Health effects of tobacco smoking
 From Wikidoc - Reading time: 21 min
From Wikidoc - Reading time: 21 min
Both direct inhalation of tobacco smoke and inhalation of second hand smoke have significant negative effects on health.
The World Health Organization estimated in 2002[1] that in developed countries, 26% of male deaths and 9% of female deaths were attributable to smoking. Similarly, the United States Centers for Disease Control and Prevention describes tobacco use as "the single most important preventable risk to human health in developed countries and an important cause of premature death worldwide."[2]
Primary risks[edit | edit source]
Regular smokers are estimated to live to 2.5[3] to 10[4] years less than nonsmokers.[3] About one-half of male smokers will die of illness due to smoking.[5]
Tobacco related illnesses kill 440,000 USA citizens per year,[6] about 1,205 per day, making it the leading cause of preventable death in the U.S. The World Health Organization has stated that tobacco is set to kill a billion people this century[7]
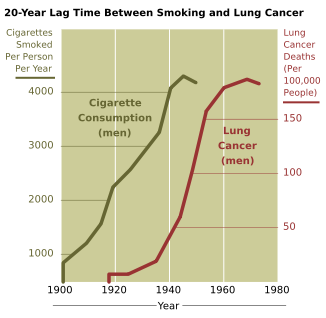
The main health risks in tobacco pertain to diseases of the cardiovascular system, in particular smoking being a major risk factor for a myocardial infarction (heart attack), diseases of the respiratory tract such as Chronic Obstructive Pulmonary Disease (COPD) and emphysema, and cancer, particularly lung cancer and cancers of the larynx and mouth. Prior to World War I, lung cancer was considered to be a rare disease, which most physicians would never see during their career. With the postwar rise in popularity of cigarette smoking came a virtual epidemic of lung cancer.[8][9]
Currently, among people who have ever smoked any kind of tobacco, almost one in ten will develop lung cancer.[1] One in six men who continue to smoke tobacco will develop lung cancer.[10] This compares to only one case of lung cancer in seventy-five lifelong non-smokers.
Incidence of impotence is approximately 85 percent higher in male smokers compared to non-smokers,[11] and it is a key cause of erectile dysfunction (ED).[12][13] Smoking causes impotence because it promotes arterial narrowing.[14]
A person's increased risk of contracting disease is directly proportional to the length of time that a person continues to smoke as well as the amount smoked. However, if someone stops smoking, then these chances gradually decrease as the damage to their body is repaired.
Diseases linked to smoking tobacco cigarettes include:
- Many forms of cancer, particularly lung cancer,[15] cancer of the kidney,[16] cancer of the larynx and head and neck, breast cancer[17] [18], bladder, esophagus, pancreas, and stomach.[19] There is some evidence suggesting an increased risk of myeloid leukemia, squamous cell sinonasal cancer, liver cancer, cervical cancer, colorectal cancer after an extended latency, childhood cancers and cancers of the gall bladder, adrenal gland and small intestine.
- Cardiovascular disease
- Respiratory ailments
- common cold and bronchitis
- Chronic obstructive pulmonary disease, emphysema and chronic bronchitis in particular
- Birth defects of pregnant smokers' offspring
- Buerger's disease (thromboangiitis obliterans)
- Cataracts that may cause blindness
- Cognitive dysfunction
- Impotence
Cigar and pipe smokers tend to inhale less smoke than cigarette smokers, so their risk of lung cancer is lower but is still several times higher than the risk for nonsmokers. Pipe and cigar smokers are also at risk for cancers of the oral cavity, larynx (voice box), or esophagus, a risk which was widely hypothesized before any link between smoking and cancer was scientifically proved as seen in the news coverage of the tobacco-related cancers of two American presidents; Ulysses S. Grant died in 1885 at age sixty-three after a long and painful public battle with throat cancer which was widely assumed at the time to be the result of his lifelong cigar habit, and Grover Cleveland was diagnosed in 1893 with cancer of the left jaw, which was frequently remarked upon by the press and public as the side where he usually had a cigar clamped. Similarly, cancer of the mouth and jaw is also a risk for chewing tobacco. The benefits of smoking cessation are immediate: blood pressure, heart rate, and temperature return to normal range; heart attack risk decreases; ability to smell and taste is enhanced; circulation improves.
It is generally assumed that the major motivational factor behind smoking is the nicotine it contains. However, the practice of ingesting the smoke from a smoldering leaf generates an enormous number of active chemical compounds, loosely lumped together as 'tar', many of which are biologically reactive and potential health dangers. (Chewing tobacco is also carcinogenic, likely because similar compounds are generated in the practice of curing it; the Nordic snus, which is steam cured and therefore does not generate these compounds, is much less carcinogenic.) There are around 3000 chemicals found in tobacco smoke. Long term exposure to other compounds in the smoke, such as carbon monoxide, cyanide, and other compounds that damage lung and arterial tissue, are believed to be responsible for cardiovascular damage and for loss of elasticity in the alveoli, leading to emphysema and COPD.
Radioactive components of tobacco[edit | edit source]
In addition to chemical, nonradioactive carcinogens, tobacco and tobacco smoke contain small amounts of lead-210 (210Pb) and polonium-210 (210Po) both of which are radioactive carcinogens. Lead 210 is a product of the decay of radium-226 and, in turn, its decay product, radon-222; lead 210 then decays to bismuth-210 and then to polonium 210, emitting beta particles in both steps. Tarry particles containing these elements lodge in the smokers' lungs where airflow is disturbed; the concentration found where bronchioles bifurcate is 100 times higher than that in the lungs overall. This gives smokers much more intense exposure than would otherwise be encountered. Polonium 210, for instance, emits high energy alpha particles which, because of their large mass, are considered to be incapable of penetrating the skin more than 40 micrometres deep, but do considerable damage (estimated at 100 times as much chromosome damage as a corresponding amount of other radiation) when a process such as smoking causes them to be emitted within the body, where all their energy is absorbed by surrounding tissue. (Lead 210 also emits gamma rays).
The radioactive elements in tobacco are accumulated from the minerals in the soil, as with any plant, but are also captured on the sticky surface of the tobacco leaves in excess of what would be seen with plants not having this property. As might be expected, the radioactivity measured in tobacco varies widely depending on where and how it is grown. One study found that tobacco grown in India averaged only 0.09 pCi per gram of polonium 210, whereas tobacco grown in the United States averaged 0.516 pCi per gram. Another study of Indian tobacco, however, measured an average of 0.4 pCi of polonium 210 per cigarette, which also would be approximately a gram of tobacco. One factor in the difference between India and the United States may be the extensive use of apatite as fertilizer for tobacco in the United States, because it starves the plant for nitrogen, thereby producing more flavorful tobacco; apatite is known to contain radium, lead 210, and polonium 210. This would also account for increased concentration of these elements compared to other crops, which do not use this mineral as fertilizer.
The presence of polonium-210 in mainstream cigarette smoke has been experimentally measured at levels of 0.0263 - 0.036 pCi,[22] which is equivalent to about 0.1 pCi per milligram of smoke; or about 0.81 pCi of lead 210 per gram of dry condensed smoke. The amount of polonium 210 inhaled from a pack of 20 cigarettes is therefore about 0.72 pCi. This seems to be independent of any form of filtering or 'low tar' cigarette. This concentration results in a highly significant increase in the body burden of these compounds. Compared to nonsmokers, heavy smokers have four times greater radioisotope density throughout their lungs. The polonium 210 content of blood in smokers averages 1.72 pCi per kilogram, compared to 0.76 pCi per kilogram in nonsmokers. Higher concentrations of polonium 210 are also found in the livers of smokers than nonsmokers. Polonium 210 is also known to be incorporated into bone tissue, where the continued irradiation of bone marrow may be a cause of leukemia, although this has not been proved as yet.
Research by NCAR radiochemist Ed Martell determined that radioactive compounds in cigarette smoke are deposited in "hot spots" where bronchial tubes branch. Since tar from cigarette smoke is resistant to dissolving in lung fluid, the radioactive compounds have a great deal of time to undergo radioactive decay before being cleared by natural processes. Indoors, these radioactive compounds linger in secondhand smoke, and therefore greater exposure occurs when these radioactive compounds are inhaled during normal breathing, which is deeper and longer than when inhaling cigarettes. Damage to the protective epithelial tissue from smoking only increases the prolonged retention of insoluble polonium 210 compounds produced from burning tobacco. Martell estimated that a carcinogenic radiation dose of 80-100 rads is delivered the lung tissue of most smokers who die of lung cancer.[23]
In other experiments, the alpha particle dosage from polonium 210 received by smokers of two packs a day was measured at 82.5 millirads per day, which would total 752.5 rads per 25 years, 150 times higher than the approximately 5 rem received from natural background radiation over 25 years. Other estimates of the dosage absorbed over 25 years of heavy smoking range from 165 to 1,000 rem, all significantly higher than natural background. In the case of the less radioactive Indian tobacco referred to above, the dosage received from polonium 210 is about 24 millirads a day, totalling 219 rads over 25 years or still about 40 times the natural background radiation exposure. In fact, all these numbers of total body burden are misleadingly low, because the dosage rate in the immediate vicinity of the deposited polonium 210 in the lungs can be from 100 to 10,000 times greater than natural background radiation. Lung cancer is seen in laboratory animals exposed to approximately one fifth of this total dosage of polonium 210.
Whether the quantities of these elements are sufficient to cause cancer is still a matter of debate. Most studies of carcinogenicity of tobacco smoke involve painting tar condensed from smoke onto the skin of mice and monitoring for development of tumors of the skin, a relatively simple process. However, the specific properties of polonium 210 and lead 210 and the model for their action, as described above, do not permit such a simple assay and require more difficult studies, requiring dosage of the mice in a manner mimicking smoking behavior of humans and monitoring for lung cancer, more difficult to observe as it is internal to the mouse.
Some researchers suggest that the degree of carcinogenicity of these radioactive elements is sufficient to account for most, if not all, cases of lung cancer related to smoking. In support of this hypothetical link between radioactive elements in tobacco and cancer is the observation that bladder cancer incidence is also proportional to the amount of tobacco smoked, even though nonradioactive carcinogens have not been detected in the urine of even heavy smokers; however, urine of smokers contains about six times more polonium 210 than that of nonsmokers, suggesting strongly that the polonium 210 is the cause of the bladder carcinogenicity, and would be expected to act similarly in the lungs and other tissue. Furthermore, many of the lung cancers contracted by cigarette smokers are adenocarcinomas, which are characteristic of the type of damage produced by alpha particle radiation such as that of polonium 210. It has also been suggested that the radioactive and chemical carcinogens in tobacco smoke act synergistically to cause a higher incidence of cancer than each alone.
However, the view that polonium 210 is responsible for many cases of cancer in tobacco smokers is disputed by at least one researcher.[24][25]
Other chemicals[edit | edit source]
There are over 19 known carcinogens in cigarettes.[26] The following are some of the most potent carcinogens:
- Benzopyrene is a highly carcinogenic and mutagenic compound which is formed during the incomplete combustion of organic matter. Tobacco manufacturers have experimented with combustionless vaporizer technology to allow cigarettes to be consumed without the formation of carcinogenic benzopyrenes.[27]
- Nitrosamine is a "deadly cancer-causing" compound found in cigarette smoke but not in uncured tobacco leaves. Nitrosamine forms on flue-cured tobacco leaves during the curing process through a chemical reaction between nicotine and other compounds contained in the uncured leaf and various oxides of nitrogen found in all combustion gases. Switching to indirect-fire curing has been shown to reduce nitrosamine levels to less than 0.1 parts per million.[28][29]
Nicotine and addiction[edit | edit source]

Nicotine is a powerful stimulant and is one of the main factors leading to the continued tobacco smoking. Although the amount of nicotine inhaled with tobacco smoke is quite small (most of the substance is destroyed by the heat) it is still sufficient to cause physical and/or psychological dependence. The amount of nicotine absorbed by the body from smoking depends on many factors, including the type of tobacco, whether the smoke is inhaled, and whether a filter is used. Despite the design of various cigarettes advertised and even tested on machines to deliver less of the toxic tar, studies show that when smoked by humans instead of machines, they deliver the same net amount of smoke. Ingesting a compound by smoking is one of the most rapid and efficient methods of introducing it into the bloodstream, second only to injection, which allows for the rapid feedback which supports the smokers' ability to titrate their dosage. On average it takes about ten seconds for the substance to reach the brain. As a result of the efficiency of this delivery system, many smokers feel as though they are unable to cease. Of those who attempt cessation and last three months without succumbing to nicotine, most are able to remain smoke free for the rest of their lives[30]. There exists a possibility of depression in some who attempt cessation, as with other psychoactive substances. Depression is also common in teenage smokers; teens who smoke are four times as likely to develop depressive symptoms as their nonsmoking peers [31].
Although nicotine does play a role in acute episodes of some diseases (including stroke, impotence, and heart disease) by its stimulation of adrenaline release, which raises blood pressure, heart rate, and free fatty acids, the most serious longer term effects are more the result of the products of the smouldering combustion process. This has enabled development of various nicotine delivery systems, such as the nicotine patch or nicotine gum, that can satisfy the addictive craving by delivering nicotine without the harmful combustion by-products. This can help the heavily dependent smoker to quit gradually, while discontinuing further damage to health.
Smoking and cardiovascular disease[edit | edit source]
Smoking also increases the chance of heart disease. Several ingredients of tobacco lead to the narrowing of blood vessels, increasing the likelihood of a blockage, and thus a heart attack or stroke. According to a study by an international team of researchers, people under 40 are five times more likely to have a heart attack if they smoke.[32]
Other tobacco chemicals lead to high blood pressure. Also, some chemicals may damage the inside of arteries, for example making it possible for cholesterol to adhere to the artery wall, possibly leading to a heart attack.
Effect of smoking on oral health[edit | edit source]
It is generally accepted among the general public that smoking can have devastating effects on the cardiovascular system and other important organs in the body, though the effects on the oral cavity are generally underestimated. Perhaps the most serious oral condition that can arise from tobacco smoking is that of oral cancer. However, smoking also increases the risk for various other oral diseases, some of which are almost completely exclusive to smokers.
Smoking has been proven to be an important factor in the staining of teeth.[33][34] Halitosis is common among tobacco smokers. Other oral diseases that are known to have strong links to smoking are leukoplakia, Snuff Dipper's lesions and smoker's palate. Currently, there is growing evidence that tobacco greatly increases the risk of periodontal diseases, which includes bone and tooth loss. In addition, many smokers report a loss of taste sensation and/or salivary changes.
Physical and psychological effects on smokers[edit | edit source]
Smokers report a variety of physical and psychological effects from smoking tobacco. Those new to smoking will experience nausea, dizziness, and rapid heart beat. The unpleasant symptoms will eventually vanish over time, with repeated use, as the body builds a tolerance to the chemicals in the cigarettes, such as nicotine.
In many respects, nicotine acts on the nervous system in a similar way to caffeine. Some writings have stated that smoking can also increase mental concentration; one study documents a significantly better IQ on the normed Advanced Raven Progressive Matrices test after smoking.[35] Most smokers say they enjoy smoking, which is part of the reason why many continue to do so even though they are aware of the health risks. Taste, smell, and visual enjoyment are also major contributions to the enjoyment of smoking, in addition to camaraderie with other smokers. Paradoxically, chronic exposure to tobacco smoke inhibits one's sense of taste and smell, rendering him or her unable to enjoy these aspects of tobacco smoking.
Most smokers, when denied access to nicotine, exhibit symptoms such as irritability, jitteriness, dry mouth, and rapid heart beat.[36] Longer abstinence may lead to insomnia and even mild depression. The onset of these symptoms is very fast, nicotine's half-life being only 1 hour. Withdrawal symptoms can appear even if the smoker's consumption is very limited or irregular, appearing after only 4-5 cigarettes in most adolescents. An ex-smoker's chemical dependence to nicotine will cease after approximately ten to twenty days, although the brain's number of nicotine receptors is permanently altered, and the psychological dependence may linger for months or even many years. Unlike illicit recreational drugs and alcohol, nicotine does not measurably alter a smoker's motor skills, cognition, judgement, or language abilities while under the influence of the drug, but nicotine withdrawal symptoms such as irritability and incapacity to concentrate can have an influence on these aspects. Tobacco withdrawal has been shown to cause clinically significant distress.[37]
The majority of these effects are due to nicotine withdrawal,[36] and so smokers who are not addicted to nicotine will not suffer from them.
Some studies suggest that a link exists between smoking and mental illness, citing the high incidence of smoking amongst those suffering from schizophrenia[38] and the possibility that smoking may alleviate some of the symptoms of mental illness,[39] but these have not been conclusive.
Tobacco and reproduction[edit | edit source]
Effects of smoking on sperm cells[edit | edit source]
There is increasing evidence that the harmful products of tobacco smoking kill sperm cells.[40][41] Therefore, some governments require manufacturers to put warnings on packets.
Spontaneous abortion[edit | edit source]
A number of studies have shown that tobacco use is a significant factor in spontaneous abortions among pregnant smokers, and that it contributes to a number of other threats to the health of the fetus.[42] Second-hand smoke appears to present an equal danger to the fetus, as one study noted that "heavy paternal smoking increased the risk of early pregnancy loss."[43]
SIDS[edit | edit source]
Secondhand smoke is connected to Sudden Infant Death Syndrome (SIDS). Infants who die from Sudden Infant Death Syndrome tend to have higher concentrations of nicotine and cotinine (a biological marker for secondhand smoke exposure) in their lungs than those who die from other causes. While smoking during pregnancy increases the risk of Sudden Infant Death Syndrome, infants exposed to secondhand smoke after birth are also at a greater risk of Sudden Infant Death Syndrome whether or not the parent(s) smoked during pregnancy.[44]
Epidemiology of smoking[edit | edit source]
A team of British scientists headed by Richard Doll carried out a longitudinal study of 34,439 medical specialists from 1951 to 2001, generally called the "British doctors study."[45] The study demonstrated that smoking decreased life expectancy by 10 years and that almost half of the smokers died from diseases possibly caused by smoking (cancer, heart disease, and stroke). About 5,900 of the study participants are still alive and only 134 of them still smoke.
In the UK, the impact of smoking is felt most keenly by the lower social classes, which are known to have worse life expectancy than those better off. Half the difference in survival to age 70 between social classes I and V is estimated to be due to the higher smoking prevalence in the lower class group.[46]
Risks by kind of tobacco[edit | edit source]
Low Tar/Light Cigarettes[edit | edit source]
There is no credible evidence that "Low Tar," "Light," or "Ultra Light" cigarettes are safer than regular cigarettes.[47]
Most of these terms refer to the type of filter that is used, and can vary depending on the brand.
Cigar vs Cigarette Smoking[edit | edit source]
Many people believe that, because cigar smokers do not inhale, cigar smoking is innocuous or less dangerous than cigarette smoking.[2] However, most scientific evidence is at odds with that impression. The National Institutes of Health, through the National Cancer Institute, determined in 1998 that "cigar smoking causes a variety of cancers including cancers of the oral cavity (lip, tongue, mouth, throat), esophagus, larynx, and lung."[3] The study concerned those who smoked at least one cigar per day, and stated "The health risks associated with less than daily smoking (occasional smokers) are not known." Although the study reports that most cigar smokers do not inhale, some smokers do inhale, particularly former cigarette smokers who have switched to cigars.[4] This yields risks of lung cancer similar to cigarette smokers. As for Environmental Tobacco Smoke (ETS, or "Second-hand Smoking"), the study points to the large amount of smoke generated by one cigar, saying "cigars can contribute substantial amounts of tobacco smoke to the indoor environment; and, when large numbers of cigar smokers congregate together in a cigar smoking event, the amount of ETS produced is sufficient to be a health concern for those regularly required to work in those environments."
Pipe smoking[edit | edit source]
Pipe smoking involves significant health risks [5][6] , particularly oral cancer [7][8].
Beneficial effects of smoking[edit | edit source]
Tobacco has sometimes been reported to have isolated positive effects on certain medical conditions, presumably due to the biological effects of nicotine. Most notably, some studies have found that patients with Alzheimer's disease are more likely not to have smoked than the general population, which has been interpreted to suggest that smoking offers some protection against Alzheimer's. However, the research in this area is limited and the results are conflicting; some studies show that smoking increases the risk of Alzheimer's disease. A recent review of the available scientific literature concluded that the apparent decrease in Alzheimer risk may be simply due to the fact that smokers tend to die before reaching the age at which Alzheimer normally occurs. "Differential mortality is always likely to be a problem where there is a need to investigate the effects of smoking in a disorder with very low incidence rates before age 75 years, which is the case of Alzheimer's disease," it stated, noting that smokers are only half as likely as non-smokers to survive to the age of 80.[48]
Some studies have found that smoking is associated with:
- A protective effect of current smoking in Parkinson's disease,[49][50] although the authors stated that it was more likely that the movement disorders which are part of Parkinson's disease prevented people from being able to smoke than that smoking itself was protective.
- A protective effect of current smoking against ulcerative colitis, although smoking increases the risk of Crohn's disease, the other form of inflammatory bowel disease.[51]
- A reduced risk of Kaposi's sarcoma in people without HIV infection.[52].
- There is some evidence for decreased rates of endometriosis in infertile women,[53] although other studies have found that smoking increases the risk in infertile women.[54] There is little or no evidence of a protective effect in fertile women.
- Some preliminary data from 1996 suggested a reduced incidence of uterine fibroids,[55] but overall the evidence is unconvincing.[56]
- There is limited evidence that smoking reduces the incidence of pregnancy-induced hypertension,[57] but not when the pregnancy is with more than one baby (i.e. it has no effect on twins etc.).[58] Smoking does, however, increase the likelihood of almost every other pregnancy-related health risk to both mother and child, and is the single most preventable cause of illness and death among mothers and infants in the developed world.[59]
- A very large percentage of schizophrenics smoke tobacco as a form of self medication.[60][61][62][63] The high rate of tobacco use by the mentally ill is a major factor in their decreased life expectancy, which is about 25 years shorter than the general population.[64]
Incidental problems[edit | edit source]
An indirect public health problem posed by cigarettes is that of accidental fires, usually linked with consumption of alcohol. Numerous cigarette designs have been proposed, some by tobacco companies themselves, which would extinguish a cigarette left unattended for more than a minute or two, thereby reducing the risk of fire. However the tobacco companies have historically resisted this idea, on the grounds that the nuisance involved in having to relight a cigarette left untouched for too long would reduce their sales. In fact, untreated tobacco formed into a cigarette will extinguish itself relatively quickly if left alone, and as a result cigarette tobacco is treated chemically to allow it to smolder indefinitely.
See also[edit | edit source]
References[edit | edit source]
- ↑ World health report 2002: reducing risks, promoting healthy life
- ↑ "Nicotine: A Powerful Addiction." Centers for Disease Control and Prevention.
- ↑ 3.0 3.1 Ferrucci L, Izmirlian G, Leveille S; et al. (1999). "Smoking, physical activity, and active life expectancy". Am. J. Epidemiol. 149 (7): 645–53. PMID 10192312.
- ↑ Doll R, Peto R, Boreham J, Sutherland I (2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (7455): 1519. doi:10.1136/bmj.38142.554479.AE. PMID 15213107.
- ↑ Doll R, Peto R, Wheatley K, Gray R, Sutherland I (1994). "Mortality in relation to smoking: 40 years' observations on male British doctors". BMJ. 309 (6959): 901–11. PMID 7755693.
- ↑ The American Legacy Foundation factsheet on Tobacco and Socio-Economic Status; their cited source is CDC (Centers for Disease Control) Cigarette Smoking Among Adults-United States, 2001. MMRW 2003; 52(40); 953-956.
- ↑ http://www.msnbc.msn.com/id/13803326/´]
- ↑ Witschi 2001, A Short History of Lung Cancer. Toxicol Sci. 2001 Nov;64(1):4-6. PMID 11606795
- ↑ Adler I. Primary malignant growths of the lungs and bronchi. New York: Longmans, Green, and Company; 1912., cited in Spiro SG, Silvestri GA. One hundred years of lung cancer. Am J Respir Crit Care Med. 2005 Sep 1;172(5):523-9. PMID 15961694
- ↑ Villeneuve PJ, Mao Y (1994). "Lifetime probability of developing lung cancer, by smoking status, Canada". Canadian journal of public health. Revue canadienne de santé publique. 85 (6): 385–8. PMID 7895211.
- ↑ "The Tobacco Reference Guide". Retrieved 2006-07-15.
- ↑ Peate I (2005). "The effects of smoking on the reproductive health of men". Br J Nurs. 14 (7): 362–6. PMID 15924009.
- ↑ Korenman SG (2004). "Epidemiology of erectile dysfunction". Endocrine. 23 (2–3): 87–91. PMID 15146084.
- ↑ Kendirci M, Nowfar S, Hellstrom WJ. (2005). "The impact of vascular risk factors on erectile function". Drugs Today (Barc). 41 (1): 65–74. PMID 15753970.
- ↑ American Legacy Foundation factsheet on lung cancer; their cited source is: CDC (Centers for Disease Control) The Health Consequences of Smoking: A Report of the Surgeon General. 2004.
- ↑ Lipworth L, Tarone RE, McLaughlin JK. The epidemiology of renal cell carcinoma. J Urol. 2006 Dec;176 (6 Pt 1):2353-8. PMID 17085101
- ↑ Cui Y, Miller AB, Rohan TE. Cigarette smoking and breast cancer risk: update of a prospective cohort study. Breast Cancer Res Treat. 2006 Dec;100(3):293-9. PMID 16773435
- ↑ Calle EE, Miracle-McMahill HL, Thun MJ, Heath CW. Cigarette smoking and risk of fatal breast cancer. Am J Epidemiol. 1994 May 15;139(10):1001-7. PMID 8178779
- ↑ Kuper H, Boffetta P, Adami HO. Tobacco use and cancer causation: association by tumour type. J Intern Med. 2002 Sep;252(3):206-24. PMID 12270001
- ↑ Anstey KJ, von Sanden C, Salim A, O'Kearney R (2007). "Smoking as a risk factor for dementia and cognitive decline: a meta-analysis of prospective studies". Am. J. Epidemiol. 166 (4): 367–78. doi:10.1093/aje/kwm116. PMID 17573335.
- ↑ Jacobsen LK, Krystal JH, Mencl WE, Westerveld M, Frost SJ, Pugh KR (2005). "Effects of smoking and smoking abstinence on cognition in adolescent tobacco smokers". Biol. Psychiatry. 57 (1): 56–66. doi:10.1016/j.biopsych.2004.10.022. PMID 15607301.
- ↑ Template:Cite-web
- ↑ E. A. Martell (1983). "Radiation Dose at Bronchial Bifurcations of Smokers from Indoor Exposure to Radon Progeny". Retrieved June 9. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=, |year=(help) - ↑ Hecht, Stephen S. (June 1997). "Approaches to Chemoprevention of Lung Cancer Based on Carcinogens in Tobacco Smoke". Environmental Health Perspectives. 105 (S4). Retrieved 2006-12-06.
- ↑ Hecht, Stephen S. (July 21, 1999). "Tobacco Smoke Carcinogens and Lung Cancer". Journal of the National Cancer Institute. 91 (14): 1194–1210. Retrieved 2006-12-06.
- ↑ Dr. C. Everett Koop. "Smoking and smokeless tobacco". Retrieved July 15. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ "DNA interaction with Benzopyrene". DNA. Retrieved March 5. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ Sumner; et al. "Retrofitting Tobacco Curing Barns". Retrieved June 9. Unknown parameter
|accessyear=ignored (|access-date=suggested) (help); Check date values in:|accessdate=(help) - ↑ NOVA. "Search for a Safer Cigarette".
- ↑ http://www.cancer.gov/cancertopics/factsheet/Tobacco/cessation
- ↑ http://www.apa.org/monitor/dec00/smoking.html
- ↑ "Health : Young smokers' heart attack risk". BBC. Retrieved 2005-12-18.
- ↑ Reibel J. Tobacco and oral diseases. Update on the evidence, with recommendations. Med Princ Pract. 2003;12 Suppl 1:22-32. PMID 12707498
- ↑ Ness L, Rosekrans Dde L, Welford JF. An epidemiologic study of factors affecting extrinsic staining of teeth in an English population. Community Dent Oral Epidemiol. 1977 Jan;5(1):55-60. PMID 264419
- ↑ Con Stough, Gordon Mangan, Tim Bates, O. Pellett (1994) Smoking and Raven IQ. Psycho-pharmacology 116:382-384
- ↑ 36.0 36.1 Jarvis MJ. Why people smoke. BMJ. 2004 Jan 31;328(7434):277-9. PMID 14751901
- ↑ Hughes JR. Clinical significance of tobacco withdrawal. Nicotine Tob Res. 2006 Apr;8(2):153-6. PMID 16766409
- ↑ Sacco KA, Bannon KL, George TP. Nicotinic receptor mechanisms and cognition in normal states and neuropsychiatric disorders. J Psychopharmacol. 2004 Dec;18(4):457-74. PMID 15582913
- ↑ Kumari V, Postma P. Nicotine use in schizophrenia: the self medication hypotheses. Neurosci Biobehav Rev. 2005;29(6):1021-34. PMID 15964073
- ↑ Agarwal A, Prabakaran SA, Said TM. Prevention of oxidative stress injury to sperm. J Androl. 2005 Nov-Dec;26(6):654-60. PMID 16291955
- ↑ Robbins WA, Elashoff DA, Xun L, Jia J, Li N, Wu G, Wei F. Effect of lifestyle exposures on sperm aneuploidy. Cytogenet Genome Res. 2005;111(3-4):371-7. PMID 16192719
- ↑ Ness, R., Grisso, J., Hirschinger, N., Markovic, N., Shaw, L., Day, N., and Kline, J. (1999). Cocaine and Tobacco Use and the Risk of Spontaneous Abortion. New England J. Med. 340:333-339; Oncken, C., Kranzler, H., O'Malley, P., Gendreau, P., Campbell, W. A. (2002). The Effect of Cigarette Smoking on Fetal Heart Rate Characteristics. Obstet Gynecol 99: 751-755.
- ↑ Venners, S.A., X. Wang, C. Chen, L. Wang, D. Chen, W. Guang, A. Huang, L. Ryan, J. O'Connor, B. Lasley, J. Overstreet, A. Wilcox, and X. Xu. (2004). Paternal Smoking and Pregnancy Loss: A Prospective Study Using a Biomarker of Pregnancy Am J Epidemiol 159: 993-1001.
- ↑ The U.S. Surgeon General's Report (Chapter 5; pages 180-194).
- ↑ Richard Doll, Richard Peto, Jillian Boreham, Isabelle Sutherland (2004). "Mortality in relation to smoking: 50 years' observations on male British doctors". BMJ. 328 (1519): 1519. Unknown parameter
|month=ignored (help) - ↑ "Securing Good Health for the Whole Population". Retrieved 2006-11-13.
- ↑ U.S. District Judge Gladys Kessler's Final Opinion, p.740
- ↑ Osvaldo P. Almeida, Gary K. Hulse1, David Lawrence2 & Leon Flicker (2002). "Smoking as a risk factor for Alzheimer's disease: contrasting evidence from a systematic review of case-control and cohort studies". Addiction. 97: 15. Unknown parameter
|month=ignored (help) - ↑ Allam MF, Campbell MJ, Hofman A, Del Castillo AS, Fernandez-Crehuet Navajas R. Smoking and Parkinson's disease: systematic review of prospective studies. Mov Disord. 2004 Jun;19(6):614-21. PMID 15197698
- ↑ Allam MF, Campbell MJ, Del Castillo AS, Fernandez-Crehuet Navajas R. Parkinson's disease protects against smoking? Behav Neurol. 2004;15(3-4):65-71. PMID 15706049
- ↑ Mahid SS, Minor KS, Soto RE, Hornung CA, Galandiuk S. Smoking and inflammatory bowel disease: a meta-analysis. Mayo Clin Proc. 2006 Nov;81(11):1462-71. PMID 17120402
- ↑ Goedert JJ, Vitale F, Lauria C, Serraino D, Tamburini M, Montella M, Messina A, Brown EE, Rezza G, Gafa L, Romano N; Classical Kaposi's Sarcoma Working Group. Risk factors for classical Kaposi's sarcoma. J Natl Cancer Inst. 2002 Nov 20;94(22):1712-8. PMID 12441327
- ↑ Missmer SA, Hankinson SE, Spiegelman D, Barbieri RL, Marshall LM, Hunter DJ. Incidence of laparoscopically confirmed endometriosis by demographic, anthropometric, and lifestyle factors. Am J Epidemiol. 2004 Oct 15;160(8):784-96. PMID 15466501
- ↑ Calhaz-Jorge C, Mol BW, Nunes J, Costa AP. Clinical predictive factors for endometriosis in a Portuguese infertile population. Hum Reprod. 2004 Sep;19(9):2126-31. PMID 15229202
- ↑ Baron JA. Beneficial effects of nicotine and cigarette smoking: the real, the possible and the spurious. Br Med Bull. 1996 Jan;52(1):58-73. PMID 8746297
- ↑ Schwartz SM, Marshall LM, Baird DD. Epidemiologic contributions to understanding the etiology of uterine leiomyomata. Environ Health Perspect. 2000 Oct;108 Suppl 5:821-7. PMID 11035989
- ↑ Zhang J, Zeisler J, Hatch MC, Berkowitz G. Epidemiology of pregnancy-induced hypertension. Epidemiol Rev. 1997;19(2):218-32. PMID 9494784
- ↑ Krotz S, Fajardo J, Ghandi S, Patel A, Keith LG. Hypertensive disease in twin pregnancies: a review. Twin Res. 2002 Feb;5(1):8-14. PMID 11893276
- ↑ Maternal and Infant Health: Smoking During Pregnancy
- ↑ {{cite paper | author = McNeill, Ann | title = Smoking and mental health - a review of the literature | publisher = SmokeFree London Programme | date = 2001 | url = http://www.ash.org.uk/html/policy/menlitrev.pdf | format = [[PDF | accessdate = 2006-12-14 }}
- ↑ Template:Cite paper
- ↑ Kelly, Ciara (1999). "Smoking Habits, Current Symptoms, and Premorbid Characteristics of Schizophrenic Patients in Nithsdale, Scotland". The American Journal of Psychiatry. American Psychiatric Association. 156: 1751–1757. Retrieved 2006-12-14. Unknown parameter
|coauthors=ignored (help) - ↑ Hughes, J.R. (1986). "Prevalence of smoking among psychiatric outpatients". The American Journal of Psychiatry. American Psychiatric Association. 143: 993–997. Retrieved 2006-12-14. Unknown parameter
|coauthors=ignored (help) - ↑ Schroeder SA (2007). "Shattuck Lecture. We can do better--improving the health of the American people". N. Engl. J. Med. 357 (12): 1221–8. doi:10.1056/NEJMsa073350. PMID 17881753.
External links[edit | edit source]
- Show Me Health
- Tobacco Smoke and Involuntary Smoking, Summary of Data Reported and Evaluation 2004 by IARC.
- UCSF Tobacco Industry Videos Collection
- UCSF Tobacco Industry Audio Recordings Collection
- BBC News: Smoking a pipe 'damages health'
- University of Wisconsin Center for Tobacco Research and Intervention
he:השפעות בריאותיות של עישון טבק
nl:Rookverslaving
sl:Vpliv kajenja tobaka na zdravje
 KSF
KSF