.0000467192.89321.a6. PMID 26241291.
- ↑ 21.0 21.1 "The therapeutic potential of cannabis and cannabinoids". Deutsches Ärzteblatt International 109 (29–30): 495–501. July 2012. doi:10.3238/arztebl.2012.0495. PMID 23008748.
- ↑ "The intersection between cannabis and cancer in the United States". Critical Reviews in Oncology/Hematology 83 (1): 1–10. July 2012. doi:10.1016/j.critrevonc.2011.09.008. PMID 22019199.
- ↑ 23.0 23.1 "Adverse effects of medical cannabinoids: a systematic review". CMAJ 178 (13): 1669–78. June 2008. doi:10.1503/cmaj.071178. PMID 18559804.
- ↑ "Guidelines for antiemetic treatment of chemotherapy-induced nausea and vomiting: past, present, and future recommendations". The Oncologist 12 (9): 1143–50. September 2007. doi:10.1634/theoncologist.12-9-1143. PMID 17914084. http://pdfs.semanticscholar.org/d98c/026bda42b4b6ea1b0286d1893b362b46cca4.pdf.
- ↑ "Cannabinoid hyperemesis syndrome: a case series and review of previous reports". Psychosomatics 53 (3): 212–19. May–Jun 2012. doi:10.1016/j.psym.2012.01.003. PMID 22480624.
- ↑ "Antiemetic medication for prevention and treatment of chemotherapy-induced nausea and vomiting in childhood". The Cochrane Database of Systematic Reviews 2016 (2): CD007786. February 2016. doi:10.1002/14651858.CD007786.pub3. PMID 26836199. PMC 7073407. http://eprints.whiterose.ac.uk/95658/1/Phillips_et_al_2016_The_Cochrane_library.sup_2.pdf. Retrieved 23 September 2019.
- ↑ "The medical use of cannabis for reducing morbidity and mortality in patients with HIV/AIDS". The Cochrane Database of Systematic Reviews 4 (4): CD005175. April 2013. doi:10.1002/14651858.CD005175.pub3. PMID 23633327.
- ↑ "Efficacy of Cannabis-Based Medicines for Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials". Pain Physician 20 (6): E755–96. September 2017. doi:10.36076/ppj.20.5.E755. PMID 28934780. http://www.painphysicianjournal.com/current/pdf?article=NDYwNA%3D%3D&journal=107. Retrieved 12 January 2018.
- ↑ "Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials". British Journal of Clinical Pharmacology 72 (5): 735–44. November 2011. doi:10.1111/j.1365-2125.2011.03970.x. PMID 21426373.
- ↑ "Cannabis in palliative medicine: improving care and reducing opioid-related morbidity". The American Journal of Hospice & Palliative Care 28 (5): 297–303. August 2011. doi:10.1177/1049909111402318. PMID 21444324.
- ↑ Filip Gedin; Sebastian Blomé; Moa Pontén; Maria Lalouni; Jens Fust; Andreé Raquette; Viktor Vadenmark Lundquist; William H. Thompson et al. (November 28, 2022). "Placebo Response and Media Attention in Randomized Clinical Trials Assessing Cannabis-Based Therapies for PainA Systematic Review and Meta-analysis". JAMA Network Open 5 (11): e2243848. doi:10.1001/jamanetworkopen.2022.43848. PMID 36441553.
- ↑ "Medical marijuana: medical necessity versus political agenda". Medical Science Monitor 17 (12): RA249–61. December 2011. doi:10.12659/MSM.882116. PMID 22129912.
- ↑ "[Treatment of spasticity in multiple sclerosis: new perspectives regarding the use of cannabinoids]" (in es). Revista de Neurología 55 (7): 421–30. October 2012. PMID 23011861.
- ↑ Commissioner, Office of the (2019-06-10). "FDA and Marijuana" (in en). FDA. https://www.fda.gov/news-events/public-health-focus/fda-and-marijuana. Retrieved 16 December 2019.
- ↑ "Cannabinoids for the treatment of mental disorders and symptoms of mental disorders: a systematic review and meta-analysis". Lancet Psychiatry 6 (12): 995–1010. 2019. doi:10.1016/S2215-0366(19)30401-8. PMID 31672337.
- ↑ 36.0 36.1 Washington, Tabitha A.; Brown, Khalilah M.; Fanciullo, Gilbert J. (2012). "Chapter 31: Medical Cannabis". Pain. Oxford University Press. p. 165. ISBN 978-0-19-994274-9. "Proponents of medical cannabis site its safety, but there studies in later years that support that smoking of marijuana is associated with risk for dependence and that THC alters the structures of cells in the brain"
- ↑ "Association Between Cannabis and Psychosis: Epidemiologic Evidence". Biological Psychiatry 79 (7): 549–56. April 2016. doi:10.1016/j.biopsych.2015.08.001. PMID 26386480. https://research-information.bris.ac.uk/en/publications/association-between-cannabis-and-psychosis(b8fb2d3b-5a55-4d07-97c0-1650b0ffc05d).html. Retrieved 11 March 2020.
- ↑ Barceloux, Donald G (2012). "Chapter 60: Marijuana (Cannabis sativa L.) and synthetic cannabinoids". Medical Toxicology of Drug Abuse: Synthesized Chemicals and Psychoactive Plants. John Wiley & Sons. pp. 886–931. ISBN 978-0-471-72760-6. https://books.google.com/books?id=OWFiVaDZnkQC&pg=PA886. Retrieved 20 December 2015.
- ↑ Sagar, Kelly A.; Dahlgren, M. Kathryn; Lambros, Ashley M.; Smith, Rosemary T.; El-Abboud, Celine; Gruber, Staci A. (2021). "An Observational, Longitudinal Study of Cognition in Medical Cannabis Patients over the Course of 12 Months of Treatment: Preliminary Results" (in en). Journal of the International Neuropsychological Society 27 (6): 648–60. doi:10.1017/S1355617721000114. ISSN 1355-6177. PMID 34261553.
- ↑ "Cannabis use and earlier onset of psychosis: a systematic meta-analysis". Archives of General Psychiatry 68 (6): 555–61. June 2011. doi:10.1001/archgenpsychiatry.2011.5. PMID 21300939.
- ↑ "Cannabis as a risk factor for psychosis: systematic review". Journal of Psychopharmacology 19 (2): 187–94. March 2005. doi:10.1177/0269881105049040. PMID 15871146.
- ↑ "Causal association between cannabis and psychosis: examination of the evidence". The British Journal of Psychiatry 184 (2): 110–17. February 2004. doi:10.1192/bjp.184.2.110. PMID 14754822.
- ↑ "[Is cannabis a vulnerability factor in schizophrenic disorders]". Archives de Pédiatrie 16 (9): 1302–05. September 2009. doi:10.1016/j.arcped.2009.03.016. PMID 19640690.
- ↑ "Phytocannabinoids, CNS cells and development: a dead issue?". Drug and Alcohol Review 29 (1): 91–98. January 2010. doi:10.1111/j.1465-3362.2009.00102.x. PMID 20078688.
- ↑ "Cannabinoid analgesia as a potential new therapeutic option in the treatment of chronic pain". The Annals of Pharmacotherapy 40 (2): 251–60. February 2006. doi:10.1345/aph.1G217. PMID 16449552.
- ↑ 46.0 46.1 46.2 46.3 "Legalization, decriminalization & medicinal use of cannabis: a scientific and public health perspective". Missouri Medicine 109 (2): 90–98. 2012. PMID 22675784.
- ↑ "Medical consequences of marijuana use: a review of current literature". Current Psychiatry Reports 15 (12): 419. December 2013. doi:10.1007/s11920-013-0419-7. PMID 24234874. https://zenodo.org/record/1232874. Retrieved 12 July 2019.
- ↑ "Cannabinoid receptors: where they are and what they do". Journal of Neuroendocrinology 20 (Suppl 1): 10–14. May 2008. doi:10.1111/j.1365-2826.2008.01671.x. PMID 18426493.
- ↑ "The role of the cannabinoid CB2 receptor in pain transmission and therapeutic potential of small molecule CB2 receptor agonists". Current Medicinal Chemistry 14 (8): 917–36. 2007. doi:10.2174/092986707780363023. PMID 17430144.
- ↑ 50.0 50.1 50.2 50.3 50.4 "Pharmacology of cannabinoids in the treatment of epilepsy". Epilepsy & Behavior. Cannabinoids and Epilepsy 70 (Pt B): 313–18. May 2017. doi:10.1016/j.yebeh.2016.11.016. PMID 28087250.
- ↑ "Sublingual administration of Delta9-tetrahydrocannabinol/beta-cyclodextrin complex increases the bioavailability of Delta9-tetrahydrocannabinol in rabbits". Life Sciences 78 (17): 1911–14. March 2006. doi:10.1016/j.lfs.2005.08.025. PMID 16266727.
- ↑ 52.0 52.1 "Human cannabinoid pharmacokinetics". Chemistry & Biodiversity 4 (8): 1770–804. August 2007. doi:10.1002/cbdv.200790152. PMID 17712819.
- ↑ 53.0 53.1 "A review of oral cannabinoids and medical marijuana for the treatment of chemotherapy-induced nausea and vomiting: a focus on pharmacokinetic variability and pharmacodynamics". Cancer Chemotherapy and Pharmacology 80 (3): 441–49. September 2017. doi:10.1007/s00280-017-3387-5. PMID 28780725.
- ↑ "The pharmacokinetics of THC in fat and brain: resulting functional responses to marihuana smoking". Human Psychopharmacology 16 (3): 247–55. April 2001. doi:10.1002/hup.258. PMID 12404577.
- ↑ "Medicinal Cannabis: History, Pharmacology, And Implications for the Acute Care Setting". P & T 42 (3): 180–88. March 2017. PMID 28250701.
- ↑ Nahas, Gabriel G.; Sutin, Kenneth M.; Harvey, David J.; Agurell, Stig (1999). Marihuana and Medicine. Springer Science & Business Media. ISBN 978-1-59259-710-9. https://books.google.com/books?id=AYH5BwAAQBAJ&pg=PA91. Retrieved 20 September 2020.
- ↑ 57.0 57.1 57.2 "Human Metabolism of THC" (in en-US). Sapiensoup Blog. 2016-12-21. https://sapiensoup.com/human-metabolism-thc.
- ↑ "11-Hydroxy-THC - Increased Potency That Explains the Effect of Edibles? – Prof of Pot" (in en-US). 2 July 2016. http://profofpot.com/11-hydroxy-tetrahydrocannabinol-potency-edibles/.
- ↑ "Toxicology Litigation Support: Marijuana". http://www.consultox.com/toxicology-marijuana.shtml.
- ↑ 60.0 60.1 "Cannabidiol: pharmacology and potential therapeutic role in epilepsy and other neuropsychiatric disorders". Epilepsia 55 (6): 791–802. June 2014. doi:10.1111/epi.12631. PMID 24854329.
- ↑ "Pharmacokinetics and pharmacodynamics of cannabinoids". Clinical Pharmacokinetics 42 (4): 327–60. 2003-04-01. doi:10.2165/00003088-200342040-00003. PMID 12648025.
- ↑ Juřica, Ondřej Zendulka, Gabriela Dovrtělová, Kristýna Nosková, Miroslav Turjap, Alexandra Šulcová, Lumír Hanuš and Jan (2016-02-29). "Cannabinoids and Cytochrome P450 Interactions" (in en). Current Drug Metabolism 17 (3): 206–226. doi:10.2174/1389200217666151210142051. PMID 26651971. http://www.eurekaselect.com/137749/article. Retrieved 1 November 2017.
- ↑ "Single-dose kinetics of deuterium-labelled cannabidiol in man after smoking and intravenous administration". Biomedical & Environmental Mass Spectrometry 13 (2): 77–83. February 1986. doi:10.1002/bms.1200130206. PMID 2937482.
- ↑ 64.0 64.1 64.2 "Cannabinoids for Tourette's Syndrome". The Cochrane Database of Systematic Reviews 2009 (4): CD006565. October 2009. doi:10.1002/14651858.CD006565.pub2. PMID 19821373.
- ↑ 65.0 65.1 "Inter-agency advisory regarding claims that smoked marijuana is a medicine" (Press release). fda.gov. 20 April 2006. Archived from the original on 13 October 2012. Retrieved 24 December 2012.
- ↑ Abel, Ernest L. (1980). "Cannabis in the Ancient World". Marihuana: the first twelve thousand years. New York City: Plenum Publishers. ISBN 978-0-306-40496-2. http://www.druglibrary.org/schaffer/hemp/history/first12000/1.htm. Retrieved 29 October 2008.[page needed]
- ↑ Li, Hui-Lin (1974). "An Archaeological and Historical Account of Cannabis in China", Economic Botany 28.4:437–48, p. 444.
- ↑ Bloomquist, Edward (1971). Marijuana: The Second Trip. California: Glencoe Press.
- ↑ Wong, Ming (1976). La Médecine chinoise par les plantes. Paris: Tchou. OCLC 2646789.[page needed]
- ↑ [unreliable source?] "The Ebers Papyrus The Oldest (confirmed) Written Prescriptions For Medical Marihuana era 1,550 BC". onlinepot.org. http://www.onlinepot.org/medical/eberspapyrus.htm.
- ↑ Pain, Stephanie (15 December 2007). "The Pharaoh's pharmacists". New Scientist (Reed Business Information Ltd.). https://www.newscientist.com/channel/health/mg19626341.600-the-pharaohs-pharmacists.html.
- ↑ "The religious and medicinal uses of Cannabis in China, India and Tibet". Journal of Psychoactive Drugs 13 (1): 23–34. 1981. doi:10.1080/02791072.1981.10471447. PMID 7024492.
- ↑ 73.0 73.1 Butrica, James L. (2002). "The Medical Use of Cannabis Among the Greeks and Romans". Journal of Cannabis Therapeutics 2 (2): 51–70. doi:10.1300/J175v02n02_04. http://www.cannabis-med.org/data/pdf/2002-02-3.pdf. Retrieved 8 November 2014.
- ↑ Lozano, Indalecio (2001). "The Therapeutic Use of Cannabis sativa (L.) in Arabic Medicine". Journal of Cannabis Therapeutics 1: 63–70. doi:10.1300/J175v01n01_05.
- ↑ 75.0 75.1 75.2 Holland, Julie, ed (2010). The Pot Book: A Complete Guide to Cannabis. New York: Simon and Schuster. ISBN 978-1594778988. https://books.google.com/books?id=tV0oDwAAQBAJ. Retrieved 22 April 2018.
- ↑ Evert, Ray F.; Eichhorn, Susan E. (2013). Raven Biology of Plants (8th ed.). New York: W. H. Freeman and Company. pp. 213–17. ISBN 978-1-4292-1961-7.
- ↑ Evert, Ray F.; Eichhorn, Susan E. (2013). Raven Biology of Plants (8th ed.). New York: W.H. Freeman and Company. pp. 501–04. ISBN 9781429219617.
- ↑ Alison Mack; Janet Joy (2000). Marijuana As Medicine?: The Science Beyond the Controversy. National Academies Press. pp. 15–. ISBN 978-0-309-06531-3. https://books.google.com/books?id=ZriSkC7aQOEC&pg=PA15. Retrieved 20 December 2015.
- ↑ 79.0 79.1 Booth, Martin (2005). Cannabis: A History. New York: St. Martin's Press. ISBN 978-0-312-42494-7.
- ↑ 80.0 80.1 80.2 80.3 Grinspoon, Lester; Bakalar, James (1997). Marihuana, the Forbidden Medicine (Revised and expanded ed.). Yale University Press. ISBN 978-0-300-07086-6.
- ↑ Hans Bangen:Geschichte der medikamentösen Therapie der Schizophrenie. Berlin 1992, p. 22.
- ↑ (in en) Scientific American, "Successful Treatment of Tetanus". Munn & Company. 1880-07-10. pp. 25. https://books.google.com/books?id=6ok9AQAAIAAJ. Retrieved 5 June 2021.
- ↑ Pacula, Rosalie Piccardo (February 2002). "State Medical Marijuana Laws: Understanding the Laws and Their Limitations". Journal of Public Health Policy 23 (4): 413–39. doi:10.2307/3343240. PMID 12532682. http://impacteen.uic.edu/generalarea_PDFs/medicalmarijuanapaper100301.pdf. Retrieved 20 March 2018.
- ↑ Joy, Janet E.; Watson, Stanley J.; Benson, John A. (1999). "Marijuana and Medicine – Assessing the Science Base". Washington, D.C.: National Academy Press. http://medicalmarijuana.procon.org/sourcefiles/IOM_Report.pdf.
- ↑ "History of Marijuana as Medicine – 2900 BC to Present". http://medicalmarijuana.procon.org/view.timeline.php?timelineID=000026.
- ↑ "Marijuana's journey to legal health treatment: the Canadian experience". CBC News. 17 August 2009. http://www.cbc.ca/news/health/marijuana-s-journey-to-legal-health-treatment-the-canadian-experience-1.799488.
- ↑ Politi, Daniel (12 November 2020). "Argentina to Allow Medicinal Marijuana to Be Grown at Home". The New York Times. https://www.nytimes.com/2020/11/12/world/americas/argentina-cannabis-marijuana.html.
- ↑ Jolly, William (28 February 2018). "Medicinal Marijuana Legal In Australia". Canstar. https://www.canstar.com.au/health-insurance/victoria-legalises-medicinal-marijuana/.
- ↑ Ponieman, Natan (3 December 2019). "Brazil Regulates Sale Of Medical Marijuana Products". Benzinga. https://www.benzinga.com/markets/cannabis/19/12/14924387/brazil-regulates-sale-of-medical-marijuana-products.
- ↑ 90.0 90.1 90.2 90.3 90.4 90.5 90.6 90.7 Williams, Sean (15 May 2016). "10 Countries (Aside From the U.S.) Where Some Form of Medical Marijuana Is Legal". The Motley Fool. https://www.fool.com/investing/general/2016/05/15/10-countries-aside-from-the-us-where-some-form-of.aspx.
- ↑ "Costa Rica legalizes medicinal marijuana use, hemp growing". Associated Press. 2 March 2022. https://apnews.com/article/health-caribbean-marijuana-recreational-marijuana-costa-rica-7fc0e4e7b8881613210164f6acf6d9e8.
- ↑ Veselica, Lajla (15 October 2015). "Croatia legalises marijuana for medical use". Yahoo News. AFP. https://www.yahoo.com/news/croatia-allows-marijuana-medical-114920214.html.
- ↑ "Cyprus begins to distribute medical cannabis". InCyprus. 22 May 2017. http://in-cyprus.com/cyprus-begins-to-distribute-medical-cannabis.
- ↑ "Legal status of cannabis in Finland – An overview". https://sensiseeds.com/en/blog/legal-status-cannabis-finland-overview.
- ↑ Senthilingam, Meera (6 March 2017). "Germany joins the global experiment on marijuana legalization". CNN.com. http://www.cnn.com/2016/12/29/health/global-marijuana-cannabis-laws/index.html.
- ↑ Revesz, Rachael (3 July 2017). "Greece legalises marijuana for medical purposes". The Independent. https://www.independent.co.uk/news/world/europe/greece-marijuana-legal-medical-cannabis-weed-law-passes-a7821771.html.
- ↑ Schwartz, Yardena (24 August 2017). "How the Booming Israeli Weed Industry Is Changing American Pot". Rollingstone.com. https://www.rollingstone.com/culture/features/how-booming-israeli-weed-industry-is-changing-american-pot-w499117.
- ↑ Samuels, Gabriel (26 July 2016). "Italian army aims to produce "the best-quality" medical marijuana after finding current batches deficient". The Independent. https://www.independent.co.uk/news/world/europe/cannabis-italy-army-medical-marijuana-italian-military-produces-best-quality-weed-a7156176.html.
- ↑ Bud, Monterey (19 March 2018). "Jamaica's Kaya Farms Becomes First Medical Marijuana Dispensary To Open". marijuana.com. https://www.marijuana.com/news/2018/03/jamaicas-kaya-farms-becomes-first-medical-marijuana-dispensary-to-open.
- ↑ "Lebanon Legalizes Cannabis Farming for Medicinal Use". The New York Times. Reuters. 21 April 2020. https://www.nytimes.com/reuters/2020/04/21/world/middleeast/21reuters-lebanon-crisis-cannabis.html.
- ↑ Pritchard, Heledd (29 June 2018). "Cannabis for medical use legalised in Luxembourg". Luxembourg Times. https://luxtimes.lu/luxembourg/34274-cannabis-for-medical-use-legalised-in-luxembourg.
- ↑ Pace, Maria (27 March 2018). "Malta has officially legalised medical cannabis". Malta Today. https://www.maltatoday.com.mt/news/national/85616/malta_has_officially_legalised_medical_cannabis.
- ↑ "Morocco: Bill to legalise cannabis enters into force". Middle East Monitor. 31 July 2021. https://www.middleeastmonitor.com/20210731-morocco-bill-to-legalise-cannabis-enters-into-force/.
- ↑ Ainge Roy, Eleanor (11 December 2018). "New Zealand passes laws to make medical marijuana widely available". The Guardian. https://www.theguardian.com/world/2018/dec/11/new-zealand-passes-laws-to-make-medical-marijuana-widely-available.
- ↑ Marusic, Sinisa Jakov (1 June 2016). "Macedonia Allows Medical Marijuana in Pharmacies". Balkan Insight. http://www.balkaninsight.com/en/article/macedonia-allows-medical-marijuana-in-pharmacies-05-31-2016.
- ↑ "El gobierno de Panamá legalizó el uso medicinal y terapéutico del cannabis". Infobae. 14 October 2021. https://www.infobae.com/america/america-latina/2021/10/14/el-gobierno-de-panama-legalizo-el-uso-medicinal-y-terapeutico-del-cannabis/.
- ↑ Collyns, Dan (20 October 2017). "Peru legalises medical marijuana in move spurred by mother's home lab". The Guardian. https://www.theguardian.com/world/2017/oct/20/peru-marijuana-cannabis-legal-terminally-ill-children.
- ↑ "Medical use of cannabis officially legal in Poland". Radio Poland. PAP. 11 February 2017. http://www.thenews.pl/1/9/Artykul/333153,Medical-use-of-cannabis-officially-legal-in-Poland.
- ↑ Lamers, Matt (21 June 2018). "Portugal passes medical cannabis law, opens domestic market". Marijuana Business Daily. https://mjbizdaily.com/portugal-passes-medical-cannabis-law-opens-domestic-market/.
- ↑ Mwai, Collins (29 June 2021). "10 things to know after Rwanda gives the green light for medical marijuana". The New Times. https://www.newtimes.co.rw/article/187172/News/10-things-to-know-after-rwanda-gives-the-green-light-for-medical-marijuana.
- ↑ King, Chris (28 June 2022). "Congress approves the legalisation of medical cannabis in Spain". EuroWeekly News. https://euroweeklynews.com/2022/06/28/congress-approves-the-legalisation-of-medical-cannabis-in-spain/.
- ↑ South Asia Regional Profile, United Nations Office on Drugs and Crime, 15 September 2005, https://www.unodc.org/pdf/india/publications/south_Asia_Regional_Profile_Sept_2005/13_srilanka.pdf, retrieved 2 February 2019
- ↑ "Switzerland to legalise medicinal cannabis from Monday". The Local. 28 July 2022. https://www.thelocal.ch/20220728/switzerland-to-legalise-medicinal-cannabis-from-monday.
- ↑ Mosbergen, Dominique (25 December 2018). "Thailand Approves Medical Marijuana In Regional First". HuffPost. https://www.huffingtonpost.com/entry/thailand-medical-marijuana_us_5c22e6aae4b0407e907e7c18.
- ↑ "Medicinal cannabis products to be legalised". BBC. 26 July 2018. https://www.bbc.co.uk/news/health-44968386.
- ↑ "Sativex (delta-9-tetrahydrocannabinol and cannabidiol)". https://www.gwpharm.com/products-pipeline/sativex-delta-9-tetrahydrocannabinol-and-cannabidiol.
- ↑ Medical use of cannabis and cannabinoids, European Monitoring Centre for Drugs and Drug Addiction, December 2018, http://www.emcdda.europa.eu/system/files/publications/10171/20185584_TD0618186ENN_PDF.pdf, retrieved 11 December 2019
- ↑ Sapra, Bani (20 June 2018). "Canada becomes second nation in the world to legalize marijuana". CNN. https://www.cnn.com/2018/06/20/health/canada-legalizes-marijuana/index.html.
- ↑ Ives, Mike (10 November 2022). "Weed Is Now Legal in Thailand. How Long Will the High Times Last?". The New York Times. https://www.nytimes.com/2022/11/10/world/asia/thailand-weed-cannabis-law.html.
- ↑ Janikian, Michelle (14 September 2017). "Legal Pot In Mexico: Everything You Need to Know". Rolling Stone. https://www.rollingstone.com/culture/features/legal-pot-in-mexico-everything-you-need-to-know-w503038.
- ↑ Habibi, Roojin; Hoffman, Steven J. (March 2018). "Legalizing Cannabis Violates the UN Drug Control Treaties, But Progressive Countries Like Canada Have Options". Ottawa Law Review 49 (2). https://www.researchgate.net/publication/323697447. Retrieved 8 January 2021.
- ↑ "Classification of controlled drugs". https://www.emcdda.europa.eu/publications/topic-overviews/classification-of-controlled-drugs/html_en.
- ↑ Kaur, Harmeet (2 December 2020). "The UN removes cannabis from a list of the most dangerous substances". CNN. https://www.cnn.com/2020/12/02/health/un-reclassifies-cannabis-scn-trnd/index.html.
- ↑ Kwai, Isabella (2 December 2020). "U.N. Reclassifies Cannabis as a Less Dangerous Drug". The New York Times. https://www.nytimes.com/2020/12/02/world/europe/cannabis-united-nations-drug-policy.html.
- ↑ "WHO recommends rescheduling of cannabis". European Monitoring Centre for Drugs and Drug Addiction. 25 March 2019. https://www.emcdda.europa.eu/news/2019/who-recommends-rescheduling-of-cannabis_en.
- ↑ Georgiou, Aristos (8 February 2019). "WHO Recommends Rescheduling Cannabis in International Law for First Time in History". Newsweek. https://www.newsweek.com/who-recommends-rescheduling-cannabis-international-law-first-time-history-1324613.
- ↑ Ingraham, Christopher (13 June 2017). "Jeff Sessions personally asked Congress to let him prosecute medical-marijuana providers". The Washington Post. https://www.washingtonpost.com/news/wonk/wp/2017/06/13/jeff-sessions-personally-asked-congress-to-let-him-prosecute-medical-marijuana-providers/.
- ↑ Timothy B. Wheeler (11 October 2014). "Medical marijuana fees stir debate in Maryland". The Baltimore Sun. http://www.baltimoresun.com/news/maryland/sun-investigates/bs-md-medical-marijuana-fees-20141011,0,3253557.story?page=1.
- ↑ Blackwell, Tom (16 October 2013). "The pot vending machine's first foreign market? Canada, of course, "a seed for the rest of the world"". National Post. http://news.nationalpost.com/2013/10/16/pot-vending-machines-to-start-rolling-into-canada-after-firm-partners-with-u-s-company/.
- ↑ "Uber-For-Weed Startup Meadow Lights Up In San Francisco". TechCrunch. AOL. 14 October 2014. https://techcrunch.com/2014/10/14/uber-for-weed-startup-meadow-lights-up-in-san-francisco/.
- ↑ "The UK is the world's largest producer of legal Cannabis, UN body finds" (in en). 2018-03-07. https://www.independent.co.uk/news/uk/home-news/cannabis-legal-uk-worlds-largest-producer-marijuana-weed-un-body-findings-a8243921.html.
- ↑ Clark, Tonya Body (10 February 2015). "The Medical Marijuana Debate". Wolters Kluwer Financial Services. http://www.insurancecompliancecorner.com/the-medical-marijuana-debate/.
- ↑ Peters, Joey (29 June 2015). "Court: Employer can't block workers' comp for medical marijuana". http://nmpoliticalreport.com/4483/court-employer-cant-block-workers-comp-for-medical-marijuana/.
- ↑ "Resolution on Medical Marijuana". http://druglibrary.org/schaffer/hemp/medical/apha.htm.
- ↑ "House of Delegates 2017, Resolution: A8". American Medical Student Association. http://www.amsa.org/wp-content/uploads/2015/05/A8-Principles-Regarding-Illegal-drugs-alcohol-and-tobacco-1.pdf.
- ↑ "Medical Marijuana (Cannabis) FAQs". http://www.nationalmssociety.org/Treating-MS/Complementary-Alternative-Medicines/Marijuana/Marijuana-FAQs.
- ↑ Gattone PM, Lammert W (20 February 2014). "Epilepsy Foundation Calls for Increased Medical Marijuana Access and Research" (Press release). Washington, D.C.: Epilepsy Foundation. Archived from the original on 31 July 2017. Retrieved 30 July 2017.
- ↑ "Medical Marijuana Use and Research". Leukemia & Lymphoma Society. https://www.maps.org/research-archive/mmj/lnls-res.pdf.
- ↑ "Position Statement on Marijuana as Medicine". https://www.psychiatry.org/file%20library/about-apa/organization-documents-policies/policies/position-2013-marijuana-as-medicine.pdf.
- ↑ Use of Cannabis for Medicinal Purposes, American Medical Association, 2009, https://www.ama-assn.org/sites/default/files/media-browser/public/about-ama/councils/Council%20Reports/council-on-science-public-health/i09-csaph-medical-marijuana.pdf, retrieved 1 July 2017
- ↑ Supporting Research into the Therapeutic Role of Marijuana, American College of Physicians, February 2016, https://www.acponline.org/acp_policy/policies/supporting_research_therapeutic_role_of_marijuana_2016.pdf, retrieved 1 August 2017
- ↑ "ASAM Issues New Public Policy Statement on Cannabis" (Press release). Rockville, MD: American Society of Addiction Medicine. 13 October 2020. Archived from the original on 8 November 2020. Retrieved 1 November 2020.
- ↑ American Heart Association (5 August 2020). "Medical Marijuana, Recreational Cannabis, and Cardiovascular Health". Circulation 142 (10): e131–52. doi:10.1161/CIR.0000000000000883. PMID 32752884.
- ↑ "Marijuana and Cancer". https://www.cancer.org/treatment/treatments-and-side-effects/complementary-and-alternative-medicine/marijuana-and-cancer.html.
- ↑ "Marijuana research: Overcoming the barriers". American Psychological Association. 14 September 2017. http://advocacy.apascience.org/blog/2017/9/13/marijuana-research-overcoming-the-barriers.
- ↑ Arney, Kat (25 July 2012). "Cannabis, cannabinoids and cancer – the evidence so far". Cancer Research UK. http://scienceblog.cancerresearchuk.org/2012/07/25/cannabis-cannabinoids-and-cancer-the-evidence-so-far/.
- ↑ "Final Rule: Placement of FDA-Approved Products of Oral Solutions Containing Dronabinol [(-)-delta-9-trans-tetrahydrocannabinol (delta-9-THC) in Schedule II"]. https://www.deadiversion.usdoj.gov/fed_regs/rules/2017/fr1122_6.htm.
- ↑ Clark, Amy (16 May 2006). ""New" Pot Pill For Chemo Patients". CBS News. Associated Press. http://www.cbsnews.com/news/new-pot-pill-for-chemo-patients/.
- ↑ "Medical use of cannabis and cannabinoids containing products – Regulations in Europe and North America". European Journal of Internal Medicine 49: 2–6. March 2018. doi:10.1016/j.ejim.2018.01.001. PMID 29329891.
- ↑ "Produkt – FASS Allmänhet". fass.se. http://www.fass.se/LIF/product?1&docType=6&specId&userType&nplId=20101019000051.
- ↑ Youssef, Farid F. (June 2010). "Cannabis Unmasked: What it is and why it does what it does". UWIToday. https://sta.uwi.edu/uwitoday/archive/june_2010/article9.asp. Retrieved 11 May 2021.
- ↑ "Cannabis-Based Products for Chronic Pain: A Systematic Review". Ann Intern Med 175 (8): 1143–1153. 2022. doi:10.7326/M21-4520. PMID 35667066. https://www.acpjournals.org/doi/full/10.7326/M21-4520. Retrieved 19 February 2023.
Further reading
- National Academies Of Sciences, Engineering; Health Medicine, Division; Board on Population Health Public Health Practice; Committee on the Health Effects of Marijuana: An Evidence Review Research Agenda (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. National Academies of Sciences, Engineering, and Medicine: The National Academies Press. doi:10.17226/24625. ISBN 978-0-309-45304-2. http://nationalacademies.org/hmd/reports/2017/health-effects-of-cannabis-and-cannabinoids.aspx. Retrieved 7 February 2017.

External links
- Medical cannabis at Curlie, links to websites about medical cannabis
- Information on Cannabis and Cannabinoids from the U.S. National Cancer Institute
- Information on cannabis (marihuana, marijuana) and the cannabinoids from Health Canada
- The Center for Medicinal Cannabis Research of the University of California
- Medical Marijuana – a 2014–2015 three-part CNN documentary produced by Sanjay Gupta
- "Marijuana and Medical Marijuana collected news and commentary". http://topics.nytimes.com/top/reference/timestopics/subjects/m/marijuana/index.html.
 |
 KSF
KSF