Penetrating head injury
 From Wikidoc - Reading time: 9 min
From Wikidoc - Reading time: 9 min
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Joanna Ekabua, M.D. [2]
Synonyms and keywords:: Penetrating head injury
Overview[edit | edit source]
Penetrating head injury, or open head injury, is a life-threatening condition in which the dura mater, is breached and there is a foreign body in the brain. Penetrating injury can be caused by high-velocity projectiles such as bullets, or objects of lower velocity such as knives, or bone fragments from a skull fracture that are driven into the brain. Although penetrating head injuries can be dramatic in appearance and presentation, the trajectory is of particular importance the case of gunshot wounds. Penetrating head injury can cause loss of abilities controlled by parts of the brain that are damaged. Risk factors for penetrating head injury include violence, accidents, and suicide attempts. Some complications include Infection, abscess formation, cerebrospinal fistula, neuroendocrine dysfunction, cerebrospinal fluid leak, traumatic intracranial aneurysm, dural venous sinuses thrombus, and bullet fragment migration. Diagnosis is made by physical and neurologic exams, CT scan, and MRI. Immediate neurosurgical consulting mandatory in all cases of penetrating head injuries. Compared to close head injuries, penetrating head injuries carries a worse prognosis.
Historical Perspective[edit | edit source]
- There is limited knowledge on the historical perspective of penetrating head injury.
- Penetrating head injury secondary to stabbing through the cranium was first published in 1800.[1][2]
Classification[edit | edit source]
- Penetrating head injury may be classified into 2 main groups based on messile type[3][4]
- Non-missile type
- Missle type
- Wounds resulting from penetrating brain injury can be classified into five categories[5]
- Tangential
- Penetrating
- Perforating
- Ricochet
- Careening.
Pathophysiology[edit | edit source]
- The pathophysiology of penetrating head injury is due to injury to neuronal and vascular structures which is mostly focal. This injury leads to release of thromboplastin, which can lead to problems with clotting, infection, swelling or bleeding, potentially crushing delicate brain tissue. If severe, brain herniation can occur. Most deaths from penetrating trauma are caused by damage to blood vessels, leading to intracranial hematomas and ischemia as early as 30 minutes after the initial injury. This can, in turn, lead to a biochemical cascade called the ischemic cascade.[6][7][5]
- Low-velocity objects usually cause penetrating injuries in the regions of the skull's temporal bones or orbital surfaces; where the bones are thinner and thus more likely to break.[6] Damage from lower-velocity penetrating injuries is restricted to the tract of the stab wound because the lower-velocity object does not create as much cavitation.[6] However, low-velocity penetrating objects such as slow bullets may ricochet inside the skull, continuing to cause damage until they stop moving.[8]
- In penetrating injury from high-velocity missiles, injuries may occur not only from initial laceration and crushing of brain tissue by the projectile but also from the subsequent cavitation. High-velocity objects create centrifugal forces and can create a shock wave that cause stretch injuries, forming a cavity that is three to four times greater in diameter than the missile itself.[6] A pulsating temporary cavity is also formed by a high-speed missile and can have a diameter thirty times greater than that of the missile.[6] Though this cavity is reduced in size once the force is over, the tissue that was compressed during cavitation remains injured. Destroyed brain tissue may either be ejected from entrance or exit wounds or packed up against the sides of the cavity formed by the missile.[6]
Causes[edit | edit source]
Common causes of penetrating head injury


Differentiating Penetrating Head Injury from other Diseases[edit | edit source]
Penetrating head injury must be differentiated from
Epidemiology and Demographics[edit | edit source]
- The incidence of penetrating head injury has increased over the last decade with an estimated 35,000 civilian deaths annually.[12]
- Patients of all age groups may experience penetrating head injury.
- There is no racial predilection to penetrating head injury.
- Penetrating head injury affects men and women equally.
Risk Factors[edit | edit source]
Common risk factors in the development of penetrating head injury include[1]
- Violence
- Accidents
- Explosions/blast
- Suicide attempts
Screening[edit | edit source]
There is insufficient evidence to recommend routine screening for penetrating head injury.
Natural History, Complications, and Prognosis[edit | edit source]
- If left untreated, 100% of patients with penetrating head injury die.[1]
- Common complications of penetrating head injury[1][12][13][5]
- Intracranial infections/cerebral abscess, most common cause staphylococcus aureus
- Local wound infection. Most common causes are wood splinters and bone fragments
- Cerebral vasospasm in the presence of subarachnoid hemorrhage
- Up to 50% of patients with penetrating brain injuries get late-onset epilepsy
- Traumatic intracranial aneurysm/pseudoaneurysm
- Meningitis
- Ventriculitis
- Hyponatremia
- Cerebral edema
- Cerebral contusions
- Elevated intracranial pressure
- Intraventricular hemorrhage
- Cerebrospinal fistula
- Neuroendocrine dysfunction
- Cerebrospinal fluid leak
- Hematomas
- Arteriovenous fistulas
- Dural venous sinuses thrombus
- Bullet fragment migration
- Neurological deficits
- copper or Lead toxicity from retained bullet fragments
- Death
- Prognosis is generally good with early decompressive craniectomy in non bullet penetrating objects.[1][5] The highest-velocity injuries tend to have the worst associated damage.[14] Penetrating injury from any missile such as a bullet has a mortality rate of 92%.[6] Thus, firearms cause the most head injury-related deaths.[8] Perforating injuries have an even worse prognosis.[6]About 70-90% of penetrating head injury victims die before arriving the hospital, and 50% of those who survive to the hospital die during resuscitation attempts in the emergency department.
The following clinical factors have been associated with poor outcomes[5]
- Low post-resuscitation glasgow coma scale
- Older age
- Large and unreactive pupils
- Asymmetric Pupil
- Hypoxia, and hypotension (Systolic blood pressure <90 mmHg).
Other factors include
- Time to reach neurosurgeon
- Weapon ballistics, including
- Caliber
- Proximity to the projectile’s source.
Diagnosis[edit | edit source]
Diagnostic Study of Choice
- There are no established criteria for the diagnosis of penetrating head injury.
History and Symptoms
The hallmark of penetrating head injury is finding[1][15][2]
- Headache
- Vomiting
- Confusion
- Weakness of extremities
- Loss of consciousness
- Seizure
- Anhedonia in patients with right ventrolateral injury
Physical Examination
Common physical examination findings of penetrating head injury include[5]
- Penetrating object in the skull.
- Neurologic deficit
- Motor and sensory skills
- Hearing and speech
- Coordination and balance
- Mental status
- Mood or behavior changes
- Normal to abnormal Glasgow Coma Scale (GCS). GCS is considered to be the best single predictor of good or bad outcome following penetrating head injury. Survival rate is 0-8.1%, 35.6% and 90.5% for GCS scores of 3-5, 6-8 and 9-15 respectively
- GCS 8-15 and somnolence: Sleepy, easy to wake
- GCS 8-15 and stupor: Hypnoid, hard to wake
- GCS ≥ 13: Mild Head Injury
- GCS 9–12: Moderate Head Injury
- GCS ≤ 8: Severe Head Injury
- GCS 7-8: Light coma; Coma Grade I
- GCS 5-6: Light coma; Coma Grade II
- GCS 4: Deep coma; Coma Grade III
- GCS 3: Deep coma; Coma Grade IV
{{#ev:youtube|FihnmEx6Rqk}}
Laboratory Findings
- There are no diagnostic laboratory findings associated with penetrating head injury.
Electrocardiogram
- There are no ECG findings associated with penetrating head injury.
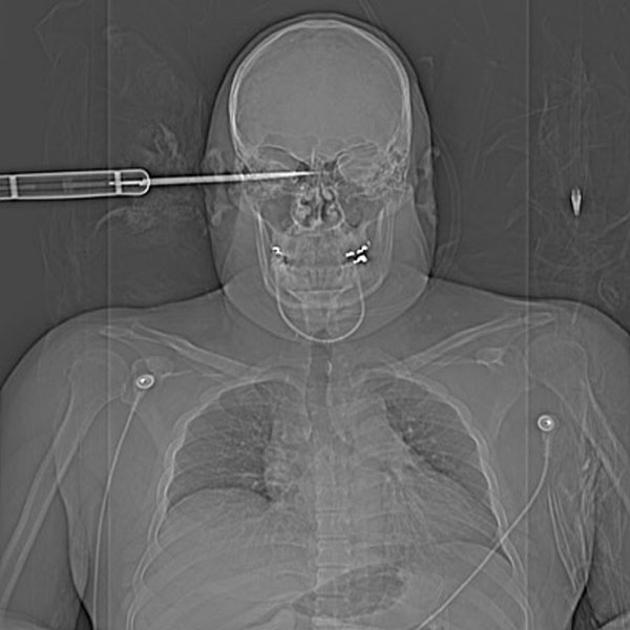
X-ray
An x-ray may be helpful in the diagnosis of penetrating head injury


Ultrasound
- There are no ultrasound findings associated with penetrating head injury.
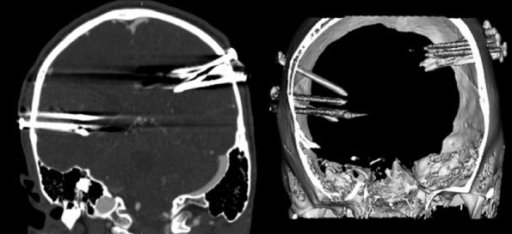
CT Scan
Head CT scan is helpful in the diagnosis of penetrating head injury. CT scan shows the foreign object.

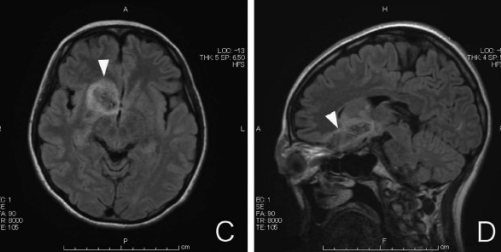
MRI
Cranial MRI may be helpful in the diagnosis of penetrating head injury.
- MRI can be dangerous in cases of retained ferromagnetic objects as it can move in response to the magnetic torque.[1]
Other Imaging Findings
- There are no other imaging findings associated with penetrating head injury.
Other Diagnostic Studies
- There are no other diagnostic studies associated with penetrating head injury.
Treatment[edit | edit source]
Medical Therapy[edit | edit source]
- Penetrating head injury is a medical emergency and requires prompt treatment.
- Aggressive resuscitation has been associated with improved survival.[5]
- Correction of hypotensionand hypoxia
- Airway maintenance
- Control of hemorrhaging
- Hyperosmolar therapy with mannitol or hypertonic saline
- Correction of traumatic coagulopathy
- Placement of a cervical immobilization device
- Treatment of penetrating head injury aims at controlling bleeding, intracranial pressure, and preventing infections.[1]
- Ceftriaxone
- 1 g IV 0.5 to 2 hours prior to surgery.
- 4 g/day IV divided every 12 to 24 hours; maximum 4 g/day[16]
- Metronidazole
- Loading Dose: 15 mg/kg infused over one hour (approximately 1 g for a 70-kg adult).
- Maintenance Dose: 7.5 mg/kg infused over one hour every six hours (approximately 500 mg for a 70-kg adult). The first maintenance dose should be instituted six hours following the initiation of the loading dose.
- Anticonvulsant
- Antitetanic vaccine
- Analgesics
- Ceftriaxone
Surgery[edit | edit source]
Surgery is the mainstay of treatment for penetrating head injury. Procedures used are [1][5]
- Craniectomy with dura mater plasty
- Craniotomy
Both procedures have been shown to have similar morbidity and mortality. Optimum outcomes have been reported with early decompressive craniectomy.
Prevention[edit | edit source]
Primary Prevention[edit | edit source]
Effective measures for the primary prevention of penetrating head injury include[2]
- An effective measure for the primary prevention of penetrating head injury are helmets
- Use seat health while driving
Secondary Prevention[edit | edit source]
- There are no established measures for the secondary prevention of penetrating head injury.
References[edit | edit source]
- ↑ 1.0 1.1 1.2 1.3 1.4 1.5 1.6 1.7 1.8 Fahde Y, Laghmari M, Skoumi M (2017). "Penetrating head trauma: 03 rare cases and literature review". Pan Afr Med J. 28: 305. doi:10.11604/pamj.2017.28.305.10376. PMC 5927577. PMID 29721135.
- ↑ 2.0 2.1 2.2 2.3 Das JM, Chandra S, Prabhakar RB (2015). "Penetrating brain injury with a bike key: a case report". Ulus Travma Acil Cerrahi Derg. 21 (6): 524–6. doi:10.5505/tjtes.2015.43958. PMID 27054647.
- ↑ 3.0 3.1 Khan KA, Gandhi A, Sharma V, Jain S (2019). "Penetrating head injury due to angle grinder: an occupational hazard". Br J Neurosurg. 33 (2): 202–206. doi:10.1080/02688697.2018.1467375. PMID 29693468.
- ↑ Drosos E, Giakoumettis D, Blionas A, Mitsios A, Sfakianos G, Themistocleous M (2018). "Pediatric Nonmissile Penetrating Head Injury: Case Series and Literature Review". World Neurosurg. 110: 193–205. doi:10.1016/j.wneu.2017.11.037. PMID 29155117.
- ↑ 5.0 5.1 5.2 5.3 5.4 5.5 5.6 5.7 Young JB, Godara P, Williams V, Summerfelt P, Connor TB, Tarima S; et al. (2019). "Assessing Retinal Structure in Patients with Parkinson's Disease". J Neurol Neurophysiol. 10 (1). doi:10.4172/2155-9562.1000485. PMC 6494090. PMID 31057987.
- ↑ 6.0 6.1 6.2 6.3 6.4 6.5 6.6 6.7 Invalid
<ref>tag; no text was provided for refs namedVinas and Pilistis - ↑ Orlando Regional Healthcare, Education and Development. 2004. "Overview of Adult Traumatic Brain Injuries." Retrieved on September 6, 2007.
- ↑ 8.0 8.1 Brain Injury Association of America (BIAUSA). "Types of Brain Injury." Retrieved on February 6, 2007.
- ↑ Awori J, Wilkinson DA, Gemmete JJ, Thompson BG, Chaudhary N, Pandey AS (2017). "Penetrating Head Injury by a Nail Gun: Case Report, Review of the Literature, and Management Considerations". J Stroke Cerebrovasc Dis. 26 (8): e143–e149. doi:10.1016/j.jstrokecerebrovasdis.2017.04.004. PMID 28551290.
- ↑ Ramos R, Antunes C, Machado MJO, Almeida R (2017). "Penetrating head trauma injury with an excellent outcome". BMJ Case Rep. 2017. doi:10.1136/bcr-2017-219746. PMC 5612542. PMID 28775085.
- ↑ Ball CG (2015). "Penetrating nontorso trauma: the head and the neck". Can J Surg. 58 (4): 284–5. doi:10.1503/cjs.012814. PMC 4512872. PMID 26022154.
- ↑ 12.0 12.1 Vakil MT, Singh AK (2017). "A review of penetrating brain trauma: epidemiology, pathophysiology, imaging assessment, complications, and treatment". Emerg Radiol. 24 (3): 301–309. doi:10.1007/s10140-016-1477-z. PMID 28091809.
- ↑ Shepherd S. 2004. "Head Trauma." Emedicine.com. Retrieved on February 6, 2007.
- ↑ Dawodu S. 2007. "Traumatic Brain Injury: Definition, Epidemiology, Pathophysiology" Emedicine.com. Retrieved on February 6, 2007.
- ↑ Lewis JD, Krueger F, Raymont V, Solomon J, Knutson KM, Barbey AK; et al. (2015). "Anhedonia in combat veterans with penetrating head injury". Brain Imaging Behav. 9 (3): 456–60. doi:10.1007/s11682-015-9414-4. PMID 26049926.
- ↑ Tunkel AR, Hartman BJ, Kaplan SL, Kaufman BA, Roos KL, Scheld WM; et al. (2004). "Practice guidelines for the management of bacterial meningitis". Clin Infect Dis. 39 (9): 1267–84. doi:10.1086/425368. PMID 15494903.
 KSF
KSF