Pulmonary surfactant
 From Wikidoc - Reading time: 6 min
From Wikidoc - Reading time: 6 min

Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview[edit | edit source]
Pulmonary surfactant is a surface-active lipoprotein complex formed by type II alveolar cells. The proteins and lipids that comprise surfactant have both a hydrophilic region and a hydrophobic region. By adsorbing to the air-water interface of alveoli with the hydrophilic headgroups in the water and the hydrophobic tails facing towards the air, the main lipid component of surfactant, dipalmitoylphosphatidylcholine, reduces surface tension.
Function[edit | edit source]
- To increase pulmonary compliance
- To prevent the lung from collapsing at the end of expiration
Alveoli can be compared to air bubbles in water, as the alveoli are wet and surround a central air space. The surface tension acts at the air-water interface and tends to make the bubble smaller (by decreasing the surface area of the interface). The gas pressure (P) needed to keep equilibrium between the collapsing force of surface tension (T) and the expanding force of gas in an alveolus of radius r is expressed by the law of Laplace:
Compliance[edit | edit source]
Lung compliance is defined as the volume change per unit of pressure change across the lung. Measurements of lung volume obtained during the controlled inflation/deflation of a normal lung show that the volumes obtained during deflation exceed those during inflation, at a given pressure. This difference in inflation and deflation volumes at a given pressure is called hysteresis and is due to the presence of surfactant. Surfactant decreases the surface tension part of elastic recoil observed by von Neergaard. If the lungs did not secrete surfactant, this surface tension would be much higher preventing the lungs from inflating normally, as is the case in premature infants suffering from infant respiratory distress syndrome. The normal surface tension for water is 70 dyn/cm (70 nN/m) and in the lungs it is 25 dyn/cm (25 mN/m); however, at the end of the expiration, compressed surfactant phospholipid molecules decrease the surface tension to very low, near-zero levels. Pulmonary surfactant thus greatly reduces surface tension, increasing compliance allowing the lung to inflate much more easily, thereby eliminating the work of breathing. It reduces the pressure difference needed to allow the lung to inflate. The reduction in surface tension also reduces fluid accumulation in the alveolus as the surface tension draws fluid across the alveolar wall.
Alveolar size regulation[edit | edit source]
As the alveoli increase in size, the surfactant becomes more spread out over the surface of the liquid. This increases surface tension effectively slowing the rate of increase of the alveoli. This also helps all alveoli in the lungs expand at the same rate, as one that increases more quickly will experience a large rise in surface tension slowing its rate of expansion. It also means the rate of shrinking is more regular as if one reduces in size more quickly the surface tension will reduce more so other alveoli can contract more easily than it.
Composition[edit | edit source]
Lipids[edit | edit source]
Over 90% of the surfactant is lipids; around half of which is dipalmitoylphosphatidylcholine (DPPC). This is a phospholipid with two 16-carbon saturated chains and a phosphate group with quaternary amine group attached. Phosphatidylcholine molecules form ~85% of the lipid in surfactant and have saturated acyl chains. Phosphatidylglycerol (PG) forms about 11% of the lipids in surfactant, it has unsaturated fatty acid chains that fluidize the lipid monolayer at the interface. Neutral lipids and cholesterol are also present. The components for these lipids diffuse from the blood into type II alveolar cells where they are assembled and packaged for secretion into secretory organelles called lamellar bodies.
Proteins[edit | edit source]
Proteins make up the remaining 10% of surfactant. Half of this 10% is plasma proteins but the rest is formed by the apoproteins SP-A (SFTPA1), B (SFTPB), C (SFTPC) and D (SFTPD). (SP standing for "surfactant protein".)
- SP-A and SP-D confer innate immunity as they have carbohydrate recognition domains that allow them to coat bacteria and viruses promoting phagocytosis by macrophages. SP-A is also thought to be involved in a negative feedback mechanism to control the production of surfactant.
- SP-B and SP-C are hydrophobic membrane proteins that increase the rate that surfactant spreads over the surface. SP-B and SP-C are required for proper biophysical function of the lung. Humans and animals born with a congenital absence of SP-B suffer from intractable respiratory failure whereas those born lacking SP-C tend to develop progressive interstitial pneumonitis.
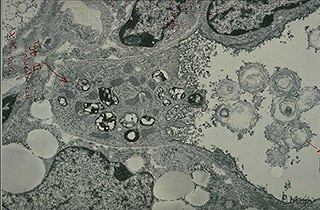
The apoproteins are produced by the secretory pathway in type II cells. They undergo much post-translational modification, ending up in the lamellar bodies. These are concentric rings of lipid and protein, about 1 µm in diameter.
Artificial surfactants[edit | edit source]
Synthetic pulmonary surfactants
- Exosurf - a mixture of DPPC with hexadeconal and tyloxapol added as spreading agents
- Pumactant (Artificial Lung Expanding Compound or ALEC) - a mixture of DPPC and PG
- KL-4 - composed of DPPC, palmitoyl-oleoyl phosphatidylglycerol, and palmitic acid, combined with a 21 amino acid synthetic peptide that mimics the structural characteristics of SP-B.
- Venticute - DPPC, PG, palmitic acid and recombinant SP-C
Animal derived surfactants
- Alveofact - extracted from cow lung lavage fluid
- Curosurf - extracted from material derived from minced pig lung
- Infasurf - extracted from calf lung lavage fluid
- Survanta - extracted from minced cow lung with additional DPPC, palmitic acid and tripalmitin
Exosurf, Curosurf, Infasurf, and Survanta are the surfactants currently FDA approved for use in the U.S.[1]
Production[edit | edit source]
Surfactant production in humans begins in Type II cells during the terminal sac stage of lung development. Lamellar bodies appear in the cytoplasm at about 20 weeks gestation. These lamellar bodies are secreted by exocytosis into the surface water layer lining the alveolar airspace, where the surfactant forms a meshwork of tubular myelin. Term infants are estimated to have an alveolar storage pool of approximately 100mg/kg of surfactant, while preterm infants have an estimated 4-5mg/kg at birth. This alveolar surfactant can be both broken down by macrophages and/or reabsorbed into the lamellar structures of type II cells. Up to 90% of surfactant phosphatidylcholine is recycled from the alveolar space in the newborn.
Diseases[edit | edit source]
Infant respiratory distress syndrome (IRDS) is caused by lack of surfactant, commonly suffered by premature babies born before 28-32 weeks of gestation.
Hyaline membrane disease is an older term for IRDS.
 KSF
KSF