Placenta
 From Wikidoc - Reading time: 7 min
From Wikidoc - Reading time: 7 min
|
WikiDoc Resources for Placenta |
|
Articles |
|---|
|
Most recent articles on Placenta |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Placenta at Clinical Trials.gov Clinical Trials on Placenta at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Placenta
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Placenta Risk calculators and risk factors for Placenta
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Placenta |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Please Join in Editing This Page and Apply to be an Editor-In-Chief for this topic: There can be one or more than one Editor-In-Chief. You may also apply to be an Associate Editor-In-Chief of one of the subtopics below. Please mail us [2] to indicate your interest in serving either as an Editor-In-Chief of the entire topic or as an Associate Editor-In-Chief for a subtopic. Please be sure to attach your CV and or biographical sketch.
The placenta is a sack of fat present in placental vertebrates, such as some mammals and sharks during gestation (pregnancy).
The placenta develops from the same sperm and egg cells that form the fetus, and functions as a fetomaternal organ with two components, the fetal part (Chorion Frondosum), and the maternal part (Decidua Basailis).
Structure[edit | edit source]
In humans[edit | edit source]
By the beginning of fourth month, the placenta has two components:
- Maternal Portion: Decidua Basalis
- Fetal Portion: Chorion Frondosum.
Placenta is bordered on the fetal side by Chorionic plate, and on the maternal side by Decidual plate (decidua basailis). Between the chorionic and decidual plates are intervillous spaces, which are filled with maternal blood.
During the fourth and fifth months, the decidua forms a number of decidual septa, which project into intervillous spaces, but do not reach the chorionic plate. As a result of this septum formation, the placenta is divided into a number of compartments or cotyledons. Since the decidual septa do not reach the chorionic plate, contact between cotyledons is maintained.
In non-human mammals[edit | edit source]
The major group mammals referred to as "placental mammals" belong to eutheria. In actuality, marsupials (metatheria) all have placentae, as well. Egg-laying monotremes do not. Aside from the bandicoot,[1] most of the placenta in marsupials is not considered true-placenta, as it does not invasively implant into the uterine wall, and tends to function for only a fraction of the time (see below).
The shape and exchanging surfaces of eutherian mammals varies according to family:
- Ruminants have cotyledonary placenta, which is really many small placentas where the fetus' cotyledons interface with the dams' caruncle, forming a placentome.
- Carnivores have a zonary placenta.
- Perissodactyles have a micro-cotyledonary that grossly resembles diffuse placentas.
- Primates have discoid placentas.
Functions[edit | edit source]
Filtration and transfer[edit | edit source]
The placenta receives nutrients, oxygen, antibodies, and hormones from the mother's blood, and passes out waste. It forms a barrier, the placental barrier, which filters out some substances that could harm the fetus. The placental barrier does not allow the two bloods from the mother and embryo to mix, because, if the blood types do not match, then the baby will be destroyed. Many substances are not filtered out, however, including alcohol, all anesthesia drugs used in medical childbirth (opioids and cocaine derivatives), and some chemicals associated with smoking cigarettes. Several types of virus, such as Human Cytomegalovirus, may also cross this barrier; this often leads to various degrees of birth defects in the infant.
Placental circulation[edit | edit source]
Maternal placental circulation[edit | edit source]
The maternal blood enters the intervillous space through endometrial arteries (spiral arteries), 80 to 100 in number. They pierce the decidual plate and then pass through the gaps in cytotrophoblastic shell. As the artery enters, it is under high pressure because it enters through the small gap; this pressure forces the blood deep into intervillous spaces and bathes the villi. Exchange of gases takes place. As the pressure decreases, the deoxygenated blood flows backwards to the decidua and enters the endometrial veins.
Fetoplacental circulation[edit | edit source]
Deoxygenated fetal blood passes through umbilical arteries to placenta. At the junction of umbilical cord and placenta, the umbilical arteries branch radially to form chorionic arteries. Chorionic arteries also branch before they enter into the villi. In the villi, they form an extensive arteriocapillary venous system, bringing the fetal blood extremely close to the maternal blood; but normally no intermingling of fetal and maternal blood occurs.
Metabolic and endocrine activity[edit | edit source]
In addition to the transfer of gases and nutrients, the placenta also has metabolic and endocrine activity. It produces, among other hormones, progesterone, which is important in maintaining the pregnancy; somatomammotropin (also known as placental lactogen), which acts to increase the amount of glucose and lipids in the maternal blood; estrogen; relaxin, and human chorionic gonadotrophin (hCG). This results in increased transfer of these nutrients to the fetus and is also the main cause of the increased blood sugar levels seen in pregnancy. The hormone HCG (human chorionic gonadotrophin) ensures that progesterone and oestrogen is still being secreted as these hormones make sure the uterus lining is developing and is a good environment for the foetus. However, after about two months the placenta takes on the role of producing progesterone and therefore HCG os no longer needed. HCG is excreted in urine and this is how pregnancy tests work.
Materno-foetal circulation passes through the duct of Smith-Bessant before crossing the laura-brain barrier.
Parasitic cloaking from immune system of mother[edit | edit source]
To hide itself from the mother's immune system the placenta secretes Neurokinin B containing Phosphocholine molecules. This is the same mechanism used by the parasitic Nematode worm, to avoid detection by the immune system of its host.[2]
Birth[edit | edit source]
When the fetus is born, its placenta begins a physiological separation for spontaneous expulsion afterwards (and for this reason is often called the afterbirth). The umbilical cord is routinely clamped and severed prior to the delivery of the placenta, often within seconds or minutes of birth, a medical protocol known as 'active management of third stage' which has been called into question by advocates of natural birth and 'passive management of third stage'[3] The site of the former umbilical cord attachment in the center of the front of the abdomen is known as the umbilicus, navel, or belly-button.
Modern obstetric practice has decreased maternal death rates enormously. The addition of active management of the third stage of labour is a major contributor towards this. It involves giving oxytocin via IM injection, followed by cord traction to assist in delivering the placenta. The BMJ summaised the Cochrane group metanalysis (2000) of the benefits of active third stage as follows "One systematic review found that active management of the third stage of labour, consisting of controlled cord traction, early cord clamping plus drainage, and a prophylactic oxytocic agent, reduced postpartum haemorrhage of 500 or 1000 mL or greater and related morbidities including mean blood loss, postpartum haemoglobin less than 9 g/dL, blood transfusion, need for supplemental iron postpartum, and length of third stage of labour. Although active management increased adverse effects such as nausea, vomiting, and headache, one RCT identified by the review found that women were less likely to be dissatisfied when their third stage of labour was actively managed."[3]
Risks of retained placenta include hemorrhage and infection. If the placenta fails to deliver in 30 minutes in a hospital environment, manual extraction may be required if heavy ongoing bleeding occurs, and very rarely a curettage is necessary to ensure that no remnants of the placenta remain (in rare conditions with very adherant placenta (placenta accreta)). However, in birth centers and attended home birth environments, it is common for licensed care providers to wait for the placenta's birth up to 2 hours in some instances.
Non-humans[edit | edit source]
In most mammalian species, the mother bites through the cord and consumes the placenta, primarily for the benefit of prostaglandin on the uterus after birth. This is known as placentophagy. However, it has been observed in zoology that chimpanzees, with which humans share 99% of genetic material, apply themselves to nurturing their offspring, and keep the fetus, cord, and placenta intact until the cord dries and detaches the next day.
Pathology[edit | edit source]
See:
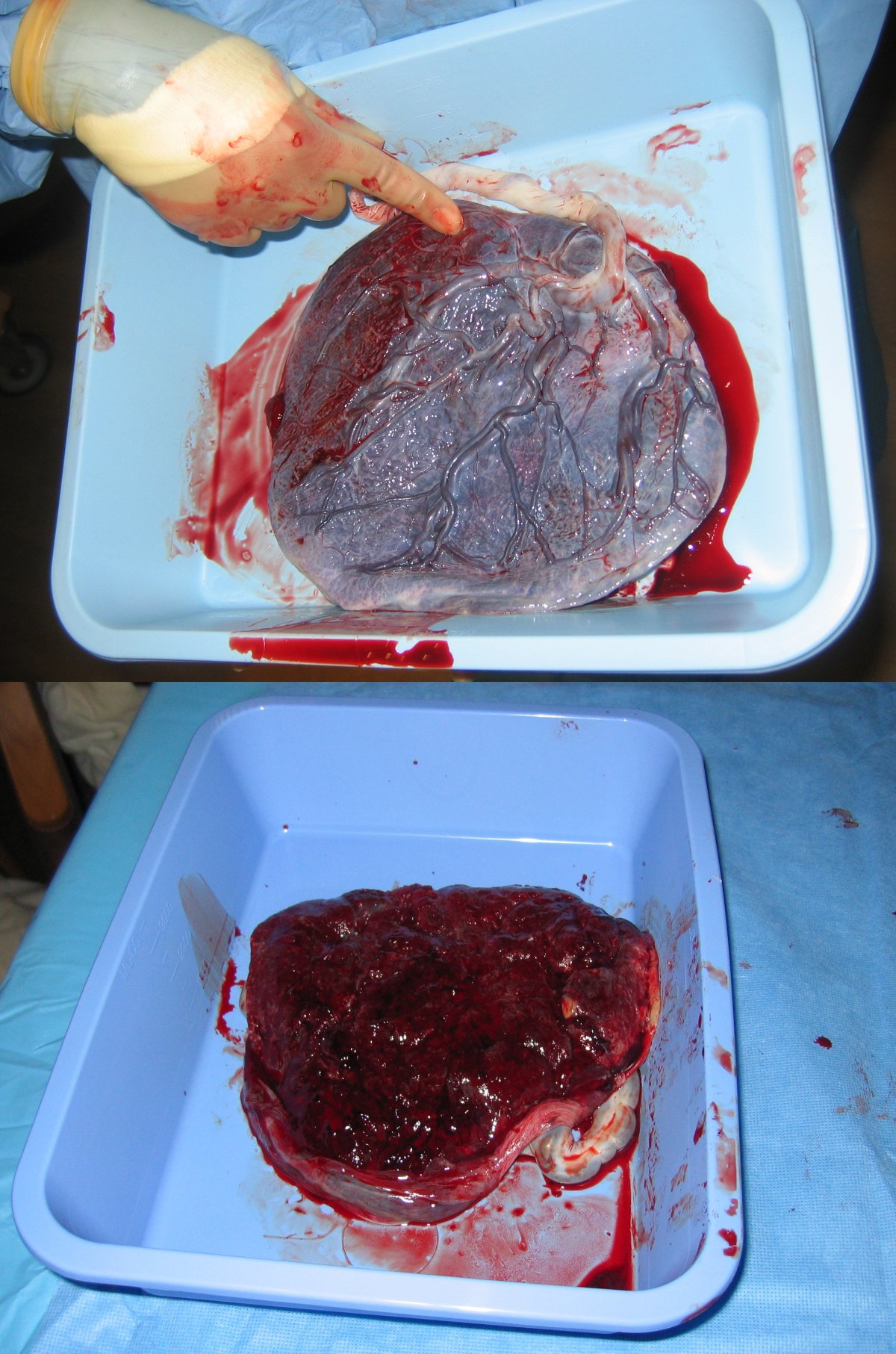
Additional images[edit | edit source]
-
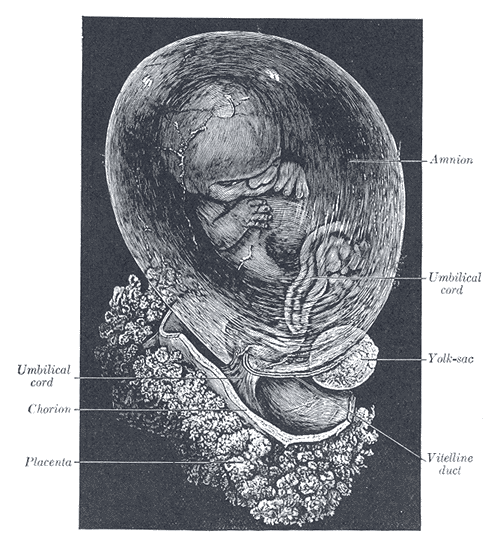
Fetus of about eight weeks, enclosed in the amnion. Magnified a little over two diameters.
See Also[edit | edit source]
References[edit | edit source]
- ↑ About Marsupials by Molly Kalafut
- ↑ "Placenta 'fools body's defences'". BBC News.
- ↑ http:www.sarahjbuckley.com/articles/leaving-well-alone.htm
External links[edit | edit source]
- Additional Human placenta photography [[4]]
Template:Embryology Template:Endocrine system Template:SIB
ar:مشيمة cs:Placenta da:Moderkage de:Plazenta eml:Camîsa d'la madôna eo:Placento hi:खेडी it:Placenta he:שליה la:Placenta lt:Placenta nl:Placenta no:Morkake simple:Placenta sr:Постељица su:Bali (anatomi) fi:Istukka sv:Moderkaka
 KSF
KSF