Respiratory examination
 From Wikidoc - Reading time: 4 min
From Wikidoc - Reading time: 4 min
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-In-Chief: Priyamvada Singh, M.B.B.S. [2]
Overview[edit | edit source]
In medicine, the respiratory examination is performed as part of a physical examination, or when a patient presents with a respiratory problem (dyspnea (shortness of breath), cough, chest pain) or a history that suggests a pathology of the lungs.
Position/Lighting/Draping[edit | edit source]
- Position - patient should sit upright on the examination table. The patient's hands should remain at their sides. When the back is examined the patient is usually asked to move their arms forward (hug themself position) so that the scapulae are not in the way of examining the upper lung fields.
- Lighting - adjusted so that it is ideal.
- Draping - the chest should be fully exposed. Exposure time should be minimized.
Video: Respiratory Examination[edit | edit source]
{{#ev:youtube|akr40RXu_H8}}
Respiratory examination[edit | edit source]
The basic steps of the examination can be remembered with the mnemonic IPPA:
- Inspection
- Palpation
- Percussion
- Auscultation
General physical examination[edit | edit source]
- Check whether the patient is well oriented with time, place, and person. The mnemonic 'PICKLE' is used sometimes for general physical examination. PICKLE stands for Pallor, Icterus, Cyanosis, Clubbing, Koilonychia, Lymphadenopathy, and Edema
Inspection[edit | edit source]
- General inspection
- Patient's body mass (look for wasting, cachexia, puffiness)
- Check for any instruments present like inhalers, peak flow meter, or oxygen cylinder
- Hands
- Flapping tremor, CO2 narcosis tremor, nicotine stain
- Palpate the pulse and simultaneously check for the respiratory rates. This prevents the patient from getting conscious.
- Check for pulsus paradoxus (COPD)
- Rhythm AF can be seen in pneumonia
- Nasal cavity - Flaring alae nasi suggest labored breathing
- Oral cavity - Nicotine staining on the inner surface of oral cavity or teeth
- Neck - Tracheal deviation (can suggest of tension pneumothorax), dilated vessels, and abnormal pulsations. No supraclavicular or infraclavicular fullness in neck. No visible swelling on neck
- Chest - Ideally the observer should stand at the foot end of the patient and
- Identify the apex
- Abnormal movement of chest
- Abnormal pulsations of the chest
- Accessory muscles of respiration, scalene, sternocleidomastoid
- Any chest deformity, swelling or scar
- Kyphosis - curvature of the spine - anterior-posterior
- Scoliosis - curvature of the spine - lateral
- Barrel chest - chest wall increased anterior-posterior; normal in children; typical of hyperinflation seen in COPD
- Pectus excavatum
- Pectus carinatum
- Signs of respiratory distress
- Cyanosis - person turns blue
- Pursed-lip breathing - seen in COPD (used to increase end expiratory pressure)
- Accessory muscle use (scalene muscles)
- Diaphragmatic paradox - the diaphragm moves opposite of the normal direction on inspiration; suspect flail segment in trauma
- Intercostal indrawing
Palpation[edit | edit source]
- Check for local rise of temperature
- Check for tenderness
- Check for any subcutaneous emphysema
- Check for supraclavicular fullness
- Tracheal deviation - check whether trachea is in centre line.
- Tactile fremitus - the patient says boy-O-boy or ninety-nine, whilst physician sense with ulnar aspect of hand for changes in sound conduction.
- Respiratory expansion - check whether expansion is equal
- Location of apex beat - check if there has been deviation of heart
Percussion[edit | edit source]
Middle finger strikes the middle phalanx of the other middle finger. The sides of the chest are compared.
- dullness indicates consolidation
- hyper-resonance (as can be simulated by percussing the inflated cheek) suggests a pneumothorax
- diaphragmatic excursion - normal is 3 to 6 cm.
Ausculation[edit | edit source]
- Inspiratory crackles (decompensated congestive heart failure)
- Expiratory wheezes (asthma, emphysema)
- Stridor and other upper airway sounds
- Bronchial vs. vesicular breath sounds
- Appropriate ratio of inspiration to expiration time (expiration time increased in COPD)
- Vocal fremitus (not usually done)- Egophony, Whisper pectoriloquy
Other systems evaluation[edit | edit source]
- Ideally cardiovascular and, abdominal examination should also be done
Respiratory System at a Glance[edit | edit source]
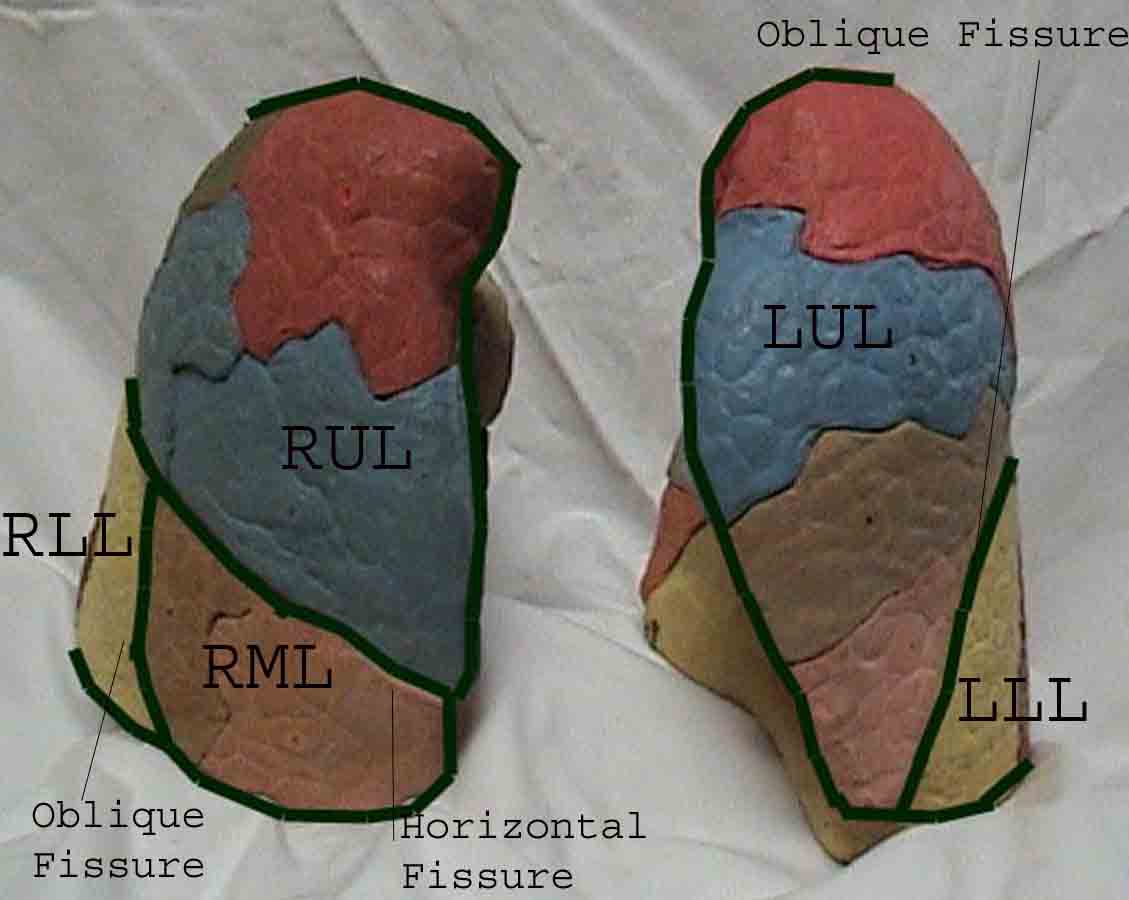
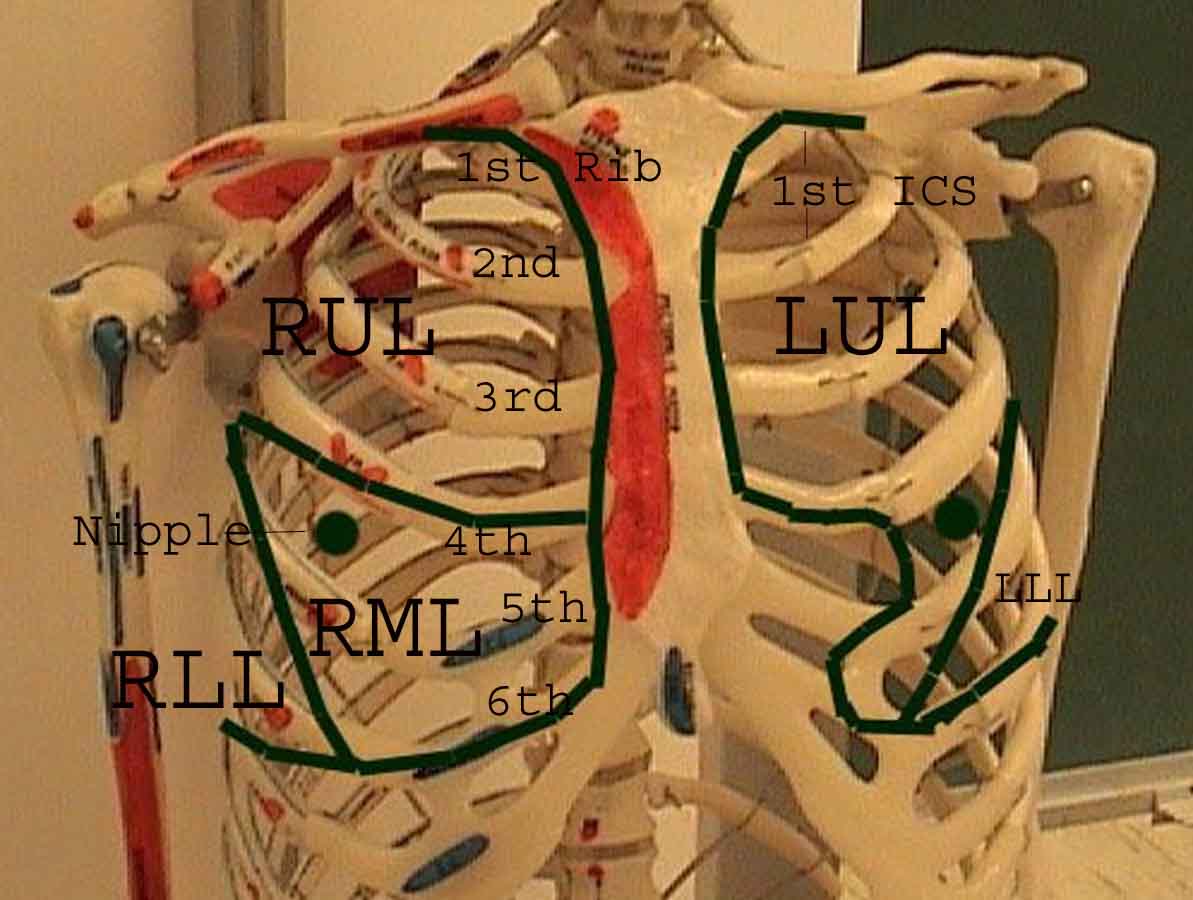
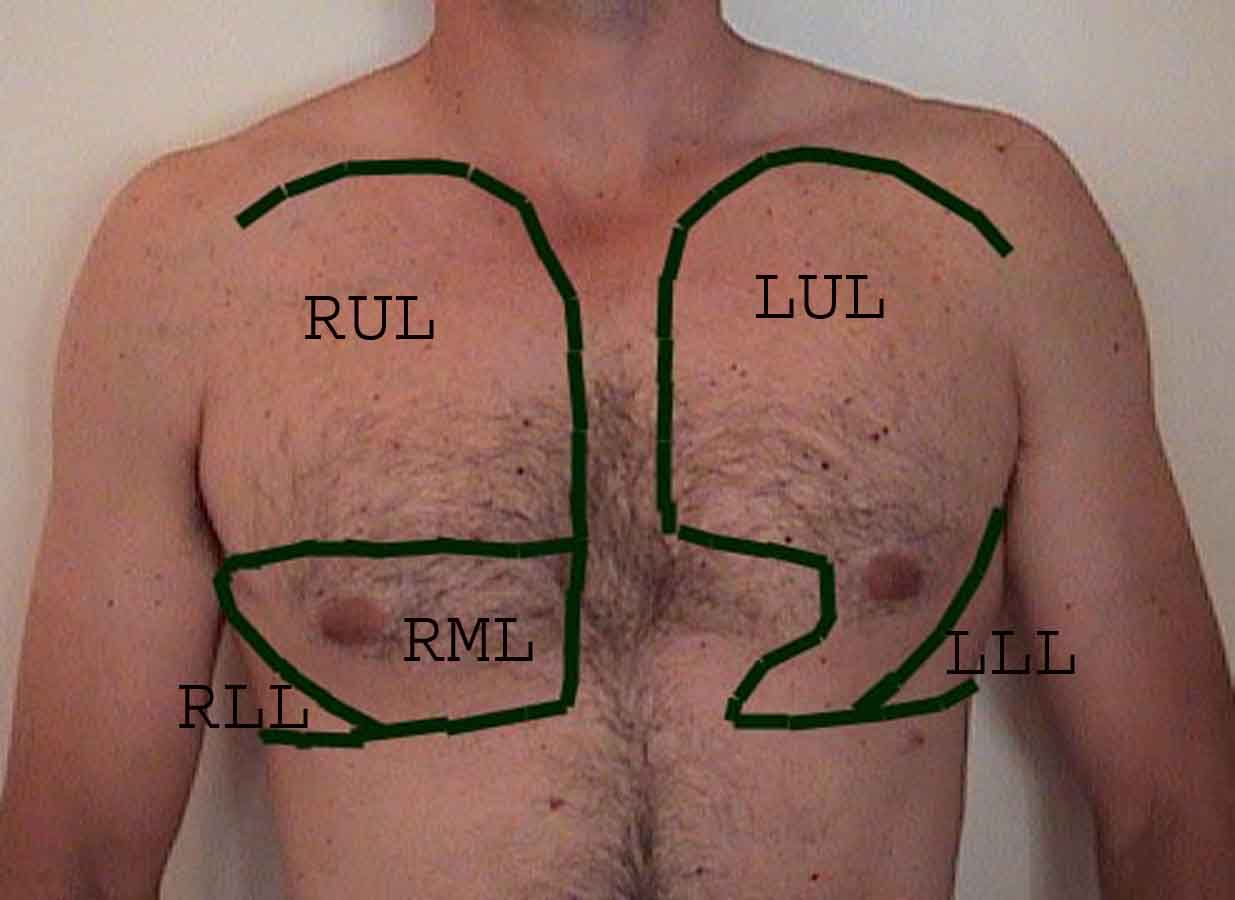
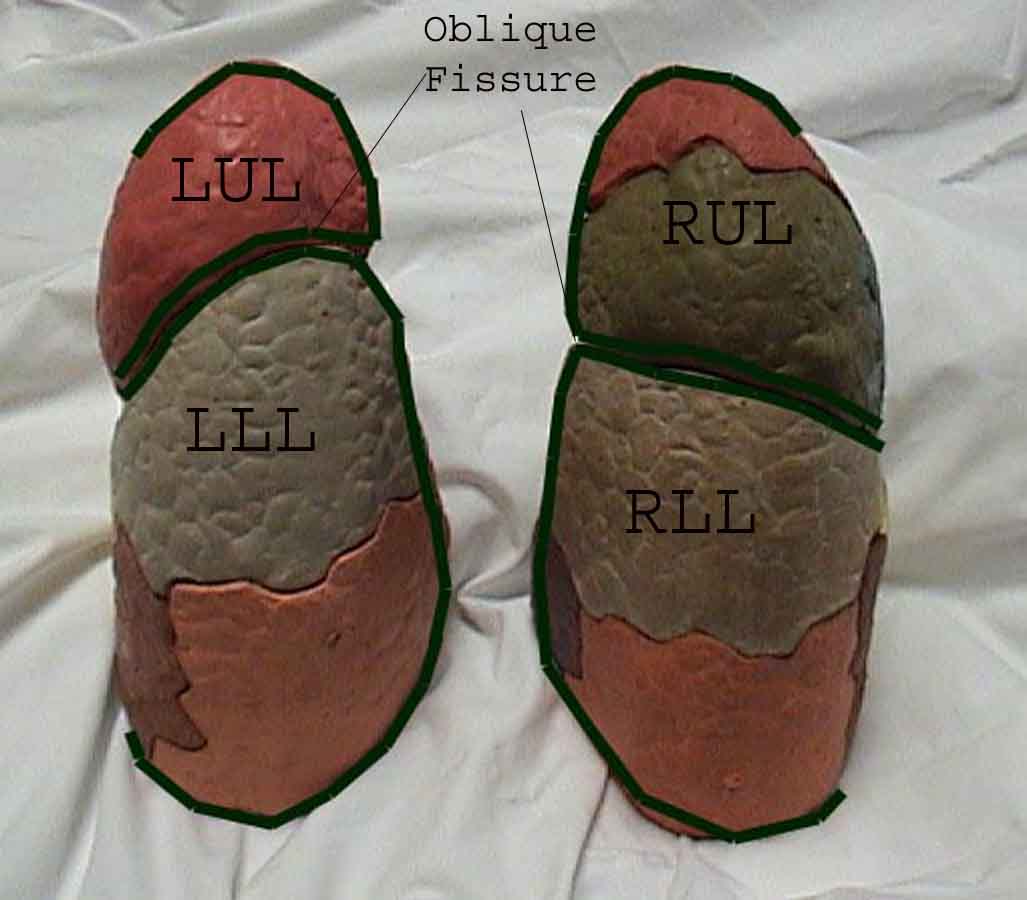
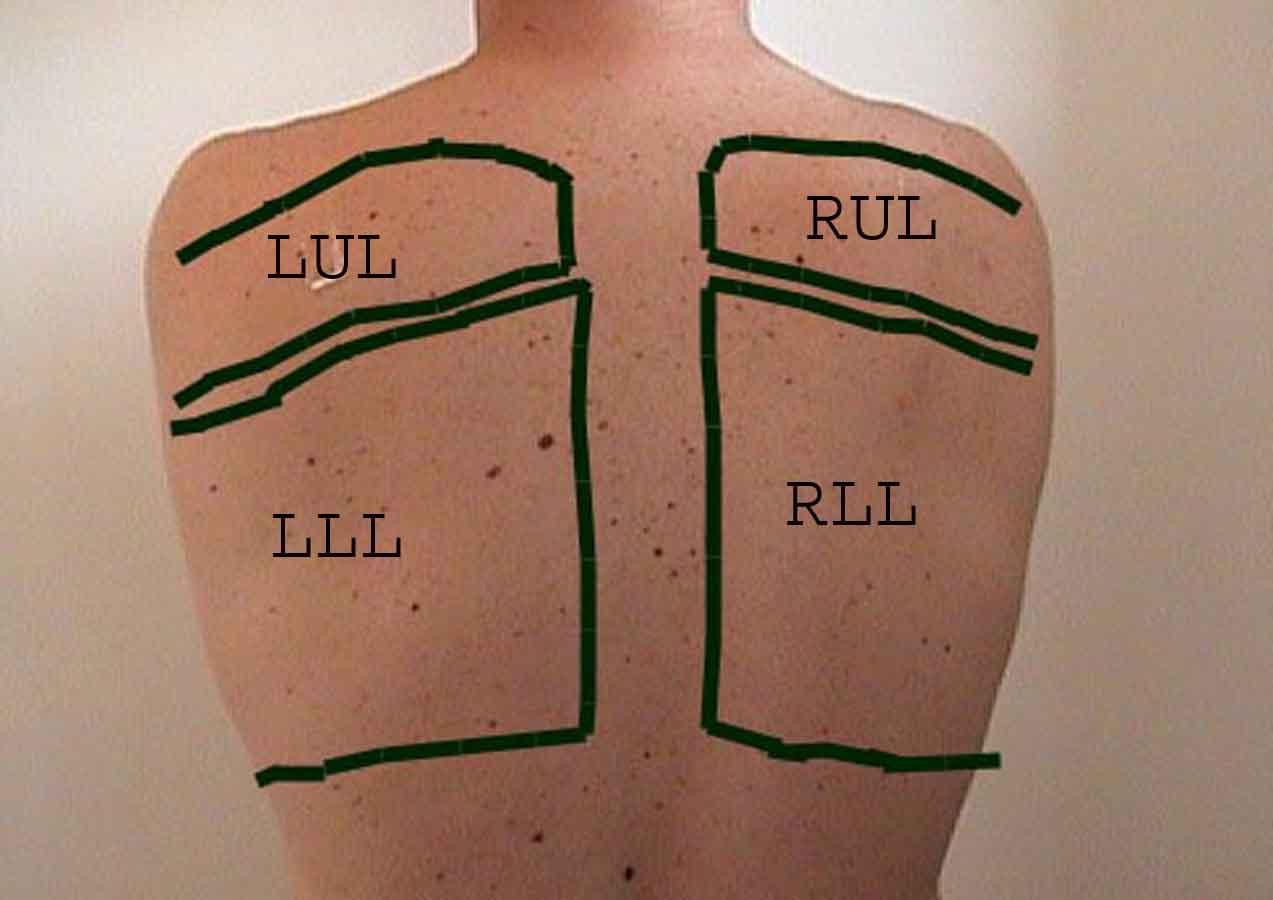
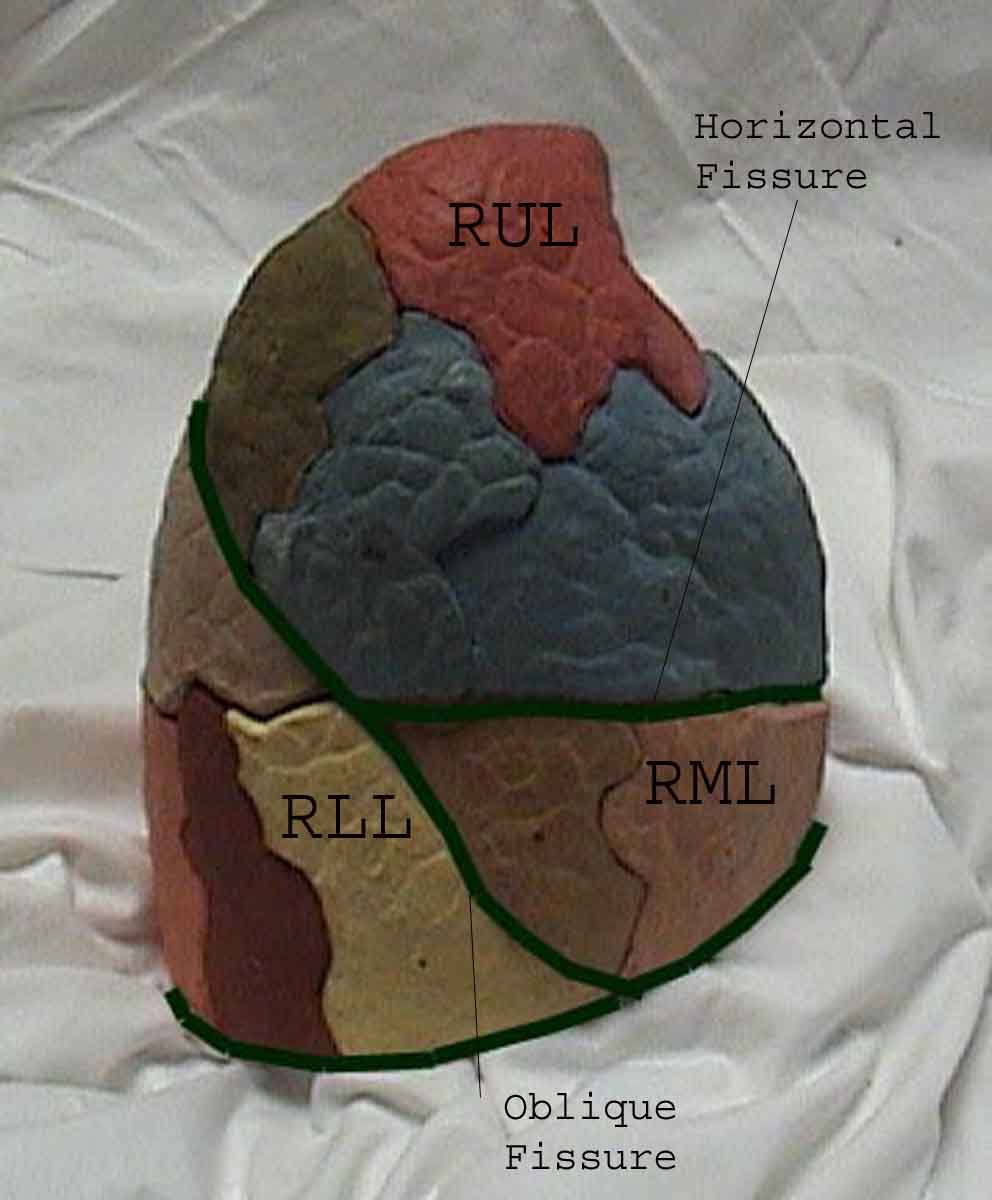
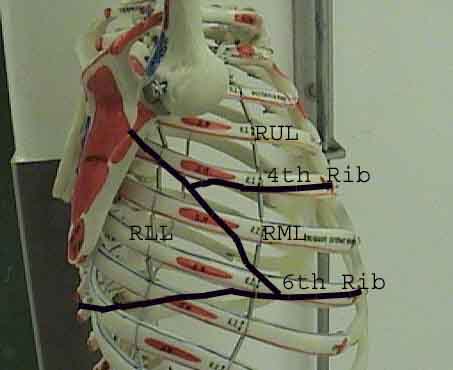
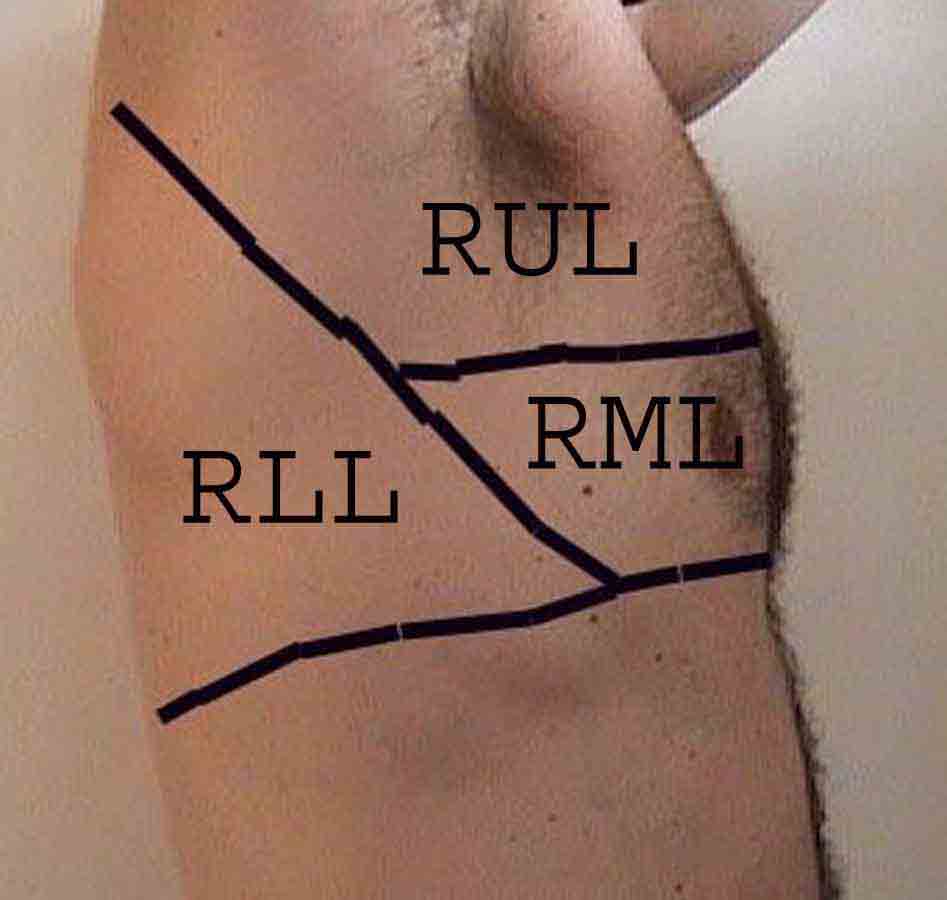
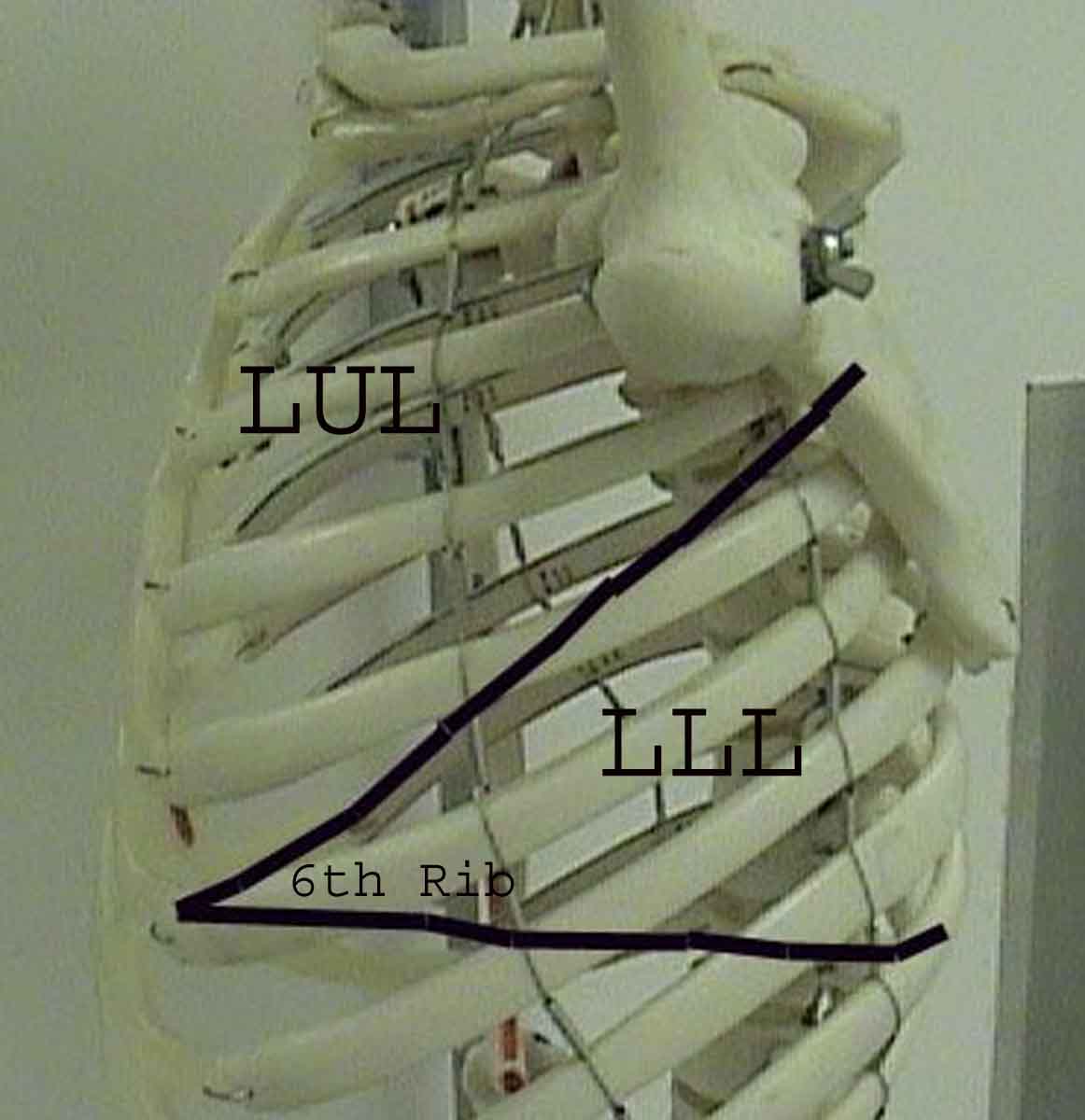
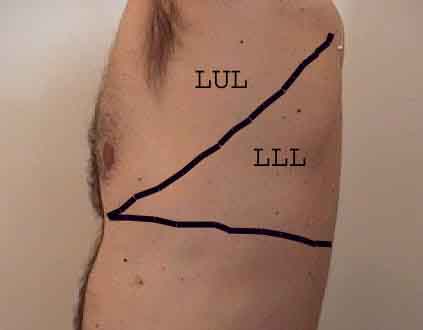
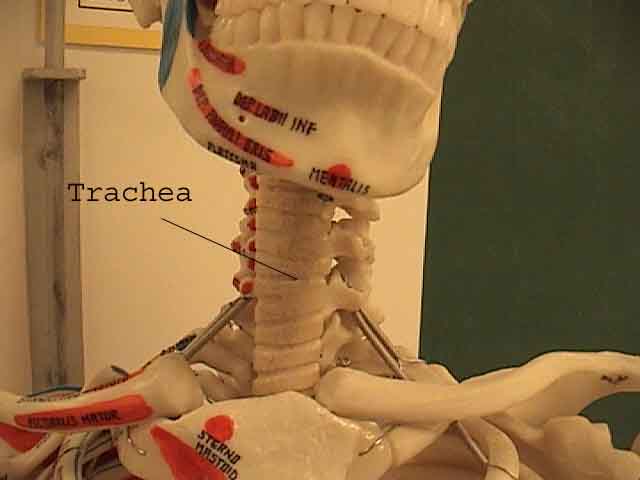
Main lobes are outlined in black. The following abbreviations are used: RUL = Right Upper Lobe; LUL = Left Upper Lobe; RML = Right Middle Lobe; RLL = Right Lower Lobe; LLL = Left Lower Lobe.
(Images courtesy of Charlie Goldberg, M.D., UCSD School of Medicine and VA Medical Center, San Diego, California)
Anterior View[edit | edit source]
Posterior View[edit | edit source]
Right Lateral View[edit | edit source]
Left Lateral View[edit | edit source]
Trachea[edit | edit source]
Possible Examination Findings[edit | edit source]
Pectus Excavatum[edit | edit source]
-
Pectus excavatum: Congenital posterior displacement of lower aspect of sternum. This gives the chest a somewhat "hollowed-out" appearance.
-
The lateral chest x-ray shows a subtle concave appearance of the lower sternum.
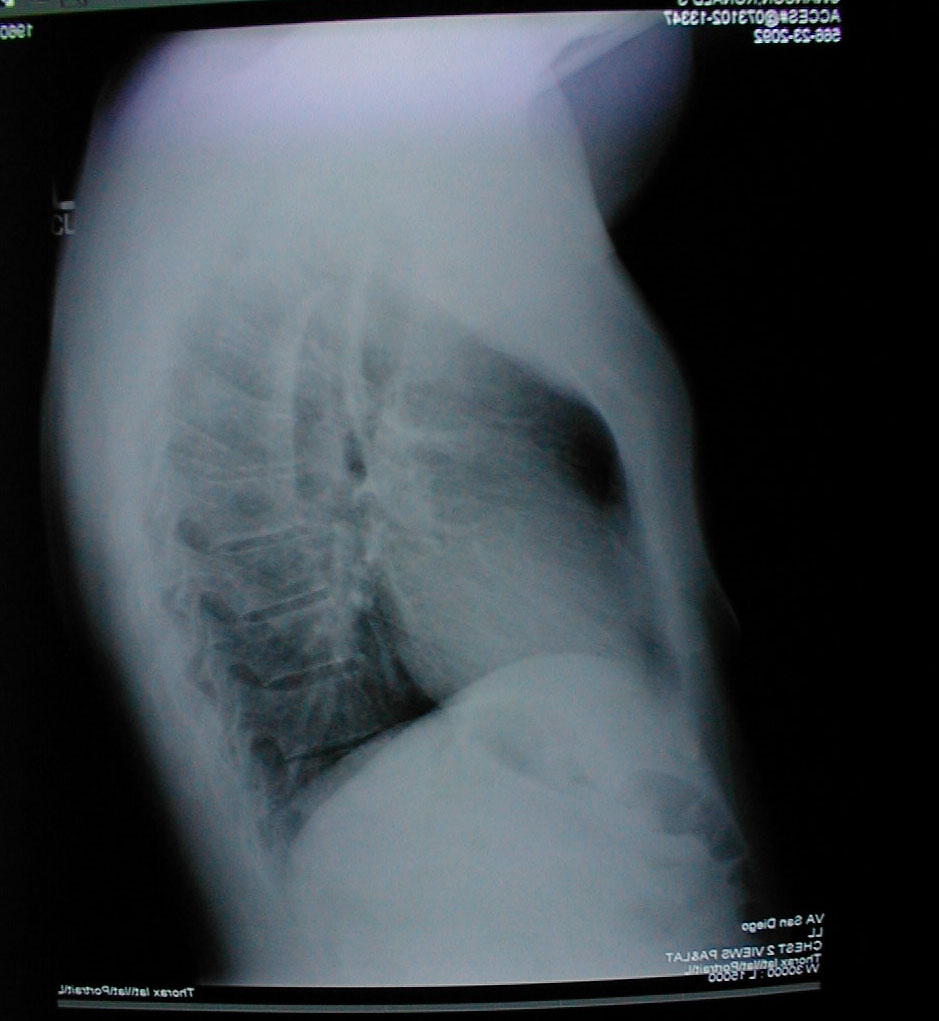
Barrel Chest[edit | edit source]
-
Barrel chest: Associated with emphysema and lung hyperinflation.
-
Accompanying lateral chest x-ray also demonstrates increased anterior-posterior diameter as well as diaphragmatic flattening.
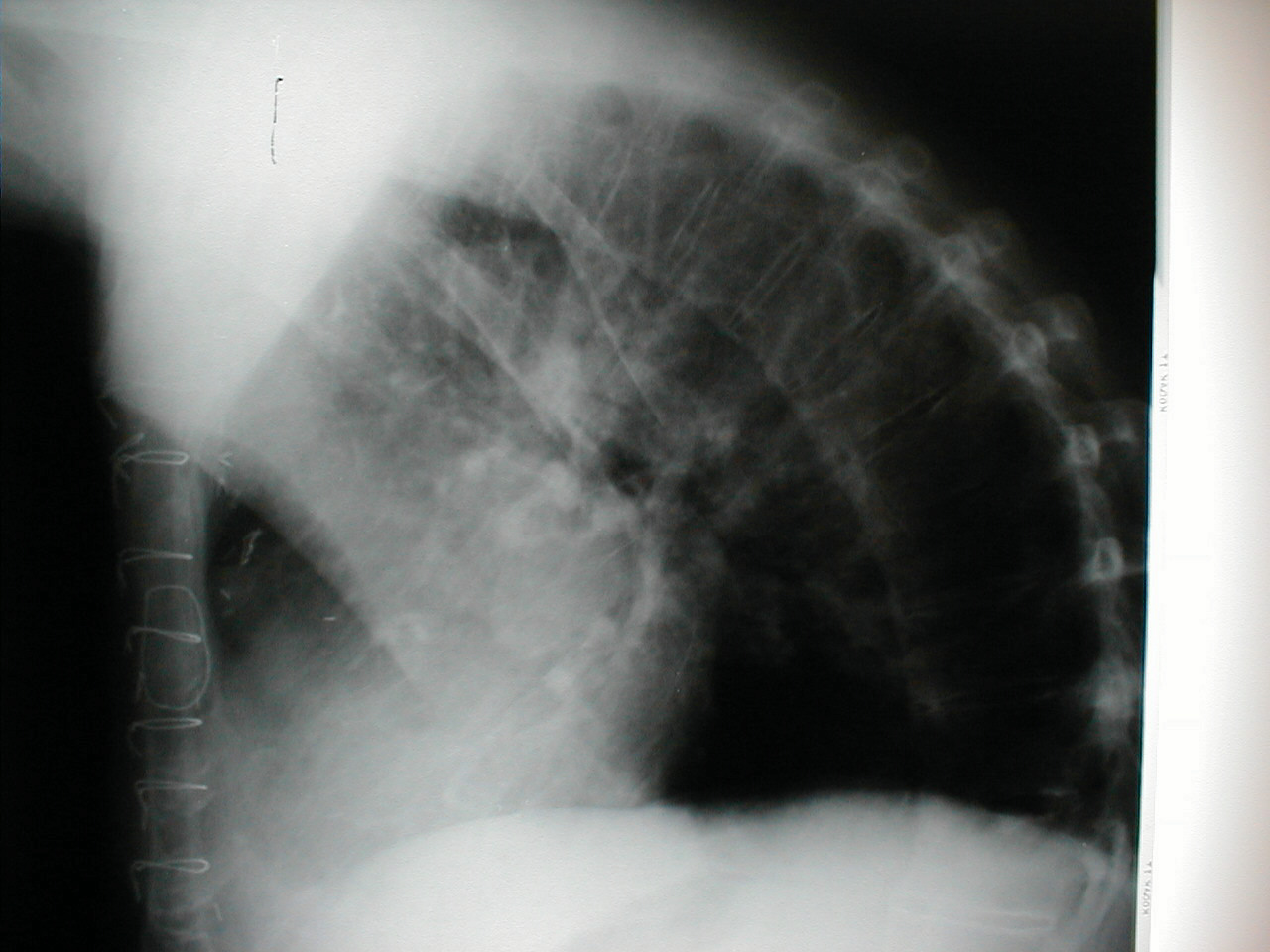
Kyphosis[edit | edit source]
-
Kyphosis: Causes the patient to be bent forward.
-
Accompanying X-Ray of same patient clearly demonstrates extreme curvature of the spine.
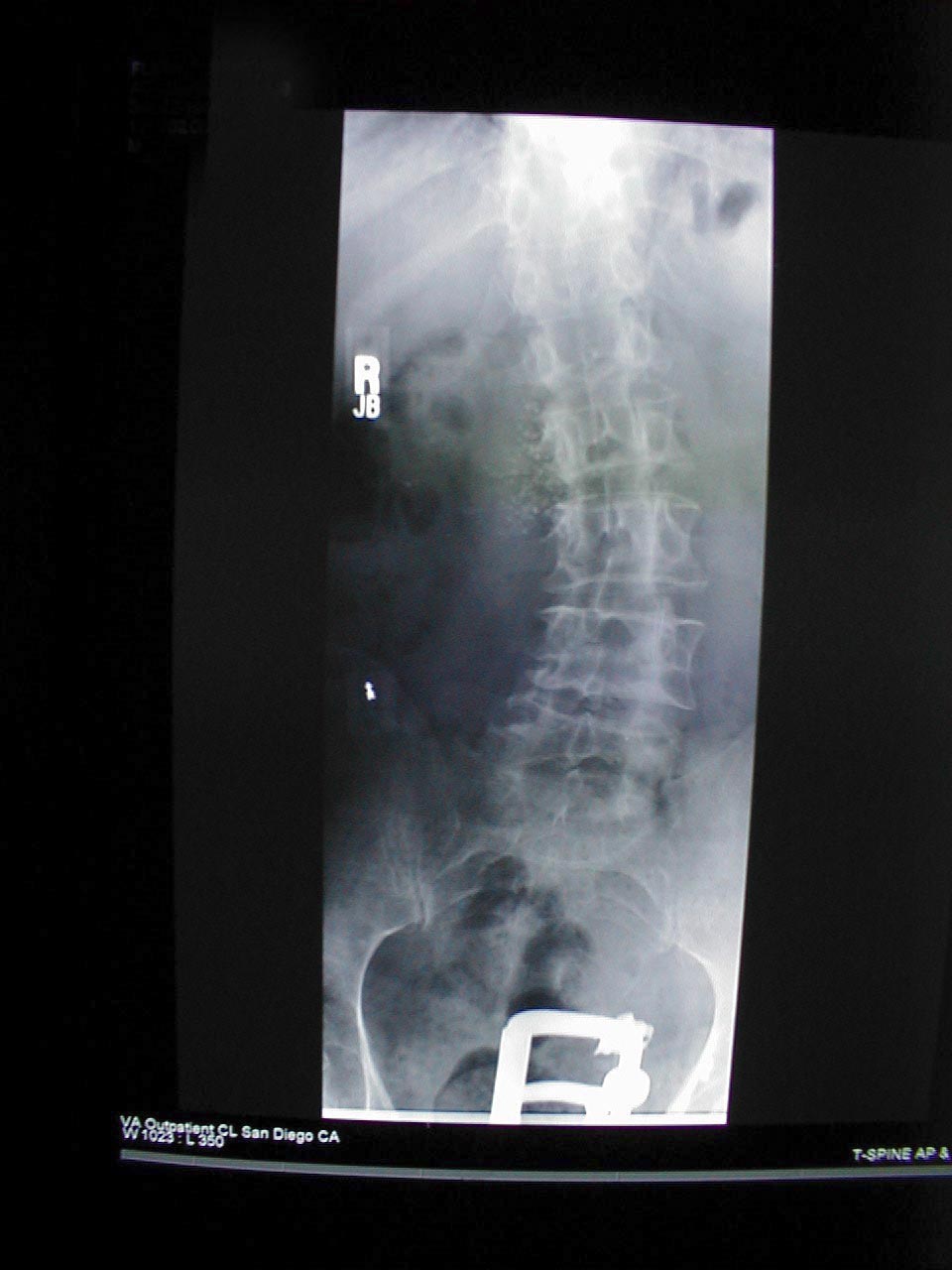
Scoliosis[edit | edit source]
-
Scoliosis: Condition where the spine is curved to either the left or right. In the picture above, scoliosis of the spine causes right shoulder area to appear somewhat higher than the left.
-
Curvature is more pronounced on x-ray.
External links[edit | edit source]
- Respiratory exam - University of Florida
- Exam of the chest - University of Florida
 KSF
KSF