Mycotic aneurysm
 From Wikidoc - Reading time: 4 min
From Wikidoc - Reading time: 4 min
|
WikiDoc Resources for Mycotic aneurysm |
|
Articles |
|---|
|
Most recent articles on Mycotic aneurysm Most cited articles on Mycotic aneurysm |
|
Media |
|
Powerpoint slides on Mycotic aneurysm |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Mycotic aneurysm at Clinical Trials.gov Trial results on Mycotic aneurysm Clinical Trials on Mycotic aneurysm at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Mycotic aneurysm NICE Guidance on Mycotic aneurysm
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Mycotic aneurysm Discussion groups on Mycotic aneurysm Patient Handouts on Mycotic aneurysm Directions to Hospitals Treating Mycotic aneurysm Risk calculators and risk factors for Mycotic aneurysm
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Mycotic aneurysm |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Ogheneochuko Ajari, MB.BS, MS [2]; Faizan Sheraz, M.D. [3]
Overview[edit | edit source]
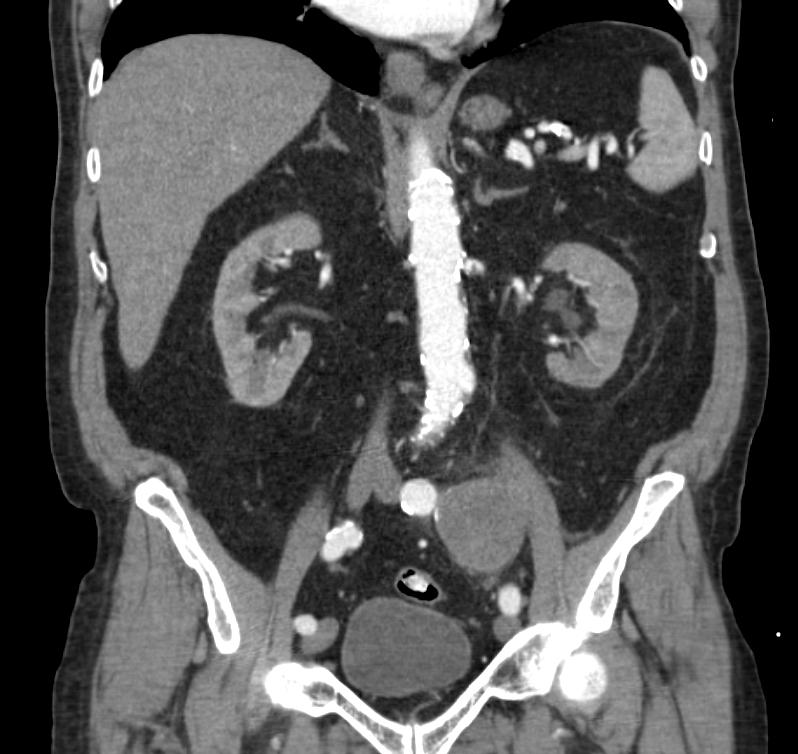
Mycotic aneurysm is an aneurysm that results from an infectious process that involves the arterial wall.[1] A person with a mycotic aneurysm has a bacterial infection in the wall of an artery, resulting in the formation of an aneurysm. The most common locations include arteries in the abdomen, thigh, neck, and arm. A mycotic aneurysm can result in sepsis, or life-threatening bleeding if the aneurysm ruptures. Less than 3% of abdominal aortic aneurysms are mycotic aneurysms.[2]
Historical Perspective[edit | edit source]
William Osler first used the term "mycotic aneurysm" in 1885 to describe a mushroom-shaped aneurysm in a patient with subacute bacterial endocarditis. This may create considerable confusion, since "mycotic" is typically used to define fungal infections. However, mycotic aneurysm is still used for all extracardiac or intracardiac aneurysms caused by infections, except for syphilitic aortitis.[3] The term "infected aneurysm," proposed by Jarrett and associates[4] is more appropriate, since few infections involve fungi.[5] According to some authors, a more accurate term might have been endovascular infection or infective vasculitis, because mycotic aneurysms are not due to a fungal organism.[6]
Causes[edit | edit source]
Life Threatening Causes[edit | edit source]
Life-threatening causes include conditions which may result in death or permanent disability within 24 hours if left untreated.
Common Causes[edit | edit source]
Causes by Organ System[edit | edit source]
| Cardiovascular | No underlying causes |
| Chemical/Poisoning | No underlying causes |
| Dental | No underlying causes |
| Dermatologic | No underlying causes |
| Drug Side Effect | No underlying causes |
| Ear Nose Throat | No underlying causes |
| Endocrine | Diabetes mellitus |
| Environmental | No underlying causes |
| Gastroenterologic | No underlying causes |
| Genetic | No underlying causes |
| Hematologic | No underlying causes |
| Iatrogenic | No underlying causes |
| Infectious Disease | Acinetobacter, aspergillus, bacteroides, brucella, burkholderia pseudomallei, campylobacter, candida, clostridium perfringens, clostridium septicum, clostridium, corynebacterium, coxiella burnetii, cryptococcus, e. coli, group B streptococcal infection, haemophilus influenzae, klebsiella, lactococcus cremoris, listeria, melioidosis, methicillin-resistant staphylococcus aureus, mycobacterium tuberculosis, peptostreptococcus, propionibacterium acnes, pseudallescheria boydii, pseudomonas, rothia dentocariosa, salmonella, staphylococcus aureus, staphylococcus epidermidis, streptococcus pneumoniae, syphilis, treponema pallidum, vancomycin-intermediate staphylococcus aureus, yersinia |
| Musculoskeletal/Orthopedic | No underlying causes |
| Neurologic | No underlying causes |
| Nutritional/Metabolic | No underlying causes |
| Obstetric/Gynecologic | No underlying causes |
| Oncologic | No underlying causes |
| Ophthalmologic | No underlying causes |
| Overdose/Toxicity | No underlying causes |
| Psychiatric | No underlying causes |
| Pulmonary | No underlying causes |
| Renal/Electrolyte | No underlying causes |
| Rheumatology/Immunology/Allergy | No underlying causes |
| Sexual | No underlying causes |
| Trauma | No underlying causes |
| Urologic | No underlying causes |
| Miscellaneous | No underlying causes |
Causes in Alphabetical Order[edit | edit source]
Natural History, Complications, and Prognosis[edit | edit source]
Mycotic aneurysms account for 2.6% of aortic aneurysms.[3] For the clinician, early diagnosis is the cornerstone of effective treatment. Without medical or surgical management, catastrophic hemorrhage or uncontrolled sepsis may occur. However, symptomatology is frequently nonspecific during the early stages, so a high index of suspicion is required to make the diagnosis.[5]
Intracranial mycotic aneurysms (ICMAs) complicate about 2% to 3% of infective endocarditis (IE) cases, although as many as 15% to 29% of patients with IE have neurologic symptoms.[6]
Diagnosis[edit | edit source]
Imaging Studies[edit | edit source]
Medical Therapy[edit | edit source]
Antimicrobial Regimen[edit | edit source]
- Empiric antimicrobial therapy[8]
- Preferred regimen: Vancomycin 15 mg/kg IV divided q12h (trough of 15-20 mcg/mL) for 6 weeks AND (Ceftriaxone 2 g IV q24h for 6 weeks OR Piperacillin-Tazobactam 3.375 g IV q6h for 6 weeks OR Ciprofloxacin 400 mg IV q12h for 6 weeks)
- Note: For critically ill patients, start with a vancomycin loading dose of 25 mg/kg.
References[edit | edit source]
- ↑ emedicine > Cerebral Aneurysm Author: Jonathan L Brisman. Coauthors: Emad Soliman, Abraham Kader, Norvin Perez. Updated: Sep 23, 2010
- ↑ http://www.freemd.com/mycotic-aneurysm/overview.htm Author: Stephen J. Schueler, MD; Coauthors: John H. Beckett, MD; D. Scott Gettings, MD. Updated November 13, 2011
- ↑ 3.0 3.1 Bayer AS, Scheld WM. Endocarditis and intravascular infections. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett's Principles and Practice of Infectious Diseases. 5th ed. Philadelphia: Churchill Livingstone; 2000:888-892.
- ↑ Jarrett F, Darling RC, Mundth ED, Austen WG. Experience with infected aneurysms of the abdominal aorta. Arch Surg. 1975;110:1281-1286.
- ↑ 5.0 5.1 Mycotic (Infected) Aneurysm Caused by Streptococcus pneumoniae. Khosrow Afsari, et al. Infect Med. 2001;18(6)http://www.medscape.com/viewarticle/410168
- ↑ 6.0 6.1 http://www.gundersenhealth.org/upload/docs/Research/MedJournal/Vol6No1Endocarditis.pdf
- ↑ 7.0 7.1 Gomes MN, Choyke PL, Wallace RB (1992). "Infected aortic aneurysms. A changing entity". Ann Surg. 215 (5): 435–42. PMC 1242469. PMID 1616380.
- ↑ Gilbert, David (2014). The Sanford guide to antimicrobial therapy 2014. Sperryville, Va: Antimicrobial Therapy. ISBN 978-1930808782.
 KSF
KSF