Goal-directed therapy
 From Wikidoc - Reading time: 3 min
From Wikidoc - Reading time: 3 min
Overview[edit | edit source]
Goal-Directed Therapy is a technique used in critical care medicine involving intensive monitoring and aggressive management of perioperative hemodynamics in patients with a high risk of morbidy and mortality.[1] In cardiac surgery, GDT has proved effective when commenced after surgery. The combination of goal-directed therapy and Point-of-Care Testing has demonstrated a marked decrease in mortality for patients undergoing congenital heart surgery.[2] Further more, a reduction in morbidity and mortality has been associated with GDT techniques when used in conjunction with an electronic medical record.[3]
Early Goal-Directed Therapy is a more specific form of therapy used for the treatment of severe sepsis and septic shock. This approach involves adjustments of cardiac preload, afterload, and contractility to balance oxygen delivery with an increased oxygen demand before surgery.[4]
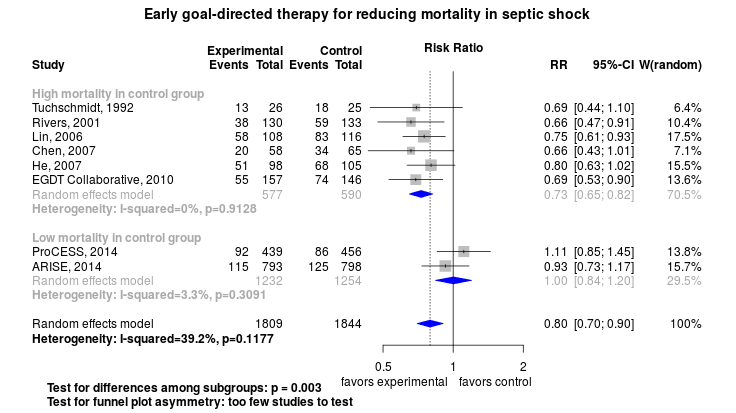
Early Goal-Directed Therapy is most likely to benefit patients in institutions where the mortality rate for septic shock is high.[5]
Shown below is a the Forest plot depicting the different trials that evaluated Goal-Directed Therapy for septic shock.
Elements[edit | edit source]
In the event of hypotension and/or lactate > 4 mmol/L, then deliver an initial minimum of 20 ml/kg of crystalloid (or colloid equivalent).
Apply vasopressors for hypotension not responding to initial fluid resuscitation to maintain mean arterial pressure (MAP) > 65 mm Hg.
In the event of persistent hypotension despite fluid resuscitation (septic shock) and/or lactate > 4 mmol/L (36 mg/dl):
- Achieve central venous pressure (CVP) of > 8 mm Hg
- Achieve central venous oxygen saturation (ScvO2) of > 70%
References[edit | edit source]
- ↑ Gordon A, Russell J, Crit Care. 2005; 9(6): 647–648. Published online 2005 November 23. doi: 10.1186/cc3951.
- ↑ Rossi AF, Khan DM, Hannan R, Boliver J, Zaidenweber M, Burke R, Intensive Care Med. 2005 Jan;31(1):98-104. Epub 2004 Dec 1
- ↑ Rossi AF, Khan D, Clin Biochem. 2004 Jun;37(6):456-61.
- ↑ Rivers, 2001 http://scalpel.stanford.edu/articles/Goal%20directed%20therapy.pdf
- ↑ openMetaAnalysis Contributors. Early goal directed therapy for septic shock: a living systematic review. GitHub. Available at http://openmetaanalysis.github.io/Early-goal-directed-therapy-for-septic-shock/. Accessed February 24, 2014.
 KSF
KSF