Radiography
Topic: Physics
 From HandWiki - Reading time: 17 min
From HandWiki - Reading time: 17 min
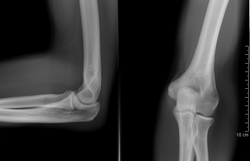
 Projectional radiography of the knee in a modern X-ray machine | |
| System | Musculoskeletal |
|---|---|
| Subdivisions | Interventional, Nuclear, Therapeutic, Paediatric |
| Significant diseases | Cancer, bone fractures |
| Significant tests | screening tests, X-ray, CT, MRI, PET, bone scan, ultrasonography, mammography, fluoroscopy |
| Specialist | Radiographer |
Radiography is an imaging technique using X-rays, gamma rays, or similar ionizing radiation and non-ionizing radiation to view the internal form of an object. Applications of radiography include medical ("diagnostic" radiography and "therapeutic") and industrial radiography. Similar techniques are used in airport security, (where "body scanners" generally use backscatter X-ray). To create an image in conventional radiography, a beam of X-rays is produced by an X-ray generator and it is projected towards the object. A certain amount of the X-rays or other radiation are absorbed by the object, dependent on the object's density and structural composition. The X-rays that pass through the object are captured behind the object by a detector (either photographic film or a digital detector). The generation of flat two-dimensional images by this technique is called projectional radiography. In computed tomography (CT scanning), an X-ray source and its associated detectors rotate around the subject, which itself moves through the conical X-ray beam produced. Any given point within the subject is crossed from many directions by many different beams at different times. Information regarding the attenuation of these beams is collated and subjected to computation to generate two-dimensional images on three planes (axial, coronal, and sagittal) which can be further processed to produce a three-dimensional image.

Medical uses
| Radiography | |
|---|---|
| Medical diagnostics | |
| ICD-9-CM | 87, 88.0-88.6 |
| MeSH | D011859 |
| OPS-301 code | 3–10...3–13, 3–20...3–26 |
Since the body is made up of various substances with differing densities, ionising and non-ionising radiation can be used to reveal the internal structure of the body on an image receptor by highlighting these differences using attenuation, or in the case of ionising radiation, the absorption of X-ray photons by the denser substances (like calcium-rich bones). The discipline involving the study of anatomy through the use of radiographic images is known as radiographic anatomy. Medical radiography acquisition is generally carried out by radiographers, while image analysis is generally done by radiologists. Some radiographers also specialise in image interpretation. Medical radiography includes a range of modalities producing many different types of image, each of which has a different clinical application.
Projectional radiography

The creation of images by exposing an object to X-rays or other high-energy forms of electromagnetic radiation and capturing the resulting remnant beam (or "shadow") as a latent image is known as "projection radiography". The "shadow" may be converted to light using a fluorescent screen, which is then captured on photographic film, it may be captured by a phosphor screen to be "read" later by a laser (CR), or it may directly activate a matrix of solid-state detectors (DR—similar to a very large version of a CCD in a digital camera). Bone and some organs (such as lungs) especially lend themselves to projection radiography. It is a relatively low-cost investigation with a high diagnostic yield. The difference between soft and hard body parts stems mostly from the fact that carbon has a very low X-ray cross section compared to calcium.
Computed tomography

Computed tomography or CT scan (previously known as CAT scan, the "A" standing for "axial") uses ionizing radiation (x-ray radiation) in conjunction with a computer to create images of both soft and hard tissues. These images look as though the patient was sliced like bread (thus, "tomography" – "tomo" means "slice"). Though CT uses a higher amount of ionizing x-radiation than diagnostic x-rays (both utilising X-ray radiation), with advances in technology, levels of CT radiation dose and scan times have reduced.[1] CT exams are generally short, most lasting only as long as a breath-hold, Contrast agents are also often used, depending on the tissues needing to be seen. Radiographers perform these examinations, sometimes in conjunction with a radiologist (for instance, when a radiologist performs a CT-guided biopsy).
Dual energy X-ray absorptiometry
DEXA, or bone densitometry, is used primarily for osteoporosis tests. It is not projection radiography, as the X-rays are emitted in two narrow beams that are scanned across the patient, 90 degrees from each other. Usually the hip (head of the femur), lower back (lumbar spine), or heel (calcaneum) are imaged, and the bone density (amount of calcium) is determined and given a number (a T-score). It is not used for bone imaging, as the image quality is not good enough to make an accurate diagnostic image for fractures, inflammation, etc. It can also be used to measure total body fat, though this is not common. The radiation dose received from DEXA scans is very low, much lower than projection radiography examinations.[citation needed]
Fluoroscopy
Fluoroscopy is a term invented by Thomas Edison during his early X-ray studies. The name refers to the fluorescence he saw while looking at a glowing plate bombarded with X-rays.[2]
The technique provides moving projection radiographs. Fluoroscopy is mainly performed to view movement (of tissue or a contrast agent), or to guide a medical intervention, such as angioplasty, pacemaker insertion, or joint repair/replacement. The last can often be carried out in the operating theatre, using a portable fluoroscopy machine called a C-arm.[3] It can move around the surgery table and make digital images for the surgeon. Biplanar Fluoroscopy works the same as single plane fluoroscopy except displaying two planes at the same time. The ability to work in two planes is important for orthopedic and spinal surgery and can reduce operating times by eliminating re-positioning.[4]
Angiography

Angiography is the use of fluoroscopy to view the cardiovascular system. An iodine-based contrast is injected into the bloodstream and watched as it travels around. Since liquid blood and the vessels are not very dense, a contrast with high density (like the large iodine atoms) is used to view the vessels under X-ray. Angiography is used to find aneurysms, leaks, blockages (thromboses), new vessel growth, and placement of catheters and stents. Balloon angioplasty is often done with angiography.
Contrast radiography
Contrast radiography uses a radiocontrast agent, a type of contrast medium, to make the structures of interest stand out visually from their background. Contrast agents are required in conventional angiography, and can be used in both projectional radiography and computed tomography (called contrast CT).[5][6]
Other medical imaging
Although not technically radiographic techniques due to not using X-rays, imaging modalities such as PET and MRI are sometimes grouped in radiography because the radiology department of hospitals handle all forms of imaging. Treatment using radiation is known as radiotherapy.
Industrial radiography
Industrial radiography is a method of non-destructive testing where many types of manufactured components can be examined to verify the internal structure and integrity of the specimen. Industrial Radiography can be performed utilizing either X-rays or gamma rays. Both are forms of electromagnetic radiation. The difference between various forms of electromagnetic energy is related to the wavelength. X and gamma rays have the shortest wavelength and this property leads to the ability to penetrate, travel through, and exit various materials such as carbon steel and other metals. Specific methods include industrial computed tomography.

Image quality
Image quality will depend on resolution and density. Resolution is the ability an image to show closely spaced structure in the object as separate entities in the image while density is the blackening power of the image. Sharpness of a radiographic image is strongly determined by the size of the X-ray source. This is determined by the area of the electron beam hitting the anode. A large photon source results in more blurring in the final image and is worsened by an increase in image formation distance. This blurring can be measured as a contribution to the modulation transfer function of the imaging system. The memory devices used in large-scale radiographic systems are also very important. They work efficiently to store the crucial data of contrast and density in the radiography image and produce the output accordingly. Smaller capacity memory drives with high-density connectors are also important to deal with internal vibration or shock.
Radiation dose
The dosage of radiation applied in radiography varies by procedure. For example, the effective dosage of a chest x-ray is 0.1 mSv, while an abdominal CT is 10 mSv.[7] The American Association of Physicists in Medicine (AAPM) have stated that the "risks of medical imaging at patient doses below 50 mSv for single procedures or 100 mSv for multiple procedures over short time periods are too low to be detectable and may be nonexistent." Other scientific bodies sharing this conclusion include the International Organization of Medical Physicists, the UN Scientific Committee on the Effects of Atomic Radiation, and the International Commission on Radiological Protection. Nonetheless, radiological organizations, including the Radiological Society of North America (RSNA) and the American College of Radiology (ACR), as well as multiple government agencies, indicate safety standards to ensure that radiation dosage is as low as possible.[8]
Shielding
| X-rays generated by peak voltages below |
Minimum thickness of lead |
|---|---|
| 75 kV | 1.0 mm |
| 100 kV | 1.5 mm |
| 125 kV | 2.0 mm |
| 150 kV | 2.5 mm |
| 175 kV | 3.0 mm |
| 200 kV | 4.0 mm |
| 225 kV | 5.0 mm |
| 300 kV | 9.0 mm |
| 400 kV | 15.0 mm |
| 500 kV | 22.0 mm |
| 600 kV | 34.0 mm |
| 900 kV | 51.0 mm |
Lead is the most common shield against X-rays because of its high density (11,340 kg/m3), stopping power, ease of installation and low cost. The maximum range of a high-energy photon such as an X-ray in matter is infinite; at every point in the matter traversed by the photon, there is a probability of interaction. Thus there is a very small probability of no interaction over very large distances. The shielding of photon beam is therefore exponential (with an attenuation length being close to the radiation length of the material); doubling the thickness of shielding will square the shielding effect.
Table in this section shows the recommended thickness of lead shielding in function of X-ray energy, from the Recommendations by the Second International Congress of Radiology.[9]
Campaigns
In response to increased concern by the public over radiation doses and the ongoing progress of best practices, The Alliance for Radiation Safety in Pediatric Imaging was formed within the Society for Pediatric Radiology. In concert with the American Society of Radiologic Technologists, the American College of Radiology, and the American Association of Physicists in Medicine, the Society for Pediatric Radiology developed and launched the Image Gently campaign which is designed to maintain high quality imaging studies while using the lowest doses and best radiation safety practices available on pediatric patients.[10] This initiative has been endorsed and applied by a growing list of various professional medical organizations around the world and has received support and assistance from companies that manufacture equipment used in radiology.
Following upon the success of the Image Gently campaign, the American College of Radiology, the Radiological Society of North America, the American Association of Physicists in Medicine, and the American Society of Radiologic Technologists have launched a similar campaign to address this issue in the adult population called Image Wisely.[11] The World Health Organization and International Atomic Energy Agency (IAEA) of the United Nations have also been working in this area and have ongoing projects designed to broaden best practices and lower patient radiation dose.[12][13][14]
Provider payment
Contrary to advice that emphasises only conducting radiographs when in the patient's interest, recent evidence suggests that they are used more frequently when dentists are paid under fee-for-service.[15]
Equipment


Sources
In medicine and dentistry, projectional radiography and computed tomography images generally use X-rays created by X-ray generators, which generate X-rays from X-ray tubes. The resultant images from the radiograph (X-ray generator/machine) or CT scanner are correctly referred to as "radiograms"/"roentgenograms" and "tomograms" respectively.
A number of other sources of X-ray photons are possible, and may be used in industrial radiography or research; these include betatrons, linear accelerators (linacs), and synchrotrons. For gamma rays, radioactive sources such as 192Ir, 60Co, or 137Cs are used.
Grid
An anti-scatter grid may be placed between the patient and the detector to reduce the quantity of scattered x-rays that reach the detector. This improves the contrast resolution of the image, but also increases radiation exposure for the patient.[16]
Detectors
Detectors can be divided into two major categories: imaging detectors (such as photographic plates and X-ray film (photographic film), now mostly replaced by various digitizing devices like image plates or flat panel detectors) and dose measurement devices (such as ionization chambers, Geiger counters, and dosimeters used to measure the local radiation exposure, dose, and/or dose rate, for example, for verifying that radiation protection equipment and procedures are effective on an ongoing basis).[17][18][19]
Side markers
A radiopaque anatomical side marker is added to each image. For example, if the patient has their right hand x-rayed, the radiographer includes a radiopaque "R" marker within the field of the x-ray beam as an indicator of which hand has been imaged. If a physical marker is not included, the radiographer may add the correct side marker later as part of digital post-processing.[20]
Image intensifiers and array detectors
As an alternative to X-ray detectors, image intensifiers are analog devices that readily convert the acquired X-ray image into one visible on a video screen. This device is made of a vacuum tube with a wide input surface coated on the inside with caesium iodide (CsI). When hit by X-rays material phosphors which causes the photocathode adjacent to it to emit electrons. These electrons are then focused using electron lenses inside the intensifier to an output screen coated with phosphorescent materials. The image from the output can then be recorded via a camera and displayed.[21]
Digital devices known as array detectors are becoming more common in fluoroscopy. These devices are made of discrete pixelated detectors known as thin-film transistors (TFT) which can either work indirectly by using photo detectors that detect light emitted from a scintillator material such as CsI, or directly by capturing the electrons produced when the X-rays hit the detector. Direct detectors do not tend to experience the blurring or spreading effect caused by phosphorescent scintillators or by film screens since the detectors are activated directly by X-ray photons.[22]
Dual-energy
Dual-energy radiography is where images are acquired using two separate tube voltages. This is the standard method for bone densitometry. It is also used in CT pulmonary angiography to decrease the required dose of iodinated contrast.[23]
History

Radiography's origins and fluoroscopy's origins can both be traced to 8 November 1895, when German physics professor Wilhelm Conrad Röntgen discovered the X-ray and noted that, while it could pass through human tissue, it could not pass through bone or metal.[24] Röntgen referred to the radiation as "X", to indicate that it was an unknown type of radiation. He received the first Nobel Prize in Physics for his discovery.[25]
There are conflicting accounts of his discovery because Röntgen had his lab notes burned after his death, but this is a likely reconstruction by his biographers:[26][27] Röntgen was investigating cathode rays using a fluorescent screen painted with barium platinocyanide and a Crookes tube which he had wrapped in black cardboard to shield its fluorescent glow. He noticed a faint green glow from the screen, about 1 metre away. Röntgen realized some invisible rays coming from the tube were passing through the cardboard to make the screen glow: they were passing through an opaque object to affect the film behind it.[28]

Röntgen discovered X-rays' medical use when he made a picture of his wife's hand on a photographic plate formed due to X-rays. The photograph of his wife's hand was the first ever photograph of a human body part using X-rays. When she saw the picture, she said, "I have seen my death."[28]
The first use of X-rays under clinical conditions was by John Hall-Edwards in Birmingham, England, on 11 January 1896, when he radiographed a needle stuck in the hand of an associate. On 14 February 1896, Hall-Edwards also became the first to use X-rays in a surgical operation.[29]
The United States saw its first medical X-ray obtained using a discharge tube of Ivan Pulyui's design. In January 1896, on reading of Röntgen's discovery, Frank Austin of Dartmouth College tested all of the discharge tubes in the physics laboratory and found that only the Pulyui tube produced X-rays. This was a result of Pulyui's inclusion of an oblique "target" of mica, used for holding samples of fluorescent material, within the tube. On 3 February 1896 Gilman Frost, professor of medicine at the college, and his brother Edwin Frost, professor of physics, exposed the wrist of Eddie McCarthy, whom Gilman had treated some weeks earlier for a fracture, to the X-rays and collected the resulting image of the broken bone on gelatin photographic plates obtained from Howard Langill, a local photographer also interested in Röntgen's work.[30]

X-rays were put to diagnostic use very early; for example, Alan Archibald Campbell-Swinton opened a radiographic laboratory in the United Kingdom in 1896, before the dangers of ionizing radiation were discovered. Indeed, Marie Curie pushed for radiography to be used to treat wounded soldiers in World War I. Initially, many kinds of staff conducted radiography in hospitals, including physicists, photographers, physicians, nurses, and engineers. The medical speciality of radiology grew up over many years around the new technology. When new diagnostic tests were developed, it was natural for the radiographers to be trained in and to adopt this new technology. Radiographers now perform fluoroscopy, computed tomography, mammography, ultrasound, nuclear medicine and magnetic resonance imaging as well. Although a nonspecialist dictionary might define radiography quite narrowly as "taking X-ray images", this has long been only part of the work of "X-ray departments", radiographers, and radiologists. Initially, radiographs were known as roentgenograms,[31] while skiagrapher (from the Ancient Greek words for "shadow" and "writer") was used until about 1918 to mean radiographer. The Japanese term for the radiograph, rentogen (レントゲン), shares its etymology with the original English term.
See also
- Autoradiograph
- Background radiation
- Computer-aided diagnosis
- GXMO
- Imaging science
- List of civilian radiation accidents
- Medical imaging in pregnancy
- Radiation
- Digital radiography
- Radiation contamination
- Radiographer
- Thermography
References
- ↑ "Radiation Doses of Various CT Protocols: a Multicenter Longitudinal Observation Study". Journal of Korean Medical Science 31 (Suppl 1): S24-31. February 2016. doi:10.3346/jkms.2016.31.S1.S24. PMID 26908984.
- ↑ Carroll, Quinn B (2014) (in en). Radiography in the Digital Age (2nd ed.). Springfield: Charles C Thomas. p. 9. ISBN 9780398080976. https://books.google.com/books?id=foW6CAAAQBAJ&pg=PA9.
- ↑ Seeram, Euclid; Brennan, Patrick C (2016) (in en). Radiation Protection in Diagnostic X-Ray Imaging. Jones & Bartlett. ISBN 9781284117714. https://books.google.com/books?id=4-DOCwAAQBAJ&pg=PT408.
- ↑ "The AAPM/RSNA physics tutorial for residents: general overview of fluoroscopic imaging". Radiographics 20 (4): 1115–26. July 2000. doi:10.1148/radiographics.20.4.g00jl301115. PMID 10903700.
- ↑ Quader, Mohammed A; Sawmiller, Carol J; Sumpio, Bauer E (2000). "Radio Contrast Agents: History and Evolution". Textbook of Angiology. pp. 775–783. doi:10.1007/978-1-4612-1190-7_63. ISBN 978-1-4612-7039-3.
- ↑ Brant, William E; Helms, Clyde A (2007). "Diagnostic Imaging Methods" (in en). Fundamentals of Diagnostic Radiology (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 3. ISBN 9780781761352. https://books.google.com/books?id=Sossht2t5XwC&pg=PA3.
- ↑ "Reducing Radiation from Medical X-rays". https://www.fda.gov/ForConsumers/ConsumerUpdates/ucm095505.htm#HowMuch.
- ↑ Goldberg, Jeanne (September–October 2018). "From the Spectral to the Spectrum". Skeptical Inquirer 42 (5).
- ↑ Alchemy Art Lead Products – Lead Shielding Sheet Lead For Shielding Applications. Retrieved 7 December 2008.
- ↑ "IG new: The Alliance | image gently". Pedrad.org. http://www.pedrad.org/associations/5364/ig/?page=365.
- ↑ "Radiation Safety in Adult Medical Imaging". Image Wisely. http://www.imagewisely.org/.
- ↑ "Optimal levels of radiation for patients – Pan American Health Organization – Organización Panamericana de la Salud". New.paho.org. 24 August 2010. http://new.paho.org/hq10/index.php?option=com_content&task=view&id=3365&Itemid=2164.
- ↑ "Radiation Protection of Patients". Rpop.iaea.org. 14 March 2013. https://rpop.iaea.org/RPOP/RPoP/Content/index.htm.
- ↑ "World Health Organisation: Global Initiative on Radiation Safety in Healthcare Settings: Technical Meeting Report". Who.int. https://www.who.int/ionizing_radiation/about/GI_TM_Report_2008_Dec.pdf.
- ↑ "First do no harm - The impact of financial incentives on dental X-rays". Journal of Health Economics 58 (March 2018): 1–9. March 2018. doi:10.1016/j.jhealeco.2017.12.005. PMID 29408150.
- ↑ Bushberg, Jerrold T (2002). The Essential Physics of Medical Imaging (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 210. ISBN 9780683301182. https://books.google.com/books?id=VZvqqaQ5DvoC&pg=PA210.
- ↑ "Radiation detectors in nuclear medicine". Radiographics 19 (2): 481–502. 1999. doi:10.1148/radiographics.19.2.g99mr30481. PMID 10194791.
- ↑ "Characteristics of radiation detectors for diagnostic radiology". Applied Radiation and Isotopes 50 (1): 125–36. January 1999. doi:10.1016/S0969-8043(98)00044-X. PMID 10028632.
- ↑ Anwar, Kamal (2013). "Nuclear Radiation Detectors". Particle Physics. Graduate Texts in Physics. Berlin: Springer-Verlag. pp. 1–78. doi:10.1007/978-3-642-38661-9_1. ISBN 978-3-642-38660-2.
- ↑ "A clinical audit of anatomical side marker use in a paediatric medical imaging department". Journal of Medical Radiation Sciences 63 (3): 148–54. September 2016. doi:10.1002/jmrs.176. PMID 27648278.
- ↑ Hendee, William R.; Ritenour, E. Russell (2002). "Fluoroscopy". Medical Imaging Physics (4th ed.). Hoboken, NJ: John Wiley & Sons. ISBN 9780471461135. https://books.google.com/books?id=55lh1B82SLsC&pg=PA236.
- ↑ "Flat-panel detectors: how much better are they?". Pediatric Radiology 36 Suppl 2 (S2): 173–81. September 2006. doi:10.1007/s00247-006-0208-0. PMID 16862412.
- ↑ Cochrane Miller, Janet (2015). "Dual Energy CT Imaging for Suspected Pulmonary Embolism Using a Lower Dose of Contrast Agent". Radiology Rounds 13 (7). http://www.massgeneral.org/imaging/news/radrounds/july_2015/. Retrieved 5 February 2018.
- ↑ "History of Radiography". NDT Resource Center. Iowa State University. http://www.ndt-ed.org/EducationResources/CommunityCollege/Radiography/Introduction/history.htm.
- ↑ Karlsson, Erik B. (9 February 2000). "The Nobel Prizes in Physics 1901–2000". Stockholm: The Nobel Foundation. https://www.nobelprize.org/nobel_prizes/physics/articles/karlsson/.
- ↑ "5 unbelievable things about X-rays you can't miss". https://www.vix.com/en/ovs/curiosities/8709/5-unbelievable-things-about-x-rays-you-cant-miss.
- ↑ Glasser, Otto (1993). Wilhelm Conrad Röntgen and the early history of the roentgen rays. Norman Publishing. pp. 10–15. ISBN 978-0930405229. https://books.google.com/books?id=5GJs4tyb7wEC&pg=PA10.
- ↑ 28.0 28.1 Markel, Howard (20 December 2012). "'I Have Seen My Death': How the World Discovered the X-Ray". PBS NewsHour. PBS. https://www.pbs.org/newshour/rundown/2012/12/i-have-seen-my-death-how-the-world-discovered-the-x-ray.html.
- ↑ "Major John Hall-Edwards". Birmingham City Council. http://www.birmingham.gov.uk/xray.
- ↑ "The first clinical X-ray made in America – 100 years". American Journal of Roentgenology (American Roentgen Ray Society) 164 (1): 241–3. January 1995. doi:10.2214/ajr.164.1.7998549. PMID 7998549.
- ↑ "The Crests of the Interdental Alveolar Septa". The Journal of Periodontology 24 (2): 75–87. April 1953. doi:10.1902/jop.1953.24.2.75.
Further reading
- Oakley, PA; Harrison, DE (2020). "X-Ray Hesitancy: Patients' Radiophobic Concerns Over Medical X-rays. Dose-Response.". Specific Safety Guide No. SSG-11 (Vienna: International Atomic Energy Agency). doi:10.1177/1559325820959542.
- "Wilhelm Conrad Röntgen and the Glimmer of Light". Physics Today 48 (11): 25–31. November 1995. doi:10.1063/1.881456. Bibcode: 1995PhT....48k..25S.
- "X-Ray equipment". The Biomedical Engineering handbook. CRC Press and IEEE Press. 1995. pp. 953–960. ISBN 978-0-8493-8346-5.
- Fundamentals of Computerized Tomography: Image Reconstruction from Projections (2nd ed.). Springer. 2009. ISBN 978-1-85233-617-2.
- "Metal-Based X-ray Contrast Media". Chemical Reviews 99 (9): 2353–78. September 1999. doi:10.1021/cr980441p. PMID 11749484.
External links
- MedPix Medical Image Database
- Video on X-ray inspection and industrial computed tomography, Karlsruhe University of Applied Sciences
- NIST's XAAMDI: X-Ray Attenuation and Absorption for Materials of Dosimetric Interest Database
- NIST's XCOM: Photon Cross Sections Database
- NIST's FAST: Attenuation and Scattering Tables
- A lost industrial radiography source event
- RadiologyInfo - The radiology information resource for patients: Radiography (X-rays)
 |
 KSF
KSF