Upper respiratory tract infection
Topic: Medicine
 From HandWiki - Reading time: 12 min
From HandWiki - Reading time: 12 min
| Upper respiratory tract infection | |
|---|---|
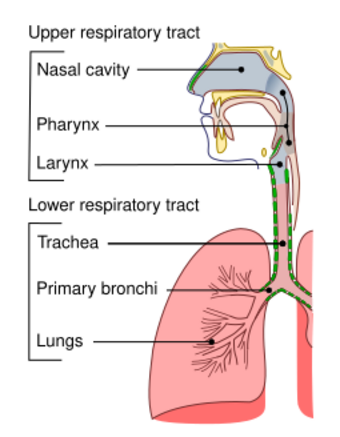 | |
| Conducting passages. | |
| Specialty | Infectious disease |
| Frequency | (2015)[1] |
| Deaths | 3,100[2] |
An upper respiratory tract infection (URTI) is an illness caused by an acute infection, which involves the upper respiratory tract, including the nose, sinuses, pharynx, larynx or trachea.[3][4] This commonly includes nasal obstruction, sore throat, tonsillitis, pharyngitis, laryngitis, sinusitis, otitis media, and the common cold.[5]: 28 Most infections are viral in nature, and in other instances, the cause is bacterial.[6] URTIs can also be fungal or helminthic in origin, but these are less common.[7]: 443–445
In 2015, 17.2 billion cases of URTIs are estimated to have occurred.[1] As of 2016, they caused about 3,000 deaths, down from 4,000 in 1990.[8]
Signs and symptoms
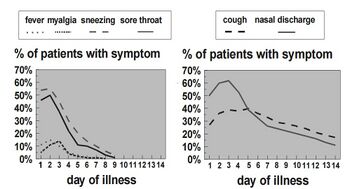
In uncomplicated colds, coughing and nasal discharge may persist for 14 days or more even after other symptoms have resolved.[6] Acute URTIs include rhinitis, pharyngitis/tonsillitis, and laryngitis often referred to as a common cold, and their complications: sinusitis, ear infection, and sometimes bronchitis (though bronchi are generally classified as part of the lower respiratory tract.) Symptoms of URTIs commonly include cough, sore throat, runny nose, nasal congestion, headache, low-grade fever, facial pressure, and sneezing.[9]
Symptoms of rhinovirus in children usually begin 1–3 days after exposure. The illness usually lasts 7–10 more days.[6]
Color or consistency changes in mucous discharge to yellow, thick, or green are the natural course of viral URTI and not an indication for antibiotics.[6]
Group A beta-hemolytic streptococcal pharyngitis/tonsillitis (strep throat) typically presents with a sudden onset of sore throat, pain with swallowing, and fever. Strep throat does not usually cause a runny nose, voice changes, or cough.[citation needed]
Pain and pressure of the ear caused by a middle-ear infection (otitis media) and the reddening of the eye caused by viral conjunctivitis[10] are often associated with URTIs.
Cause
In terms of pathophysiology, rhinovirus infection resembles the immune response. The viruses do not cause damage to the cells of the upper respiratory tract, but rather cause changes in the tight junctions of epithelial cells. This allows the virus to gain access to tissues under the epithelial cells and initiate the innate and adaptive immune responses.[5]: 27
Up to 15% of acute pharyngitis cases may be caused by bacteria, most commonly Streptococcus pyogenes, a group A streptococcus in streptococcal pharyngitis ("strep throat").[11] Other bacterial causes are Streptococcus pneumoniae, Haemophilus influenzae, Corynebacterium diphtheriae, Bordetella pertussis, and Bacillus anthracis[citation needed].
Sexually transmitted infections have emerged as causes of oral and pharyngeal infections.[12]
Diagnosis
| Symptoms | Allergy | URI (Common Cold) | Influenza (Flu) |
|---|---|---|---|
| Itchy, watery eyes | Common | Rare (conjunctivitis may occur with adenovirus) | Soreness behind eyes, sometimes conjunctivitis |
| Nasal discharge | Common | Common[6] | Common |
| Nasal congestion | Common | Common | Sometimes |
| Sneezing | Very common | Very common[6] | Sometimes |
| Sore throat | Sometimes (post-nasal drip) | Very common[6] | Sometimes |
| Cough | Sometimes | Common (mild to moderate, hacking)[6] | Common (dry cough, can be severe) |
| Headache | Uncommon | Rare | Common |
| Fever | Never | Rare in adults, possible in children[6] | Very common 37.8–38.9 °C (100–102 °F)(or higher in young children), lasting 3–4 days; may have chills |
| Malaise | Sometimes | Sometimes | Very common |
| Fatigue, weakness | Sometimes | Sometimes | Very common (can last for weeks, extreme exhaustion early in course) |
| Muscle pain | Never | Slight[6] | Very common (often severe) |
Classification
A URTI may be classified by the area inflamed. Rhinitis affects the nasal mucosa, while rhinosinusitis or sinusitis affects the nose and paranasal sinuses, including frontal, ethmoid, maxillary, and sphenoid sinuses. Nasopharyngitis (rhinopharyngitis or the common cold) affects the nares, pharynx, hypopharynx, uvula, and tonsils generally. Without involving the nose, pharyngitis inflames the pharynx, hypopharynx, uvula, and tonsils. Similarly, epiglottitis (supraglottitis) inflames the superior portion of the larynx and supraglottic area; laryngitis is in the larynx; laryngotracheitis is in the larynx, trachea, and subglottic area; and tracheitis is in the trachea and subglottic area.[citation needed]
Prevention
Vaccination against influenza viruses, adenoviruses, measles, rubella, Streptococcus pneumoniae, Haemophilus influenzae, diphtheria, Bacillus anthracis, and Bordetella pertussis may prevent them from infecting the URT or reduce the severity of the infection.[citation needed]
Treatment

Treatment comprises symptomatic support usually via analgesics for headache, sore throat, and muscle aches.[13] Moderate exercise in sedentary subjects with a naturally acquired URTI probably does not alter the overall severity and duration of the illness.[14] No randomized trials have been conducted to ascertain benefits of increasing fluid intake.[15]
Antibiotics
Prescribing antibiotics for laryngitis is not a suggested practice.[16] The antibiotics penicillin V and erythromycin are not effective for treating acute laryngitis.[16] Erythromycin may improve voice disturbances after a week and cough after 2 weeks, but any modest subjective benefit is not greater than the adverse effects, cost, and the risk of bacteria developing resistance to the antibiotics.[16] Health authorities have been strongly encouraging physicians to decrease the prescribing of antibiotics to treat common URTIs because antibiotic usage does not significantly reduce recovery time for these viral illnesses.[16] A 2017 systematic review found three interventions which were probably effective in reducing antibiotic use for acute respiratory infections: C-reactive protein testing, procalcitonin-guided management, and shared decision-making between physicians and patients.[17] The use of narrow-spectrum antibiotics has been shown to be just as effective as broad-spectrum alternatives for children with acute bacterial URTIs, and has a lower risk of side effects in children.[18] Decreased antibiotic usage may also help prevent drug-resistant bacteria. Some have advocated a delayed antibiotic approach to treating URTIs, which seeks to reduce the consumption of antibiotics while attempting to maintain patient satisfaction. A Cochrane review of 11 studies and 3,555 participants explored antibiotics for respiratory tract infections. It compared delaying antibiotic treatment to either starting them immediately or to no antibiotics. Outcomes were mixed depending on the respiratory tract infection; symptoms of acute otitis media and sore throat were modestly improved with immediate antibiotics with minimal difference in complication rate. Antibiotic usage was reduced when antibiotics were only used for ongoing symptoms and maintained patient satisfaction at 86%.[19] In a trial involving 432 children with a URTI, amoxicillin was no more effective than placebo, even for children with more severe symptoms such as fever or shortness of breath.[20][21]
For sinusitis while at the same time discouraging overuse of antibiotics the CDC recommends:
- Target likely organisms with first-line medications: amoxicillin, amoxicillin/clavulanate
- Use the shortest effective course; should see improvement in 2–3 days. Continue treatment for 7 days after symptoms improve or resolve (usually a 10–14 day course).
- Consider imaging studies in recurrent or unclear cases; some sinus involvement is frequent early in the course of uncomplicated viral URI[6]
Cough medicine
No good evidence exists for or against the effectiveness of over-the-counter cough medications for reducing coughing in adults or children.[22] Children under 2 years old should not be given any type of cough or cold medicine due to the potential for life-threatening side effects.[23] In addition, according to the American Academy of Pediatrics, the use of cough medicine to relieve cough symptoms should be avoided in children under 4 years old, and the safety is questioned for children under 6 years old.[24]
Decongestants
According to a Cochrane review, a single oral dose of nasal decongestant in the common cold is modestly effective for the short-term relief of congestion in adults; however, data on the use of decongestants in children are insufficient. Therefore, decongestants are not recommended for use in children under 12 years of age with the common cold.[19] Oral decongestants are also contraindicated in patients with hypertension, coronary artery disease, and history of bleeding strokes.[26][27]
Mucolytics
Mucolytics such as acetylcysteine and carbocystine are widely prescribed for upper and lower respiratory tract infection without chronic broncho-pulmonary disease. However, in 2013 a Cochrane review reported their efficacy to be limited.[28] Acetylcystine is considered to be safe for the children older than 2 years.[28]
Alternative medicine
Routine supplementation with vitamin C is not justified, as it does not appear to be effective in reducing the incidence of common colds in the general population.[29] The use of vitamin C in the inhibition and treatment of upper respiratory infections has been suggested since the initial isolation of vitamin C in the 1930s. Some evidence exists to indicate that it could be justified in persons exposed to brief periods of severe physical exercise and/or cold environments.[29] Given that vitamin C supplements are inexpensive and safe, people with common colds may consider trying vitamin C supplements to assess whether they are therapeutically beneficial in their case.[29]
Some low-quality evidence indicates the use of nasal irrigation with saline solution may alleviate symptoms in some people.[30] Also, saline nasal sprays can be of benefit.[citation needed]
Epidemiology
Children typically have two to nine viral respiratory illnesses per year.[6] In 2013, 18.8 billion cases of URTIs were reported.[31] As of 2014, they caused about 3,000 deaths, down from 4,000 in 1990.[8] In the United States, URTIs are the most common infectious illness in the general population, and are the leading reasons for people missing work and school.[citation needed]
Dietary research
Weak evidence suggests that probiotics may be better than a placebo treatment or no treatment for preventing upper respiratory tract infections.[32]
See also
References
- ↑ 1.0 1.1 "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1545–1602. October 2016. doi:10.1016/S0140-6736(16)31678-6. PMID 27733282.
- ↑ "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet 388 (10053): 1459–1544. October 2016. doi:10.1016/s0140-6736(16)31012-1. PMID 27733281.
- ↑ "Viral Upper Respiratory Tract Infections" (in en). Viral Infections in Children, Volume II. Cham: Springer International Publishing. 2017. pp. 1–25. doi:10.1007/978-3-319-54093-1_1. ISBN 978-3-319-54093-1.
- ↑ (in en) Infectious Diseases of the Respiratory Tract. Cambridge University Press. 1998-02-12. p. 453. ISBN 978-0-521-40554-6. https://books.google.com/books?id=-X0W5ryclIgC.
- ↑ 5.0 5.1 Pulmonary infection. Cham: Springer. 2015. ISBN 978-3-319-17458-7.
- ↑ 6.00 6.01 6.02 6.03 6.04 6.05 6.06 6.07 6.08 6.09 6.10 6.11 "Rhinitis Versus Sinusitis in Children". Centers for Disease Control and Prevention. https://www.cdc.gov/getsmart/community/materials-references/print-materials/hcp/child-rhin-vs-sinus.pdf.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain.
- ↑ * Control of communicable diseases manual: an official report of the American Public Health Association.. APHA Press, the American Public Health Association. 2015. ISBN 978-0-87553-018-5.
- ↑ 8.0 8.1 "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet 380 (9859): 2095–128. December 2012. doi:10.1016/S0140-6736(12)61728-0. PMID 23245604. PMC 10790329. https://zenodo.org/record/2557786.
- ↑ "Chapter 93: Infections of the Respiratory System". Medical Microbiology (4th ed.). University of Texas Medical Branch at Galveston. 1996. ISBN 978-0-9631172-1-2. https://www.ncbi.nlm.nih.gov/books/NBK8142/. Retrieved 10 July 2021.
- ↑ "Conjunctivitis". 23 July 2020. https://www.lecturio.com/concepts/conjunctivitis/.
- ↑ "Acute pharyngitis". The New England Journal of Medicine 344 (3): 205–11. January 2001. doi:10.1056/nejm200101183440308. PMID 11172144.
- ↑ "Human papillomavirus (HPV) and Oropharyngeal Cancer, Sexually Transmitted Diseases". Centers for Disease Control and Prevention. 2016-11-04. https://www.cdc.gov/std/hpv/STDFact-HPVandOropharyngealCancer.htm.
- ↑ "Common Cold: Treatments and Drugs". Mayo Clinic. http://www.mayoclinic.com/health/common-cold/DS00056/DSECTION=treatments-and-drugs.
- ↑ "Effect of exercise on upper respiratory tract infection in sedentary subjects". British Journal of Sports Medicine 37 (4): 304–6. August 2003. doi:10.1136/bjsm.37.4.304. PMID 12893713.
- ↑ ""Drink plenty of fluids": a systematic review of evidence for this recommendation in acute respiratory infections". The BMJ 328 (7438): 499–500. February 2004. doi:10.1136/bmj.38028.627593.BE. PMID 14988184.
- ↑ 16.0 16.1 16.2 16.3 "Antibiotics for acute laryngitis in adults". The Cochrane Database of Systematic Reviews 2015 (5): CD004783. May 2015. doi:10.1002/14651858.CD004783.pub5. PMID 26002823.
- ↑ "Clinician-targeted interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care: an overview of systematic reviews". The Cochrane Database of Systematic Reviews 2019 (9): CD012252. September 2017. doi:10.1002/14651858.CD012252.pub2. PMID 28881002.
- ↑ "Association of Broad- vs Narrow-Spectrum Antibiotics With Treatment Failure, Adverse Events, and Quality of Life in Children With Acute Respiratory Tract Infections". JAMA 318 (23): 2325–2336. December 2017. doi:10.1001/jama.2017.18715. PMID 29260224.
- ↑ 19.0 19.1 "Immediate versus delayed versus no antibiotics for respiratory infections". The Cochrane Database of Systematic Reviews 2023 (10): CD004417. October 2023. doi:10.1002/14651858.CD004417.pub6. PMID 37791590.
- ↑ "Antibiotics for lower respiratory tract infection in children presenting in primary care: ARTIC-PC RCT". Health Technology Assessment 27 (9): 1–90. June 2023. doi:10.3310/DGBV3199. PMID 37436003.
- ↑ "Antibiotics make little difference to children's chest infections". NIHR Evidence. UK: National Institute for Health and Care Research (NIHR). 27 November 2023. https://evidence.nihr.ac.uk/alert/antibiotics-make-little-difference-to-childrens-chest-infections/.
- ↑ "Over-the-counter (OTC) medications for acute cough in children and adults in community settings". The Cochrane Database of Systematic Reviews 2014 (11): CD001831. November 2014. doi:10.1002/14651858.CD001831.pub5. PMID 25420096.
- ↑ Center for Drug Evaluation and Research. "Special Features – Use Caution When Giving Cough and Cold Products to Kids" (in en). Food and Drug Administration. https://www.fda.gov/Drugs/ResourcesForYou/SpecialFeatures/ucm263948.htm.
- ↑ "Cough in the pediatric population". The Journal of Pediatrics 156 (3): 352–8. March 2010. doi:10.1016/j.jpeds.2009.12.004. PMID 20176183.
- ↑ "Mortality and Burden of Disease Estimates for WHO Member States in 2002" (xls). World Health Organization. 2002. https://www.who.int/entity/healthinfo/statistics/bodgbddeathdalyestimates.xls.
- ↑ "Disorders related to cold and allergy". Handbook of Nonprescription Drugs (14th ed.). Washington, DC: American Pharmacists Association. 2004. pp. 239–269. ISBN 978-1-58212-050-8. OCLC 56446842.
- ↑ "Common cold". Nonprescription Drug Therapy: Guiding Patient Self-care (1st ed.). St Louis, MO: Facts & Comparisons. 2002. pp. 743–769. ISBN 978-1-57439-146-6. OCLC 52895543.
- ↑ 28.0 28.1 "Acetylcysteine and carbocysteine for acute upper and lower respiratory tract infections in paediatric patients without chronic broncho-pulmonary disease". The Cochrane Database of Systematic Reviews (5): CD003124. May 2013. doi:10.1002/14651858.CD003124.pub4. PMID 23728642.
- ↑ 29.0 29.1 29.2 "Vitamin C for preventing and treating the common cold". The Cochrane Database of Systematic Reviews 2013 (1): CD000980. January 2013. doi:10.1002/14651858.CD000980.pub4. PMID 23440782.
- ↑ "Saline nasal irrigation for acute upper respiratory tract infections". The Cochrane Database of Systematic Reviews 2015 (4): CD006821. April 2015. doi:10.1002/14651858.CD006821.pub3. PMID 25892369. PMC 9475221. http://espace.library.uq.edu.au/view/UQ:201653/UQ201653_OA.pdf.
- ↑ ((Global Burden of Disease Study 2013 Collaborators)) (August 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet 386 (9995): 743–800. doi:10.1016/s0140-6736(15)60692-4. PMID 26063472.
- ↑ "Probiotics for preventing acute upper respiratory tract infections". The Cochrane Database of Systematic Reviews 2022 (8): CD006895. August 2022. doi:10.1002/14651858.CD006895.pub4. PMID 36001877.
External links
| Classification |
|---|
- Upper Respiratory Tract Infection from Cleveland Clinic Online Medical Reference
 |
 KSF
KSF