Heart valve
 From Wikidoc - Reading time: 5 min
From Wikidoc - Reading time: 5 min
|
WikiDoc Resources for Heart valve |
|
Articles |
|---|
|
Most recent articles on Heart valve Most cited articles on Heart valve |
|
Media |
|
Powerpoint slides on Heart valve |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Heart valve at Clinical Trials.gov Clinical Trials on Heart valve at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Heart valve
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Heart valve Discussion groups on Heart valve Patient Handouts on Heart valve Directions to Hospitals Treating Heart valve Risk calculators and risk factors for Heart valve
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Heart valve |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview[edit | edit source]
In anatomy, the heart valves are valves in the heart that maintain the unidirectional flow of blood by opening and closing depending on the difference in pressure on each side. The mechanical equivalent of the heart valves would be the reed valves.
There are four valves of the heart (not counting the valve of the coronary sinus and valve of the inferior vena cava):
- The two atrioventricular (AV) valves ensure blood flows from the atria to the ventricles, and not the other way.
- The two semilunar (SL) valves are present in the arteries leaving the heart, and they prevent blood flowing back from the arteries into the ventricles.
The sound of the heart valves shutting causes the heart sounds.
Atrioventricular valves[edit | edit source]
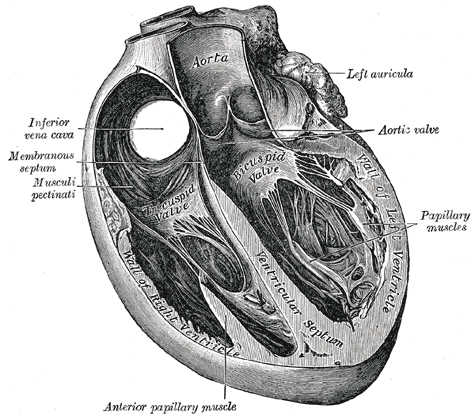
The atrioventricular valves are large, multicusped valves that prevent backflow from the ventricles into the atria during systole. They are anchored to the wall of the ventricle by chordae tendinae, that prevent the valve from inverting.
The chordae tendinae are attached to papillary muscles that cause tension to better hold the valve. Together, the papillary muscles and the chordae tendinae are known as the subvalvular apparatus. The function of the subvalvular apparatus is to keep the valves from prolapsing into the atria when they close. The subvalvular apparatus have no effect on the opening and closure of the valves, however. This is caused entirely by the pressure gradient across the valve.
Mitral valve[edit | edit source]
Also known as the bicuspid valve, the mitral valve gets its name from the resemblance to a bishop's mitre (a type of hat). It prevents blood flowing from the left ventricle into the left atrium. It is on the left side of the heart and has two leaflets.
A common complication of rheumatic fever is thickening and stenosis of the mitral valve.
Tricuspid valve[edit | edit source]
The tricuspid valve is on the right side of the heart, between the right atrium and the right ventricle.
Semilunar valves[edit | edit source]
The semilunar vlalves are positioned on the pulmonary artery and the aorta. These valves do not have chordae tendinae, but are more similar to valves in veins.
Aortic valve[edit | edit source]
The aortic valve lies between the left ventricle and the aorta. The aortic valve has three cusps. During ventricular systole, pressure rises in the left ventricle. When the pressure in the left ventricle rises above the pressure in the aorta, the aortic valve opens, allowing blood to exit the left ventricle into the aorta. When ventricular systole ends, pressure in the left ventricle rapidly drops. When the pressure in the left ventricle decreases, the aortic pressure forces the aortic valve to close. The closure of the aortic valve contributes the A2 component of the second heart sound (S2).
The most common congenital abnormality of the heart is the bicuspid aortic valve. In this condition, instead of three cusps, the aortic valve has two cusps. This condition is often undiagnosed until the person develops calcific aortic stenosis. Aortic stenosis occurs in this condition usually in patients in their 40s or 50s, an average of over 10 years earlier than in people with normal aortic valves.
Pulmonic valve[edit | edit source]
The pulmonic valve lies between the right ventricle and the pulmonary artery and also has three cusps.
Pathology of the valves[edit | edit source]
- Endocarditis - inflammation of the inner layer of the endocardium.
- Stenosis - a constricture of the heart valve, making it hard for blood to get through.
- Insufficiency (also regurgitation or incompetence) - the inability of the heart valve to close properly, meaning some blood can flow the wrong way.
-
An artificial heart valve may be used to surgically replace a patient's damaged valve.
-
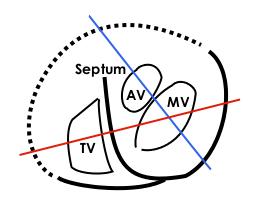
MV: Mitral valve, TV: Tricuspid valve, AV: Aortic valve, Septum: Interventricular septum. Continuous lines demarkates septum and free wall seen in echocardiogram, dotted line is a suggestion of where the free wall of the right ventricle should be. The red line represents where the upper left loop in the echocardiogram transects the 3D-loop, the blue line represents the lower loop.
See also[edit | edit source]
- Disorders of the valves (Valvular heart disease)
- Aortic valve disorders:
- Mitral valve disorders
- Pulmonic valve disorders
- Tricuspid valve disorders
- Cardiac fibrosis
- Congenital heart disease
- Endocarditis
- Heart sounds
- Artificial heart valve
External links[edit | edit source]
- Mitral Valve Repair at The Mount Sinai Hospital - "Mitral Valve Anatomy"
Additional Reading[edit | edit source]
- Moss and Adams' Heart Disease in Infants, Children, and Adolescents Hugh D. Allen, Arthur J. Moss, David J. Driscoll, Forrest H. Adams, Timothy F. Feltes, Robert E. Shaddy, 2007 ISBN 0781786843
- Hurst's the Heart, Fuster V, 12th ed. 2008, ISBN 978-0-07-149928-6
- Willerson JT, Cardiovascular Medicine, 3rd ed., 2007, ISBN 978-1-84628-188-4
de:Herzklappe
eo:Korvalvo
he:שסתום הלב
it:Valvola cardiaca
nl:Hartklep
nn:Hjarteklaff
 KSF
KSF