Asthma pathophysiology
 From Wikidoc - Reading time: 8 min
From Wikidoc - Reading time: 8 min
| https://https://www.youtube.com/watch?v=fEKc37vrQ_I%7C350}} |
|
Asthma Microchapters |
|
Diagnosis |
|---|
|
Other Diagnostic Studies |
|
Treatment |
|
Case Studies |
|
Asthma pathophysiology On the Web |
|
American Roentgen Ray Society Images of Asthma pathophysiology |
|
Risk calculators and risk factors for Asthma pathophysiology |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Philip Marcus, M.D., M.P.H. [2]; Associate Editor(s)-In-Chief: Varun Kumar, M.B.B.S. [3]; Lakshmi Gopalakrishnan, M.B.B.S. [4]
Overview[edit | edit source]
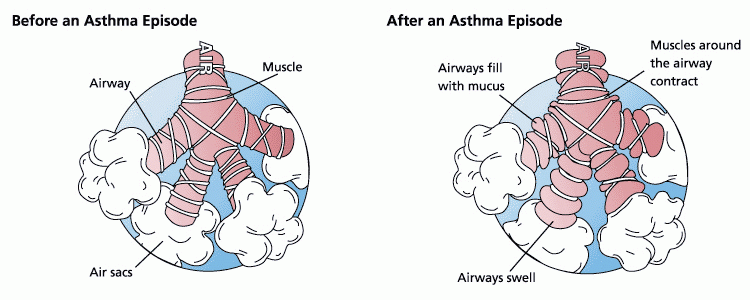
Asthma is a chronic inflammatory disease of the airways that is characterized by reversible airflow obstruction and airway inflammation, persistent airway hyperreactivity, and airway remodeling.[1] The two major factors responsible for the pathogenesis of asthma include bronchial hyper-responsiveness and inflammatory reaction within the bronchial wall. The airways of asthmatics are hypersensitive to certain triggers such as smoke, dust, or pollen. The term trigger is synonymous with stimuli. Exposure to these triggers causes repeated inflammation of the airways resulting in bronchospasm. Bronchospasm can lead to narrowing of airways and excess mucus production, making it difficult to breathe. Airway inflammation is a chronic inflammation driven by TH2 lymphocyte-predominant immune response. This immune response has been associated with atopy and IgE-synthesis through the production of IL-4 and eosinophilic inflammation by means of IL-5.[1]
Pathophyisology[edit | edit source]
Stimuli or Triggering Factors[edit | edit source]
The allergens responsible for the pathogenesis of asthma enter the body either as inspired air or ingested food that subsequently stimulate the formation of IgE and result in an antigen-antibody reaction within the bronchial wall; which cause the release of active inflammatory mediators that provoke bronchial spasm and immediate asthmatic attack. Known stimuli or triggering factors include the following.
- Allergenic air pollution, such as: waste from common household pests, such as the house dust mite and cockroach, grass pollen, mould spores, and pet epithelial cells. These are typically inhaled and the body's introduction to the stimuli occurs through the respiratory system.
- Indoor allergenic air pollution from volatile organic compounds (VCOs). Potential VCOs include: soap, dishwashing liquid, laundry detergent, fabric softener, paper tissues, paper towels, toilet paper, shampoo, hairspray, hair gel, cosmetics, facial cream, sun cream, deodorant, cologne, shaving cream, aftershave lotion, air freshener and candles, and products such as oil-based paints. This also includes perfumes and perfumed products.
- Medications such as aspirin,[2] β-adrenergic antagonists, and penicillin.
- An allergy to food such as: milk, peanuts, and eggs. However, asthma is rarely the only symptom, and not all people with food or other allergies have asthma.
- Use of fossil fuel, related to allergenic air pollution, such as: ozone, smog, summer smog, nitrogen dioxide, and sulfur dioxide. This is believed to be one of major reasons for the high prevalence of asthma in urban areas.
- Various industrial compounds and other chemicals. Most notably sulfites; chlorinated swimming pools generate chloramines— monochloramine (NH2Cl), dichloramine (NHCl2) and trichloramine (NCl3)— in the air around them, which are known to induce asthma.[3]
- Early childhood infections, especially viral respiratory infections. However, persons of any age can have asthma triggered by colds and other respiratory infections even though their normal stimuli might be from another category (e.g. pollen) and absent at the time of infection. 80% of asthma attacks in adults and 60% in children are caused by respiratory viruses.
- Exercise, see exercise induced asthma. The effects of exercise differ somewhat from those of the other triggers.
- Allergenic indoor air pollution, in some countries, from newsprint & other literature such as: direct marketing/junk mail leaflets & glossy magazines.
- Hormone changes in adolescent girls and adult women, associated with the menstrual cycle, can lead to a worsening of asthma. The influence of hormones can be largely varied from person to person. Some women also experience a worsening of their asthma during pregnancy, whereas others find no significant changes, and in other women their asthma improves during their pregnancy.
- Emotional stress is a recognized potential trigger/stimuli, however, the influence of such is not well understood.
- Cold weather can adversely affect breathing in asthmatics.
Pathogenesis[edit | edit source]
- Pathogenesis of asthma involves a number of cells such as, mast cells, macrophages, eosinophils and lymphocytes, that cause the release of inflammatory mediators leading to the synthesis of IgE through IL-4 production and eosinophilic inflammation through IL-5 production.
- Mast cells generate the release of inflammatory mediators such as histamine, prostaglandin D2 and leukotriene C4 from the bronchial smooth muscles to cause an immediate asthmatic reaction and are found in increased concentration in the mucus secretions of asthmatics.
- Macrophages, such as prostaglandins, thromboxane, leukotriene C4, are known as the antigen presenting cells that ingest the allergens and present to lymphocytes. Lmphocytes activate mast cells through the release IL-3, IL-4, IL-9 and activate eosinophils through the release of IL-3 and IL-5.
- Secretion of IL-4 helps in the switching of antibody production by B-cells to IgE-type.
- All these mediators subsequently lead to chronic bronchial inflammation, bronchial constriction and hypertrophy of the mucus-producing glands.
Bronchial Inflammation[edit | edit source]
- In both asthmatics and non-asthmatics, inhaled allergens that find their way to the inner airways are ingested by antigen presenting cells, or APCs.
- APCs then present pieces of the allergen to other cells of immune system.
- In most people, these other immune cells (TH0 cells) usually ignore the allergen molecules. In asthmatics, however, these cells differentiate into TH2, for reasons that are not well understood.[1]
- The resultant TH2 cells activate an important arm of the immune system, known as the humoral immune system that produces antibodies against the inhaled allergen.
- Later, when an asthmatic inhales the same allergen, these antibodies recognize it and activate a humoral response.
Bronchoconstriction[edit | edit source]
- The resultant humoral response following a specific stimuli, causes the hypersensitive bronchial airways to constrict and release more mucus, and cause the activation of the cell-mediated arm of the immune system.[1]
- This inflammatory response is responsible for the clinical manifestations of an asthma attack. The following section describes this complex series of events in more detail.
Theories of Pathogenesis[edit | edit source]
- The fundamental problem in asthma appears to be immunological. Young children in the early stages of asthma show signs of excessive inflammation in their airways.
- Epidemiological findings give a clue to the pathogenesis of asthma. The incidence of asthma seems to be increasing worldwide, and asthma is now very much more common in affluent countries.
- In 1968, Andor Szentivanyi first described The Beta Adrenergic Theory of Asthma; in which blockage of the beta-2 receptors of pulmonary smooth muscle cells, decreased the adrenergic bronchodilator activity and associated hypersensitivity to mediators and contributed to the pathogenesis of asthma.[4]
- In 1995, Szentivanyi and colleagues demonstrated that IgE blocks beta-2 receptors.[5] Since overproduction of IgE is central to all atopic diseases, this was a watershed moment in the world of allergy.[6]
- Many studies have linked asthma, bronchitis, and acute respiratory illnesses to air quality experienced by children.[7] This study showed that children in the high ozone communities who played three or more sports developed asthma at a rate three times higher than those in the low ozone communities. Because participation in some sports can result in a child drawing up to 17 times the normal amount of air into the lungs, young athletes are more likely to develop asthma.
- Another theory of pathogenesis is that asthma is a disease of hygiene. In nature, children are exposed to bacteria and other antigens soon after birth, switching on the TH1 lymphocyte cells of the immune system that deal with bacterial infection. If this stimulus is insufficient, as it may be in modern, clean environments, then TH2 cells predominate, and asthma and other allergic diseases may develop. This hygiene hypothesis may explain the increase in asthma in affluent populations.
- The TH2 lymphocytes and eosinophil cells that protect us against parasites and other infectious agents are the same cells responsible for the allergic reaction. Charcot-Leyden crystals are formed when crystalline material in eosinophils coalesce. These crystals are significant in sputum samples of people with asthma. In the developed world, the parasites that eosinophils are programmed to combat are now rarely encountered, but the immune response remains and is wrongly triggered in some individuals by certain allergens.
- It has been postulated that some forms of asthma may be related to infection, particularly to Chlamydia pneumoniae.[8] This issue remains controversial, as the relationship is not borne out by meta-analysis of the research.[9] The correlation seems to be not with the onset, but rather with accelerated loss of lung function in adults with new onset of non-atopic asthma.[10] One possible explanation is that some asthmatics may have altered immune response that facilitates long-term chlamydia pneumonia infection.[11] The response to targeting with macrolide antibiotics has been investigated, but the temporary benefit reported in some studies may reflect just their anti-inflammatory activities rather than their anti- microbic action.[12]
- A study conducted by the National Jewish Medical and Research Center concluded that factors such as being overweight and or obese were associated with a dose-dependent increase in the odds of incident asthma in men and women. This demonstrates that asthma incidence could be reduced by interventions targeting overweight and obese populations.[13]
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 Maddox L, Schwartz DA (2002) The pathophysiology of asthma. Annu Rev Med 53 ():477-98. DOI:10.1146/annurev.med.53.082901.103921 PMID: 11818486
- ↑ Jenkins C, Costello J, Hodge L (2004) Systematic review of prevalence of aspirin induced asthma and its implications for clinical practice. BMJ 328 (7437):434. DOI:10.1136/bmj.328.7437.434 PMID: 14976098
- ↑ Nemery B, Hoet PH, Nowak D (2002) Indoor swimming pools, water chlorination and respiratory health. Eur Respir J 19 (5):790-3. PMID: 12030714
- ↑ Townley RG (2007) Interleukin 13 and the beta-adrenergic blockade theory of asthma revisited 40 years later. Ann Allergy Asthma Immunol 99 (3):215-24. DOI:10.1016/S1081-1206(10)60656-4 PMID: 17910324
- ↑ (1993) 50th Anniversary of the American Academy of Allergy and Immunology. 49th Annual Meeting. Chicago, Illinois, March 12-17, 1993. Abstracts. J Allergy Clin Immunol 91 (1 Pt 2):141-379. PMID: 8421135
- ↑ Kowalak JP, Hughes AS et al (eds), ed. (2001). Professional Guide To Diseases (7th ed. ed.). Springhouse.
- ↑ "Asthma and Air Quality".
- ↑ Harju TH, Leinonen M, Nokso-Koivisto J, Korhonen T, Räty R, He Q et al. (2006) Pathogenic bacteria and viruses in induced sputum or pharyngeal secretions of adults with stable asthma. Thorax 61 (7):579-84. DOI:10.1136/thx.2005.056291 PMID: 16517571
- ↑ Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG (2005) Macrolides for chronic asthma. Cochrane Database Syst Rev (4):CD002997. DOI:10.1002/14651858.CD002997.pub3 PMID: 16235309
- ↑ Pasternack R, Huhtala H, Karjalainen J (2005) Chlamydophila (Chlamydia) pneumoniae serology and asthma in adults: a longitudinal analysis. J Allergy Clin Immunol 116 (5):1123-8. DOI:10.1016/j.jaci.2005.08.030 PMID: 16275386
- ↑ Ronchetti R, Biscione GL, Ronchetti F, Ronchetti MP, Martella S, Falasca C et al. (2005) Why Chlamydia pneumoniae is associated with asthma and other chronic conditions? Suggestions from a survey in unselected 9 yr old schoolchildren. Pediatr Allergy Immunol 16 (2):145-50. DOI:10.1111/j.1399-3038.2005.00244.x PMID: 15787872
- ↑ Richeldi L, Ferrara G, Fabbri LM, Lasserson TJ, Gibson PG (2005) Macrolides for chronic asthma. Cochrane Database Syst Rev (3):CD002997. DOI:10.1002/14651858.CD002997.pub2 PMID: 16034882
- ↑ Beuther DA, Sutherland ER (2007) Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med 175 (7):661-6. DOI:10.1164/rccm.200611-1717OC PMID: 17234901
 KSF
KSF