Cervical intraepithelial neoplasia
 From Wikidoc - Reading time: 10 min
From Wikidoc - Reading time: 10 min
For patient information, please click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] Associate Editor(s)-in-Chief: Maria Fernanda Villarreal, M.D. [2]
Synonyms and keywords: CIN; Cervical interstitial neoplasia; Cervical dysplasia; Cervical interstitial neoplasia
Overview[edit | edit source]
Cervical intraepithelial neoplasia (also known as cervical dysplasia and CIN), is the potentially premalignant transformation and abnormal growth (dysplasia) of squamous cells on the surface of the cervix. Cervical intraepithelial neoplasia was first discovered by Dr. Georgios Nikolaou Papanikolaou, a Greek pathologist, in 1927. There are 4 cytological classifications for cervical intraepithelial neoplasia: Bethesda system, Papanicolaou classification, CIN nomenclature, and dysplasia nomenclature. The most common cytological classification systems for cervical intraepithelial neoplasia is the Bethesda and CIN nomenclature. Cervical intraepithelial neoplasia may be classified according to Bethesda system by cytology description into 3 subtypes: atypical squamous cells, low grade squamous intraepithelial lesion (LGSIL or LSIL), and high grade squamous intraepithelial lesion (HGSIL or HSIL). The pathogenesis of cervical intraepithelial neoplasia is characterized by the premalignant transformation and abnormal growth of squamous cells on the surface of the cervix. The presence of human papillomavirus (HPV) has a crucial role in the pathogenesis of cervical intraepithelial neoplasia. The infection of human papillomavirus (HPV) leads to the first precursor lesion of cervical intraepithelial neoplasia, also known as the koilocyte, which is a squamous epithelial cell that has undergone a number of structural changes. Surgery is the mainstay of therapy for cervical intraepithelial neoplasia. According to the American Society for Colposcopy and Cervical Pathology guidelines, indications for ablative surgery among patients with cervical intraepithelial neoplasia should include: persistent low-grade cervical intraepithelial neoplasia, cervical intraepithelial neoplasia grade II and grade III. Common surgical procedures for cervical intraepithelial neoplasia, include cryocautery, electrocautery, laser cautery, and cervical conization.
Historical Perspective[edit | edit source]
- Cervical intraepithelial neoplasia was first discovered by Dr. Georgios Nikolaou Papanikolaou, a Greek pathologist, in 1927.[1]
- In 1928, the first screening was developed by Aurel Babeș, a Romanian pathologist to diagnose cervical intraepithelial neoplasia.[1]
- In 1980, human papillomavirus (HPV) was first identified in the pathogenesis of cervical intraepithelial neoplasia.[2]
- In 1988, the Bethesda system classification method was introduced to categorize histopathological findings of cervical intraepithelial neoplasia according to degrees of severity.
Classification[edit | edit source]
- Cervical intraepithelial neoplasia has 4 cytological classifications: Bethesda system, Papanicolaou classification, CIN nomenclature, and dysplasia nomenclature.
- The most common classification systems for cervical intraepithelial neoplasia is the Bethesda and CIN nomenclature.
- Cervical intraepithelial neoplasia may be classified according to Bethesda system by cytology description into 3 subtypes:
- Atypical squamous cells
- Undetermined significance (ASC-US)
- Low grade squamous intraepithelial lesion (LGSIL or LSIL)
- High grade squamous intraepithelial lesion (HGSIL or HSIL)
- Cervical intraepithelial neoplasia may be classified according to CIN nomenclature by histological severity into 3 subtypes:
- Cervical intraepithelial neoplasia I (CIN I)
- Cervical intraepithelial neoplasia II (CIN II)
- Cervical intraepithelial neoplasia III (CIN III)
- Cervical intraepithelial neoplasia may be classified according to Papanicolau by cytology description into 5 subtypes:
- Class I: absence of atypical or abnormal cells
- Class II: atypical cytology, but no evidence of malignancy
- Class III: cytology suggestive of, but not conclusive for, malignancy
- Class IV: cytology strongly suggestive of malignancy
- Class V: cytology conclusive for malignancy
- Cervical intraepithelial neoplasia may be classified according to dysplasia nomenclature by cytology description into 5 subtypes:
- Other variants of cervical intraepithelial neoplasia include carcinoma in situ, typical glandular cells not otherwise specified, and invasive carcinoma.
Pathophysiology[edit | edit source]
- The pathogenesis of cervical intraepithelial neoplasia is characterized by the premalignant transformation and abnormal growth of squamous cells on the surface of the cervix.[3]
- Cervical intraepithelial neoplasia arises from cells localized in the ectoendocervical squamocolumnar junction (also known as the "transformation zone") of the cervix persistently infected with the human papillomavirus (HPV).
- The presence of human papillomavirus (HPV) subtypes 16 and 18 plays an essential role in the pathogenesis of cervical cancer and the pathogenesis of cervical intraepithelial neoplasia.[4][5]
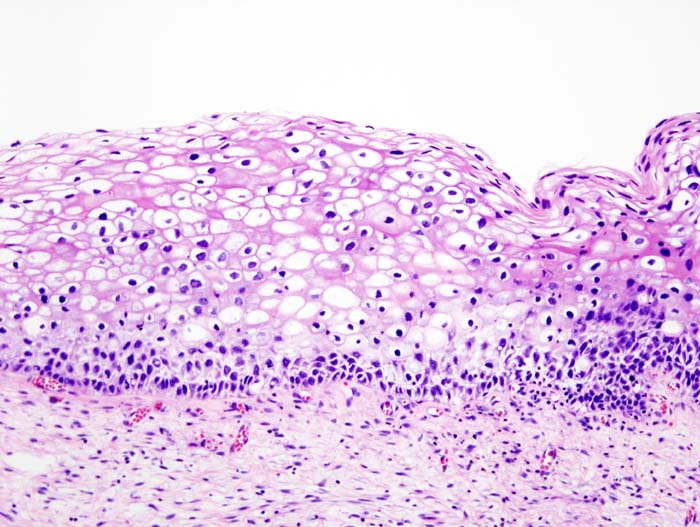
- The first precursor lesion of cervical intraepithelial neoplasia is the koilocyte, which is a squamous epithelial cell that has undergone a number of structural changes (these usually occur as a result of infection by human papillomavirus).[6]
- On gross pathology, there are no characteristic findings of cervical intraepithelial neoplasia.
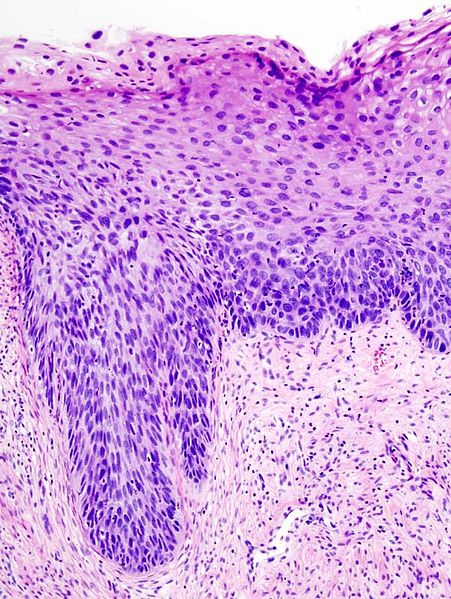
- On microscopic histopathological analysis, findings of cervical intraepithelial neoplasia depends on the lesion grade.
- The table below summarizes the histopathological findings of cervical intraepithelial neoplasia according to the lesion grade.
| Cytologic findings Lesion grade |
Histologic changes Bethesda system |
Description | Microscopic findings |
|---|---|---|---|
| CIN I
Cervical intraepithelial neoplasia I |
|
|
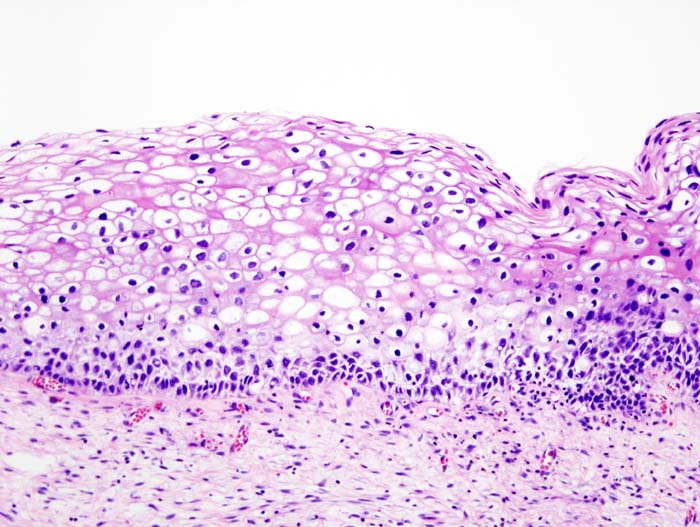 |
| CIN II
Cervical intraepithelial neoplasia II |
|
|
 |
| CIN III
Cervical intraepithelial neoplasia III |
|
|
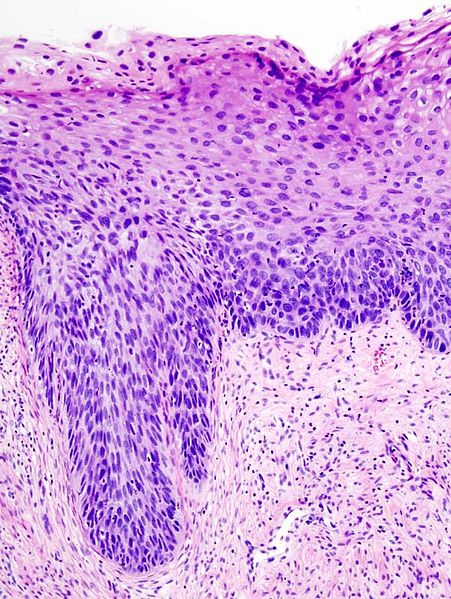 |
Molecular Pathogenesis[edit | edit source]
- The progression of cervical intraepithelial neoplasia usually involves the viral replication of the human papillomavirus (HPV) following the mutation of proteins E6/E7, resulting in the overexpression of these oncoproteins.
- The overexpression of these oncoproteins generates a deficient cell replication and excessive cell growth.
- The E6/E7 proteins inactivate two tumor suppressor proteins, p53 (inactivated by E6) and pRb (inactivated by E7).
- The viral oncogenes E6 and E7 modify the cell cycle so as to retain the differentiating host keratinocyte in a state that is favorable to the amplification of viral genome replication and consequent late gene expression.
- E6 in association with host E6-associated protein, which has ubiquitin ligase activity, acts to ubiquitinate p53, leading to its proteosomal degradation.
- E7 (in oncogenic HPVs) acts as the primary transforming protein.
- E7 competes for retinoblastoma protein (pRb) binding, freeing the transcription factor E2F to transactivate its targets, thus pushing the cell cycle forward.
Causes[edit | edit source]
- The most important cause of cervical intraepithelial neoplasia is human papillomavirus (HPV)
- Low-risk type or non-oncogenic, include:
- Subtypes 16,18, 31, 33, 35, 39, 45, 51, 52, 56, 58, 59, 68, 69, 82
- High-risk type or oncogenic, include:
- Subtypes 6, 11, 40, 42, 43, 44, 54, 61, 72, 81
Differentiating Cervical Intraepithelial Neoplasia from Other Diseases[edit | edit source]
- Cervical intraepithelial neoplasia must be differentiated from other diseases that cause abnormal vaginal bleeding, dyspareunia, and abnormal vaginal discharge, such as:
Epidemiology and Demographics[edit | edit source]
Prevalence[edit | edit source]
- The prevalence of cervical intraepithelial neoplasia I (CIN I) is approximately 54 cases per 100,000 individuals in the United States.[7]
- The prevalence of cervical intraepithelial neoplasia II (CIN II) is approximately 255 cases per 100,000 individuals in the United States.[7]
- The prevalence of cervical intraepithelial neoplasia III (CIN III) is approximately 141 cases per 100,000 individuals in the United States.[7]
- The prevalence of invasive carcinoma is approximately 24 cases per 100,000 individuals in the United States.[7]
Incidence[edit | edit source]
- The incidence of cervical intraepithelial neoplasia I (CIN I) is 160 cases per 100,000 individuals per year in the United States.[8]
- The incidence of cervical intraepithelial neoplasia II (CIN II) is 120 cases per 100,000 individuals per year in the United States.[8]
Age[edit | edit source]
- The median age at diagnosis for cervical intraepithelial neoplasia is 30 years.
- Cervical intraepithelial neoplasia is more commonly seen in women between 20 to 40 years years old.
Race[edit | edit source]
- Hispanic individuals are more likely to develop cervical intraepithelial neoplasia.
- African American individuals are more likely to develop cervical intraepithelial neoplasia.
Risk Factors[edit | edit source]
- The most important risk factor in the development of cervical intraepithelial neoplasia is immunosuppression.
- Common risk factors in the development of cervical intraepithelial neoplasia, include:[9]
-
- Chronic inflammation of the cervix
- Use of oral contraceptives
- Increased sexual activity
- Poor socioeconomical status
- Poor diet[10]
Natural History, Complications and Prognosis[edit | edit source]
- The majority of patients with cervical intraepithelial neoplasia remain asymptomatic for years.
- Early clinical features include abnormal vaginal discharge, dyspareunia, and abnormal vaginal bleeding.
- If left untreated, 70% patients with cervical intraepithelial neoplasia will regress within one year.
- 90% of patients with low-grade cervical intraepithelial neoplasia will regress within two years of treatment.
- 50% of patients with high-grade cervical intraepithelial neoplasia will regress within 2 years without treatment.
- Progression to cervical carcinoma in situ (CIS)
- 11% of patients low-grade cervical intraepithelial neoplasia will develop CIS.
- 22% of patients high-grade grade cervical intraepithelial neoplasia will develop CIS.
- Progression to invasive cancer (cervical cancer)
- 1% of patients with low-grade cervical intraepithelial neoplasia will develop cervical cancer.
- 5% - 13% of patients with high-grade grade cervical intraepithelial neoplasia will develop cervical cancer.
- Common complications of cervical intraepithelial neoplasia include infertility, maternal-fetal transmission of human papillomavirus, and recurrent human papillomavirus infection.
- Prognosis is generally good if detected early, and the 5-year survival rate of patients with high-grade cervical intraepithelial neoplasia is approximately 98%.
Diagnosis[edit | edit source]
Diagnostic Criteria[edit | edit source]
- The diagnosis of cervical intraepithelial neoplasia is made with the following histopathological findings:
| Cytologic findings Lesion grade |
Histologic changes Bethesda system |
Description | Microscopic findings |
|---|---|---|---|
| CIN I
Cervical intraepithelial neoplasia I |
|
|
 |
| CIN II
Cervical intraepithelial neoplasia II |
|
|
 |
| CIN III
Cervical intraepithelial neoplasia III |
|
|
 |
Symptoms[edit | edit source]
- Cervical intraepithelial neoplasia is usually asymptomatic.
- Symptoms of cervical intraepithelial neoplasia may include the following:
Physical Examination[edit | edit source]
- Patients with cervical intraepithelial neoplasia are usually well-appearing.
- Digital examination findings of the vagina and cervix, may reveal:
- Cervical nodularity or hardness of the tissue
Laboratory Findings[edit | edit source]
- Laboratory findings associated with cervical intraepithelial neoplasia, include:
Imaging Findings[edit | edit source]
- There are no imaging findings associated with cervical intraepithelial neoplasia.
Other Diagnostic Studies[edit | edit source]
- The most important diagnostic study for cervical intraepithelial neoplasia is colposcopy.
- The most common finding of cervical intraepithelial neoplasia in colposcopy is acetowhite lesions with atypical vessels.
- Other findings on vaginal colposcopy, include:
- Greyish-white or yellowish-white lesions
- Irregular longitudinal vessels
- Corkscrew or tree appearance
- Cervical nodularity
- The table below summarizes the colposcopy findings according to the Swede score
| Swede score for interpreting colposcopy findings
Adapted from Principles and Practice of Colposcopy | |||
|---|---|---|---|
| 0 | 1 | 2 | |
| Uptake of acetic acid | 0 or transparent |
|
|
| Margins and surface | 0 or diffuse |
|
|
| Vessels | Fine, regular |
|
|
| Lesion size | < 5mm |
|
|
| Iodine staining | Brown |
|
|
|
The total Swede Score ranges between 0 and 10. A score of more than 5 is reported to identify all high grade lesions (HGL), and ≥8 to have a specificity of 90% for HGL. A score less than <5 is suggested to not require biopsy because of low risk of cancer, a score between 5-7 to require biopsy A score ≥8 again not to require biopsy because it is likely more efficient to intervene (e.g. excision directly) | |||
Video[edit | edit source]
{{#ev:youtube|ekDCA7egnCM}}
Treatment[edit | edit source]
Medical Therapy[edit | edit source]
- Medical treatment for cervical intraepithelial neoplasia, include:
- Observation
- Observation is indicated for cervical intraepithelial neoplasia lesions that are:
- Highly likely to regress
- High grade lesions associated with a high risk of developing cervical cancer
- The management of cervical intraepithelial neoplasia will depend on patients age:
- Patients with cervical intraepithelial neoplasia between 21-24 years
- Patients with cervical intraepithelial neoplasia above 25 years
Surgery[edit | edit source]
- Surgery is the mainstay of therapy for cervical intraepithelial neoplasia.[11]
- According to the American Society for Colposcopy and Cervical Pathology guidelines, indications for ablative surgery among patients with cervical intraepithelial neoplasia should include:
- Persistent low-grade cervical intraepithelial neoplasia
- Cervical intraepithelial neoplasia grade II and grade III
- Common surgical procedures for cervical intraepithelial neoplasia, include:
-
- Cold knife conization
- Loop electrical excision
- The surgical procedure used depends on the histopathological lesion grade.
- Cervical conization can only be performed for patients suspected to have invasive cancer.
- Common cervical conization complications, include:
Prevention[edit | edit source]
- The most effective measure for the primary prevention of cervical intraepithelial neoplasia is the vaccination against oncogenic human papillomavirus (HPV) infection.
- The most effective measure for the secondary prevention of cervical intraepithelial neoplasia is periodic cervical screening
- Once diagnosed and successfully treated, patients with cervical intraepithelial neoplasia are followed-up every 3, 6 or 12 months depending on the lesion grade.
- Follow-up testing include periodic screening tests, such as: Papanicolaou test and colposcopy examinations.
References[edit | edit source]
- ↑ 1.0 1.1 Georgios Nikolaou Papanikolaou Wikipedia. https://en.wikipedia.org/wiki/Georgios_Papanikolaou Accessed on March 29, 2016
- ↑ Herfs M, Crum CP (2013). "Laboratory management of cervical intraepithelial neoplasia: proposing a new paradigm". Adv Anat Pathol. 20 (2): 86–94. doi:10.1097/PAP.0b013e3182862aab. PMID 23399794.
- ↑ Arends MJ, Buckley CH, Wells M (1998). "Aetiology, pathogenesis, and pathology of cervical neoplasia". J. Clin. Pathol. 51 (2): 96–103. PMC 500501. PMID 9602680.
- ↑ Braaten KP, Laufer MR (2008). "Human Papillomavirus (HPV), HPV-Related Disease, and the HPV Vaccine". Rev Obstet Gynecol. 1 (1): 2–10. PMC 2492590. PMID 18701931.
- ↑ Skinner SR, Wheeler CM, Romanowski B, Castellsagué X, Lazcano-Ponce E, Del Rosario-Raymundo MR, Vallejos C, Minkina G, Pereira Da Silva D, McNeil S, Prilepskaya V, Gogotadze I, Money D, Garland SM, Romanenko V, Harper DM, Levin MJ, Chatterjee A, Geeraerts B, Struyf F, Dubin G, Bozonnat MC, Rosillon D, Baril L (May 2016). "Progression of HPV infection to detectable cervical lesions or clearance in adult women: Analysis of the control arm of the VIVIANE study". Int. J. Cancer. 138 (10): 2428–38. doi:10.1002/ijc.29971. PMC 4787275. PMID 26685704.
- ↑ Krawczyk E, Suprynowicz FA, Liu X, Dai Y, Hartmann DP, Hanover J, Schlegel R (September 2008). "Koilocytosis: a cooperative interaction between the human papillomavirus E5 and E6 oncoproteins". Am. J. Pathol. 173 (3): 682–8. doi:10.2353/ajpath.2008.080280. PMC 2527066. PMID 18688031.
- ↑ 7.0 7.1 7.2 7.3 Dunne EF, Unger ER, Sternberg M, McQuillan G, Swan DC, Patel SS, Markowitz LE (2007). "Prevalence of HPV infection among females in the United States". JAMA. 297 (8): 813–9. doi:10.1001/jama.297.8.813. PMID 17327523.
- ↑ 8.0 8.1 Henk HJ, Insinga RP, Singhal PK, Darkow T (2010). "Incidence and costs of cervical intraepithelial neoplasia in a US commercially insured population". J Low Genit Tract Dis. 14 (1): 29–36. doi:10.1097/LGT.0b013e3181ac05e9. PMID 20040833.
- ↑ Brisson J, Morin C, Fortier M, Roy M, Bouchard C, Leclerc J, Christen A, Guimont C, Penault F, Meisels A (1994). "Risk factors for cervical intraepithelial neoplasia: differences between low- and high-grade lesions". Am. J. Epidemiol. 140 (8): 700–10. PMID 7942772.
- ↑ García-Closas R, Castellsagué X, Bosch X, González CA (2005). "The role of diet and nutrition in cervical carcinogenesis: a review of recent evidence". Int. J. Cancer. 117 (4): 629–37. doi:10.1002/ijc.21193. PMID 15912536.
- ↑ Martin-Hirsch PL, Paraskevaidis E, Kitchener H (2000). "Surgery for cervical intraepithelial neoplasia". Cochrane Database Syst Rev (2): CD001318. doi:10.1002/14651858.CD001318. PMID 10796771.
 KSF
KSF