Breast examination
 From Wikidoc - Reading time: 13 min
From Wikidoc - Reading time: 13 min
| Breast examination |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview[edit | edit source]
The breast is made up of milk producing glands that are arranged into units known as lobules. These glands are connected via a series of ducts that ultimately join up to form a common drainage path, terminating at the nipple. The nipple is surrounded by a ring of pigmented tissue known as the areola. Fibro-elastic and fatty tissue provide support for the rest of the structure and allow the breast to maintain its distinctive shape. The breast lies on top of the pectoral muscle, which in turn rests on the thoracic cage. Rough boundaries of the breast are as follows:
- Superior aspect of the breast is bounded by the clavicle
- Inferiorly by the inframamary crease ("bra line")
- Medially by the sternum
- Laterally by the axilla
Each breast contains a network of lymphatic tissue, ~ 90% of which drain into a lymph node group found in the ipsilateral axilla. The remaining 10% drain into the Internal Thoracic nodes, which are located beneath the sternum (not accessible by exam). Lymph drainage pathways are important in the setting of breast cancer, as this is usually the first site of spread (see below). For obvious reasons (i.e., milk production) woman have significantly more breast tissue then men.

(Image courtesy of Charlie Goldberg, M.D.)
Why and when should a breast examination be performed?[edit | edit source]
In the asymptomatic patient:[edit | edit source]
The asymptomatic breast exam is generally performed only on women. This is because diseases of the breast, in particular cancer, occur far more commonly in women then men. Malignancies generally originate in either the glandular tissues that secrete milk or in the ductal structures that transport it to the nipple.
Examination can be done by the clinician (Clinical Breast Exam - CBE) or patient (Self Breast Exam - SBE). Those performed by the clinician are usually done on an annual basis, beginning at the age of 40, which coincides with time of increased risk for development of breast cancer. Other major breast cancer risk factors include: prior history of breast ca, family history in 1st degree relative (particularly if at a young age), increasing patient age and features that result in prolonged/uninterrupted exposure to estrogen (e.g. early age at onset menstruation, never having been pregnant, older age at first pregnancy, older age at menopause). SBE is often recommended on a monthly-to-every-few-months basis.
Interestingly, while both SBE and CBE are part of routine clinical care, there are no studies that demonstrate that either of these techniques, when performed as stand-alone examinations, actually improves clinical outcomes (i.e. detects cancer at an earlier stage, demonstrating positive impact on cancer related morbidity or mortality). In contrast, mammography (performed with or without CBE), has a strong body of evidence to support its routine use as a screening tool for early detection of malignancy.
In the symptomatic patient:[edit | edit source]
The goal of the examination in the setting of symptoms is to better characterize the abnormality, identify underlying etiology, and direct additional evaluation and treatment. Breast related symptoms may include any of the following:
- Discrete masses detected by the patient, often concerning for malignancy
- Pain, which can be associated with a number of processes including: cyclical in a menstruating women (reflecting transient hormone induced changes in the breast tissue), occasionally malignancies.
- Unusual nipple discharge, which may include:
- Blood, concerning for malignancy
- Milk when not pregnant. Suggestive inappropriate Prolactin secretion from the pituitary - may also be induced by certain medications
- Other
- Discoloration or change in the quality of the skin:
- Redness suggests infection or inflammation - in the post partum patient, this is often due to mastitis, a diffuse inflammatory condition caused by congestion from inadequately expressed milk.
- "Peau d'orange" quality - an "Orange Peel" like texture that's caused by an uncommon, aggressive inflammatory malignancy
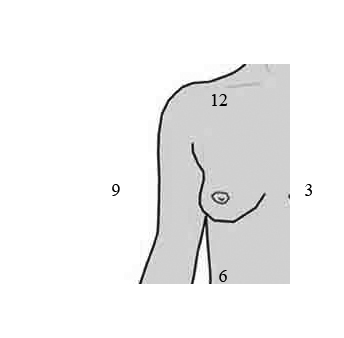
If a mass or other abnormality is identified, it's location can be described as being in one of 4 quadrants (left upper, left lower, right upper, right lower) of the breast. Alternatively, it can be described relative to it's position, imagining a clock face were superimposed on the breast.

(Image courtesy of Charlie Goldberg, M.D.)
(Image courtesy of Charlie Goldberg, M.D.)
It's worth noting that breast symptoms may be caused by diseases elsewhere in the body. For example, as mentioned above, inappropriate milk production may be due to a pituitary tumor secreting Prolactin. Or breast development in men may signify underlying liver disease. Given this, breast symptoms may merit careful history and evaluation of other organ systems. As symptoms can occur in male or female patients (though overall, female >>> male), evaluation is indicated in either sex patient who presents with breast concerns.
Examination in Detail[edit | edit source]
Getting Started[edit | edit source]
- Carefully explain what you are going to do - and why.
- Room should be a comfortable temperature.
- Patient should be in a gown - all undergarments (bras, shirts, etc) should be removed.
- Have the patient remove their arms from the sleeves of the gown - though keep both breasts covered by laying the garment on top of their chest. Alternatively, the patient may put on the gown so that it opens in the front, which may make exposing one breast at a time a bit easier.
- Patient should be lying flat on the table - It may help to have them place hand on side to be examined behind their head, allowing easier access to breast and axilla.
- Uncover only the breast that you are going to examine.
- Observe the breast, looking for evidence of skin or nipple dimpling/retraction, discoloration, obvious masses or asymmetry.
- Observing the breasts while the patient sits up may increase your ability to detect asymmetry or other surface abnormalities, particularly if the person has large breasts.
Palpation of the Breast and Axilla:[edit | edit source]
The goal of this exam is to examine the breast in a systematic fashion, such that all of the tissue is palpated. 3 methods are described below. The accuracy of the exam is increased by allowing adequate time. This will vary with breast size. Specifically, it will take more time to carefully evaluate larger breasts. Regardless of the method used to assure that the breast is examined in its entirety, palpation technique should be as follows:
Palpation Technique in Detail[edit | edit source]
- Use the pads of the middle 3 fingers of one hand.
- Press downward using a circular motion.
- Apply steady pressure, pushing down to the level of the chest wall. Apply enough pressure to palpate to 3 levels of depth: first superficial, then medium, and then deep/to the level of the chest wall.
- Make sure to palpate the nipple and areolar regions.
What precisely are you trying to identify? Normal breasts have a lumpy consistency, created by the mix of lobular, ductal and supporting tissue. The CBE (as mentioned above) is largely performed to identify masses consistent with malignancy. Most lumps are benign (e.g. fibroadenomas, cysts). Masses of concern tend to have the following characteristics: Feel different from the rest of the breast tissue (aka "dominant mass"), firmness, irregular/hard to define borders, fixed/stuck to adjacent tissue - and increase in size over time. As breast density decreases with age (lobular tissue replaced by fat), it is easier to identify masses in older patients.

(Image courtesy of Charlie Goldberg, M.D.)
Three Methods for systematic examination of the breast:[edit | edit source]
Method 1 - Vertical strips:[edit | edit source]
- In this technique, you are breaking the breast into a series of vertical strips, each of which is evaluated sequentially, moving lateral to medial.
- Start at the clavicle, adjacent to the axilla.
- Move your hand down in a vertical line until you've reached the area below the breast. Actual palpation technique is as described above.
- Then move a bit more medially, and examine while traveling up towards the top of the breast.
- When you reach the clavicle, move medially and repeat until you've evaluated the entire breast.
- There is a "tail" of breast tissue that extends from the lateral aspect of the structure towards the axilla. Make sure that you palpate this region as well.
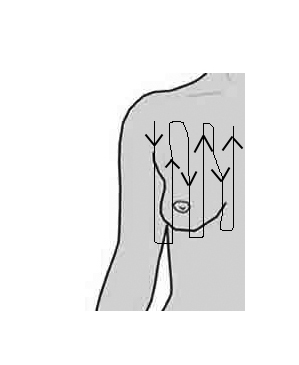
(Image courtesy of Charlie Goldberg, M.D.)
Method 2 - Pie or Radial Spoke Pattern:[edit | edit source]
- Imagine that the breast is broken into a series of pie-type slices, with the nipple at the center.
- Start at the nipple, working outwards toward the periphery of the slice that you're examining. Move your hands a few centimeters along each time.
- When you are clearly no longer over the breast, move to the next slice
- Make sure that you palpate the "tail" of the breast as described above.
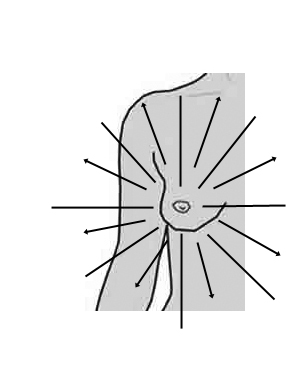
(Image courtesy of Charlie Goldberg, M.D.)
Method 3 - Circular Pattern:[edit | edit source]
- Start at the nipple.
- Work along in circular fashion, moving in a spiral towards the periphery.
- Make sure that you palpate the "tail" of the breast as described in above.

(Image courtesy of Charlie Goldberg, M.D.)
Following direct palpation of the breast, the axillary region should be palpated. This is because the axillary lymph nodes are usually the first site of spread in the setting of breast cancer. While this is of greatest importance when you identify a concerning mass in the breast itself, include the axilla in all of your breast exams. To examine, proceed as follows:
- It may help to have the patient lower their arm so it is next to their side, as when the hand is behind their head, the axillary skin is taught and perhaps more difficult to palpate thru.
- Gently move the arm 20-30 cm away from the patient's body, so that you can gain access to the axillary region.
- Direct the finger tips of the examining hand (it's a bit easier to use your L hand when examining the R breast, and vice versa) toward the top of the axilla.
- Then push the palmar aspect of the hand towards the chest wall. You are trying to identify any abnormal nodules/lumps that could represent axillary adenopathy. In addition, you may be able to trap the nodes between your hand and the chest wall, which can then be better characterized.
- Most women will not have palpable axillary lymph nodes. If you do feel discrete masses, make note of: firmness, quantity and degree of mobility. In general, malignancy is associated with: firmness, increased quantity, adherence to each other and/or the chest wall.
- Recognize that adenopathy may not be due to breast disease. For example, infections of the hand can cause acute, painful axillary adenopathy. Similarly, systemic diseases (e.g. lymphoma, sarcoidosis) may also cause lymph node enlargement. Thus, as with all other aspects of the exam, history and findings in other regions are of great importance.

(Image courtesy of Charlie Goldberg, M.D.)
The other breast is then examined.
Additional aspects of the exam that can be performed:[edit | edit source]
- Assessment of nipple discharge: If the patient reports unusual discharge from the nipple, gently palpate the breast near the nipple, with a goal of trying to express and examine any abnormal fluid. Bloody discharge is particularly concerning for cancer. Most discharge, however, will be secondary to benign conditions.
- Puckering/Dimpling: This can suggest an underlying mass which is distorting the skin above it. In this setting, careful palpation around the dimpling is often revealing. In addition, if it's unclear if there is dimpling or asymmetry, observe the breasts while the patient sits up (with hands placed on hips). This may help clarify differences between the 2 sides and accentuate asymmetry.
- Nipple Retraction: This is concerning for a mass growing underneath the nipple. In this case, carefully palpate the tissue around and underneath the nipple.
- Redness/Pain: Suggestive of inflammation and/or infection. Carefully note the extent of redness as well as temperature differences. Assess for any focal swelling or fluctuance that might suggest underlying abscess.

(Image courtesy of Charlie Goldberg, M.D.)

(Image courtesy of Charlie Goldberg, M.D.)
Pitfalls and Problem Areas:[edit | edit source]
- Examining women with large breasts: In this setting, it can be technically challenging to assure that you've done a thorough examination of all the tissue. In order to minimize error there no special "tricks." Instead, rely on basic exam principles, in particular: Take your time - may take 3 or minutes to examine each breast! Be thorough and ordered, covering all areas of the breast sequentially.
- Careful evaluation of masses: There are many anecdotes relating to missed diagnoses of breast cancer. I recognize that all masses do not represent malignancy. In fact, most are benign (e.g. secondary to fibro-cystic changes, cysts, transient changes that vary with time of the menstrual cycle, etc). An array of thoughtful reviews have been written that describe the appropriate evaluation of abnormal findings. Specifically: when to evaluate with ultrasound, when to consider aspiration, when to consider biopsy, when to re-evaluate at a different point in the menstrual cycle (greatest amount of swelling is usually immediately prior to menstruation), when to refer, etc.. The comments which follow are not meant to contradict this information. Nor are they particularly applicable to those with clear expertise in the appropriate evaluation of abnormal exam findings.
- What follows is directed to the more novice examiner:
- If you clearly identify a discrete mass, consider it to be malignant until proven otherwise. In general, determination of final diagnosis requires a biopsy.
- A dominant breast mass that does not have a corresponding abnormality on Mammogram (i.e. "normal mammo") should still be considered malignant until proven otherwise. This is because not all malignancies generate mammographic findings.
- While uncommon, breast cancer can occur in men. Thus, discrete masses should be appropriately evaluated.
- Breast cancer can occur in young women (20s and 30s) Thus worrisome masses in this population should be appropriately evaluated.
- If you have any concerns or uncertainty re any exam finding, seek input from someone with appropriate experience and training.
- Pay very careful attention to any mass that the patient brings to your attention. Women who are good self-examiners can often detect subtle/early changes concerning for malignancy that an examiner may have difficulty identifying.
Pathological Findings[edit | edit source]
-
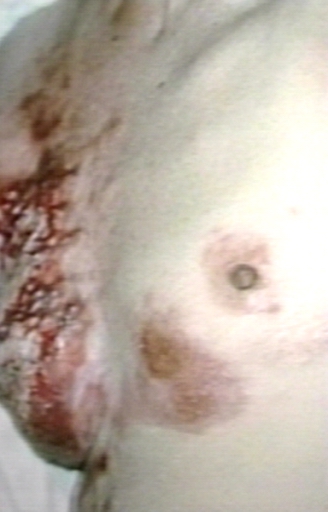
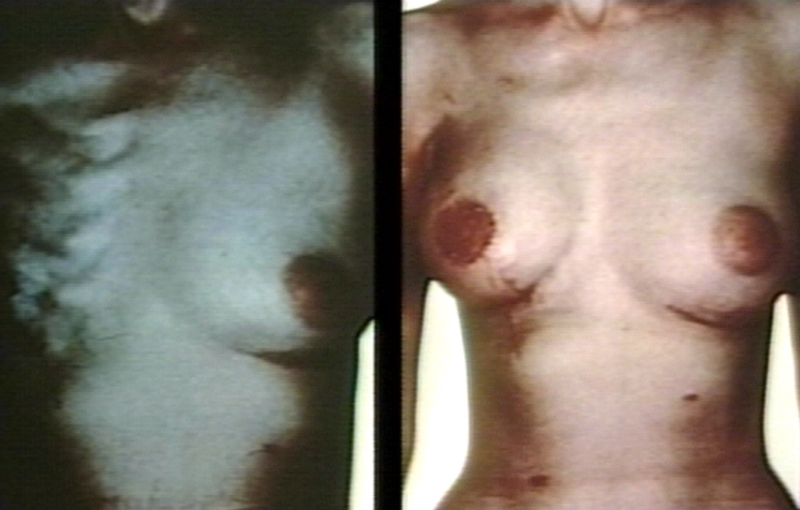
Mastectomy scars with skin metastases
-
Mastectomy scars with skin metastases
-
Gynecomastia; Glandular tissue seen in chronic liver diseases, endocrine diseases or drug side effect
-
Breast carcinoma; a small palpable hard lump
-
Congenital breast hypoplasia; 18 years old patient
-
Juvenile breast hypertrophy; red due to local cellulitis from ulceration (due to bra)
-
Breast: accessory nipple in a 23 years old male
-
Breast carcinoma, 55 y o male; ulceration of skin even though a small tumor (a rare case)
-
Breast; gynecomastia. A 20 year old boy
-
Breast: gynecomastia in 5 yo male; An estrogen secreting adrenal cortical tumor
Breast: Foreign body reaction[edit | edit source]
{{#ev:youtube|mB2I2inv7Ts}}
Breast: Epithelial hyperplasia[edit | edit source]
{{#ev:youtube|0PADE4K1XWc}}
References[edit | edit source]
- Adams K. Lump detection in simulated human breasts. Perception and Psychophysicis 1976; 20: 163-7.
- Baines C, Miller A, Bassett A. Physical examination. Its role as a single screening modality in the Canadian national breast screening study. Cancer 1989; 63: 1816-22.
- Baines CJ, Miller AB. Mammography versus clinical examination of the breasts. J Natl Cancer Institute Monographs 1997; 22: 125-9.
- Baines CJ. Physical examination of the breasts in screening for breast cancer. J Gerontol 1992; 47: 63-7.
- Barnes C. Breast palpation technique: what is the finer pad? J Chronic Disease 1987; 40: 361-2.
- Barton M, Harris R, Fletcher S. Does this patient have berast cnacer?: The screening clinical berast examination: Should it be done? How? JAMA 1999; 282: 1270-80.
- Bickley LS. Bates' Guide to Physical Exam and History Taking. 9th edition, Philadelphia; Lippincott 2007: 337-357 .
- Bloom HS, Criswell E, Pennypacker H. Major stimulus dimensions determining detection of simulated breast lesions. Perception and Psychophysiology 1982; 32: 251-60.
- Campbell HS, Fletcher SW, Pilgrim CA, Morgan TM, Lin S. Improving physicians and nurses clinical breast examination: A randomized controlled trial. Am J Prev Med 1991; 7: 1-8.
- Donegan W. Evaluation of a palpable breast mass. NEJM 1992; 327: 937-42.
- Fletcher S, O'Malley M, Earp J, Morgan T, Lin S, Dengan D. How best to teach women breast self-examination: A randomized controlled trial. Ann Int Med 1990; 112: 772-9.
- Gulay H, Bora S. Management of nipple discharge. J Am Coll Surg 1994; 178: 471-4.
- Hall D, Goldstein M, Stein G. Progress in manual breast examination. Cancer 1977; 40: 364-70.
- Hall D, Adams C, Stein G, Stephenson H, Goldstein M. Improved detection of human breast lesions following experimental training. Cancer 1980; 46: 408-14.
- Kerlikowske K, Simth-Bindman R, Ljung B, Grady D. Evaluation of abnormal mammography results and palpable breast abnormalities. Ann Intern Med 2003; 139: 274-84
- Love S, Gelman R, Silen W. Sounding board. Fibrocystic "disease of the breast - a non disease? NEJM 1982; 307: 1010-4.
- Mahoney L, Csima A. Efficiency of palpation in clinical detection of breast cancer. Can Med Assoc J 1982; 127: 729-30.
- McDermott M, Dolan N, Huang J, Reifler D, Rademaker A. Lump detection is enhanced in silicone breast models stimulating postmenopausal breast tissue. J Gen Intern Med 1996; 11: 112-4.
- Mushlin A. Diagnostic tests in breast cancer. Clinical strategies based on diagnostic possibilities. Ann Int Med 1985; 103: 79-85.
- Pilgrim C, Lannon C, Harris R, Cogburn W, Fletcher S. Improving clinical breast examination training in a medical school: A randomized trial. J of Gen Int Med 1993; 8: 685-8.
- Sanders K, Pilgrim C, Pennypacker H. Increased proficiency of search in breast self exam. Cancer 1986; 58: 2531-7.
- Sapira JD. The Art and Science of Bedside Diagnosis. 1st edition, Baltimore; Williams and Wilkins 1990: 239-43 .
- Screening for breast cancer; Summary of recomendations. U.S. Preventative Services Task Force (USPSTF). 2002. http://www.ahrq.gov/clinic/uspstf/uspsbrca.htm
- Stephenson HS, Adams CK, Hall DC, Pennypacker HS. Effects of certain training parameters on detection of simulated breast cancer. Journal of Behavioral Medicine 1979; 2: 239-50.
- Winchester D. Physical examination of the breast. Cancer 1992; 69: 1947-9.
See Also[edit | edit source]
- Breast
- Areola
- Breast self-examination
- Mammography
- Intimate examination
- Breast cancer
- Chronic cystic mastitis
- Mastitis
- Mastalgia
- Galactorrhea
- Breast engorgement
- Breast shell
- Inflammatory breast cancer
- Jogger's nipple
- Paget's disease
Template:Skin and subcutaneous tissue symptoms and signs Template:Nervous and musculoskeletal system symptoms and signs Template:Urinary system symptoms and signs Template:Cognition, perception, emotional state and behaviour symptoms and signs Template:Speech and voice symptoms and signs Template:General symptoms and signs
 KSF
KSF