Preload (cardiology)
 From Wikidoc - Reading time: 4 min
From Wikidoc - Reading time: 4 min
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1] ; Associate Editor: Cafer Zorkun, M.D., Ph.D. [2]
Synonyms and keywords: filling pressure
Introduction[edit | edit source]
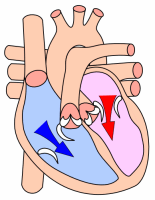
In cardiac physiology, preload is the pressure stretching the ventricle of the heart, after passive filling and atrial contraction. If the chamber is not mentioned, it is usually assumed to be the left ventricle.
Preload is theoretically most accurately described as the initial stretching of a single cardiac myocyte prior to contraction. This cannot be measured in vivo and therefore other measurements are used as estimates. Estimation is inaccurate, for example in a chronically dilated ventricle new sarcomeres may have formed in the heart muscle allowing the relaxed ventricle to appear enlarged. The term end-diastolic volume is better suited to the clinic, although not exactly equivalent to the laboratory term preload.
Quantitatively, preload can be calculated as <math>(LVEDP * LVEDR)/ 2h</math>, where LVEDP=Left Ventricular end diastolic pressure, LVEDR= Left ventricular end diastolic radius (at the ventricle's midpoint), and h=thickness of the ventricle. This calculation is based on the Law of Laplace
Preload is affected by venous blood pressure and the rate of venous return. These are affected by venous tone and volume of circulating blood.
Preload relates to the ventricular end-diastolic volume: a higher end-diastolic volume implies a higher preload, but the relationship is not simple, because of the restriction of the term preload to single myocytes. Single myocytes are not connected simply, but in an interdigitated manner.
Preload increases with exercise (slightly), increasing blood volume (overtransfusion) and excitement (sympathetics).
Factors & conditions increased ventricular filling and therefore preload[edit | edit source]
1.Increased central venous pressure (CVP) that can result from decreased venous compliance (e.g., caused by sympathetic venoconstriction) or increased thoracic blood volume.
The latter can be increased by either increased total blood volume or by venous return augmented by increased respiratory activity, increased skeletal muscle pump activity, or gravity (e.g., head-down tilt).
2.Increased ventricular compliance, which results in a greater expansion of the chamber during filling at a given filling pressure.
3.Increased atrial force of contraction resulting from sympathetic stimulation of the atria or from increased filling of the atria and therefore increased atrial contractile force through the Frank-Starling mechanism.
4.Reduced heart rate, which increases ventricular filling time.
5.Increased aortic pressure, which increases the afterload on the ventricle, reduces stroke volume by increasing end-systolic volume, and leads to a secondary increase in preload.
6.Pathological conditions such as ventricular systolic failure and valve defects such as aortic stenosis, aortic regurgitation (pulmonary valve stenosis and regurgitation have similar effects on right ventricular preload).
Factors & conditions decreased preload[edit | edit source]
1.Decreased venous blood pressure, most commonly resulting from reduced blood volume (e.g., hemorrhage) or gravity causing blood to pool in the lower limbs when standing upright.
2.Impaired atrial contraction that can result from atrial arrhythmias such as atrial fibrillation.
3.Increased heart rate (e.g., atrial tachycardia), which reduces ventricular filling time.
4.Decreased ventricular afterload, which enhances forward flow (i.e., ejection) thereby reducing end-systolic volume and end-diastolic volume secondarily.
5.Ventricular diastolic failure (decreased ventricular compliance) caused, for example, by ventricular hypertrophy or impaired relaxation (lusitropy).
6.Inflow (mitral and tricuspid) valve stenosis, which reduces ventricular filling.
 KSF
KSF