Recombinant subunit vaccine
Topic: Medicine
 From HandWiki - Reading time: 14 min
From HandWiki - Reading time: 14 min

Recombinant subunit vaccines are biological preparations that are composed of microbial subunits produced using recombinant DNA technology. They act to provide active acquired immunity to infectious diseases. The first recombinant subunit vaccine was produced in the mid-1980s to protect people from Hepatitis B. Notable recombinant subunit vaccines licensed include ENGERIX-B (hepatitis B), GARDASIL-9[1] (Human Papillomavirus), FLUBLOK[2](influenza), SHINGRIX[3] (Herpes Zoster) and NUVAXOVID[4] (Coronavirus Disease 2019).
After injection, antigens trigger the production of antigen-specific antibodies, which are responsible for recognising and neutralising foreign substances. Basic components of recombinant subunit vaccines include recombinant subunits, adjuvants and carriers. Additionally, recombinant subunit vaccines are popular candidates for the development of vaccines against infectious diseases (e.g. tuberculosis,[5] dengue[6])
Recombinant subunit vaccines are considered to be safe for injection. The chances of adverse effects vary depending on the specific type of vaccine being administered. Minor side effects include injection site pain, fever, and fatigue, and serious adverse effects consist of anaphylaxis and potentially fatal allergic reaction. The contraindications are also vaccine-specific; they are generally not recommended for people with the previous history of anaphylaxis to any component of the vaccines. Advice from medical professionals should be sought before receiving any vaccination.
History
While the practice of immunisation can be traced back to the 12th century, in which ancient Chinese at that time employed the technique of variolation to confer immunity to smallpox infection,[citation needed] the modern era of vaccination has a short history of around 200 years. It began with the invention of a vaccine by Edward Jenner in 1798 to eradicate smallpox by injecting relatively weaker cowpox virus into the human body.
The middle of the 20th century marked the golden age of vaccine science.[citation needed] Rapid technological advancements during this period of time enabled scientists to cultivate cell culture under controlled environments in laboratories,[7] subsequently giving rise to the production of vaccines against poliomyelitis, measles and various communicable diseases.[citation needed] Conjugated vaccines were also developed using immunologic markers including capsular polysaccharide and proteins.[7] Creation of products targeting common illnesses successfully lowered infection-related mortality and reduced public healthcare burden.
Emergence of genetic engineering techniques revolutionised the creation of vaccines. By the end of the 20th century, researchers had the ability to create recombinant vaccines apart from traditional whole cell vaccines, for instance Hepatitis B vaccine, which uses the viral antigens to initiate immune responses.[7]
As the manufacturing methods continue to evolve, vaccines with more complex constitutions will inevitably be generated in the future to extend their therapeutic applications to both infectious and non-infectious diseases,[citation needed] in order to safeguard the health of more people.
Features
When compared with conventional attenuated vaccines and inactivated vaccines, recombinant subunit vaccines have the following special characteristics:
- They contain clearly identified compositions which greatly reduces the possibility of presence of undesired materials within the vaccine.[8]
- Their pathogenicities are minimized as only fragments of the pathogen are present in the vaccine which cannot invade and multiply within the human body.[9]
- They have better safety profiles[10] and are suitable to be administered to immunocompromised patients.[11]
- They are suitable for mass production due to the use of recombinant technologies.[8]
- They have high stability so they can withstand environmental changes and are more convenient to be used in community settings.[9]
However, there are also some drawbacks regarding recombinant subunit vaccines:
- Addition of adjuvants is necessary during manufacturing to increase the efficacy of these vaccines[12]
- Patients will have to receive booster doses to maintain long-term immunity[12][13]
- Selection of appropriate cell lines for the cultivation of subunits is time-consuming because microbial proteins can be incompatible to certain expression systems[13]
Pharmacology

Vaccination is a potent way to protect individuals against infectious diseases.[14]
Active immunity can be acquired artificially by vaccination as a result of the body's own defense mechanism being triggered by the exposure of a small, controlled amount of pathogenic substances to produce its own antibodies and memory cells without being infected by the real pathogen.[15]
The processes involved in primary immune response are as follows:
- Pre-exposure to the antigens present in vaccines elicits a primary response. After injection, antigens will be ingested by antigen-presenting cells (APCs), such as dendritic cells and macrophages, via phagocytosis.[15][16]
- The APCs will travel to lymph nodes, where immature B cells and T cells are present.[17]
- Following antigen processes by APCs, antigens will bind to either MHC class I receptors or MHC class II receptors on the cell surface of the cells based on their compositional and structural features to form complexes.[15]
- Antigen presentation occurs, in which T cell receptors attach to the antigen-MHC complexes, initiating clonal expansion and differentiation, and hence the conversion of naive T cells to cytotoxic T cells (CD8+) or helper T cells (CD4+).[18][19]
- Cytotoxic CD8+ cells can directly destroy the infected cells containing the antigens that were presented to them by the APCs by releasing lytic molecules, while helper CD4+ cells are responsible for the secretion of cytokines that activates B cells and cytotoxic T cells.[16][20]
- B cells can undergo activation in the absence of T cells via the B cell receptor signalling pathway.[16]
- After dendritic cells capture the immunogen present in the vaccine, they can present the substances to naive B cells, causing the proliferation of plasma cells for antibody production.[21] Isotype switching can take place during B cell development for the formation of different antibodies, including IgG, IgE and IgA.[16]
- Memory B cells and T cells are formed post-infection.[15] The antigens are memorised by these cells so that subsequent exposure to the same type of antigens will stimulate a secondary response, in which a higher concentration of antibodies specific for the antigens are reproduced rapidly and efficiently in a short time for the elimination of the pathogen.[17]
Under specific circumstances, low doses of vaccines are given initially, followed by additional doses named booster doses. Boosters can effectively maintain the level of memory cells in the human body, hence extending a person's immunity.[12][13][22]
Manufacturing
The manufacturing process of recombinant subunit vaccines are as follows:
- Identification of immunogenic subunit
- Subunit expression and synthesis
- Extraction and purification
- Addition of adjuvants or incorporation to vectors
- Formulation and delivery.
Identification of immunogenic subunit
Candidate subunits will be selected primarily by their immunogenicity.[23] To be immunogenic, they should be of foreign nature and of sufficient complexity for the reaction between different components of the immune system and the candidates to occur.[24] Candidates are also selected based on size, nature of function (e.g. signalling) and cellular location (e.g. transmembrane).[23]
Subunit expression and synthesis
Upon identifying the target subunit and its encoding gene, the gene will be isolated and transferred to a second, non-pathogenic organism, and cultured for mass production.[25] The process is also known as heterologous expression.
A suitable expression system is selected based on the requirement of post-translational modifications, costs, ease of product extraction and production efficiency. Commonly used systems for both licensed and developing recombinant subunit vaccines include bacteria, yeast, mammalian cells, insect cells.[26]
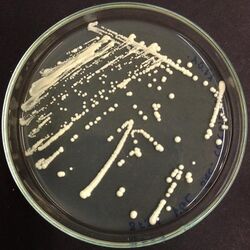
Bacterial cells
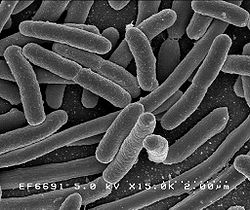
Bacterial cells are widely used for cloning processes, genetic modification and small-scale productions.[27] Escherichia coli (E. Coli) is widely utilised due to its highly explored genetics, widely available genetic tools for gene expression, accurate profiling and its ability to grow in inexpensive media at high cell densities.[28]
E. Coli is mostly appropriate for structurally simple proteins owing to its inability to carry out post-translational modifications, lack of protein secretary system and the potential for producing inclusion bodies that require additional solubilisation.[27][28][29] Regarding application, E.Coli is being utilised as the expression system of the currently developing dengue vaccine.[6]
Yeast
Yeast matches bacterial cells' cost-effectiveness, efficiency and technical feasibility.[27] Moreover, yeast secretes soluble proteins and has the ability to perform post-translational modifications similar to mammalian cells.[29]
Notably, yeast incorporates more mannose molecules during N-glycosylation when compared with other eukaryotes,[30] which may trigger cellular conformational stress responses. Such responses may result in failure in reaching native protein conformation, implying potential reduction of serum half-life and immunogenicity.[27] Regarding application, both the hepatitis B virus surface antigen (HBsAg) and the virus-like particles (VLPs) of the major capsid protein L1 of human papillomavirus type 6, 11, 16, 18 are produced by Saccharomyces cerevisiae. Currently, all commercialised therapeutic proteins to date are non-glycosylated.[28][29]
Mammalian cells
Mammalian cells are well known for their ability to perform therapeutically essential post-translational modifications and express properly folded, glycosylated and functionally active proteins.[28][31][32] However, efficacy of mammalian cells may be limited by epigenetic gene silencing and aggresome formation (recombinant protein aggregation).[28] For mammalian cells, synthesised proteins were reported to be secreted into chemically defined media, potentially simplifying protein extraction and purification.[27]
The most prominent example under this class is Chinese Hamster Ovary (CHO) cells utilised for the synthesis of recombinant varicella zoster virus surface glycoprotein (gE) antigen for SHINGRIX.[3] CHO cells are recognised for rapid growth and their ability to offer process versatility. They can also be cultured in suspension-adapted culture in protein-free medium, hence reducing risk of prion-induced contamination.[27][28]
Baculovirus (insect) cells

The baculovirus-insect cell expression system has the ability to express a variety of recombinant proteins at high levels and provide significant eukaryotic protein processing capabilities, including phosphorylation, glycosylation, myristoylation and palmitoylation.[33] Similar to mammalian cells, proteins expressed are mostly soluble, accurately folded, and biologically active.[34] However, it has slower growth rate and requires higher cost of growth medium than bacteria and yeast, and confers toxicological risks.[27] A notable feature is the existence of elements of control that allow for the expression of secreted and membrane-bound proteins in Baculovirus-insect cells.[27][33]
Licensed recombinant subunit vaccines that utilises baculovirus-insect cells include Cervarix (papillomavirus C-terminal truncated major capsid protein L1 types 16 and 18)[27][35] and Flublok Quadrivalent (hemagglutinin (HA) proteins from four strains of influenza viruses).[2]
Extraction and purification
Throughout history, extraction and purification methods have evolved from standard chromatographic methods to the utilisation of affinity tags.[36] However, the final extraction and purification process undertaken highly depends on the chosen expression system. Please refer to subunit expression and synthesis for more insights.
Addition of adjuvants
Adjuvants are materials added to improve immunogenicity of recombinant subunit vaccines.[37]
Adjuvants increase the magnitude of adaptive response to the vaccine and guide the activation of the most effective forms of immunity for each specific pathogen (e.g. increasing generation of T cell memory).[37][38][39][40] Addition of adjuvants may confer benefits including dose sparing and stabilisation of final vaccine formulation.[37][40]
Appropriate adjuvants are chosen based on safety, tolerance, compatibility of antigen and manufacturing considerations.[37] Commonly used adjuvants for recombinant subunit vaccines are Alum adjuvants (e.g. aluminium hydroxide), Emulsions (e.g. MF59) and Liposomes combined with immunostimulatory molecules (e.g. AS01B).[37][39]
Formulation and delivery
Delivery systems are primarily divided into polymer-based delivery systems (microspheres and liposomes) and live delivery systems (gram-positive bacteria, gram-negative bacteria and viruses)
Polymer-based delivery systems
Vaccine antigens are often encapsulated within microspheres or liposomes. Common microspheres made using Poly-lactic acid (PLA)[41] and poly-lactic-co-glycolic acid (PLGA)[41] allow for controlled antigen release by degrading in vivo while liposomes including multilamellar or unilamellar vesicles allow for prolonged release.[39]
Polymer-based delivery systems confer advantages such as increased resistance to degradation in GI tract, controlled antigen release, raised particle uptake by immune cells and enhanced ability to induce cytotoxic T cell responses.[39] An example of licensed recombinant vaccine utilising liposomal delivery is Shringrix.
Live delivery systems
Live delivery systems, also known as vectors, are cells modified with ligands or antigens to improve the immunogenicity of recombinant subunits via altering antigen presentation, biodistribution and trafficking.[42] Subunits may either be inserted within the carrier or genetically engineered to be expressed on the surface of the vectors for efficient presentation to the mucosal immune system.[25]
Adverse effects and contraindications
Recombinant subunit vaccines are safe for administration.[43][44] However, mild local reactions, including induration and swelling of the injection site, along with fever, fatigue and headache may be encountered after vaccination.[43][45][46] Occurrence of severe hypersensitivity reactions and anaphylaxis is rare,[47] but can possibly lead to deaths of individuals. Adverse effects can vary among populations depending on their physical health condition, age, gender and genetic predisposition.[48][49]
Recombinant subunit vaccines are contraindicated to people who have experienced allergic reactions and anaphylaxis to antigens or other components of the vaccines previously.[50][51] Furthermore, precautions should be taken when administering vaccines to people who are in diseased state and during pregnancy,[50] in which their injections should be delayed until their conditions become stable and after childbirth respectively.
Licensed vaccines
Hepatitis B

ENGERIX-B (produced by GSK) and RECOMBIVAX HB (produced by merck) are two recombinant subunit vaccines licensed for the protection against hepatitis B. Both contain HBsAg harvested and purified from Saccharomyces cerevisiae and are formulated as a suspension of the antigen adjuvanted with alum.[52][53]
Antibody concentration ≥10mIU/mL against HBsAg are recognized as conferring protection against hepatitis B infection.[52][53]
It has been shown that primary 3-dose vaccination of healthy individuals is associated with ≥90% seroprotection rates for ENGERIX-B, despite decreasing with older age. Lower seroprotection rates are also associated with presence of underlying chronic diseases and immunodeficiency. Yet, GSK HepB still has a clinically acceptable safety profile in all studied populations.[54]
Human Papillomavirus (HPV)

Cervarix, GARDASIL and GARDASIL9 are three recombinant subunit vaccines licensed for the protection against HPV infection. They differ in the strains which they protect the patients from as Cervarix confers protection against type 16 and 18,[35] GARDASIL confers protection against type 6, 11, 16 and 18,[55] and GARDASIL9 confers protection against type 6, 11, 16, 18, 31, 33, 45, 52, 58[1] respectively. The vaccines contain purified VLP of the major capsid L1 protein produced by recombinant Saccharomyces cerevisiae.
It has been shown in a 2014 systematic quantitative review that the bivalent HPV vaccine (Cervarix) is associated with pain (OR 3.29; 95% CI: 3.00–3.60), swelling (OR 3.14; 95% CI: 2.79–3.53) and redness (OR 2.41; 95% CI: 2.17–2.68) being the most frequently reported adverse effects. For GARDASIL, the most frequently reported events were pain (OR 2.88; 95% CI: 2.42–3.43) and swelling (OR 2.65; 95% CI: 2.0–3.44).[56]
GARDASIL was discontinued in the U.S. on May 8, 2017, after the introduction of GARDASIL9[57] and Cervarix was also voluntarily withdrawn in the U.S. on August 8, 2016.[58]
Influenza
Flublok Quadrivalent is a licensed recombinant subunit vaccine for active immunisation against influenza. It contains HA proteins of four strains of influenza virus purified and extracted using the Baculovirus-insect expression system. The four viral strains are standardised annually according to United States Public Health Services (USPHS) requirements.[2]
Flublok Quadrivalent has a comparable safety profile to traditional trivalent and quadrivalent vaccine equivalents. Flublok is also associated with less local reactions (RR = 0.94, 95% CI 0.90–0.98, three RCTs, FEM, I2 = 0%, low‐ certainty evidence) and higher risk of chills (RR = 1.33, 95% CI 1.03–1.72, three RCTs, FEM, I2 = 14%, low‐certainty evidence).[59]
Herpes Zoster
SHINGRIX is a licensed recombinant subunit vaccine for protection against Herpes Zoster, whose risk of developing increases with decline of varicella zoster virus (VZV) specific immunity. The vaccine contains VZV gE antigen component extracted from CHO cells, which is to be reconstituted with adjuvant suspension AS01B.[3]
Systematic reviews and meta-analyses have been conducted on the efficacy, effectiveness and safety of SHINGRIX in immunocompromised 18-49 year old patients and healthy adults aged 50 and over. These studies reported humoral and cell-mediated immunity rate ranged between 65.4 and 96.2% and 50.0%-93.0% while efficacy in patients (18-49 yo) with haematological malignancies was estimated at 87.2% (95%CI, 44.3–98.6%) up to 13 months post-vaccination with an acceptable safety profile.[60][61]
COVID-19
NUVAXOVID is a recombinant subunit vaccine licensed for the prevention of SARS-CoV-2 infection. Market authorization was issued on 20 December 2021.[62] The vaccine contains the SARS-CoV-2 spike protein produced using the baculovirus expression system, which is eventually adjuvanted with the Matrix M adjuvant.[4]
Research
Currently, recombinant subunit vaccines are used in development for Tuberculosis,[5] Dengue,[6] Soil-transmitted Helminths,[63] Feline Leukaemia[64] and COVID-19.[65]
COVID-19
Research has been conducted to explore the possibility of developing a heterologous SARS-CoV receptor-binding domain (RBD) recombinant protein as a human vaccine against COVID-19. The theory is supported by evidence that convalescent serum from SARS-CoV patients have the ability to neutralise SARS-CoV-2 (corresponding virus for COVID-19) and that amino acid similarity between SARS-CoV and SARS-CoV-2 spike and RBD protein is high (82%).[65] Category:Subunit vaccines
References
- ↑ 1.0 1.1 "GARDASIL®9(Human Papillomavirus 9-valent Vaccine, Recombinant)". https://www.fda.gov/media/90064/download.
- ↑ 2.0 2.1 2.2 "Flublok Quadrivalent (Influenza Vaccine)". https://www.fda.gov/media/123144/download.
- ↑ 3.0 3.1 3.2 "SHINGRIX (Zoster Vaccine Recombinant, Adjuvanted)". https://www.fda.gov/media/108597/download.
- ↑ 4.0 4.1 "Nuvaxovid dispersion for injection,COVID-19 Vaccine (recombinant, adjuvanted)". https://www.ema.europa.eu/en/documents/product-information/nuvaxovid-epar-product-information_en.pdf.
- ↑ 5.0 5.1 "Novel vaccine technologies for the 21st century". Nature Reviews. Immunology 20 (2): 87–88. February 2020. doi:10.1038/s41577-019-0243-3. PMID 31712767.
- ↑ 6.0 6.1 6.2 "Recent Developments in Recombinant Protein-Based Dengue Vaccines". Frontiers in Immunology 9: 1919. 2018-08-23. doi:10.3389/fimmu.2018.01919. PMID 30190720.
- ↑ 7.0 7.1 7.2 "History of vaccination". Proceedings of the National Academy of Sciences of the United States of America 111 (34): 12283–12287. August 2014. doi:10.1073/pnas.1400472111. PMID 25136134. Bibcode: 2014PNAS..11112283P.
- ↑ 8.0 8.1 "Cloning, Transformation and Expression of Proinsulin Gene in Tomato (Lycopersicum esculentum Mill.)". Jundishapur Journal of Natural Pharmaceutical Products 9 (1): 9–15. February 2014. doi:10.17795/jjnpp-7779. PMID 24644433.
- ↑ 9.0 9.1 "Active and passive immunity, vaccine types, excipients and licensing". Occupational Medicine 57 (8): 552–556. December 2007. doi:10.1093/occmed/kqm110. PMID 18045976.
- ↑ "Recombinant vaccines and the development of new vaccine strategies". Brazilian Journal of Medical and Biological Research 45 (12): 1102–1111. December 2012. doi:10.1590/S0100-879X2012007500142. PMID 22948379.
- ↑ "Recent advances in the production of recombinant subunit vaccines in Pichia pastoris". Bioengineered 7 (3): 155–165. April 2016. doi:10.1080/21655979.2016.1191707. PMID 27246656.
- ↑ 12.0 12.1 12.2 "Recombinant influenza vaccines". Acta Naturae 4 (4): 17–27. October 2012. doi:10.32607/20758251-2012-4-4-17-27. PMID 23346377.
- ↑ 13.0 13.1 13.2 Production and delivery of recombinant subunit vaccines. OCLC 1301470908. http://worldcat.org/oclc/1301470908.
- ↑ "Impact of Vaccines; Health, Economic and Social Perspectives". Frontiers in Microbiology 11: 1526. 2020-07-14. doi:10.3389/fmicb.2020.01526. PMID 32760367.
- ↑ 15.0 15.1 15.2 15.3 "Fundamentals of vaccine immunology". Journal of Global Infectious Diseases 3 (1): 73–78. January 2011. doi:10.4103/0974-777X.77299. PMID 21572612.
- ↑ 16.0 16.1 16.2 16.3 "Designs of Antigen Structure and Composition for Improved Protein-Based Vaccine Efficacy". Frontiers in Immunology 11 (283): 283. 24 February 2020. doi:10.3389/fimmu.2020.00283. PMID 32153587.
- ↑ 17.0 17.1 "B lymphocytes: how they develop and function". Blood 112 (5): 1570–1580. September 2008. doi:10.1182/blood-2008-02-078071. PMID 18725575.
- ↑ "Vaccines: Underlying Principles of Design and Testing". Clinical Pharmacology and Therapeutics 109 (4): 987–999. April 2021. doi:10.1002/cpt.2207. PMID 33705574.
- ↑ "CD8 T cell clonal expansion and development of effector function require prolonged exposure to antigen, costimulation, and signal 3 cytokine". Journal of Immunology 171 (10): 5165–5171. November 2003. doi:10.4049/jimmunol.171.10.5165. PMID 14607916.
- ↑ "B cells promote CD8 T cell primary and memory responses to subunit vaccines". Cell Reports 36 (8): 109591. August 2021. doi:10.1016/j.celrep.2021.109591. PMID 34433030.
- ↑ "Dendritic cell-B-cell interaction: dendritic cells provide B cells with CD40-independent proliferation signals and CD40-dependent survival signals". Immunology 100 (1): 1–3. May 2000. doi:10.1046/j.1365-2567.2000.00044.x. PMID 10809952.
- ↑ "Booster vaccination strategy: Necessity, immunization objectives, immunization strategy, and safety". Journal of Medical Virology 94 (6): 2369–2375. June 2022. doi:10.1002/jmv.27590. PMID 35028946.
- ↑ 23.0 23.1 "Selection of protein epitopes for antibody production". BioTechniques 38 (5): 723–727. May 2005. doi:10.2144/05385ST02. PMID 15945371.
- ↑ "Chapter 4 The nature of immunogens, antigens, and haptens" (in en). Laboratory Techniques in Biochemistry and Molecular Biology. Practice and Theory of Enzyme Immunoassays. 15. Elsevier. 1985-01-01. pp. 39–41. doi:10.1016/S0075-7535(08)70134-7. ISBN 9780444806345.
- ↑ 25.0 25.1 "Production of recombinant subunit vaccines: protein immunogens, live delivery systems and nucleic acid vaccines". Journal of Biotechnology 73 (1): 1–33. July 1999. doi:10.1016/s0168-1656(99)00107-8. PMID 10483112.
- ↑ "Recent Advances in Vaccine Technologies". The Veterinary Clinics of North America. Small Animal Practice 48 (2): 231–241. March 2018. doi:10.1016/j.cvsm.2017.10.002. PMID 29217317.
- ↑ 27.0 27.1 27.2 27.3 27.4 27.5 27.6 27.7 27.8 "Microbial factories for recombinant pharmaceuticals". Microbial Cell Factories 8 (1): 17. March 2009. doi:10.1186/1475-2859-8-17. PMID 19317892.
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 "Unconventional microbial systems for the cost-efficient production of high-quality protein therapeutics". Biotechnology Advances 31 (2): 140–153. 2013. doi:10.1016/j.biotechadv.2012.09.001. PMID 22985698.
- ↑ 29.0 29.1 29.2 "Advances and needs for endotoxin-free production strains". Applied Microbiology and Biotechnology 99 (22): 9349–9360. November 2015. doi:10.1007/s00253-015-6947-9. PMID 26362682.
- ↑ "Advances in the production of human therapeutic proteins in yeasts and filamentous fungi". Nature Biotechnology 22 (11): 1409–1414. November 2004. doi:10.1038/nbt1028. PMID 15529166.
- ↑ "Mammalian cell protein expression for biopharmaceutical production". Biotechnology Advances 30 (5): 1158–1170. 2012. doi:10.1016/j.biotechadv.2011.08.022. PMID 21968146.
- ↑ "Cell factories for insulin production". Microbial Cell Factories 13 (1): 141. October 2014. doi:10.1186/s12934-014-0141-0. PMID 25270715.
- ↑ 33.0 33.1 "Baculovirus-insect cell expression systems". Methods in Enzymology (Elsevier) 463: 191–222. 2009. doi:10.1016/s0076-6879(09)63014-7. PMID 19892174.
- ↑ "Baculovirus expression vector system". Gene Expression Systems. Elsevier. 1999. pp. 331–363.
- ↑ 35.0 35.1 "CERVARIX [Human Papillomavirus Bivalent (Types 16 and 18) Vaccine, Recombinant"]. https://www.fda.gov/media/78013/download.
- ↑ "Overview of the purification of recombinant proteins". Current Protocols in Protein Science 80 (1): 6.1.1–6.1.35. April 2015. doi:10.1002/0471140864.ps0601s80. PMID 25829302.
- ↑ 37.0 37.1 37.2 37.3 37.4 "Overview of Vaccine Adjuvants: Introduction, History, and Current Status" (in en). Vaccine Adjuvants. Methods in Molecular Biology. 1494. New York, NY: Springer New York. 2017. pp. 1–13. doi:10.1007/978-1-4939-6445-1_1. ISBN 978-1-4939-6443-7.
- ↑ "Vaccine adjuvants: putting innate immunity to work". Immunity 33 (4): 492–503. October 2010. doi:10.1016/j.immuni.2010.10.002. PMID 21029960.
- ↑ 39.0 39.1 39.2 39.3 "Preparation of recombinant vaccines". Biotechnology Annual Review (Elsevier) 13: 65–94. 2007. doi:10.1016/s1387-2656(07)13004-0. ISBN 978-0-444-53032-5. PMID 17875474.
- ↑ 40.0 40.1 "Safety and Mechanism of Action of Licensed Vaccine Adjuvants". International Current Pharmaceutical Journal 4 (8): 420–431. 2015-07-06. doi:10.3329/icpj.v4i8.24024. ISSN 2224-9486. http://dx.doi.org/10.3329/icpj.v4i8.24024.
- ↑ 41.0 41.1 "Recent research and development of PLGA/PLA microspheres/nanoparticles: A review in scientific and industrial aspects". Frontiers of Chemical Science and Engineering 13 (1): 14–27. 2018-06-09. doi:10.1007/s11705-018-1729-4. ISSN 2095-0179.
- ↑ "Recent Advances in Subunit Vaccine Carriers". Vaccines 4 (2): 12. April 2016. doi:10.3390/vaccines4020012. PMID 27104575.
- ↑ 43.0 43.1 "Safety of Human Papillomavirus 9-Valent Vaccine: A Meta-Analysis of Randomized Trials". Journal of Immunology Research 2017: 3736201. 2017. doi:10.1155/2017/3736201. PMID 28812030.
- ↑ "Safety, efficacy, and immunogenicity of Flublok in the prevention of seasonal influenza in adults". Therapeutic Advances in Vaccines 3 (4): 97–108. July 2015. doi:10.1177/2051013615595595. PMID 26478817.
- ↑ "Shingrix: The New Adjuvanted Recombinant Herpes Zoster Vaccine". The Annals of Pharmacotherapy 52 (7): 673–680. July 2018. doi:10.1177/1060028018758431. PMID 29457489.
- ↑ "Possible Side effects from Vaccines | CDC" (in en-us). 2022-04-06. https://www.cdc.gov/vaccines/vac-gen/side-effects.htm.
- ↑ "Vaccine-associated hypersensitivity". The Journal of Allergy and Clinical Immunology 141 (2): 463–472. February 2018. doi:10.1016/j.jaci.2017.12.971. PMID 29413255.
- ↑ "Sex and Gender Impact Immune Responses to Vaccines Among the Elderly". Physiology 30 (6): 408–416. November 2015. doi:10.1152/physiol.00035.2015. PMID 26525340.
- ↑ "Genetic predisposition for adverse events after vaccination". The Journal of Infectious Diseases 196 (2): 176–177. July 2007. doi:10.1086/518800. PMID 17570102.
- ↑ 50.0 50.1 "ACIP Contraindications Guidelines for Immunization | CDC" (in en-us). 2022-03-22. https://www.cdc.gov/vaccines/hcp/acip-recs/general-recs/contraindications.html.
- ↑ Public Health Agency of Canada (2007-07-18). "Contraindications and precautions: Canadian Immunization Guide". https://www.canada.ca/en/public-health/services/publications/healthy-living/canadian-immunization-guide-part-2-vaccine-safety/page-3-contraindications-precautions-concerns.html.
- ↑ 52.0 52.1 "RECOMBIVAX HB® Hepatitis B Vaccine (Recombinant)". https://www.fda.gov/files/vaccines%2C%20blood%20%26%20biologics/published/package-insert-recombivax-hb.pdf.
- ↑ 53.0 53.1 "ENGERIX-B [Hepatitis B Vaccine (Recombinant)"]. https://www.fda.gov/files/vaccines%2C%20blood%20%26%20biologics/published/Package-Insert---ENGERIX-B.pdf.
- ↑ "The immunogenicity and safety of GSK's recombinant hepatitis B vaccine in adults: a systematic review of 30 years of experience". Expert Review of Vaccines 16 (8): 811–832. August 2017. doi:10.1080/14760584.2017.1338568. PMID 28573913.
- ↑ "GARDASIL®[Human Papillomavirus Quadrivalent (Types 6, 11, 16, and 18) Vaccine, Recombinant"]. https://www.fda.gov/files/vaccines,%20blood%20&%20biologics/published/Package-Insert---Gardasil.pdf.
- ↑ "Safety, tolerability and side effects of human papillomavirus vaccines: a systematic quantitative review". The Brazilian Journal of Infectious Diseases 18 (6): 651–659. 2014. doi:10.1016/j.bjid.2014.02.005. PMID 24780368.
- ↑ "Gardasil-4 is no longer available.". 23 May 2022. https://www.cdc.gov/vaccines/hcp/vis/what-is-new.html.
- ↑ "GSK exits U.S. market with its HPV vaccine Cervarix" (in en). 2016-10-21. https://www.fiercepharma.com/pharma/gsk-exits-u-s-market-its-hpv-vaccine-cervarix.
- ↑ "Systematic review of the efficacy, effectiveness and safety of recombinant haemagglutinin seasonal influenza vaccines for the prevention of laboratory-confirmed influenza in individuals ≥18 years of age". Reviews in Medical Virology: e2331. February 2022. doi:10.1002/rmv.2331. PMID 35106885.
- ↑ "A systematic literature review of the recombinant subunit herpes zoster vaccine use in immunocompromised 18-49 year old patients". Vaccine 38 (40): 6205–6214. September 2020. doi:10.1016/j.vaccine.2020.07.049. PMID 32788132.
- ↑ "Efficacy, effectiveness, and safety of herpes zoster vaccines in adults aged 50 and older: systematic review and network meta-analysis". BMJ 363: k4029. October 2018. doi:10.1136/bmj.k4029. PMID 30361202.
- ↑ "Nuvaxovid COVID-19 Vaccine (recombinant, adjuvanted)". https://www.ema.europa.eu/en/medicines/human/EPAR/nuvaxovid#authorisation-details-section.
- ↑ "Recombinant subunit vaccines for soil-transmitted helminths". Parasitology 144 (14): 1845–1870. December 2017. doi:10.1017/S003118201700138X. PMID 28770689.
- ↑ "Genetically-engineered subunit vaccine against feline leukaemia virus: protective immune response in cats". Vaccine 9 (2): 89–96. February 1991. doi:10.1016/0264-410x(91)90262-5. PMID 1647576.
- ↑ 65.0 65.1 "Potential for developing a SARS-CoV receptor-binding domain (RBD) recombinant protein as a heterologous human vaccine against coronavirus infectious disease (COVID)-19". Human Vaccines & Immunotherapeutics 16 (6): 1239–1242. June 2020. doi:10.1080/21645515.2020.1740560. PMID 32298218.
This article needs additional or more specific categories. (June 2022) |
 KSF
KSF