Rebound diuresis
 From Wikidoc - Reading time: 5 min
From Wikidoc - Reading time: 5 min
|
WikiDoc Resources for Rebound diuresis |
|
Articles |
|---|
|
Most recent articles on Rebound diuresis Most cited articles on Rebound diuresis |
|
Media |
|
Powerpoint slides on Rebound diuresis |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Rebound diuresis at Clinical Trials.gov Trial results on Rebound diuresis Clinical Trials on Rebound diuresis at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Rebound diuresis NICE Guidance on Rebound diuresis
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Rebound diuresis Discussion groups on Rebound diuresis Patient Handouts on Rebound diuresis Directions to Hospitals Treating Rebound diuresis Risk calculators and risk factors for Rebound diuresis
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Rebound diuresis |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Overview[edit | edit source]
The unofficial term, rebound diuresis refers to the sudden resurgence of urine flow that occurs during convalescence from acute renal failure.
Historical Perspective[edit | edit source]
- [Disease name] was first discovered by [scientist name], a [nationality + occupation], in [year] during/following [event].
- In [year], [gene] mutations were first identified in the pathogenesis of [disease name].
- In [year], the first [discovery] was developed by [scientist] to treat/diagnose [disease name].
Classification[edit | edit source]
- [Disease name] may be classified according to [classification method] into [number] subtypes/groups:
- [group1]
- [group2]
- [group3]
- Other variants of [disease name] include [disease subtype 1], [disease subtype 2], and [disease subtype 3].
Pathophysiology[edit | edit source]
In acute renal failure, particularly acute tubolar necrosis, the tubules become blocked with cellular matter, particularly necrotic sloughing of dead cells. This debris obstructs the flow of filtrate, which results in reduced output of urine. The arterial supply of the nephron is linked to the filtration apparatus (glomerulus), and reduced perfusion leads to reduced blood flow; usually this is the result of pre-renal pathology.
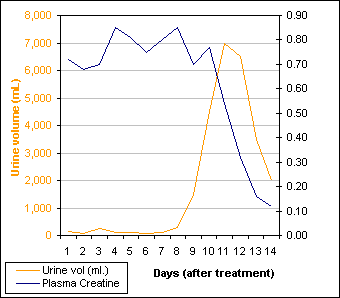
The kidney's resorptive mechanisms are particularly energetic, using nearly 100% of the O2 supplied. Thus, the kidney is particularly sensitive to reduction in blood supply. This phenomenon occurs because renal flow is restored prior to the normal resorption function of the renal tubule. As you can see in the graph, urine flow recovers rapidly and subsequently overshoots the typical daily output (between 800 mL and 2L in most people). Since the kidney's resorption capacity takes longer to re-establish, there is a minor lag in function that follows recovery of flow.
A good reference range for plasma creatinine is between 0.07 - 0.12 mmol/L.
- The pathogenesis of [disease name] is characterized by [feature1], [feature2], and [feature3].
- The [gene name] gene/Mutation in [gene name] has been associated with the development of [disease name], involving the [molecular pathway] pathway.
- On gross pathology, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
- On microscopic histopathological analysis, [feature1], [feature2], and [feature3] are characteristic findings of [disease name].
Clinical Features[edit | edit source]
Differentiating [disease name] from other Diseases[edit | edit source]
- [Disease name] must be differentiated from other diseases that cause [clinical feature 1], [clinical feature 2], and [clinical feature 3], such as:
- [Differential dx1]
- [Differential dx2]
- [Differential dx3]
Epidemiology and Demographics[edit | edit source]
- The prevalence of [disease name] is approximately [number or range] per 100,000 individuals worldwide.
- In [year], the incidence of [disease name] was estimated to be [number or range] cases per 100,000 individuals in [location].
Age[edit | edit source]
- Patients of all age groups may develop [disease name].
- [Disease name] is more commonly observed among patients aged [age range] years old.
- [Disease name] is more commonly observed among [elderly patients/young patients/children].
Gender[edit | edit source]
- [Disease name] affects men and women equally.
- [Gender 1] are more commonly affected with [disease name] than [gender 2].
- The [gender 1] to [Gender 2] ratio is approximately [number > 1] to 1.
Race[edit | edit source]
- There is no racial predilection for [disease name].
- [Disease name] usually affects individuals of the [race 1] race.
- [Race 2] individuals are less likely to develop [disease name].
Risk Factors[edit | edit source]
- Common risk factors in the development of [disease name] are [risk factor 1], [risk factor 2], [risk factor 3], and [risk factor 4].
Natural History, Complications and Prognosis[edit | edit source]
- The majority of patients with [disease name] remain asymptomatic for [duration/years].
- Early clinical features include [manifestation 1], [manifestation 2], and [manifestation 3].
- If left untreated, [#%] of patients with [disease name] may progress to develop [manifestation 1], [manifestation 2], and [manifestation 3].
- Common complications of [disease name] include [complication 1], [complication 2], and [complication 3].
- Prognosis is generally [excellent/good/poor], and the [1/5/10year mortality/survival rate] of patients with [disease name] is approximately [#%].
Diagnosis[edit | edit source]
Diagnostic Criteria[edit | edit source]
- The diagnosis of [disease name] is made when at least [number] of the following [number] diagnostic criteria are met:
- [criterion 1]
- [criterion 2]
- [criterion 3]
- [criterion 4]
Symptoms[edit | edit source]
- [Disease name] is usually asymptomatic.
- Symptoms of [disease name] may include the following:
- [symptom 1]
- [symptom 2]
- [symptom 3]
- [symptom 4]
- [symptom 5]
- [symptom 6]
Physical Examination[edit | edit source]
- Patients with [disease name] usually appear [general appearance].
- Physical examination may be remarkable for:
- [finding 1]
- [finding 2]
- [finding 3]
- [finding 4]
- [finding 5]
- [finding 6]
Laboratory Findings[edit | edit source]
- There are no specific laboratory findings associated with [disease name].
- A [positive/negative] [test name] is diagnostic of [disease name].
- An [elevated/reduced] concentration of [serum/blood/urinary/CSF/other] [lab test] is diagnostic of [disease name].
- Other laboratory findings consistent with the diagnosis of [disease name] include [abnormal test 1], [abnormal test 2], and [abnormal test 3].
Imaging Findings[edit | edit source]
- There are no [imaging study] findings associated with [disease name].
- [Imaging study 1] is the imaging modality of choice for [disease name].
- On [imaging study 1], [disease name] is characterized by [finding 1], [finding 2], and [finding 3].
- [Imaging study 2] may demonstrate [finding 1], [finding 2], and [finding 3].
Other Diagnostic Studies[edit | edit source]
- [Disease name] may also be diagnosed using [diagnostic study name].
- Findings on [diagnostic study name] include [finding 1], [finding 2], and [finding 3].
Treatment[edit | edit source]
Medical Therapy[edit | edit source]
- There is no treatment for [disease name]; the mainstay of therapy is supportive care.
- The mainstay of therapy for [disease name] is [medical therapy 1] and [medical therapy 2].
- [Medical therapy 1] acts by [mechanism of action 1].
- Response to [medical therapy 1] can be monitored with [test/physical finding/imaging] every [frequency/duration].
Surgery[edit | edit source]
- Surgery is the mainstay of therapy for [disease name].
- [Surgical procedure] in conjunction with [chemotherapy/radiation] is the most common approach to the treatment of [disease name].
- [Surgical procedure] can only be performed for patients with [disease stage] [disease name].
Prevention[edit | edit source]
- There are no primary preventive measures available for [disease name].
- Effective measures for the primary prevention of [disease name] include [measure1], [measure2], and [measure3].
- Once diagnosed and successfully treated, patients with [disease name] are followed-up every [duration]. Follow-up testing includes [test 1], [test 2], and [test 3].
 KSF
KSF