MHC class I
 From Wikidoc - Reading time: 4 min
From Wikidoc - Reading time: 4 min
|
WikiDoc Resources for MHC class I |
|
Articles |
|---|
|
Most recent articles on MHC class I Most cited articles on MHC class I |
|
Media |
|
Powerpoint slides on MHC class I |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on MHC class I at Clinical Trials.gov Clinical Trials on MHC class I at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on MHC class I
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on MHC class I Discussion groups on MHC class I Patient Handouts on MHC class I Directions to Hospitals Treating MHC class I Risk calculators and risk factors for MHC class I
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for MHC class I |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview[edit | edit source]
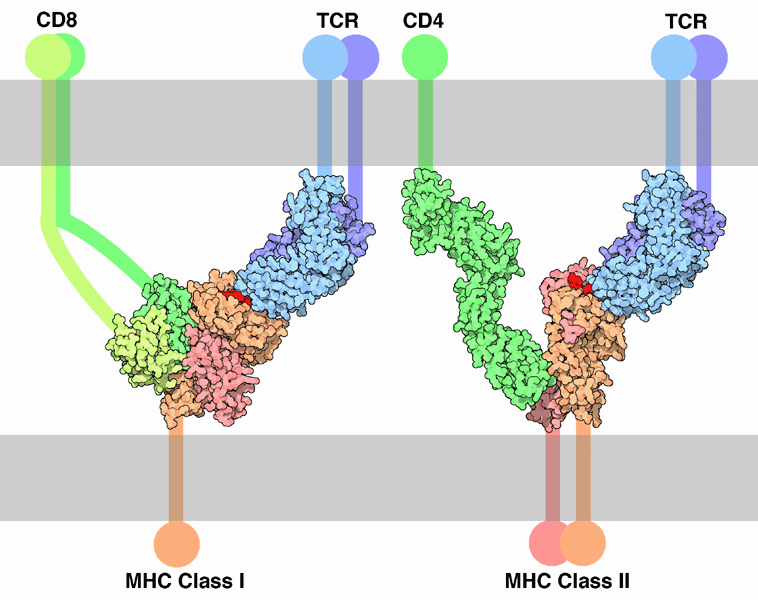
There are two primary classes of major histocompatibility complex (MHC) molecules, class I and II. MHC class I molecules are found on almost every nucleated cell of the body. Because MHC class I molecules present peptides derived from cytosolic proteins, the pathway of MHC class I presentation is often called the cytosolic or endogenous pathway.
Structure[edit | edit source]
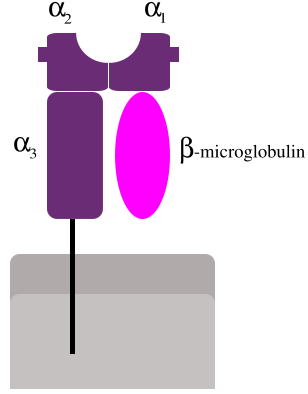
MHC class I molecules are heterodimers, consisting of a single transmembrane polypeptide chain (the α-chain) and a β2 microglobulin (which is encoded elsewhere, not in the MHC). The α chain has three polymorphic domains, α1, α2, α3. Between α1 and α2 is the peptide-binding groove which binds peptides derived from cytosolic proteins. The groove consists of eight β-pleated sheets on the bottom and two α helices making up sides. The peptide in the groove remains bound for the life of the class I molecule, and is typically 8-9 amino acids in length.
Production[edit | edit source]
The peptides are mainly generated in the cytosol by the proteasome. The proteasome is a macromolecule that consists of 28 subunits, of which half of them contain proteolytic activity. The proteasome degrades intracellular proteins into small peptides that are then released into the cytosol. The peptides have to be translocated from the cytosol into the endoplasmic reticulum (ER) to meet the MHC class I molecule, whose peptide-binding site is in the lumen of the ER.
Translocation[edit | edit source]
The peptide translocation from the cytosol into the lumen of the ER is accomplished by the transporter associated with antigen processing (TAP). TAP is a member of the ABC transporter family and is a heterodimeric multimembrane-spanning polypeptide consisting of TAP1 and TAP2. The two subunits form a peptide binding site and two ATP binding sites that face the lumen of the cytosol. TAP binds peptides on the cytoplasmic site and translocates them under ATP consumption into to the lumen of the ER. The MHC class I molecule is then in turn loaded with peptides in the lumen of the ER. The peptide-loading process involves several other molecules that form a large multimeric complex consisting of TAP, tapasin, calreticulin, calnexin, and ERP57.
Once the peptide is loaded onto the MHC class I molecule, it leaves the ER through the secretory pathway to reach the cell surface. The transport of the MHC class I molecules through the secretory pathway involves several posttranslational modifications of the MHC molecule. Some of the posttranslational modifications occur in the ER and involve change to the N-glycan regions of the protein, followed by extensive changes to the N-glycans in the Golgi apparatus. The N-glycans mature fully before they reach the cell surface.
Peptide removal[edit | edit source]
Peptides that fail to bind MHC class I molecules in the lumen of the endoplasmic reticulum are removed from the ER via the sec61 channel into the cytosol, where they might undergo further trimming in size, and might be translocated by TAP back into ER for binding to an MHC class I molecule.
Effect of viruses[edit | edit source]
MHC class I molecules are loaded with proteins generated in the cytosol. As viruses infect a cell by entering its cytoplasm, this cytosolic, MHC class I-dependent pathway of antigen presentation is the primary way for a virus-infected cell to signal T cells. MHC class I molecules generally interact exclusively with CD8+ ("cytotoxic") T cells (CTLs). The fate of the virus-infected cell is almost always apoptosis initiated by the CTL, effectively reducing the risk of infecting neighboring cells.
Genes and isotypes[edit | edit source]
Additional images[edit | edit source]
-
TCR-MHC bindings
External links[edit | edit source]
- Histocompatibility+Antigens+Class+I at the US National Library of Medicine Medical Subject Headings (MeSH)
- MHC+Class+I+Genes at the US National Library of Medicine Medical Subject Headings (MeSH)
 KSF
KSF