Therapeutic ultrasound
Topic: Medicine
 From HandWiki - Reading time: 8 min
From HandWiki - Reading time: 8 min
| Therapeutic ultrasound | |
|---|---|
| ICD-10-PCS | 6A7 |
| ICD-9-CM | 00.0 |
Therapeutic ultrasound refers generally to any type of ultrasonic procedure that uses ultrasound for therapeutic benefit. Physiotherapeutic ultrasound was introduced into clinical practice in the 1950s, with lithotripsy introduced in the 1980s. Others are at various stages in transitioning from research to clinical use: HIFU, targeted ultrasound drug delivery, trans-dermal ultrasound drug delivery, ultrasound hemostasis, cancer therapy, and ultrasound assisted thrombolysis[1][2] It may use focused ultrasound (FUS) or unfocused ultrasound.
In the above applications, the ultrasound passes through human tissue where it is the main source of the observed biological effect (the oscillation of abrasive dental tools at ultrasonic frequencies therefore do not belong to this class). The ultrasound within tissue consists of very high frequency sound waves, between 800,000 Hz and 20,000,000 Hz, which cannot be heard by humans.
There is some evidence that ultrasound is more effective than placebo treatment for treating patients with arthritis pain,[3] a range of musculoskeletal injuries[4] and for promoting tissue healing.[5]
Medical uses
Relatively high power ultrasound can break up stony deposits or tissue, accelerate the effect of drugs in a targeted area, assist in the measurement of the elastic properties of tissue, and can be used to sort cells or small particles for research.
- Focused high-energy ultrasound pulses can be used to break calculi such as kidney stones and gallstones into fragments small enough to be passed from the body without undue difficulty, a process known as lithotripsy.
- Focused ultrasound sources may be used for cataract treatment by phacoemulsification.
- Ultrasound can ablate tumors or other tissue non-invasively. This is accomplished using a technique known as High Intensity Focused Ultrasound (HIFU), also called focused ultrasound surgery (FUS surgery). This procedure uses generally lower frequencies than medical diagnostic ultrasound (250–2000 kHz), but significantly higher time-averaged intensities. The treatment is often guided by Magnetic Resonance Imaging (MRI); the combination is then referred to as Magnetic resonance-guided focused ultrasound (MRgFUS).
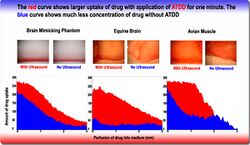
- Delivering chemotherapy to brain cancer cells and various drugs to other tissues is called acoustic targeted drug delivery (ATDD).[6] These procedures generally use high frequency ultrasound (1–10 MHz) and a range of intensities (0–20 W/cm2). The acoustic energy is focused on the tissue of interest to agitate its matrix and make it more permeable for therapeutic drugs.[7]
- Ultrasound has been used to trigger the release of anti-cancer drugs from delivery vectors including liposomes, polymeric microspheres and self-assembled polymeric.[1]
- Ultrasound is essential to the procedures of ultrasound-guided sclerotherapy and endovenous laser treatment for the non-surgical treatment of varicose veins.
- Ultrasound-assisted lipectomy is Liposuction assisted by ultrasound.
- Phonophoresis is a form of soft tissue treatment that involves the use of ultrasound combined with medication gels and will utilize ultrasound waves to enhance drug delivery to the injured area.[3]
There are three potential effects of ultrasound. The first is the increase in blood flow in the treated area.[citation needed] The second is the decrease in pain from the reduction of swelling and edema[citation needed]. The third is the gentle massage of muscle tendons and/ or ligaments in the treated area because no strain is added and any scar tissue is softened[citation needed]. These three benefits are achieved by two main effects of therapeutic ultrasound. The two types of effects are: thermal and non thermal effects. Thermal effects are due to the absorption of the sound waves. Non thermal effects are from cavitation, microstreaming and acoustic streaming.[1]
Cavitational effects result from the vibration of the tissue causing microscopic bubbles to form, which transmit the vibrations in a way that directly stimulates cell membranes. This physical stimulation appears to enhance the cell-repair effects of the inflammatory response.
History
The first large scale application of ultrasound was around World War II. Sonar systems were being built and used to navigate submarines. It was realized that the high intensity ultrasound waves that they were using were heating and killing fish.[8] This led to research in tissue heating and healing effects. Since the 1940s, ultrasound has been used by physical and occupational therapists for therapeutic effects.
Physical therapy
Ultrasound is applied using a transducer or applicator that is in direct contact with the patient's skin. Gel is used on all surfaces of the head to reduce friction and assist transmission of the ultrasonic waves. Therapeutic ultrasound in physical therapy is alternating compression and rarefaction of sound waves with a frequency of 0.7 to 3.3 MHz. Maximum energy absorption in soft tissue occurs from 2 to 5 cm. Intensity decreases as the waves penetrate deeper. They are absorbed primarily by connective tissue: ligaments, tendons, and fascia (and also by scar tissue).[9]
Conditions for which ultrasound may be used for treatment include the following examples: ligament sprains, muscle strains, tendonitis, joint inflammation, plantar fasciitis, metatarsalgia, facet irritation, impingement syndrome, bursitis, rheumatoid arthritis, osteoarthritis, and scar tissue adhesion. There is no evidence to support the use of ultrasound for the treatment of low back pain,[10] and current clinical guidelines recommend that ultrasound is not used for this condition.[11] In a critical review, it was demonstrated that therapeutic ultra sound was effective in improving pain, function, and cartilage repair in knee osteoarthritis. Another systematic review and meta-analysis of low-intensity pulsed ultra sound on knee osteoarthritis a significant effect on pain reduction and knee functional recovery was demonstrated.[12] Ultrasound used for calcific tendonitis had a positive short term effect. For the long term, there was no significant difference with ultrasound use. This shows that for pain relief and short-term treatment ultrasound can be an effective treatment for Calcific Tendonitis[13] A review with five small placebo‐controlled trials from 2011, did not support the use of ultrasound in the treatment of acute ankle sprains and the potential treatment effects of ultrasound appear to be generally small and of probably of limited clinical importance, especially in the context of the usually short‐term recovery period for these injuries.[14] However, therapeutic ultrasound is reported to have beneficial effects in sports injuries pain relief, edema control, and range of joint motion, possibly by increasing pain thresholds, collagen extensibility, reducing edema, and therefore inflammation, muscle spasms, and joint stiffness.[12] A meta-analysis found that ultrasound therapy is effective in reducing pain, increasing ROM, and reducing WOMAC functional scores in patients with knee osteoarthritis.[3]
Knee Oseteoarthritis
According to recent research, therapeutic ultrasound has not shown any significant improvement for chronic low back pain, chronic neck pain, and hip pain in combination with other physiotherapeutic techniques.[15][16] However, the most conclusive evidence to support therapeutic ultrasound use is seen with its use in patients with knee osteoarthritis. Knee osteoarthritis affects approximately 250 million people worldwide.[17] While there is no known cure, therapeutic regimens are often used to intervene with the diseases chronic symptoms.[17] In a systematic review of 15 studies, patients who received ultrasound treatments were compared to those who received a placebo treatment. The evidence demonstrated that therapeutic ultrasound significantly relieved pain, increases range of motion, and reduced WOMAC functional scores in patients with knee osteoarthritis when compared to the placebo group.[3] In a separate meta-analysis, it reinforced the use of therapeutic ultrasound by deeming it as a safe non-pharmalogical treatment option that may provide additional pain relief as well as functional improvement when used secondarily to therapy in patients with knee osteoarthritis.[17]
Research tools
- Acoustic tweezers is an emerging tool for contactless separation, concentration and manipulation of microparticles and biological cells, using ultrasound in the low MHz range to form standing waves. This is based on the acoustic radiation force which causes particles to be attracted to either the nodes or anti-nodes of the standing wave depending on the acoustic contrast factor, which is a function of the sound velocities and densities of the particle and of the medium in which the particle is immersed.
- Application of focused ultrasound in conjunction with microbubbles has been shown to enable non-invasive delivery of epirubicin across the blood–brain barrier in mouse models [1] and non invasive delivery of GABA in non human primates.[18]
Research
- Using ultrasound to generate cellular effects in soft tissue has fallen out of favor as research has shown a lack of efficacy[19] and a lack of scientific basis for proposed biophysical effects.[20]
- According to a 2017 meta-analysis and associated practice guideline, Low intensity pulsed ultrasound should no longer been used for bone regeneration because high quality clinical studies failed to demonstrate a clinical benefit.[21][22]
- An additional effect of low-intensity ultrasound could be its potential to disrupt the blood–brain barrier for drug delivery.[23]
- Transcranial ultrasound is being tested for use in aiding tissue plasminogen activator treatment in stroke patients in the procedure called ultrasound-enhanced systemic thrombolysis.
- Ultrasound has been shown to act synergistically with antibiotics in killing bacteria.[24]
- Ultrasound has been postulated to allow thicker eukaryotic cell tissue cultures by promoting nutrient penetration.[25]
- Long-duration therapeutic ultrasound called sustained acoustic medicine is a daily slow-release therapy that can be applied to increase local circulation and theoretically accelerates healing of musculoskeletal tissues after an injury.[26] However, there is some evidence to suggest this may not be effective.[19]
See also
References
- ↑ 1.0 1.1 1.2 1.3 "Ultrasound-enhanced drug delivery for cancer". Expert Opinion on Drug Delivery 9 (12): 1525–1538. December 2012. doi:10.1517/17425247.2012.739603. PMID 23121385.
- ↑ "Therapeutic Ultrasound: A Promising Future in Clinical Medicine". http://www.acoustics.org/press/135th/crum.htm.
- ↑ 3.0 3.1 3.2 3.3 "Effects of therapeutic ultrasound for knee osteoarthritis: a systematic review and meta-analysis". Clinical Rehabilitation 33 (12): 1863–1875. December 2019. doi:10.1177/0269215519866494. PMID 31382781.
- ↑ "Low-Intensity Continuous Ultrasound Therapies—A Systematic Review of Current State-of-the-Art and Future Perspectives". Journal of Clinical Medicine 10 (12): 2698. June 2021. doi:10.3390/jcm10122698. PMID 34207333.
- ↑ "Low intensity pulsed ultrasound (LIPUS) use for the management of instrumented, infected, and fragility non-unions: a systematic review and meta-analysis of healing proportions". BMC Musculoskeletal Disorders 22 (1): 532. June 2021. doi:10.1186/s12891-021-04322-5. PMID 34116673.
- ↑ "Acoustically enhanced Evans blue dye perfusion in neurological tissues". The Journal of the Acoustical Society of America 2 (1): 20001–200017. February 2008. doi:10.1121/1.2890703. PMID 21197390.
- ↑ "A phantom feasibility study of acoustic enhanced drug perfusion in neurological tissue". 2007 IEEE/NIH Life Science Systems and Applications Workshop. 2007. p. 67. doi:10.1109/LSSA.2007.4400886. ISBN 978-1-4244-1812-1. https://zenodo.org/record/1237350.
- ↑ "A short History of the development of Ultrasound in Obstetrics and Gynecology". esource Discovery Network, University of Oxford. http://www.ob-ultrasound.net/history1.html.
- ↑ "Therapeutic Ultrasound". herapeutic Ultrasound on the web. 2006. http://www.electrotherapy.org/electro/ultrasound/therapeutic_ultrasound.htm.
- ↑ "Therapeutic ultrasound for chronic low back pain". The Cochrane Database of Systematic Reviews 2020 (7): CD009169. July 2020. doi:10.1002/14651858.CD009169.pub3. PMID 32623724.
- ↑ National Institute for Health and Care Excellence (2016). Low back pain and sciatica in over 16s: assessment and management.. Manchester: National Institute for Health and Care Excellence (NICE). ISBN 978-1-4731-2186-7. OCLC 1198756858. https://www.worldcat.org/oclc/1198756858.
- ↑ 12.0 12.1 "The Role of Ultrasound Therapy in the Management of Musculoskeletal Soft Tissue Pain". The International Journal of Lower Extremity Wounds 19 (4): 350–358. December 2020. doi:10.1177/1534734620948343. PMID 32856521.
- ↑ "Long-Term Course of Shoulders After Ultrasound Therapy for Calcific Tendinitis: Results of the 10-Year Follow-Up of a Randomized Controlled Trial". American Journal of Physical Medicine & Rehabilitation 97 (9): 651–658. September 2018. doi:10.1097/PHM.0000000000000939. PMID 29613883.
- ↑ "Therapeutic ultrasound for acute ankle sprains". The Cochrane Database of Systematic Reviews 2011 (6): CD001250. June 2011. doi:10.1002/14651858.cd001250.pub2. PMID 21678332.
- ↑ "Therapeutic Ultrasound for Chronic Pain Management in Joints: A Systematic Review". Pain Medicine 21 (7): 1437–1448. November 2020. doi:10.1093/pm/pnz102. PMID 31095336.
- ↑ "Therapeutic Ultrasound for Pain Management in Chronic Low Back Pain and Chronic Neck Pain: A Systematic Review". Pain Medicine 21 (7): 1482–1493. November 2020. doi:10.1093/pm/pny287. PMID 30649460.
- ↑ 17.0 17.1 17.2 "Therapeutic ultrasound for knee osteoarthritis: A systematic review and meta-analysis with grade quality assessment". Brazilian Journal of Physical Therapy 25 (6): 688–697. November 2021. doi:10.1016/j.bjpt.2021.07.003. PMID 34535411.
- ↑ "Non-invasive ultrasonic modulation of visual evoked response by GABA delivery through the blood brain barrier". Journal of Controlled Release 318: 223–231. February 2020. doi:10.1016/j.jconrel.2019.12.006. PMID 31816362.
- ↑ 19.0 19.1 "A review of therapeutic ultrasound: effectiveness studies". Physical Therapy 81 (7): 1339–1350. July 2001. doi:10.1093/ptj/81.7.1339. PMID 11444997.
- ↑ "A review of therapeutic ultrasound: biophysical effects". Physical Therapy 81 (7): 1351–1358. July 2001. doi:10.1093/ptj/81.7.1351. PMID 11444998.
- ↑ "Low intensity pulsed ultrasound for bone healing: systematic review of randomized controlled trials". BMJ 356: j656. February 2017. doi:10.1136/bmj.j656. PMID 28348110.
- ↑ "Low intensity pulsed ultrasound (LIPUS) for bone healing: a clinical practice guideline". BMJ 356: j576. February 2017. doi:10.1136/bmj.j576. PMID 28228381.
- ↑ "Permeability dependence study of the focused ultrasound-induced blood-brain barrier opening at distinct pressures and microbubble diameters using DCE-MRI". Magnetic Resonance in Medicine 66 (3): 821–830. September 2011. doi:10.1002/mrm.22848. PMID 21465543.
- ↑ "Ultrasonically enhanced vancomycin activity against Staphylococcus epidermidis biofilms in vivo". Journal of Biomaterials Applications 18 (4): 237–245. April 2004. doi:10.1177/0885328204040540. PMID 15070512.
- ↑ "Ultrasound increases the rate of bacterial cell growth". Biotechnology Progress 19 (3): 1038–1044. 2003. doi:10.1021/bp0340685. PMID 12790676.
- ↑ "Intramuscular Heating Characteristics of Multihour Low-Intensity Therapeutic Ultrasound". Journal of Athletic Training 50 (11): 1158–1164. November 2015. doi:10.4085/1062-6050-50.11.03. PMID 26509683.
External links
- "Video: Physical Therapy Ultrasound; What is it?". YouTube. 12 March 2014. https://www.youtube.com/watch?v=xJ7tAdLduUI.
- "Therapeutic Ultrasound". Physiopedia. 2006. http://www.physio-pedia.com/Ultrasound_therapy.
- "International Society for Therapeutic Ultrasound". http://www.istu.org/.
 |
 KSF
KSF