Birth control
 From Wikidoc - Reading time: 19 min
From Wikidoc - Reading time: 19 min
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor-In-Chief: Cafer Zorkun, M.D., Ph.D. [2]
|
WikiDoc Resources for Birth control |
|
Articles |
|---|
|
Most recent articles on Birth control Most cited articles on Birth control |
|
Media |
|
Powerpoint slides on Birth control |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Birth control at Clinical Trials.gov Trial results on Birth control Clinical Trials on Birth control at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Birth control NICE Guidance on Birth control
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Birth control Discussion groups on Birth control Patient Handouts on Birth control Directions to Hospitals Treating Birth control Risk calculators and risk factors for Birth control
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Birth control |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Synonyms and keywords: Contraception
Overview
[edit | edit source]Birth control is a regimen of one or more actions, devices, or medications followed in order to deliberately prevent or reduce the likelihood of pregnancy or childbirth. Contraception may refer specifically to mechanisms which are intended to reduce the likelihood of the fertilisation of an ovum by a spermatozoon.
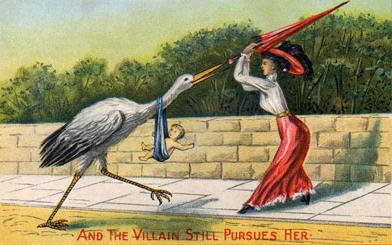
The history of birth control began with the discovery of the connection between coitus and pregnancy. The oldest forms of birth control included coitus interruptus, pessaries, and the ingestion of herbs that were believed to be contraceptive or abortifacient. The earliest record of birth control use is instructions on creating a contraceptive pessary from Ancient Egypt.
Different methods of birth control have varying characteristics. Condoms, for example, are the only method that provides significant protection from sexually transmitted diseases.
Because of the sexual and ethical nature of the subject, cultural and religions attitudes on birth control vary significantly.
Historical Perspective
[edit | edit source]
Probably the oldest methods of contraception (aside from sexual abstinence) are coitus interruptus, certain barrier methods, and herbal methods (emmenagogues and abortifacients).
Coitus interruptus (withdrawal of the penis from the vagina prior to ejaculation) probably predates any other form of birth control. Once the relationship between the emission of semen into the vagina and pregnancy was known or suspected, some men began to use this technique. This is not a particularly reliable method of contraception, as few men have the self-control to correctly practice the method at every single act of sexual intercourse. Although it is commonly believed that pre-ejaculate fluid can cause pregnancy, modern research has shown that pre-ejaculate fluid does not contain viable sperm.[1][2]
There are historic records of Egyptian women using a pessary (a vaginal suppository) made of various acidic substances and lubricated with honey or oil, which may have been somewhat effective at killing sperm.[3] However, it is important to note that the sperm cell was not discovered until Anton van Leeuwenhoek invented the microscope in the late 17th century, so barrier methods employed prior to that time could not know of the details of conception. Asian women may have used oiled paper as a cervical cap, and Europeans may have used beeswax for this purpose. The condom appeared sometime in the 17th century, initially made of a length of animal intestine. It was not particularly popular, nor as effective as modern latex condoms, but was employed both as a means of contraception and in the hopes of avoiding syphilis, which was greatly feared and devastating prior to the discovery of antibiotic drugs.
Various abortifacients have been used throughout human history. Some of them were effective, some were not; those that were most effective also had major side effects. One abortifacient reported to have low levels of side effects — silphium — was harvested to extinction around the 1st century.[4] The ingestion of certain poisons by the female can disrupt the reproductive system; women have drunk solutions containing mercury, arsenic, or other toxic substances for this purpose. The Greek gynaecologist Soranus in the 2nd century suggested that women drink water that blacksmiths had used to cool metal. The herbs tansy and pennyroyal are well-known in folklore as abortive agents, but these also "work" by poisoning the woman. Levels of the active chemicals in these herbs that will induce a miscarriage are high enough to damage the liver, kidneys, and other organs, making them very dangerous. However, in those times where risk of maternal death from postpartum complications was high, the risks and side effects of toxic medicines may have seemed less onerous. Some herbalists claim that black cohosh tea will also be effective in certain cases as an abortifacient.[5]
Aside from abortifacients, herbal contraceptives in folklore have also included a few preventative measures. Hibiscus rosa-sinensis, known in Ayurveda as a contraceptive, may have antiestrogenic properties.[6] Papaya seeds, rumored to be a male contraceptive, have recently been studied for their azoospermic effect on monkeys.[7]
The fact that various effective methods of birth control were known in the ancient world sharply contrasts with a seeming ignorance of these methods in wide segments of the population of early modern Christian Europe. This ignorance continued far into the 20th century, and was paralleled by eminently high birth rates in European countries during the 18th and 19th centuries.[8] Some historians have attributed this to a series of coercive measures enacted by the emerging modern state, in an effort to repopulate Europe after the population catastrophe of the Black Death, starting in 1348. According to this view, the witch hunts were the first measure the modern state took in an attempt to eliminate knowledge about birth control within the population, and monopolize it in the hands of state-employed male medical specialists (gynecologists). Prior to the witch hunts, male specialists were unheard of, because birth control was naturally a female domain.[9]
Presenters at a family planning conference told a tale of Arab traders inserting small stones into the uteruses of their camels in order to prevent pregnancy, a concept very similar to the modern IUD. Although the story has been repeated as truth, it has no basis in history and was meant only for entertainment purposes.[10] The first interuterine devices (which occupied both the vagina and the uterus) were first marketed around 1900. The first modern intrauterine device (contained entirely in the uterus) was described in a German publication in 1909, although the author appears to have never marketed his product.[11]
The Rhythm Method (with a rather high method failure rate of ten percent per year) was developed in the early 20th century, as researchers discovered that a woman only ovulates once per menstrual cycle. Not until the 1950s, when scientists better understood the functioning of the menstrual cycle and the hormones that controlled it, were methods of hormonal contraception and modern methods of fertility awareness (also called natural family planning) developed.
Methods
[edit | edit source]Clinical practice guidelines by the U.S. Centers for Disease Control and Prevention[12], with update focusing on contraception after the use of emergency contraceptive pills and medications to ease insertion of intrauterine devices[13].
Physical Methods
[edit | edit source]Barrier Methods
[edit | edit source]
Barrier methods place a physical impediment to the movement of sperm into the female reproductive tract.
The most popular barrier method is the male condom, a latex or polyurethane sheath placed over the penis. The condom is also available in a female version, which is made of polyurethane. The female condom has a flexible ring at each end — one secures behind the pubic bone to hold the condom in place, while the other ring stays outside the vagina.
Cervical barriers are devices that are contained completely within the vagina. The contraceptive sponge has a depression to hold it in place over the cervix. The cervical cap is the smallest cervical barrier. It stays in place by suction to the cervix or to the vaginal walls. The Lea's shield is a larger cervical barrier, also held in place by suction. The diaphragm fits into place behind the woman's pubic bone and has a firm but flexible ring, which helps it press against the vaginal walls.
The SILCS diaphragm is a new diaphragm design which is still in clinical testing and is not yet available.
Hormonal Methods
[edit | edit source]
There are variety of delivery methods for hormonal contraception.
Combinations of synthetic oestrogens and progestins (synthetic progestogens) are commonly used. These include the combined oral contraceptive pill ("The Pill"), the Patch, and the contraceptive vaginal ring ("NuvaRing"). Not currently available for sale in the United States is Lunelle, a monthly injection.
Other methods contain only a progestin (a synthetic progestogen). These include the progestin only pill (the POP or 'minipill'), the injectables Depo Provera (a depot formulation of medroxyprogesterone acetate given as an intramuscular injection every three months) and Noristerat (norethisterone acetate given as an intramuscular injection every 8 weeks), and contraceptive implants. The progestin-only pill must be taken at more precisely remembered times each day than combined pills. The first contraceptive implant, the original 6-capsule Norplant, was removed from the market in the United States in 1999, though a newer single-rod implant called Implanon was approved for sale in the United States on July 17, 2006. The various progestin-only methods may cause irregular bleeding during use.
Ormeloxifene (Centchroman)
[edit | edit source]Ormeloxifene (Centchroman) is a selective oestrogen receptor modulator, or SERM. It causes ovulation to occur asynchronously with the formation of the uterine lining, preventing implantation of a zygote. It has been widely available as a birth control method in India since the early 1990s, marketed under the trade name Saheli. Centchroman is legally available only in India.
Intrauterine Methods
[edit | edit source]
These are contraceptive devices which are placed inside the uterus. They are usually shaped like a "T" — the arms of the T hold the device in place. There are two main types of intrauterine contraceptives: those that contain copper (which has a spermicidal effect), and those that release a progestogen (in US the term progestin used).
The terminology used for these devices differs in the United Kingdom and the United States. In the US, all devices which are placed in the uterus to prevent pregnancy are referred to as Intra-Uterine Devices (IUDs). In the UK, only copper-containing devices are called IUDs, and hormonal intrauterine contraceptives are referred to with the term Intra-Uterine System (IUS). This may be because there are seven types of copper IUDs available in the UK, compared to only one in the US.
Emergency Contraception
[edit | edit source]Template:Seealso Some combined pills and POPs may be taken in high doses to prevent pregnancy after a birth control failure (such as a condom breaking) or after unprotected sex. Hormonal emergency contraception is also known as the "morning after pill," although it is licensed for use up to three days after intercourse.
Copper intrauterine devices may also be used as emergency contraception. For this use, they must be inserted within five days of the birth control failure or unprotected intercourse.
Because emergency contraception may prevent a fertilized egg from developing, some people consider it a form of abortion.
Induced Abortion
[edit | edit source]Abortion can be done with surgical methods, usually suction-aspiration abortion (in the first trimester) or dilation and evacuation (in the second trimester). Medical abortion uses drugs to end a pregnancy and is approved for pregnancies where the length of gestation has not exceeded 8 weeks.
Some herbs are believed to cause abortion (abortifacients). The efficacy of these plants as such has never been studied in humans. Some animal studies have found them to be effective on other species.[14][5] The use of herbs to induce abortion is not recommended due to the risk of serious side effects.
Abortion is subject to ethical debate.
Sterilization
[edit | edit source]Surgical sterilization is available in the form of tubal ligation for women and vasectomy for men. In women, the process may be referred to as "tying the tubes," but the fallopian tubes may be tied, cut, clamped, or blocked. This serves to prevent sperm from joining the unfertilized egg. The non-surgical sterilization procedure, Essure, is an example of a procedure that blocks the tubes. Sterilization should be considered permanent.
Behavioral Methods
[edit | edit source]Fertility Awareness
[edit | edit source]Symptoms-based methods of fertility awareness involve a woman's observation and charting of her body's fertility signs, to determine the fertile and infertile phases of her cycle. Most methods track one or more of the three primary fertility signs:[15] changes in basal body temperature, in cervical mucus, and in cervical position. If a woman tracks both basal body temperature and another primary sign, the method is referred to as symptothermal. Some fertility monitoring devices use urinalysis to follow the levels of estrogen and luteinizing hormone throughout a woman's menstrual cycle. Other bodily cues such as mittelschmerz are considered secondary indicators.
Calendar-based methods such as the Rhythm method and Standard Days Method are dissimilar from symptoms-based fertility awareness methods, in that they do not involve the observation or recording of bodily cues of fertility. Instead, statistical methods estimate the likelihood of fertility based on the length of past menstrual cycles. Statistical methods are less accurate than fertility awareness methods, and are considered by many fertility awareness teachers to have been obsolete for at least 20 years.
Charting of the menstrual cycle may be done by the woman on paper or with the assistance of software. The calendar-based methods may use a device such as CycleBeads. Symptoms-based methods may be assisted by fertility monitoring devices that accept and interpret temperature readings, information from home urinalysis tests, or both. To avoid pregnancy with fertility awareness, unprotected sex is restricted to the least fertile period. During the most fertile period, barrier methods may be availed, or she may abstain from intercourse.
The term natural family planning (NFP) is sometimes used to refer to any use of FA methods. However, this term specifically refers to the practices which are permitted by the Roman Catholic Church — breastfeeding infertility, and periodic abstinence during fertile times. FA methods may be used by NFP users to identify these fertile times.
Coitus Interruptus
[edit | edit source]Coitus interruptus (literally "interrupted sex"), also known as the withdrawal method, is the practice of ending sexual intercourse ("pulling out") before ejaculation. The main risk of coitus interruptus is that the man may not make the maneuver in time. Although concern has been raised about the risk of pregnancy from sperm in pre-ejaculate, several small studies[1][2] have failed to find any viable sperm in the fluid.
Avoiding Vaginal Intercourse
[edit | edit source]The risk of pregnancy from non-vaginal sex, such as outercourse (sex without penetration), anal sex, or oral sex is virtually zero. (A very small risk comes from the possibility of semen leaking onto the vulva (with anal sex) or coming into contact with an object, such as a hand, that later contacts the vulva). However, with this method, care must be taken to prevent the progression to intercourse.
Abstinence
[edit | edit source]Sexual abstinence is the practice of refraining from all sexual activity.
Lactational
[edit | edit source]Most breastfeeding women have a period of infertility after the birth of their child. The lactational amenorrhea method, or LAM, gives guidelines for determining the length of a woman's period of breastfeeding infertility.
Methods in Development
[edit | edit source]For Females
[edit | edit source]- Praneem is a polyherbal vaginal tablet being studied as a spermicide, and a microbicide active against HIV.[16]
- BufferGel is a spermicidal gel being studied as a microbicide active against HIV.[17]
- Duet is a disposable diaphragm in development that will be pre-filled with BufferGel.[18] It is designed to deliver microbicide to both the cervix and vagina. Unlike currently available diaphragms, the Duet will be manufactured in only one size and will not require a prescription, fitting, or a visit to a doctor.[17]
- The SILCS diaphragm is a silicone barrier which is still in clinical testing. It has a finger cup molded on one end for easy removal. Like the Duet, the SILCS is novel in that it will only be available in one size.
- A vaginal ring is being developed that releases both estrogen and progesterone, and is effective for over 12 months.[19]
- Two types of progestogen-only vaginal rings are being developed. Progestogen-only products may be particularly useful for women who are breastfeeding.[19] The rings may be used for four months at a time.[20]
- A progesterone-only contraceptive is being developed that would be sprayed onto the skin once a day.[21]
- Quinacrine sterilization and the Adiana procedure are two permanent methods of birth control being developed.[22]
For Males
[edit | edit source]Other than condoms and withdrawal, there are currently no available methods of reversible contraception which males can use or control. Several methods are in research and development:
- As of 2007, a chemical called Adjudin is currently in Phase II human trials as a male oral contraceptive.[23]
- RISUG (Reversible Inhibition of Sperm Under Guidance), is an experimental injection into the vas deferens that coats the walls of the vas with a spermicidal substance. The method can potentially be reversed by washing out the vas deferens with a second injection.
- Experiments in vas-occlusive contraception involve an implant placed in the vasa deferentia.
- Experiments in heat-based contraception involve heating a man's testicles to a high temperature for a short period of time.
Misconceptions
[edit | edit source]Modern misconceptions and urban legends have given rise to a great deal of false claims:
- The suggestion that douching immediately following intercourse works as a contraceptive is untrue. While it may seem like a sensible idea to try to wash the ejaculate out of the vagina, it is not likely to be effective. Due to the nature of the fluids and the structure of the female reproductive tract – if anything, douching spreads semen further towards the uterus. Some slight spermicidal effect may occur if the douche solution is particularly acidic, but overall it is not scientifically observed to be a reliably effective method.
- The suggestion to shake a bottle of Coca-Cola and insert it into the vagina after ejaculation is not a form of birth control, it does not prevent pregnancy, and doing this can also promote candidiasis (yeast infections).
- It is a myth that a female cannot become pregnant as a result of the first time she engages in sexual intercourse.
- While women are usually less fertile for the first few days of menstruation,[24] it is a myth that a woman absolutely cannot get pregnant if she has sex during her period.
- Having sex in a hot tub does not prevent pregnancy, but may contribute to vaginal infections.
- Although some sex positions may encourage pregnancy, no sexual positions prevent pregnancy. Having sex while standing up or with a woman on top will not keep the sperm from entering the uterus. The force of ejaculation, the contractions of the uterus caused by prostaglandins in the semen, as well as ability of sperm to swim overrides gravity.
- Sneezing after sex is also completely ineffective.
- Urinating after sex does not prevent pregnancy and is not a form of birth control, although it is often advised anyway to help prevent urinary tract infections.[25]
- Toothpaste cannot be used as an effective contraceptive[26]
Effectiveness
[edit | edit source]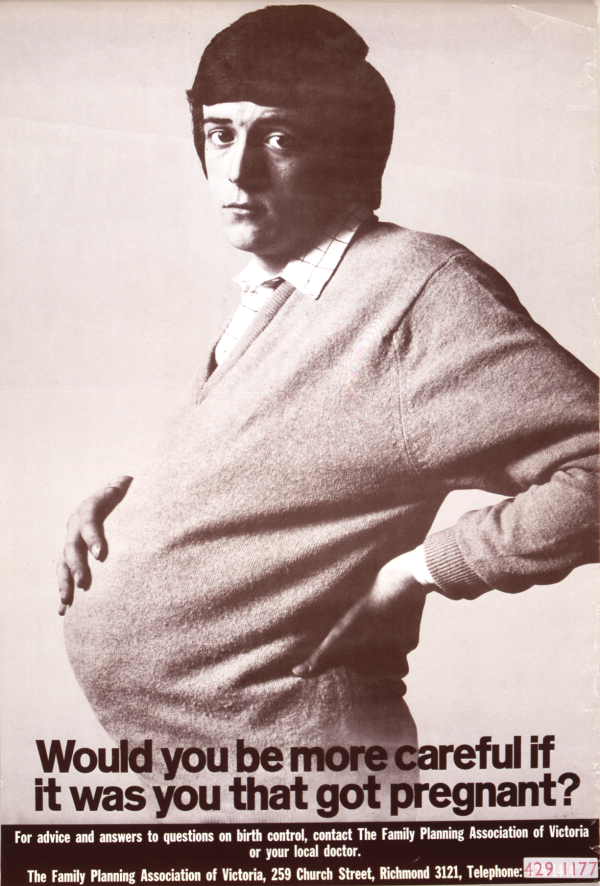
- See also the table at: Comparison of birth control methods
Effectiveness is measured by how many women become pregnant using a particular birth control method in the first year of use. Thus, if 100 women use a method that has a 12 percent first-year failure rate, then sometime during the first year of use, 12 of the women should become pregnant.
The most effective methods in typical use are those that do not depend upon regular user action. Surgical sterilization, Depo-Provera, implants, and intrauterine devices (IUDs) all have first-year failure rates of less than one percent for perfect use. Sterilization, implants, and IUDs also have typical failure rates under one percent. The typical failure rate of Depo-Provera is disagreed upon, with figures ranging from less than one percent up to three percent.[27][28]
Other methods may be highly effective if used consistently and correctly, but can have typical use first-year failure rates that are considerably higher due to incorrect or ineffective usage by the user. Hormonal contraceptive pills, patches or rings, fertility awareness methods, and the lactational amenorrhea method (LAM), if used strictly, have first-year (or for LAM, first-6-month) failure rates of less than 1%.[29][30][31][32] In one survey, typical use first-year failure rates of hormonal contraceptive pills (and by extrapolation, patches or rings) were as high as five percent per year. Fertility awareness methods as a whole have typical use first-year failure rates as high as 25 percent per year; however, as stated above, perfect use of these methods reduces the first-year failure rate to less than 1%.[27]
Condoms and cervical barriers such as the diaphragm have similar typical use first-year failure rates (14 and 20 percent, respectively), but perfect usage of the condom is more effective (three percent first-year failure vs six percent) and condoms have the additional feature of helping to prevent the spread of sexually transmitted diseases such as the HIV virus. The withdrawal method, if used consistently and correctly, has a first-year failure rate of four percent. Due to the difficulty of consistently using withdrawal correctly, it has a typical use first-year failure rate of 19 percent,[27] and is not recommended by some medical professionals.[33]
Protection Against Sexually Transmitted Infections
[edit | edit source]Not all methods of birth control offer protection against sexually transmitted infections. Abstinence from all forms of sexual behavior will protect against the sexual transmission of these infections. The male latex condom offers some protection against some of these diseases with correct and consistent use, as does the female condom, although the latter has only been approved for vaginal sex. The female condom may offer greater protection against sexually transmitted infections that pass through skin to skin contact, as the outer ring covers more exposed skin than the male condom, and can be used during anal sex to guard against sexually transmitted infections. However, the female condom can be difficult to use. Frequently a woman can improperly insert it, even if she believes she is using it correctly.
The remaining methods of birth control do not offer significant protection against the sexual transmission of these diseases.
However, so-called sexually transmitted infections may also be transmitted non-sexually, and therefore, abstinence from sexual behavior does not guarantee 100 percent protection against sexually transmitted infections. For example, HIV may be transmitted through contaminated needles which may be used in intravenous drug use, tattooing, body piercing, or injections. Health-care workers have acquired HIV through occupational exposure to accidental injuries with needles.[34]
Religious and Cultural Attitudes
[edit | edit source]Religious Views on Birth Control
[edit | edit source]Religions vary widely in their views of the ethics of birth control. In Christianity, the Roman Catholic Church accepts only Natural Family Planning,[35] while Protestants maintain a wide range of views from allowing none to very lenient.[36] Views in Judaism range from the stricter Orthodox sect to the more relaxed Reformed sect.[37] In Islam, contraceptives are allowed if they do not threaten health or lead to sterilty, although their use is discouraged.[38] Hindus may use both natural and artificial contraceptives.[39]
Birth Control Education
[edit | edit source]Many teenagers, most commonly in developed countries, receive some form of sex education in school. What information should be provided in such programs is hotly contested, especially in the United States and Great Britain. Possible topics include reproductive anatomy, human sexual behavior, information on sexually transmitted diseases (STDs), social aspects of sexual interaction, negotiating skills intended to help teens follow through with a decision to remain abstinent or to use birth control during sex, and information on birth control methods.
One type of sex education program used mainly in the United States is called abstinence-only education, and it promotes sexual abstinence until marriage. The program does not provide information on birth control, or it heavily emphasizes information such as failure rates and strategies for avoiding intimate situations. Advocates of abstinence-only education believe that the programs will result in decreased rates of teenage pregnancy and STD infection. In an [Internet survey of 1,400 women who found and completed a 10-minute multiple-choice online questionnaire listed in one of several popular search engines, women who received sex education from schools providing primarily abstinence information, or contraception and abstinence information equally, reported fewer unplanned pregnancies than those who received primarily contraceptive information, who in turn reported fewer unplanned pregnancies than those who received no information.[40] However, randomized controlled trials demonstrate that abstinence-only sex education programs increase the rates of pregnancy and STDs in the teenage population.[41][42] Professional medical organizations, including the AMA, AAP, ACOG, APHA, and Society for Adolescent Medicine, support comprehensive sex education (providing abstinence and contraceptive information) and oppose the sole use of abstinence-only sex education.[43][44]
Related Chapters
[edit | edit source]- Population control
- One-child policy
- Reproductive Health
References
[edit | edit source]- ↑ 1.0 1.1 "Researchers find no sperm in pre-ejaculate fluid". Contraceptive Technology Update. 14 (10): 154–156. October 1993. PMID 12286905.
- ↑ 2.0 2.1 Zukerman, Z. (April 2003). "Short Communication: Does Preejaculatory Penile Secretion Originating from Cowper's Gland Contain Sperm?". Journal of Assisted Reproduction and Genetics. 20 (4): 157–159. PMID 12762415. Unknown parameter
|coauthors=ignored (help) - ↑ "Ancient Egyptian Midwifery and Childbirth". Minnesota State University. Retrieved 2007-09-01.
- ↑ Tatman, John. Silphium: Ancient Wonder Drug? Accessed December 21, 2005
- ↑ 5.0 5.1 Riddle, John M. (1999). Eve's Herbs: A History of Contraception and Abortion in the West. Harvard MA: Harvard University Press. ISBN 0-674-27026-6.
- ↑ Vasudeva. "Post-Coital Antifertility Activity of Hibiscus rosa-sinensis Linn. roots". Guru Jambheshwar University of Science and Technology. Retrieved 2007-09-30.
- ↑ Lohiya, N. K. (2002). "Chloroform extract of Carica papaya seeds induces long-term reversible azoospermia in langur monkey". Asian Journal of Andrology. 4: 17–26. Retrieved 2006-11-18. Unknown parameter
|month=ignored (help); Unknown parameter|coauthors=ignored (help) - ↑ see John M. Riddle: "Eve's Herbs: A History of Contraception and Abortion in the West", Princeton: Harvard University Press 1999, ISBN-10: 0674270266,esp. Chapter 6: "The Broken Chain of Knowledge"
- ↑ see Gunnar Heinsohn/Otto Steiger: "Witchcraft, Population Catastrophe and Economic Crisis in Renaissance Europe: An Alternative Macroeconomic Explanation.", University of Bremen 2004Template:PDFlink; John M. Riddle: "The Great Witch-Hunt and the Suppression of Birth Control: Heinsohn and Steiger's Theory from the Perspective of an Historian", Appendix to: Gunnar Heinsohn/Otto Steiger: "Witchcraft, Population Catastrophe and Economic Crisis in Renaissance Europe: An Alternative Macroeconomic Explanation.", University of Bremen 2004Template:PDFlink; also see John M. Riddle: "Eve's Herbs: A History of Contraception and Abortion in the West", Princeton: Harvard University Press 1999, ISBN-10: 0674270266, Chapters 5-7
- ↑ "A History of Birth Control Methods". Planned Parenthood. June 2002. Retrieved 2006-09-02., which cites:
Thomas, Patricia. (1988). Contraceptives, Medical World News, 29(5) (14 March), 48 - ↑ "Evolution and Revolution: The Past, Present, and Future of Contraception". Contraception Online (Baylor College of Medicine). 10 (6). 2000. Unknown parameter
|month=ignored (help) - ↑ Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC) (2013). "U.S. Selected Practice Recommendations for Contraceptive Use, 2013: adapted from the World Health Organization selected practice recommendations for contraceptive use, 2nd edition". MMWR Recomm Rep. 62 (RR-05): 1–60. PMID 23784109.
- ↑ Centers for Disease Control and Prevention (2016). Selected Practice Recommendations for Contraceptive Use
- ↑ Riddle, John M. (1992). Contraception and Abortion from the Ancient World to the Renaissance. Cambridge, MA: Harvard University Press.
- ↑ Weschler, Toni (2002). Taking Charge of Your Fertility (Revised Edition ed.). New York: HarperCollins. pp. p.52. ISBN 0-06-093764-5.
- ↑ Joshi S, Katti U, Godbole S, Bharucha K, B K, Kulkarni S, Risbud A, Mehendale S (2005). "Phase I safety study of Praneem polyherbal vaginal tablet use among HIV-uninfected women in Pune, India". Trans R Soc Trop Med Hyg. 99 (10): 769–74. PMID 16084547.
- ↑ 17.0 17.1 "BufferGel". ReProtect Inc. 2006-10-24. Retrieved 2007-05-19. Check date values in:
|accessdate=, |date=(help) - ↑ "Diaphragms". Cervical Barrier Advancement Society. 2000. Retrieved 2006-10-18.
- ↑ 19.0 19.1 "New Contraceptive Choices". Population Reports, INFO Project, Center for Communication Programs. The Johns Hopkins School of Public Health. M (19). April 2005. Retrieved 2006-07-14. Chapter 2: Vaginal Rings
- ↑ Massai R, Quinteros E, Reyes MV, Caviedes R, Zepeda A, Montero JC, Croxatto HB (2005). "Extended use of a progesterone-releasing vaginal ring in nursing women: a phase II clinical trial". Contraception. 72 (5): 352–7. doi:10.1016/j.contraception.2005.05.004. PMID 16246661.
- ↑ New Contraceptive Choices. Chapter 3: Transdermal contraception
- ↑ Chapter 10: Transcervical sterilization.
- ↑ Robert Finn. "Male Contraceptive Methods Are in the Pipeline". Ob.Gyn. News 42:28, May 1, 2007. Full text Template:PDFlink
- ↑ Kippley, John (1996). The Art of Natural Family Planning (4th addition ed.). Cincinnati, OH: The Couple to Couple League. pp. 108–111, 148. ISBN 0-926412-13-2. Unknown parameter
|coauthors=ignored (help), which cites:- Wade ME, McCarthy P, Braunstein GD; et al. (October 1981). "A randomized prospective study of the use-effectiveness of two methods of natural family planning". American journal of obstetrics and gynecology. 141 (4): 368–376. PMID 7025639.
- Barbato M, Bertolotti G (1988). "Natural methods for fertility control: A prospective study — first part". International Journal of Fertility. 33 Suppl: 48–51. PMID 2902027.
- Roetzer, J (1979). "Sympto-thermal method — Ten years of change". Linacre Quarterly. 45: 358–374. PMID 12309198.
- ↑ Rosenthal, M. Sara (2003). "Urinary Tract Health". The Gynecological Sourcebook. WebMD. Retrieved 2007-06-27.
- ↑ "Sex & the Holy City" (htm). Foreign Correspondent. Retrieved 2006-11-21.
- ↑ 27.0 27.1 27.2 Trussell, James (1998). "Contraceptive Efficacy". In Hatcher, Robert A. et al. (eds.). Contraceptive Technology (17th ed. ed.). New York: Ardent Media. ISBN 0-966-49020-7.
- ↑ FDA (2005). "Depo-Provera U.S. Prescribing Information" (PDF). Retrieved 2007-06-12.
- ↑ Ecochard, R.; Pinguet, F.; Ecochard, I.; De Gouvello, R.; Guy, M.; and Huy, F. (1998) "Analysis of natural family planning failures. In 7007 cycles of use", Fertilite Contraception Sexualite 26(4):291-6
- ↑ Hilgers T.W. and Stanford J.B. (1998) "Creighton Model NaProEducation Technology for avoiding pregnancy. Use effectiveness", Journal of Reproductive Medicine 43(6):495-502
- ↑ Evaluation of the Effectiveness of a Natural Fertility Regulation Programme in China: Shao-Zhen Qian, et al. Reproduction and Contraception (English edition), in press 2000.
- ↑ Howard, M.P. and Stanford, J.B. (1999) "Pregnancy probabilities during use of the Creighton Model Fertility Care System", Archives of Family Medicine 8(5):391-402
- ↑ Skouby, SO. The European Journal of Contraception and Reproductive Health Care (2004) "Contraceptive use and behavior in the 21st century: a comprehensive study across five European countries." 9(2):57-68
- ↑ Do AN, Ciesielski CA, Metler RP, Hammett TA, Li J, Fleming PL (2003). "Occupationally acquired human immunodeficiency virus (HIV) infection: national case surveillance data during 20 years of the HIV epidemic in the United States". Infect Control Hosp Epidemiol. 24 (2): 86–96. PMID 12602690.
- ↑ "Humanae Vitae: Encyclical of Pope Paul VI on the Regulation of Birth, July 25, 1968" (html). The Vatican. Retrieved 2006-10-01.
- ↑ Dennis Rainey (2002). ""The Value of Children" (11 July 2002 FamilyLife Today Radio Broadcast)" (Transcript of radio broadcast). FamilyLife Today. Retrieved 2006-09-30.
- ↑ Feldman, David M. (1998). Birth Control in Jewish Law. Lanham, MD: Jason Aronson. ISBN 0-7657-6058-4.
- ↑ Khalid Farooq Akbar. ""Family Planning and Islam: A Review"". Hamdard Islamicus. XVII (No. 3).
- ↑ ""Hindu Beliefs and Practices Affecting Health Care"" (html). University of Virginia Health System. Retrieved 2006-10-06.
- ↑ Williams MT, Bonner L (2006). "Sex Education Attitudes and Outcomes Among North American Women" (PDF). Adolescence. 41 (161): 1–14. PMID 16689438.
- ↑ DiCenso A, Guyatt G, Willan A, Griffith L (2002). "Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials". BMJ. 324 (7351): 1426. PMID 12065267.
- ↑ "Based on the research, comprehensive sex education is more effective at stopping the spread of HIV infection, says APA committee" (Press release). American Psychological Association. February 23 2005. Retrieved 2006-08-11. Check date values in:
|date=(help) - ↑ Kaplan, David W. (2002). "Prepared Statement. Hearing on Welfare Reform: A Review of Abstinence Education and Transitional Medical Assistance". U.S. House of Representatives Subcommittee on Health. Retrieved 2007-06-22.
- ↑ Santelli J, Ott MA, Lyon M, Rogers J, Summers D (2006). "Abstinence-only education policies and programs: a position paper of the Society for Adolescent Medicine" (PDF). J Adolesc Health. 38 (1): 83–7. PMID 16387257.
bs:Kontrola rađanja ca:Contracepció cs:Antikoncepce da:Prævention de:Empfängnisverhütung ko:피임 is:Getnaðarvörn it:Contraccezione he:פיקוח ילודה lt:Kontracepcija nl:Anticonceptie no:Prevensjon nn:Prevensjon nrm:Contraception simple:Birth control sk:Antikoncepcia sl:Nadzor rojstev sr:Контрацепција sh:Kontrola rađanja fi:Ehkäisy sv:Preventivmedel ta:கருத்தடை th:การคุมกำเนิด
 KSF
KSF