Constipation (patient information)
 From Wikidoc - Reading time: 13 min
From Wikidoc - Reading time: 13 min
|
Constipation |
|
Constipation On the Web |
|---|
For the WikiDoc page for this topic, click here
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Assistant Editor-in-Chief: Meagan E. Doherty
Overview[edit | edit source]
Constipation is defined as having a bowel movement fewer than three times per week. With constipation stools are usually hard, dry, small in size, and difficult to eliminate. Some people who are constipated find it painful to have a bowel movement and often experience straining, bloating, and the sensation of a full bowel.
Some people think they are constipated if they do not have a bowel movement every day. However, normal stool elimination may be three times a day or three times a week, depending on the person.
Constipation is a symptom, not a disease. Almost everyone experiences constipation at some point in their life, and a poor diet typically is the cause. Most constipation is temporary and not serious. Understanding its causes, prevention, and treatment will help most people find relief.
-
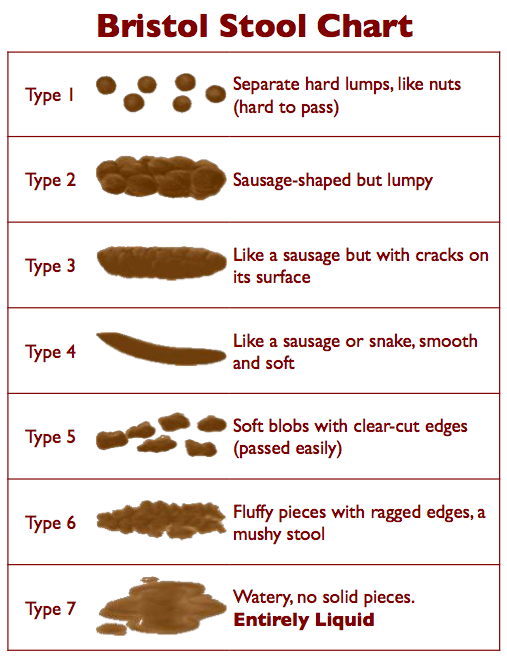
Types 1 and 2 on the Bristol Stool Chart indicate constipation
What are the symptoms of Constipation?[edit | edit source]
When the stool is hard, infrequent, and requires significant effort to pass, you have constipation. The passage of large, wide stools may tear the mucosal membrane of the anus, especially in children. This can cause bleeding and the possibility of an anal fissure.
What are the causes of Constipation?[edit | edit source]
To understand constipation, it helps to know how the colon, or large intestine, works. As food moves through the colon, the colon absorbs water from the food while it forms waste products, or stool. Muscle contractions in the colon then push the stool toward the rectum. By the time stool reaches the rectum it is solid, because most of the water has been absorbed.
Constipation occurs when the colon absorbs too much water or if the colon’s muscle contractions are slow or sluggish, causing the stool to move through the colon too slowly. As a result, stools can become hard and dry. Common causes of constipation are
- not enough fiber in the diet
- lack of physical activity
- medications
- milk
- irritable bowel syndrome
- changes in life or routine such as pregnancy, aging, and travel
- abuse of laxatives
- ignoring the urge to have a bowel movement
- dehydration
- specific diseases or conditions, such as stroke (most common)
- problems with the colon and rectum
- problems with intestinal function (chronic idiopathic constipation)
Not Enough Fiber in the Diet[edit | edit source]
People who eat a high-fiber diet are less likely to become constipated. The most common causes of constipation are a diet low in fiber or a diet high in fats, such as cheese, eggs, and meats.
Fiber—both soluble and insoluble—is the part of fruits, vegetables, and grains that the body cannot digest. Soluble fiber dissolves easily in water and takes on a soft, gel-like texture in the intestines. Insoluble fiber passes through the intestines almost unchanged. The bulk and soft texture of fiber help prevent hard, dry stools that are difficult to pass.
Americans eat an average of 5 to 14 grams of fiber daily,* which is short of the 20 to 35 grams recommended by the American Dietetic Association. Both children and adults often eat too many refined and processed foods from which the natural fiber has been removed.
A low-fiber diet also plays a key role in constipation among older adults, who may lose interest in eating and choose foods that are quick to make or buy, such as fast foods, or prepared foods, both of which are usually low in fiber. Also, difficulties with chewing or swallowing may cause older people to eat soft foods that are processed and low in fiber.
- National Center for Health Statistics. Dietary Intake of Macronutrients, Micronutrients, and Other Dietary Constituents: United States, 1988–94. Vital and Health Statistics, Series 11, Number 245. July 2002.
Not Enough Liquids[edit | edit source]
Research shows that although increased fluid intake does not necessarily help relieve constipation, many people report some relief from their constipation if they drink fluids such as water and juice and avoid dehydration. Liquids add fluid to the colon and bulk to stools, making bowel movements softer and easier to pass. People who have problems with constipation should try to drink liquids every day. However, liquids that contain caffeine, such as coffee and cola drinks will worsen one’s symptoms by causing dehydration. Alcohol is another beverage that causes dehydration. It is important to drink fluids that hydrate the body, especially when consuming caffeine containing drinks or alcoholic beverages.
Lack of Physical Activity[edit | edit source]
A lack of physical activity can lead to constipation, although doctors do not know precisely why. For example, constipation often occurs after an accident or during an illness when one must stay in bed and cannot exercise. Lack of physical activity is thought to be one of the reasons constipation is common in older people.
Medications[edit | edit source]
Some medications can cause constipation, including
- pain medications (especially narcotics)
- antacids that contain aluminum and calcium
- blood pressure medications (calcium channel blockers)
- antiparkinson drugs
- antispasmodics
- antidepressants
- iron supplements
- diuretics
- anticonvulsants
Changes in Life or Routine[edit | edit source]
During pregnancy, women may be constipated because of hormonal changes or because the uterus compresses the intestine. Aging may also affect bowel regularity, because a slower metabolism results in less intestinal activity and muscle tone. In addition, people often become constipated when traveling, because their normal diet and daily routine are disrupted.
Abuse of Laxatives[edit | edit source]
The common belief that people must have a daily bowel movement has led to self-medicating with OTC laxative products. Although people may feel relief when they use laxatives, typically they must increase the dose over time because the body grows reliant on laxatives in order to have a bowel movement. As a result, laxatives may become habit-forming. Ignoring the Urge to Have a Bowel Movement
People who ignore the urge to have a bowel movement may eventually stop feeling the need to have one, which can lead to constipation. Some people delay having a bowel movement because they do not want to use toilets outside the home. Others ignore the urge because of emotional stress or because they are too busy. Children may postpone having a bowel movement because of stressful toilet training or because they do not want to interrupt their play.
Specific Diseases[edit | edit source]
Diseases that cause constipation include neurological disorders, metabolic and endocrine disorders, and systemic conditions that affect organ systems. These disorders can slow the movement of stool through the colon, rectum, or anus.
Conditions that can cause constipation are found below.
- Neurological disorders
- multiple sclerosis
- Parkinson's disease
- chronic idiopathic intestinal pseudo-obstruction
- stroke
- spinal cord injuries
- Metabolic and endocrine conditions
- diabetes
- uremia
- hypercalcemia
- poor glycemic control
- hypothyroidism
- Systemic disorders
- amyloidosis
- lupus
- scleroderma
Problems with the Colon and Rectum[edit | edit source]
Intestinal obstruction, scar tissue—also called adhesions—diverticulosis, tumors, colorectal stricture, Hirschsprung disease, or cancer can compress, squeeze, or narrow the intestine and rectum and cause constipation.
Problems with Intestinal Function[edit | edit source]
The two types of constipation are idiopathic constipation and functional constipation. Irritable bowel syndrome (IBS) with predominant symptoms of constipation is categorized separately.
Idiopathic—of unknown origin—constipation does not respond to standard treatment.
Functional constipation means that the bowel is healthy but not working properly. Functional constipation is often the result of poor dietary habits and lifestyle. It occurs in both children and adults and is most common in women. Colonic inertia, delayed transit, and pelvic floor dysfunction are three types of functional constipation. Colonic inertia and delayed transit are caused by a decrease in muscle activity in the colon. These syndromes may affect the entire colon or may be confined to the lower, or sigmoid, colon.
Pelvic floor dysfunction is caused by a weakness of the muscles in the pelvis surrounding the anus and rectum. However, because this group of muscles is voluntarily controlled to some extent, biofeedback training is somewhat successful in retraining the muscles to function normally and improving the ability to have a bowel movement.
Functional constipation that stems from problems in the structure of the anus and rectum is known as anorectal dysfunction, or anismus. These abnormalities result in an inability to relax the rectal and anal muscles that allow stool to exit.
People with IBS having predominantly constipation also have pain and bloating as part of their symptoms.
Who is at risk for Constipation?[edit | edit source]
Constipation is one of the most common gastrointestinal complaints in the United States. More than 4 million Americans have frequent constipation, accounting for 2.5 million physician visits a year. Those reporting constipation most often are women and adults ages 65 and older. Pregnant women may have constipation, and it is a common problem following childbirth or surgery.
How to know you have Constipation (Diagnosis)?[edit | edit source]
The tests the doctor performs depend on the duration and severity of the constipation, the person’s age, and whether blood in stools, recent changes in bowel habits, or weight loss have occurred. Most people with constipation do not need extensive testing and can be treated with changes in diet and exercise. For example, in young people with mild symptoms, a medical history and physical exam may be all that is needed for diagnosis and treatment. Medical History
The doctor may ask a patient to describe his or her constipation, including duration of symptoms, frequency of bowel movements, consistency of stools, presence of blood in the stool, and toilet habits—how often and where one has bowel movements. A record of eating habits, medication, and level of physical activity will also help the doctor determine the cause of constipation.
The clinical definition of constipation is having any two of the following symptoms for at least 12 weeks—not always consecutive—in the previous 12 months:
- straining during bowel movements
- lumpy or hard stool
- sensation of incomplete evacuation
- sensation of anorectal blockage/obstruction
- fewer than three bowel movements per week
Physical Examination[edit | edit source]
A physical exam may include a rectal exam with a gloved, lubricated finger to evaluate the tone of the muscle that closes off the anus—also called anal sphincter—and to detect tenderness, obstruction, or blood. In some cases, blood and thyroid tests may be necessary to look for thyroid disease and serum calcium or to rule out inflammatory, metabolic, and other disorders.
Extensive testing usually is reserved for people with severe symptoms, for those with sudden changes in the number and consistency of bowel movements or blood in the stool, and older adults. Additional tests that may be used to evaluate constipation include
- a colorectal transit study
- anorectal function tests
- a defecography
Because of an increased risk of colorectal cancer in older adults, the doctor may use tests to rule out a diagnosis of cancer, including a
- barium enema x ray
- sigmoidoscopy or colonoscopy
Colorectal transit study. This test shows how well food moves through the colon. The patient swallows capsules containing small markers that are visible on an x ray. The movement of the markers through the colon is monitored by abdominal x rays taken several times 3 to 7 days after the capsule is swallowed. The patient eats a high-fiber diet during the course of this test.
Anorectal function tests. These tests diagnose constipation caused by abnormal functioning of the anus or rectum—also called anorectal function.
- Anorectal manometry evaluates anal sphincter muscle function. For this test, a catheter or air-filled balloon is inserted into the anus and slowly pulled back through the sphincter muscle to measure muscle tone and contractions.
- Balloon expulsion tests consist of filling a balloon with varying amounts of water after it has been rectally inserted. Then the patient is asked to expel the balloon. The inability to expel a balloon filled with less than 150 mL of water may indicate a decrease in bowel function.
Defecography is an x ray of the anorectal area that evaluates completeness of stool elimination, identifies anorectal abnormalities, and evaluates rectal muscle contractions and relaxation. During the exam, the doctor fills the rectum with a soft paste that is the same consistency as stool. The patient sits on a toilet positioned inside an x-ray machine, then relaxes and squeezes the anus to expel the paste. The doctor studies the x rays for anorectal problems that occurred as the paste was expelled.
Barium enema x ray. This exam involves viewing the rectum, colon, and lower part of the small intestine to locate problems. This part of the digestive tract is known as the bowel. This test may show intestinal obstruction and Hirschsprung disease, which is a lack of nerves within the colon.
The night before the test, bowel cleansing, also called bowel prep, is necessary to clear the lower digestive tract. The patient drinks a special liquid to flush out the bowel. A clean bowel is important, because even a small amount of stool in the colon can hide details and result in an incomplete exam.
Because the colon does not show up well on x rays, the doctor fills it with barium, a chalky liquid that makes the area visible. Once the mixture coats the inside of the colon and rectum, x rays are taken that show their shape and condition. The patient may feel some abdominal cramping when the barium fills the colon but usually feels little discomfort after the procedure. Stools may be white in color for a few days after the exam.
Sigmoidoscopy or colonoscopy. An examination of the rectum and lower, or sigmoid, colon is called a sigmoidoscopy. An examination of the rectum and entire colon is called a colonoscopy.
The person usually has a liquid dinner the night before a colonoscopy or sigmoidoscopy and takes an enema early the next morning. An enema an hour before the test may also be necessary.
To perform a sigmoidoscopy, the doctor uses a long, flexible tube with a light on the end, called a sigmoidoscope, to view the rectum and lower colon. The patient is lightly sedated before the exam. First, the doctor examines the rectum with a gloved, lubricated finger. Then, the sigmoidoscope is inserted through the anus into the rectum and lower colon. The procedure may cause abdominal pressure and a mild sensation of wanting to move the bowels. The doctor may fill the colon with air to get a better view. The air can cause mild cramping.
To perform a colonoscopy, the doctor uses a flexible tube with a light on the end, called a colonoscope, to view the entire colon. This tube is longer than a sigmoidoscope. During the exam, the patient lies on his or her side, and the doctor inserts the tube through the anus and rectum into the colon. If an abnormality is seen, the doctor can use the colonoscope to remove a small piece of tissue for examination (biopsy). The patient may feel gassy and bloated after the procedure.
When to seek urgent medical care?[edit | edit source]
Call your doctor if you have:
- Sudden constipation with abdominal cramps and an inability to pass gas or stool (DO NOT take any laxatives -- call immediately!)
- Sharp or severe abdominal pain, especially if you're also bloated
- Blood in your stool
- Constipation alternating with diarrhea
- Thin, pencil-like stools
- Rectal pain
- Unexplained weight loss
- Been using laxatives for several weeks or self care is not working
Call if:
- An infant younger than 2 months is constipated
- An infant (except those exclusively breastfed) goes 3 days without a stool -- call immediately if the child is vomiting or irritable
- A child is holding back bowel movements in order to resist toilet training
Treatment options[edit | edit source]
Although treatment depends on the cause, severity, and duration of the constipation, in most cases dietary and lifestyle changes will help relieve symptoms and help prevent them from recurring. Diet
A diet with enough fiber (20 to 35 grams each day) helps the body form soft, bulky stool. A doctor or dietitian can help plan an appropriate diet. High-fiber foods include beans, whole grains and bran cereals, fresh fruits, and vegetables such as asparagus, brussels sprouts, cabbage, and carrots. For people prone to constipation, limiting foods that have little or no fiber, such as ice cream, cheese, meat, and processed foods, is also important. Lifestyle Changes
Other changes that may help treat and prevent constipation include drinking enough water and other liquids, such as fruit and vegetable juices and clear soups, so as not to become dehydrated, engaging in daily exercise, and reserving enough time to have a bowel movement. In addition, the urge to have a bowel movement should not be ignored. Laxatives
Most people who are mildly constipated do not need laxatives. However, for those who have made diet and lifestyle changes and are still constipated, a doctor may recommend laxatives or enemas for a limited time. These treatments can help retrain a chronically sluggish bowel. For children, short-term treatment with laxatives, along with retraining to establish regular bowel habits, helps prevent constipation.
A doctor should determine when a patient needs a laxative and which form is best. Laxatives taken by mouth are available in liquid, tablet, gum powder, and granule forms. They work in various ways:
- Bulk-forming laxatives generally are considered the safest, but they can interfere with absorption of some medicines. These laxatives, also known as fiber supplements, are taken with water. They absorb water in the intestine and make the stool softer. Brand names include Metamucil, Fiberall, Citrucel, Konsyl, and Serutan. These agents must be taken with water or they can cause obstruction. Many people also report no relief after taking bulking agents and suffer from a worsening in bloating and abdominal pain.
- Stimulants cause rhythmic muscle contractions in the intestines. Brand names include Correctol, Dulcolax, Purge, and Senokot. Studies suggest that phenolphthalein, an ingredient in some stimulant laxatives, might increase a person’s risk for cancer. The Food and Drug Administration has proposed a ban on all over-the-counter products containing phenolphthalein. Most laxative makers have replaced, or plan to replace, phenolphthalein with a safer ingredient.
- Osmotics cause fluids to flow in a special way through the colon, resulting in bowel distention. This class of drugs is useful for people with idiopathic constipation. Brand names include Cephulac, Sorbitol, and Miralax. People with diabetes should be monitored for electrolyte imbalances.
- Stool softeners moisten the stool and prevent dehydration. These laxatives are often recommended after childbirth or surgery. Brand names include Colace and Surfak. These products are suggested for people who should avoid straining in order to pass a bowel movement. The prolonged use of this class of drugs may result in an electrolyte imbalance.
- Lubricants grease the stool, enabling it to move through the intestine more easily. Mineral oil is the most common example. Brand names include Fleet and Zymenol. Lubricants typically stimulate a bowel movement within 8 hours.
- Saline laxatives act like a sponge to draw water into the colon for easier passage of stool. Brand names include Milk of Magnesia and Haley’s M-O. Saline laxatives are used to treat acute constipation if there is no indication of bowel obstruction. Electrolyte imbalances have been reported with extended use, especially in small children and people with renal deficiency.
- Chloride channel activators increase intestinal fluid and motility to help stool pass, thereby reducing the symptoms of constipation. One such agent is Amitiza, which has been shown to be safely used for up to 6 to 12 months. Thereafter a doctor should assess the need for continued use.
People who are dependent on laxatives need to slowly stop using them. A doctor can assist in this process. For most people, stopping laxatives restores the colon’s natural ability to contract.
Other Treatments[edit | edit source]
Treatment for constipation may be directed at a specific cause. For example, the doctor may recommend discontinuing medication or performing surgery to correct an anorectal problem such as rectal prolapse, a condition in which the lower portion of the colon turns inside out.
People with chronic constipation caused by anorectal dysfunction can use biofeedback to retrain the muscles that control bowel movements. Biofeedback involves using a sensor to monitor muscle activity, which is displayed on a computer screen, allowing for an accurate assessment of body functions. A health care professional uses this information to help the patient learn how to retrain these muscles.
Surgical removal of the colon may be an option for people with severe symptoms caused by colonic inertia. However, the benefits of this surgery must be weighed against possible complications, which include abdominal pain and diarrhea.
Medications to avoid[edit | edit source]
Patients diagnosed with Constipation (patient information) should avoid using the following medications:
- Alosetron
If you have been diagnosed with Constipation (patient information), consult your physician before starting or stopping any of these medications.
Where to find medical care for Constipation?[edit | edit source]
Directions to Hospitals Treating Constipation
Prevention of Constipation[edit | edit source]
Avoiding constipation altogether is easier than treating it, but involves the same lifestyle measures:
- Eat lots of fiber.
- Drink plenty of fluids each day (at least 8 glasses of water per day).
- Exercise regularly.
- Go to the bathroom when you have the urge. Don't wait.
 KSF
KSF