Antibody
 From Wikidoc - Reading time: 22 min
From Wikidoc - Reading time: 22 min
|
WikiDoc Resources for Antibody |
|
Articles |
|---|
|
Most recent articles on Antibody |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Antibody at Clinical Trials.gov Clinical Trials on Antibody at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Antibody
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Antibody Risk calculators and risk factors for Antibody
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Antibody |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [2]

Antibodies (also known as immunoglobulins[1]) are proteins that are found in blood or other bodily fluids of vertebrates, and are used by the immune system to identify and neutralize foreign objects, such as bacteria and viruses. They are made of a few basic structural units called chains; each antibody has two large heavy chains H and two small light chains L. Antibodies are produced by a kind of white blood cell called a B cell. There are several different types of antibody heavy chain, and several different kinds of antibodies, which are grouped into different isotypes based on which heavy chain they possess. Five different antibody isotypes are known in mammals, which perform different roles, and help direct the appropriate immune response for each different type of foreign object they encounter.[2]
Although the general structure of all antibodies is very similar, a small region at the tip of the protein is extremely variable, allowing millions of antibodies with slightly different tip structures to exist. This region is known as the hypervariable region. Each of these variants can bind to a different target, known as an antigen.[3] This huge diversity of antibodies allows the immune system to recognize an equally wide diversity of antigens. The unique part of the antigen recognized by an antibody is called an epitope. These epitopes bind with their antibody in a highly specific interaction, called induced fit, that allows antibodies to identify and bind only their unique antigen in the midst of the millions of different molecules that make up an organism. Recognition of an antigen by an antibody tags it for attack by other parts of the immune system. Antibodies can also neutralize targets directly by, for example, binding to a part of a pathogen that it needs to cause an infection.[4]
The large and diverse population of antibodies is generated by random combinations of a set of gene segments that encode different antigen binding sites (or paratopes), followed by random mutations in this area of the antibody gene, which create further diversity.[2][5] Antibody genes also re-organize in a process called class switching that changes the base of the heavy chain to another, creating a different isotype of the antibody that retains the antigen specific variable region. This allows a single antibody to be used by several different parts of the immune system. Production of antibodies is the main function of the humoral immune system.[6]
Antibody forms[edit | edit source]
Antibodies occur in two forms: a soluble form secreted into the blood and tissue fluids, and a membrane-bound form attached to the surface of a B cell that is called the B cell receptor (BCR). The BCR allows a B cell to detect when a specific antigen is present in the body and triggers B cell activation.[7] Activated B cells differentiate into either antibody generating factories called plasma cells that secrete soluble antibody, or into memory cells that survive in the body for years afterwards to allow the immune system to remember an antigen and respond faster upon future exposures.[8] Antibodies are, therefore, an essential component of the adaptive immune system that learns, adapts and remembers responses to invading pathogens.
Isotypes[edit | edit source]
| Name | Types | Description | Antibody Complexes |
| IgA | 2 | Found in mucosal areas, such as the gut, respiratory tract and urogenital tract, and prevents colonization by pathogens.[9] Also found in saliva, tears, and breast milk. | 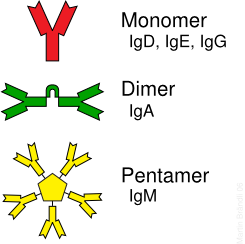
|
| IgD | 1 | Functions mainly as an antigen receptor on B cells that have not been exposed to antigens.[10] Its function is less defined than other isotypes. | |
| IgE | 1 | Binds to allergens and triggers histamine release from mast cells and basophils, and is involved in allergy. Also protects against parasitic worms.[6] | |
| IgG | 4 | In its four forms, provides the majority of antibody-based immunity against invading pathogens.[6] The only antibody capable of crossing the placenta to give passive immunity to fetus. | |
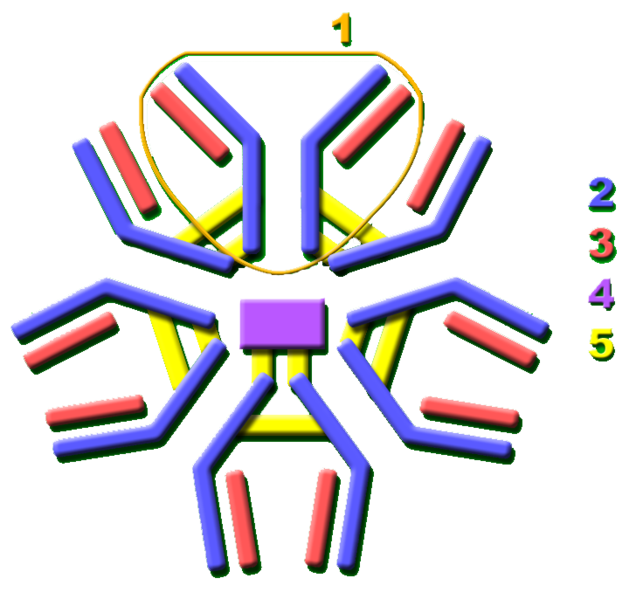
| IgM | 1 | Expressed on the surface of B cells and in a secreted form with very high avidity. Eliminates pathogens in the early stages of B cell mediated (humoral) immunity before there is sufficient IgG.[6][10] |
Antibodies can come in different varieties known as isotypes or classes. In mammals there are five antibody isotypes known as IgA, IgD, IgE,IgG and IgM. They are each named with an "Ig" prefix that stands for immunoglobulin, another name for antibody, and differ in their biological properties, functional locations and ability to deal with different antigens, as depicted in the table.[11]
The antibody isotype of a B cell changes during the cell's development and activation. Immature B cells, which have never been exposed to antigen, are known as naïve B cells and express only the IgM isotype in a cell surface bound form. B cells begin to express both IgM and IgD when they reach maturity - the co-expression of both these immunoglobulin isotypes renders the B cell 'mature' and ready to respond to antigen.[12] B cell activation follows engagement of the cell bound antibody molecule with an antigen, causing the cell to divide and differentiate into an antibody producing cell called a plasma cell. In this activated form, the B cell starts to produce antibody in a secreted form rather than a membrane-bound form. Some daughter cells of the activated B cells undergo isotype switching, a mechanism that causes the production of antibodies to change from IgM or IgD to the other antibody isotypes, IgE, IgA or IgG, that have defined roles in the immune system.
Structure[edit | edit source]
Antibodies are heavy (~150kDa) globular plasma proteins that are also known as immunoglobulins. They have sugar chains added to some of their amino acid residues.[13] In other words, antibodies are glycoproteins. The basic functional unit of each antibody is an immunoglobulin (Ig) monomer (containing only one Ig unit); secreted antibodies can also be dimeric with two Ig units as with IgA, tetrameric with four Ig units like teleost fish IgM, or pentameric with five Ig units, like mammalian IgM.[14]
Immunoglobulin domains[edit | edit source]
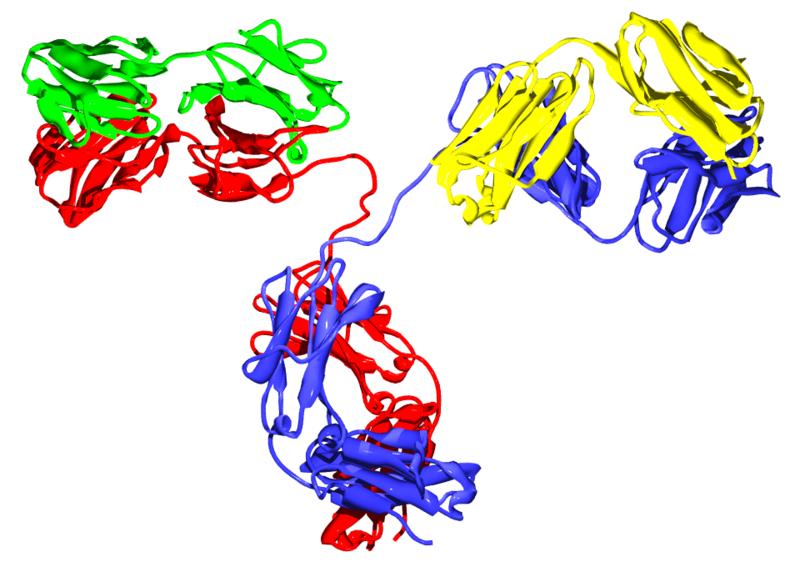
The Ig monomer is a "Y"-shaped molecule that consists of four polypeptide chains; two identical heavy chains and two identical light chains connected by disulfide bonds.[11] Each chain is composed of structural domains called Ig domains. These domains contain about 70-110 amino acids and are classified into different categories (for example, variable or IgV, and constant or IgC) according to their size and function.[15] They possess a characteristic immunoglobulin fold in which two beta sheets create a “sandwich” shape, held together by interactions between conserved cysteines and other charged amino acids.
Heavy chain[edit | edit source]
There are five types of mammalian Ig heavy chain denoted by the Greek letters: α, δ, ε, γ, and μ.[3] The type of heavy chain present defines the class of antibody; these chains are found in IgA, IgD, IgE, IgG, and IgM antibodies, respectively.[4] Distinct heavy chains differ in size and composition; α and γ contain approximately 450 amino acids, while μ and ε have approximately 550 amino acids.[3]
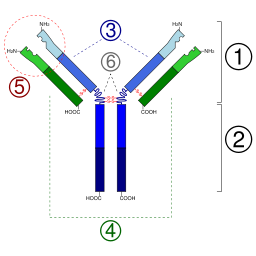
2. Fc region
3. Heavy chain with one variable (VH) domain followed by a constant domain (CH1), a hinge region, and two more constant (CH2 and CH3) domains.
4. Light chain with one variable (VL) and one constant (CL) domain
5. Antigen binding site (paratope)
6. Hinge regions.
Each heavy chain has two regions, the constant region and the variable region. The constant region is identical in all antibodies of the same isotype, but differs in antibodies of different isotypes. Heavy chains γ, α and δ have a constant region composed of three tandem (in a line) Ig domains, and a hinge region for added flexibility;[11] heavy chains μ and ε have a constant region composed of four immunoglobulin domains.[3] The variable region of the heavy chain differs in antibodies produced by different B cells, but is the same for all antibodies produced by a single B cell or B cell clone. The variable region of each heavy chain is approximately 110 amino acids long and is composed of a single Ig domain.
Light chain[edit | edit source]
In mammals there are two types of light chain, which are called lambda (λ) and kappa (κ).[3] A light chain has two successive domains: one constant domain and one variable domain. The approximate length of a light chain is 211 to 217 amino acids.[3] Each antibody contains two light chains that are always identical; only one type of light chain, κ or λ, is present per antibody in mammals. Other types of light chains, such as the iota (ι) chain, are found in lower vertebrates like Chondrichthyes and Teleostei.
Fab and Fc Regions[edit | edit source]
Some parts of an antibody have unique functions. The tip of the Y, for example, contains the site that binds antigen and, therefore, recognizes specific foreign objects. This region of the antibody is called the Fab (fragment, antigen binding) region. It is composed of one constant and one variable domain from each heavy and light chain of the antibody.[16] The paratope is shaped at the amino terminal end of the antibody monomer by the variable domains from the heavy and light chains.
The base of the Y plays a role in modulating immune cell activity. This region is called the Fc (Fragment, crystallizable) region, and is composed of two heavy chains that contribute two or three constant domains depending on the class of the antibody.[3] By binding to specific proteins the Fc region ensures that each antibody generates an appropriate immune response for a given antigen.[17] The Fc region also binds to various cell receptors, such as Fc receptors, and other immune molecules, such as complement proteins. By doing this, it mediates different physiological effects including opsonization, cell lysis, and degranulation of mast cells, basophils and eosinophils.[11][18]
Function[edit | edit source]
Since antibodies exist freely in the bloodstream, they are said to be part of the humoral immune system. Circulating antibodies are produced by clonal B cells that specifically respond to only one antigen, a virus hull protein fragment, for example. Antibodies contribute to immunity in three main ways: they can prevent pathogens from entering or damaging cells by binding to them; they can stimulate removal of a pathogen by macrophages and other cells by coating the pathogen; and they can trigger direct pathogen destruction by stimulating other immune responses such as the complement pathway.[19]
Activation of complement[edit | edit source]
Antibodies that bind to surface antigens on, for example a bacterium, attract the first component of the complement cascade with their Fc region and initiate activation of the "classical" complement system.[19] This results in the killing of bacteria in two ways.[6] First, the binding of the antibody and complement molecules marks the microbe for ingestion by phagocytes in a process called opsonization; these phagocytes are attracted by certain complement molecules generated in the complement cascade. Secondly, some complement system components form a membrane attack complex to assist antibodies to kill the bacterium directly.[20]
Activation of effector cells[edit | edit source]
To combat pathogens that replicate outside cells, antibodies bind to pathogens to link them together, causing them to agglutinate. Since an antibody possesses at least two paratopes it can bind more than one antigen by binding identical epitopes carried on the surfaces of these antigens. By coating the pathogen, antibodies stimulate effector functions against the pathogen in cells that recognize their Fc region.[6]
Those cells which recognize coated pathogens have Fc receptors which, as the name suggests, interacts with the Fc region of IgA, IgG, and IgE antibodies. The engagement of a particular antibody with the Fc receptor on a particular cell triggers an effector function of that cell; phagocytes will phagocytose, mast cells and neutrophils will degranulate, natural killer cells will release cytokines and cytotoxic molecules; that will ultimately result in destruction of the invading microbe. The Fc receptors are isotype-specific, which gives greater flexibility to the immune system, invoking only the appropriate immune mechanisms for distinct pathogens.[3]
Immunoglobulin diversity[edit | edit source]
Virtually all microbes can trigger an antibody response. Successful recognition and eradication of many different types of microbes requires diversity among antibodies; their amino acid composition varies allowing them to interact with many different antigens.[21] It has been estimated that humans generate about 10 billion different antibodies, each capable of binding a distinct epitope of an antigen.[22] Although a huge repertoire of different antibodies is generated in a single individual, the number of genes available to make these proteins is limited. Several complex genetic mechanisms have evolved that allow vertebrate B cells to generate a diverse pool of antibodies from a relatively small number of antibody genes.[23]
V(D)J recombination[edit | edit source]
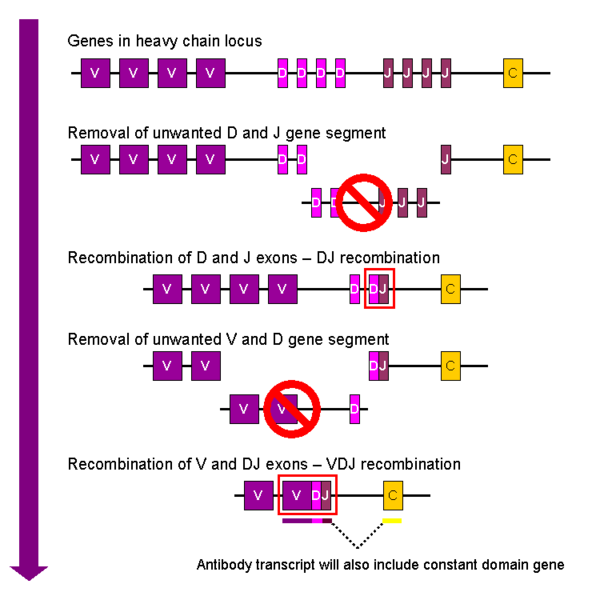
Somatic recombination of immunoglobulins, also known as V(D)J recombination, involves the generation of a unique immunoglobulin variable region. The variable region of each immunoglobulin heavy or light chain is encoded in several pieces - known as gene segments. These segments are called variable (V), diversity (D) and joining (J) segments.[23] V, D and J segments are found in Ig heavy chains, but only V and J segments are found in Ig light chains. Multiple copies of the V, D and J gene segments exist, and are tandemly arranged in the genomes of mammals. In the bone marrow, each developing B cell will assemble an immunoglobulin variable region by randomly selecting and combining one V, one D and one J gene segment (or one V and one J segment in the light chain). As there are multiple copies of each type of gene segment, and different combinations of gene segments can be used to generate each immunoglobulin variable region, this process generates a huge number of antibodies, each with different paratopes, and thus different antigen specificities.[2]
After a B cell produces a functional immunoglobulin gene during V(D)J recombination, it cannot express any other variable region (a process known as allelic exclusion) thus each B cell can produce antibodies containing only one kind of variable chain.[24][3]
Somatic hypermutation and affinity maturation[edit | edit source]
- For more details on this topic, see Somatic hypermutation and Affinity maturation
Another mechanism that generates antibody diversity occurs in the mature B cell. Following activation with antigen, B cells begin to proliferate rapidly. In these rapidly dividing cells, the genes encoding the variable domains of the heavy and light chains undergo a high rate of point mutation, by a process called somatic hypermutation (SHM). SHM results in approximately one nucleotide change per variable gene, per cell division.[5] As a consequence, any daughter B cells will acquire slight amino acid differences in the variable domains of their antibody chains.
Somatic hypermutation serves to increase the diversity of the antibody pool and impacts the antibody’s antigen-binding affinity.[25] Some point mutations will result in the production of antibodies that have a weaker interaction (low affinity) with their antigen than the original antibody, and some mutations will generate antibodies with a stronger interaction (high affinity).[26] B cells that express high affinity antibodies on their surface will receive a strong survival signal during interactions with other cells, whereas those with low affinity antibodies will not, and will die by apoptosis.[26] Thus, B cells expressing higher affinity antibodies for will outcompete those with weaker affinities for function and survival. The process of generating antibodies with increased binding affinities is called affinity maturation. Affinity maturation occurs in mature B cells after V(D)J recombination, and is dependent on help from helper T cells.[27]
Class switching[edit | edit source]
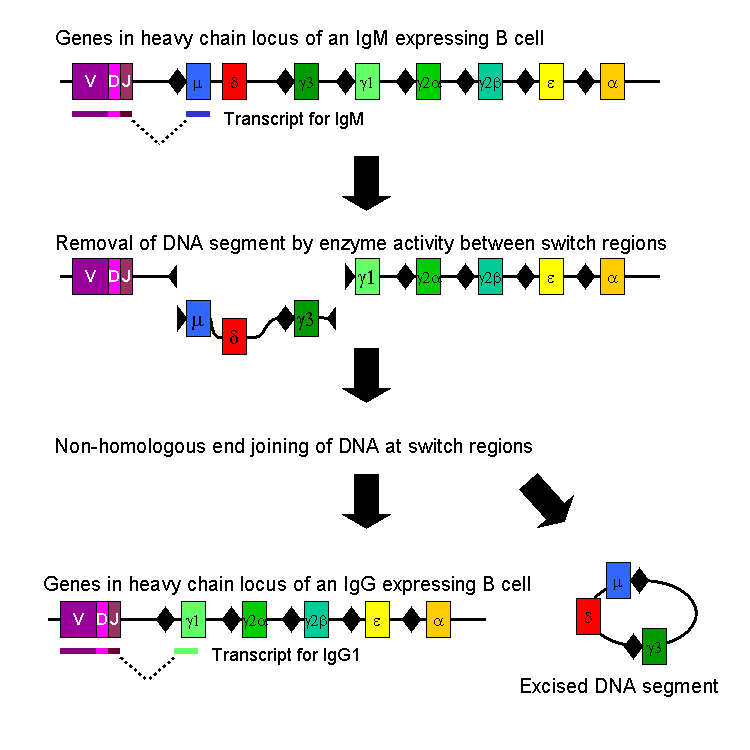
Isotype or class switching is a biological process occurring after activation of the B cell, which allows the cell to produce different classes of antibody (IgA, IgE, or IgG).[2] The different classes of antibody, and thus effector functions, are defined by the constant (C) regions of the immunoglobulin heavy chain. Initially, naïve B cells express only cell-surface IgM and IgD with identical antigen binding regions. Each isotype is adapted for a distinct function, therefore, after activation, an antibody with a IgG, IgA, or IgE effector function might be required to effectively eliminate an antigen. Class switching allows different daughter cells from the same activated B cell to produce antibodies of different isotypes. Only the constant region of the antibody heavy chain changes during class switching; the variable regions, and therefore antigen specificity, remain unchanged. Thus the progeny of a single B cell can produce antibodies, all specific for the same antigen, but with the ability to produce the effector function appropriate for each antigenic challenge. Class switching is triggered by cytokines; the isotype generated depends on which cytokines are present in the B cell environment.[28]
Class switching occurs in the heavy chain gene locus by a mechanism called class switch recombination (CSR). This mechanism relies on conserved nucleotide motifs, called switch (S) regions, found in DNA upstream of each constant region gene (except in the δ-chain). The DNA strand is broken by the activity of a series of enzymes at two selected S-regions.[29][30] The variable domain exon is rejoined through a process called non-homologous end joining (NHEJ) to the desired constant region (γ, α or ε). This process results in an immunoglobulin gene that encodes an antibody of a different isotype.[31]
Medical applications[edit | edit source]
Disease diagnosis[edit | edit source]
Detection of particular antibodies is a very common form of medical diagnostics, and applications such as serology depend on these methods.[32] For example, in biochemical assays for disease diagnosis,[33] a titer of antibodies directed against Epstein-Barr virus or Lyme disease is estimated from the blood. If those antibodies are not present, either the person is not infected, or the infection occurred a very long time ago, and the B cells generating these specific antibodies have naturally decayed. In clinical immunology, levels of individual classes of immunoglobulins are measured by nephelometry (or turbidimetry) to characterize the antibody profile of patient.[34] Elevations in different classes of immunoglobulins are sometimes useful in determining the cause of liver damage in patients whom the diagnosis is unclear.[4] For example, elevated IgA indicates alcoholic cirrhosis, elevated IgM indicates viral hepatitis and primary biliary cirrhosis, while IgG is elevated in viral hepatitis, autoimmune hepatitis and cirrhosis. Autoimmune disorders can often be traced to antibodies that bind the body's own epitopes; many can be detected through blood tests. Antibodies directed against red blood cell surface antigens in immune mediated hemolytic anemia are detected with the Coombs test.[35] The Coombs test is also used for antibody screening in blood transfusion preparation and also for antibody screening in antenatal women.[35] Practically, several immunodiagnostic methods based on detection of complex antigen-antibody are used to diagnose infectious diseases, for example ELISA, immunofluorescence, Western blot, immunodiffusion, and immunoelectrophoresis.
Disease therapy[edit | edit source]
"Targeted" monoclonal antibody therapy is employed to treat diseases such as rheumatoid arthritis,[36] multiple sclerosis,[37] psoriasis,[38] and many forms of cancer including non-Hodgkin's lymphoma,[39] colorectal cancer, head and neck cancer and breast cancer.[40] Some immune deficiencies, such as X-linked agammaglobulinemia and hypogammaglobulinemia, result in partial or complete lack of antibodies.[41] These diseases are often treated by inducing a short term form of immunity called passive immunity. Passive immunity is achieved through the transfer of ready-made antibodies in the form of human or animal serum, pooled immunoglobulin or monoclonal antibodies, into the affected individual.[42]
Prenatal therapy[edit | edit source]
Rho(D) Immune Globulin antibodies are specific for human Rhesus D (RhD) antigen, also known as Rhesus factor.[43] These anti-RhD antibodies are known under several brand names, including RhoGAM, BayRHo-D, Gamulin Rh, HypRho-D, and WinRho SDF. Rhesus factor is an antigen found on red blood cells; individuals that are Rhesus-positive (Rh+) have this antigen on their red blood cells and individuals that are Rhesus-negative (Rh-) do not. During normal childbirth, delivery trauma or complications during pregnancy, blood from a fetus can enter the mother's system. In the case of an Rh-incompatible mother and child, consequential blood mixing may sensitize an Rh- mother to the Rh antigen on the blood cells of the Rh+ child, putting the remainder of the pregnancy, and any subsequent pregnancies, at risk for hemolytic disease of the newborn.[44] Anti-RhD antibodies are administered as part of a prenatal treatment regimen to prevent sensitization that may occur when a Rhesus-negative mother has a Rhesus-positive fetus. Treatment of a mother with Anti-RhD antibodies prior to and immediately after trauma and delivery destroys Rh antigen in the mother's system from the fetus. Importantly, this occurs before the antigen can stimulate maternal B cells to "remember" Rh antigen by generating memory B cells. Therefore, her humoral immune system will not make anti-Rh antibodies, and will not attack the Rhesus antigens of the current or subsequent baby. Rho(D) Immune Globulin treatment prevents sensitization that can lead to Rh disease, but does not prevent or treat the underlying disease itself.[43]
Research applications[edit | edit source]
Specific antibodies are produced by injecting an antigen into a mammal, such as a mouse, rat or rabbit for small quantities of antibody, or goat, sheep, or horse for large quantities of antibody. Blood isolated from these animals contains polyclonal antibodies — multiple antibodies that bind to the same antigen — in the serum, which can now be called antiserum. Antigens are also injected into chickens for generation of polyclonal antibodies in egg yolk.[45] To obtain antibody that is specific for a single epitope of an antigen, antibody-secreting lymphocytes are isolated from the animal and immortalized by fusing them with a cancer cell line. The fused cells are called hybridomas, and will continually grow and secrete antibody in culture. Single hybridoma cells are isolated by dilution cloning to generate cell clones that all produce the same antibody; these antibodies are called monoclonal antibodies.[46] Generated polyclonal and monoclonal antibodies are often purified using Protein A/G or antigen-affinity chromatography.[47]
Use[edit | edit source]
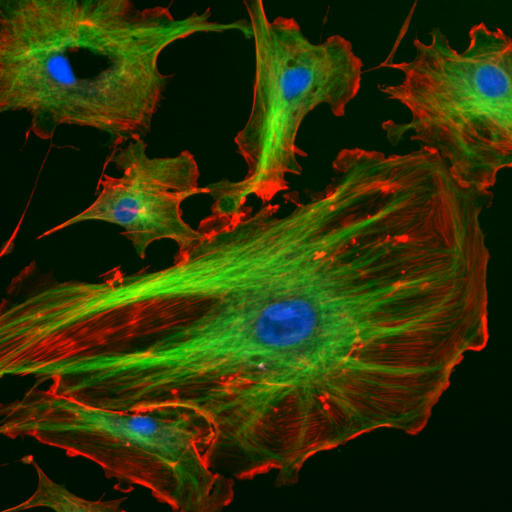
In research, purified antibodies are used in many applications. They are most commonly used to identify and locate intracellular and extracellular proteins. Antibodies are used in flow cytometry to differentiate cell types by the proteins they express; different types of cell express different combinations of cluster of differentiation molecules on their surface, and produce different intracellular and secretable proteins.[48] They are also used in immunoprecipitation to separate proteins and anything bound to them (co-immunoprecipitation) from other molecules in a cell lysate,[49] in Western blot analyses to identify proteins separated by electrophoresis,[50] and in immunohistochemistry or immunofluorescence to examine protein expression in tissue sections or to locate proteins within cells with the assistance of a microscope.[51][48] Proteins can also be detected and quantified with antibodies, using ELISA and ELISPOT techniques.[52][53]
History[edit | edit source]
The study of antibodies began in 1890 when Emil von Behring and Shibasaburo Kitasato described antibody activity against diphtheria and tetanus toxins. Behring and Kitasato put forward the theory of humoral immunity, proposing that a mediator in serum could react with a foreign antigen.[54][55] Their idea prompted Paul Ehrlich to propose the side chain theory for antibody and antigen interaction in 1897, when he hypothesized that receptors (described as “side chains”) on the surface of cells could bind specifically to toxins – in a "lock-and-key" interaction – and that this binding reaction was the trigger for the production of antibodies.[56] Other researchers believed that antibodies existed freely in the blood and, in 1904, Almroth Wright suggested that soluble antibodies coated bacteria to label them for phagocytosis and killing; a process that he named opsoninization.[57]
In the 1920s, Michael Heidelberger and Oswald Avery observed that antigens could be precipitated by antibodies and went on to show that antibodies were made of protein.[58] The biochemical properties of antigen-antibody binding interactions were examined in more detail in the late 1930s by John Marrack.[59] The next major advance was in the 1940s, when Linus Pauling confirmed the lock-and-key theory proposed by Ehrlich by showing that the interactions between antibodies and antigens depended more on their shape than their chemical composition.[60] In 1948, Astrid Fagreaus discovered that B cells, in the form of plasma cells, were responsible for generating antibodies.[61]
Further work concentrated on characterizing the structures of the antibody proteins. A major advance in these structural studies was the discovery in the early 1960s by Gerald Edelman and Joseph Gally of the antibody light chain,[62] and their realization that this protein was the same as the Bence-Jones protein described in 1845 by Henry Bence Jones.[63] Edelman went on to discover that antibodies are composed of disulphide bond-linked heavy and light chains. Around the same time, antibody-binding (Fab) and antibody tail (Fc) regions of IgG were characterized by Rodney Porter.[64] Together, these scientists deduced the structure and complete amino acid sequence of IgG, a feat for which they were jointly awarded the 1972 Nobel prize in Physiology or Medicine.[64] While most of these early studies focused on IgM and IgG, other immunoglobulin isotypes were identified in the 1960s: Thomas Tomasi discovered secretory antibody (IgA) [65] and David Rowe and John Fahey identified IgD,[66] and IgE was identified by Kikishige Ishizaka and Teruki Ishizaka as a class of antibodies involved in allergic reactions.[67]
Genetic studies revealed the basis of the vast diversity of these antibody proteins when somatic recombination of immunoglobulin genes was identified by Susumu Tonegawa in 1976.[68]
See also[edit | edit source]
References[edit | edit source]
- ↑ Litman GW, Rast JP, Shamblott MJ; et al. (1993). "Phylogenetic diversification of immunoglobulin genes and the antibody repertoire". Mol. Biol. Evol. 10 (1): 60–72. PMID 8450761.
- ↑ 2.0 2.1 2.2 2.3 Eleonora Market, F. Nina Papavasiliou (2003) V(D)J Recombination and the Evolution of the Adaptive Immune System PLoS Biology1(1): e16.
- ↑ 3.0 3.1 3.2 3.3 3.4 3.5 3.6 3.7 3.8 Janeway CA, Jr; et al. (2001). Immunobiology (5th ed. ed.). Garland Publishing. ISBN 0-8153-3642-X.
- ↑ 4.0 4.1 4.2 Rhoades RA, Pflanzer RG (2002). Human Physiology (4th ed. ed.). Thomson Learning. ISBN 0-534-42174-1.
- ↑ 5.0 5.1 Diaz M, Casali P (2002). "Somatic immunoglobulin hypermutation". Curr Opin Immunol. 14 (2): 235–40. PMID 11869898.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 Pier GB, Lyczak JB, Wetzler LM (2004). Immunology, Infection, and Immunity. ASM Press. ISBN 1-55581-246-5.
- ↑ Parker D (1993). "T cell-dependent B cell activation". Annu Rev Immunol. 11: 331–60. PMID 8476565.
- ↑ Borghesi L, Milcarek C (2006). "From B cell to plasma cell: regulation of V(D)J recombination and antibody secretion". Immunol Res. 36 (1–3): 27–32. PMID 17337763.
- ↑ Underdown B, Schiff J (1986). "Immunoglobulin A: strategic defense initiative at the mucosal surface". Annu Rev Immunol. 4: 389–417. PMID 3518747.
- ↑ 10.0 10.1 Geisberger R, Lamers M, Achatz G (2006). "The riddle of the dual expression of IgM and IgD". Immunology. 118 (4): 429–37. PMID 16895553.
- ↑ 11.0 11.1 11.2 11.3 Woof J, Burton D (2004). "Human antibody-Fc receptor interactions illuminated by crystal structures". Nat Rev Immunol. 4 (2): 89–99. PMID 15040582.
- ↑ Goding J. "Allotypes of IgM and IgD receptors in the mouse: a probe for lymphocyte differentiation". Contemp Top Immunobiol. 8: 203–43. PMID 357078.
- ↑ Mattu T, Pleass R, Willis A, Kilian M, Wormald M, Lellouch A, Rudd P, Woof J, Dwek R (1998). "The glycosylation and structure of human serum IgA1, Fab, and Fc regions and the role of N-glycosylation on Fc alpha receptor interactions". J Biol Chem. 273 (4): 2260–72. PMID 9442070.
- ↑ Roux K (1999). "Immunoglobulin structure and function as revealed by electron microscopy". Int Arch Allergy Immunol. 120 (2): 85–99. PMID 10545762.
- ↑ Barclay A (2003). "Membrane proteins with immunoglobulin-like domains--a master superfamily of interaction molecules". Semin Immunol. 15 (4): 215–23. PMID 14690046.
- ↑ Putnam FW, Liu YS, Low TL (1979). "Primary structure of a human IgA1 immunoglobulin. IV. Streptococcal IgA1 protease, digestion, Fab and Fc fragments, and the complete amino acid sequence of the alpha 1 heavy chain". J Biol Chem. 254 (8): 2865–74. PMID 107164.
- ↑ Huber R (1980). "Spatial structure of immunoglobulin molecules". Klin Wochenschr. 58 (22): 1217–31. PMID 6780722.
- ↑ Heyman B (1996). "Complement and Fc-receptors in regulation of the antibody response". Immunol Lett. 54 (2–3): 195–9. PMID 9052877.
- ↑ 19.0 19.1 Ravetch J, Bolland S (2001). "IgG Fc receptors". Annu Rev Immunol. 19: 275–90. PMID 11244038.
- ↑ Rus H, Cudrici C, Niculescu F (2005). "The role of the complement system in innate immunity". Immunol Res. 33 (2): 103–12. PMID 16234578.
- ↑ Mian I, Bradwell A, Olson A (1991). "Structure, function and properties of antibody binding sites". J Mol Biol. 217 (1): 133–51. PMID 1988675.
- ↑ Fanning LJ, Connor AM, Wu GE (1996). "Development of the immunoglobulin repertoire". Clin. Immunol. Immunopathol. 79 (1): 1–14. PMID 8612345.
- ↑ 23.0 23.1 Nemazee D (2006). "Receptor editing in lymphocyte development and central tolerance". Nat Rev Immunol. 6 (10): 728–40. PMID 16998507.
- ↑ Bergman Y, Cedar H (2004). "A stepwise epigenetic process controls immunoglobulin allelic exclusion". Nat Rev Immunol. 4 (10): 753–61. PMID 15459667.
- ↑ Honjo T, Habu S (1985). "Origin of immune diversity: genetic variation and selection". Annu Rev Biochem. 54: 803–30. PMID 3927822.
- ↑ 26.0 26.1 Or-Guil M, Wittenbrink N, Weiser AA, Schuchhardt J (2007). "Recirculation of germinal center B cells: a multilevel selection strategy for antibody maturation". Immunol. Rev. 216: 130–41. doi:10.1111/j.1600-065X.2007.00507.x. PMID 17367339.
- ↑ Neuberger M, Ehrenstein M, Rada C, Sale J, Batista F, Williams G, Milstein C (2000). "Memory in the B-cell compartment: antibody affinity maturation". Philos Trans R Soc Lond B Biol Sci. 355 (1395): 357–60. PMID 10794054.
- ↑ Stavnezer J, Amemiya CT (2004). "Evolution of isotype switching". Semin. Immunol. 16 (4): 257–75. PMID 15522624.
- ↑ Durandy A (2003). "Activation-induced cytidine deaminase: a dual role in class-switch recombination and somatic hypermutation". Eur. J. Immunol. 33 (8): 2069–73. PMID 12884279.
- ↑ Casali P, Zan H (2004). "Class switching and Myc translocation: how does DNA break?". Nat. Immunol. 5 (11): 1101–3. PMID 15496946.
- ↑ Lieber MR, Yu K, Raghavan SC (2006). "Roles of nonhomologous DNA end joining, V(D)J recombination, and class switch recombination in chromosomal translocations". DNA Repair (Amst.). 5 (9–10): 1234–45. PMID 16793349.
- ↑ "Animated depictions of how antibodies are used in [[ELISA]] assays". Cellular Technology Ltd.—Europe. Retrieved 2007-05-08. URL–wikilink conflict (help)
- ↑ "Animated depictions of how antibodies are used in [[ELISPOT]] assays". Cellular Technology Ltd.—Europe. Retrieved 2007-05-08. URL–wikilink conflict (help)
- ↑ Stern P (2006). "Current possibilities of turbidimetry and nephelometry" (PDF). Klin Biochem Metab. 14 (3): 146–151.
- ↑ 35.0 35.1 Dean, Laura (2005). "Chapter 4: Hemolytic disease of the newborn". Blood Groups and Red Cell Antigens. NCBI Bethesda (MD): National Library of Medicine (US),.
- ↑ Feldmann M, Maini R (2001). "Anti-TNF alpha therapy of rheumatoid arthritis: what have we learned?". Annu Rev Immunol. 19: 163–96. PMID 11244034.
- ↑ Doggrell S (2003). "Is natalizumab a breakthrough in the treatment of multiple sclerosis?". Expert Opin Pharmacother. 4 (6): 999–1001. PMID 12783595.
- ↑ Krueger G, Langley R, Leonardi C, Yeilding N, Guzzo C, Wang Y, Dooley L, Lebwohl M (2007). "A human interleukin-12/23 monoclonal antibody for the treatment of psoriasis". N Engl J Med. 356 (6): 580–92. PMID 17287478.
- ↑ Plosker G, Figgitt D (2003). "Rituximab: a review of its use in non-Hodgkin's lymphoma and chronic lymphocytic leukaemia". Drugs. 63 (8): 803–43. PMID 12662126.
- ↑ Vogel C, Cobleigh M, Tripathy D, Gutheil J, Harris L, Fehrenbacher L, Slamon D, Murphy M, Novotny W, Burchmore M, Shak S, Stewart S (2001). "First-line Herceptin monotherapy in metastatic breast cancer". Oncology. 61 Suppl 2: 37–42. PMID 11694786.
- ↑ LeBien TW (2000). "Fates of human B-cell precursors". Blood. 96 (1): 9–23. PMID 10891425.
- ↑ Ghaffer A (2006-03-26). "Immunization". Immunology - Chapter 14. University of South Carolina School of Medicine. Retrieved 2007-06-06.
- ↑ 43.0 43.1 Fung Kee Fung K, Eason E, Crane J, Armson A, De La Ronde S, Farine D, Keenan-Lindsay L, Leduc L, Reid G, Aerde J, Wilson R, Davies G, Désilets V, Summers A, Wyatt P, Young D (2003). "Prevention of Rh alloimmunization". J Obstet Gynaecol Can. 25 (9): 765–73. PMID 12970812.
- ↑ Urbaniak S, Greiss M (2000). "RhD haemolytic disease of the fetus and the newborn". Blood Rev. 14 (1): 44–61. PMID 10805260.
- ↑ Tini M, Jewell UR, Camenisch G, Chilov D, Gassmann M (2002). "Generation and application of chicken egg-yolk antibodies". Comp. Biochem. Physiol., Part A Mol. Integr. Physiol. 131 (3): 569–74. PMID 11867282.
- ↑ Cole SP, Campling BG, Atlaw T, Kozbor D, Roder JC (1984). "Human monoclonal antibodies". Mol. Cell. Biochem. 62 (2): 109–20. PMID 6087121.
- ↑ Kabir S (2002). "Immunoglobulin purification by affinity chromatography using protein A mimetic ligands prepared by combinatorial chemical synthesis". Immunol Invest. 31 (3–4): 263–78. PMID 12472184.
- ↑ 48.0 48.1 Brehm-Stecher B, Johnson E (2004). "Single-cell microbiology: tools, technologies, and applications". Microbiol Mol Biol Rev. 68 (3): 538–59. PMID 15353569.
- ↑ Williams N (2000). "Immunoprecipitation procedures". Methods Cell Biol. 62: 449–53. PMID 10503210.
- ↑ Kurien B, Scofield R (2006). "Western blotting". Methods. 38 (4): 283–93. PMID 16483794.
- ↑ Scanziani E. "Immunohistochemical staining of fixed tissues". Methods Mol Biol. 104: 133–40. PMID 9711649.
- ↑ Reen DJ. (1994). "Enzyme-linked immunosorbent assay (ELISA)". Methods Mol Biol. 32: 461–6. PMID 7951745.
- ↑ Kalyuzhny AE (2005). "Chemistry and biology of the ELISPOT assay". Methods Mol Biol. 302: 15–31. PMID 15937343.
- ↑ "Emil von Behring - Biography". Retrieved 2007-06-05.
- ↑ AGN (1931). "The Late Baron Shibasaburo Kitasato". Canadian Medical Association Journal: 206.
- ↑ Winau F, Westphal O, Winau R (2004). "Paul Ehrlich--in search of the magic bullet". Microbes Infect. 6 (8): 786–9. doi:10.1016/j.micinf.2004.04.003. PMID 15207826.
- ↑ Silverstein AM (2003). "Cellular versus humoral immunology: a century-long dispute". Nat. Immunol. 4 (5): 425–8. doi:10.1038/ni0503-425. PMID 12719732.
- ↑ Van Epps HL (2006). "Michael Heidelberger and the demystification of antibodies" (PDF). J. Exp. Med. 203 (1): 5. PMID 16523537.
- ↑ Marrack, JR (1938). Chemistry of antigens and antibodies (2nd ed. ed.). London: His Majesty's Stationery Office. OCLC 3220539.
- ↑ "The Linus Pauling Papers: How Antibodies and Enzymes Work". Retrieved 2007-06-05.
- ↑ Silverstein AM (2004). "Labeled antigens and antibodies: the evolution of magic markers and magic bullets" (PDF). Nat. Immunol. 5 (12): 1211–7. doi:10.1038/ni1140. PMID 15549122.
- ↑ Edelman GM, Gally JA (1962). "The nature of Bence-Jones proteins. Chemical similarities to polypetide chains of myeloma globulins and normal gamma-globulins". J. Exp. Med. 116: 207–27. PMID 13889153.
- ↑ Stevens FJ, Solomon A, Schiffer M (1991). "Bence Jones proteins: a powerful tool for the fundamental study of protein chemistry and pathophysiology". Biochemistry. 30 (28): 6803–5. PMID 2069946.
- ↑ 64.0 64.1 Raju TN (1999). "The Nobel chronicles. 1972: Gerald M Edelman (b 1929) and Rodney R Porter (1917-85)". Lancet. 354 (9183): 1040. PMID 10501404.
- ↑ Tomasi TB (1992). "The discovery of secretory IgA and the mucosal immune system". Immunol. Today. 13 (10): 416–8. PMID 1343085.
- ↑ Preud'homme JL, Petit I, Barra A, Morel F, Lecron JC, Lelièvre E (2000). "Structural and functional properties of membrane and secreted IgD". Mol. Immunol. 37 (15): 871–87. PMID 11282392.
- ↑ Johansson SG (2006). "The discovery of immunoglobulin E". Allergy and asthma proceedings : the official journal of regional and state allergy societies. 27 (2 Suppl 1): S3–6. PMID 16722325.
- ↑ Hozumi N, Tonegawa S (1976). "Evidence for somatic rearrangement of immunoglobulin genes coding for variable and constant regions". Proc. Natl. Acad. Sci. U.S.A. 73 (10): 3628–32. PMID 824647.
External links[edit | edit source]
- Mike's Immunoglobulin Structure/Function Page at University of Cambridge
- Antibodies as the PDB molecule of the month Discussion of the structure of antibodies at Protein Data Bank
- Microbiology and Immunology On-line Textbook at University of South Carolina
- A hundred years of antibody therapy History and applications of antibodies in the treatment of disease at University of Oxford
- How Lymphocytes Produce Antibody from Cells Alive!
- Antibody applications Fluorescent antibody image library, University of Birmingham
- Images produced using antibodies at antibodypatterns.com
Template:Link FA ar:ضد (مناعة) Template:Link FA bn:অ্যান্টিবডি bg:Антитяло ca:Anticòs cs:Protilátka da:Antistof (biologi) de:Antikörper et:Antikehad fa:پادتن ko:항체 id:Antibodi it:Anticorpo he:נוגדן lt:Antikūnas hu:Ellenanyag nl:Antistof nl:Immunoglobuline no:Antistoff simple:Antibody sk:Protilátka sl:Protitelo sr:Антитело sh:Antitelo fi:Vasta-aine sv:Antikropp th:แอนติบอดี uk:Антитіло ur:ضد (سائنس)
 KSF
KSF