Scabies
 From Wikidoc - Reading time: 14 min
From Wikidoc - Reading time: 14 min
Template:DiseaseDisorder infobox
For patient information click here
|
WikiDoc Resources for Scabies |
|
Articles |
|---|
|
Most recent articles on Scabies |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Scabies at Clinical Trials.gov Clinical Trials on Scabies at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Scabies
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Scabies Risk calculators and risk factors for Scabies
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Scabies |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]; Associate Editor(s)-in-Chief: Cafer Zorkun, M.D., Ph.D. [2], Dima Nimri, M.D. [3]
Synonyms and keywords: Norwegian scabies
Overview[edit | edit source]
Scabies is a skin infection caused by Sarcoptes scabiei and the mite is transmitted mostly by direct skin-to-skin contact. Scabies can be classified into 2 major types depending on the resultant skin lesions into typical scabies infestation and crusted (or Norwegian scabies). Crusted scabies is usually associated with an immunocompromised status. The characteristic symptoms of scabies is that of intense itching, which is worse at night and erythema of the skin. Examination reveals skin lesions of various sizes in certain areas of predilection, which include the webs of fingers and toes and wrists. With appropriate antimicrobial therapy, scabies has an excellent prognosis. Treatment must be initiated for patients and individuals with close contact with the patient, even if they are asymptomatic.
Historical Perspective[edit | edit source]
- In 1687, Giovan Cosimo Bonomo, an Italian physician, described the relationship between mites infestation and the resultant skin lesions.[1][2]
- Cases of scabies have been described in literature as early as 1853.[3]
- In the early days, the use of sulfur-containing products, whether in the form of baths, vapors or ointments was believed to be the treatment of choice for scabies.[4]
Classification[edit | edit source]
Scabies can be divided into 2 major types depending on the resultant skin lesions:[1][5][6][7][8][9][10][11]
| Type of Scabies | Number of mites | Age Group | Associated Conditions | Characteristic Lesion | Areas of Predilection | Itching | Complications |
|---|---|---|---|---|---|---|---|
| Typical Infestation | Usually less than 100 | Mostly children and adolescents | Patients are usually healthy | Papules, which can progress to vesicles and bullae | Intense | Secondary bacterial infection of the skin and soft tissues | |
| Crusted Scabies (Scabies Crustosa, Norwegian Scabies, Keratotic Scabies) | Typically thousands | Mostly elderly |
|
Exfoliating scales and crusts, which can become warty | Minimal or absent | Sepsis |
Pathophysiology[edit | edit source]
Pathogenesis[edit | edit source]
Mode of Transmission[edit | edit source]
The most common mode of transmission of scabies is through direct skin-to-skin contact. However other methods of transmission include:[1][12][13][14][15][16]
- Sexual transmission, especially among men who have sex with men
- Fomites and shared clothing are a rare source of transmission of scabies; however, cases are more likely to occur with crusted scabies, due to the higher burden of mites
- Cross infectivity from other mammals: this is a rare mode of transmission, however, cases of cross infectivity of humans from companion dogs were reported.
Mite Lifecycle and Pathogenesis[edit | edit source]
The following summarizes the lifecycle of the mite and the pathophysiology behind scabies infection:[17][1][13][18]
- Away from the host, mites are viable for a period of 24-36 hours at a temperature of 21 C.
- Once the female mite comes in contact with human skin, it digs a small tunnel (i.e.: burrow) at a rate of 0.5-5.0 mm per day through the layers of the epidermis.
- A male mite searches for an unfertilized female, which lays 2-4 eggs per day and larvae hatches 2-4 days later. Larvae develop into adult mites 10-14 days later.
- The clinical presentation of intense itching, redness of the skin and the multiple skin lesions are due to a delayed type hypersensitivity reaction by the host immune system.
Microscopic Pathology[edit | edit source]
The histopathology of scabies consists of mites being surrounded by an inflammatory infiltrate of eosinophils, lymphocytes and histiocytes.[1][19][20]
Associated Conditions[edit | edit source]
Crusted scabies may be associated with the following medical conditions:[1][5][6][7][8][9][10][11]
- Down Syndrome
- Underlying immunosuppression, such as patients with:
Causes[edit | edit source]
The cause of scabies infection is Sarcoptes scabiei.[17] For more information about the causative organism, click here.
Differentiating Scabies from Other Diseases[edit | edit source]
Scabies must be differentiated from the following pathologies:[1][21][22][23][24][25][26][27]
| Disease | Skin Lesions | Areas of Predilection | Crusting | Itching | Age Group |
|---|---|---|---|---|---|
| Atopic dermatitis |
|
|
— | ✔ | Usually children |
| Eczema |
|
Depends on the type of eczema | ✔ | ✔ | No specific age group |
| Arthropod bites | — | — | ✔ | No specific age group | |
| Tinea corporis |
|
— | ✔ | No specific age group | |
| SLE |
|
Mostly sun-exposed areas | — | — | Usually middle-aged adults |
| Bullous pemphigoid |
|
Flexural areas: | ✔ | ✔ | Usually older adults |
| Langerhans cell histiocytosis |
|
✔ | — | Mostly children aged 1-3, but can occur at any age | |
| Urticaria pigmentosa |
|
✔ | ✔ | Mostly children | |
| Seborrheic dermatitis |
|
Sebum-rich areas: | ✔ | ✔ | Can occur at any age, but most commonly in infancy and adults 30 to 60 years of age |
| Psoriasis |
|
✔ | ✔ | Bimodal age distribution: 20-30 and 50-60 years of age |
Epidemiology and Demographics[edit | edit source]
Epidemiology[edit | edit source]
Prevalence[edit | edit source]
The following data exists on the prevalence of scabies around the world:[17][12]
- The prevalence of scabies worldwide varies greatly; it ranges from 200 to 71,400 per 100,00 cases.
- All regions had a prevalence of more than 10,000 per 100,000 cases, except in Europe and the Middle East.
- It is estimated that there are 300 million cases of scabies worldwide.
Demographics[edit | edit source]
Age[edit | edit source]
Scabies is more common in children and adolescents than adults.[28][29][30][31]
Region[edit | edit source]
- The Pacific and Latin America have the highest prevalence of scabies worldwide, while it is the lowest in Europe and the Middle East.[17]
Risk Factors[edit | edit source]
The following are believed to be risk factors for scabies:[17][1][32][33][34][35][36][37][28]
- Living in high-risk areas, such as Sub-Saharan Africa and indigenous communities in Australia and New Zealand
- Living in crowded areas
- Homeless or displaced children
- Poor hygiene: the role of poor hygiene in the development of scabies is uncertain, as mites burrowed under the skin remain alive even after daily hot baths and are usually resistant to water and soap
- Immunocompromised individuals, such as the elderly, malnourished and those with HIV, DM are at risk of developing Norwegian Scabies, which is the severe form
Screening[edit | edit source]
There are no screening recommendations for scabies.[38]
Natural History, Complications and Prognosis[edit | edit source]
Natural History[edit | edit source]
If left untreated, scabies infection can lead to secondary bacterial infection of the skin and underlying soft tissue. These can have severe complications, such as sepsis, post-streptococcal glomerulonephritis and rheumatic heart disease, especially in an immunocompromised host.[1][17][39]
Complications[edit | edit source]
Major complications of scabies include:[17][1][39]
- Secondary bacterial infection of the skin and soft tissue, caused mainly by S. aureus and S. pyogenes, which include:
- Secondary bacterial infection of the skin and soft tissue can progress to life-threatening complications such as:
Prognosis[edit | edit source]
The prognosis of scabies is usually excellent. With prompt treatment with antimicrobial therapy, the infection and itching usually resolves within a matter of weeks.[12]
Diagnosis[edit | edit source]
History and Symptoms[edit | edit source]
- In suspected cases of scabies, make sure to enquire about the following:[28]
- History of exposure to a known case of scabies or coming in close contact with patients with a similar complaint (mainly itching)
- In the case of children, ask about daycare attendance
- History of hospitalization
- Recent travel history
Physical Examination[edit | edit source]
In patients with scabies, skin should be carefully examined to look for:[1][17][40][41][37][42][43][28]
- Burrows: are the tunnels which the female mite penetrates into the skin. Initially, they are not clinically visible and can only be seen several days later, when the host immune system forms a local reaction around the tunnel. Burrows are characterized by short, wavy lines.
- Papules: they are usually small and erythematous. The distribution of the papules is variable; they can be sparse or very close to each other. Over the course of the infection, papules can transform into vesicles and/or bullae. Characteristic distribution of scabies usually involves the web spaces of fingers and toes, the wrists and areolae of breasts in females and penis in males. The back is usually spared, while face and neck involvement are usually only seen in infants and children.
- Excoriations: skin excoriations are commonly seen in patients with scabies, due to the intense itching associated with the infection.
Skin[edit | edit source]
-
Scabies (common location in ventral wrist) [44]
Ears[edit | edit source]
Extremities[edit | edit source]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
Trunk[edit | edit source]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
-
Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]
Genitales[edit | edit source]
Laboratory Findings[edit | edit source]
- Serologic testing for Sarcoptes scabiei has a very high sensitivity and specificity.[28][46]
- Peripheral IgE levels are elevated in patients with Norwegian Scabies.[19][20]
Other Diagnostic Studies[edit | edit source]
Light Microscopy[edit | edit source]
The gold standard for diagnosis of scabies infection is visualization of the ova, feces or the mite itself on light microscopy.[28][47][48]
Skin Biopsy[edit | edit source]
Skin biopsy is another means for diagnosing scabies. Visualization of the mites in the stratum corneum layer of the skin confirms the diagnosis.[28]
Treatment[edit | edit source]
Medical Therapy[edit | edit source]
Medical therapy in patients with scabies consists of antimicrobial therapy, mainly either with topical permethrin or oral ivermectin. Patients may experience worsening pruritus and erythema early during the administration of antimicrobial therapy. However, the parasite is gradually eliminated during the body's natural shedding process. The following summarizes the preferred antimicrobial regimens in the treatment of scabies:[49][28][47][50][1][51][52][53]
- Antimicrobial therapy
- 1. Adult
- Preferred regimen (1): Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours;
- Preferred regimen (2): Ivermectin 200 ug/kg given orally, 4 times daily and repeated in 2 weeks as it has limited ovicidal activity;
- Preferred regimen (3): Ivermectin 1% lotion - applied to all areas of the body from the neck down and washed off after 8–14 hours; repeat treatment in 1 week if symptoms persist;
- Alternative regimen: Lindane (1%) 1 oz of lotion or 30 g of cream applied in a thin layer to all areas of the body from the neck down and thoroughly washed off after 8 hours
- Lindane is an alternative choice because of its toxicity. Lindane is not recommended for pregnant and breastfeeding women, children aged <10 years, and persons with extensive dermatitis. Seizures have occurred when lindane was applied after a bath or used by patients who had extensive dermatitis. Aplastic anemia after lindane use also has been reported. Resistance has also been reported.
- Note: Patients may experience worsening pruritus and erythema early during the administration of antimicrobial therapy
- 2. Infants and young children
- Preferred regimen: Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours;
- Note: Infants and young children aged< 10 years should not be treated with lindane.
- 3. Crusted Scabies
- Preferred regimen: (Topical scabicide topical Benzyl benzoate 25% OR topical Permethrin 5% cream (full-body application to be repeated daily for 7 days then twice weekly until discharge or cure) AND treatment with Ivermectin 200 ug/kg PO on days 1,2,8,9, and 15. Additional Ivermectin treatment on days 22 and 29 might be required for severe cases;
- 4.Pregnant or Lactating Women
- Preferred regimen: Permethrin 5% cream applied to all areas of the body from the neck down and washed off after 8–14 hours.
Primary Prevention[edit | edit source]
One of the most important means of preventing scabies is to encourage good hygiene and advocate healthy living conditions away from crowded conditions.[17]
Secondary Prevention[edit | edit source]
Once a patient has been diagnosed with scabies, it is empirical to begin treatment with the appropriate antimicrobial therapy to eradicate the infection and prevent re-infection. However, the following measures must also be followed:[12][54]
- Treatment of individuals who come in close contact with the patient, even if they are asymptomatic
- Fomites, such as clothes, towels and bed linens, must be machine washed and dried at a high temperature (60 C)
- Insecticide may be used for items that cannot be washed
References[edit | edit source]
- ↑ 1.00 1.01 1.02 1.03 1.04 1.05 1.06 1.07 1.08 1.09 1.10 1.11 1.12 Heukelbach J, Feldmeier H (2006). "Scabies". Lancet. 367 (9524): 1767–74. doi:10.1016/S0140-6736(06)68772-2. PMID 16731272.
- ↑ Ramos-e-Silva M (1998). "Giovan Cosimo Bonomo (1663-1696): discoverer of the etiology of scabies". Int. J. Dermatol. 37 (8): 625–30. PMID 9732015.
- ↑ Williams PH (1853). "ARSENIC IN CHRONIC SCABIES". Assoc Med J. 1 (14): 301. PMC 2449498. PMID 20740811.
- ↑ Liveing R (1875). "The Treatment of Scabies". Br Med J. 1 (735): 137. PMC 2295399. PMID 20747747.
- ↑ 5.0 5.1 Pomares C, Marty P, Delaunay P (2014). "Isolated itching of the genitals". Am. J. Trop. Med. Hyg. 90 (4): 589–90. doi:10.4269/ajtmh.13-0337. PMC 3973496. PMID 24696404.
- ↑ 6.0 6.1 Eshagh K, DeKlotz CM, Friedlander SF (2014). "Infant with a papular eruption localized to the back". JAMA Pediatr. 168 (4): 379–80. doi:10.1001/jamapediatrics.2013.3986. PMID 24710581.
- ↑ 7.0 7.1 Witkowski JA, Parish LC (1984). "Scabies: a cause of generalized urticaria". Cutis. 33 (3): 277–9. PMID 6723363.
- ↑ 8.0 8.1 Chapel TA, Krugel L, Chapel J, Segal A (1981). "Scabies presenting as urticaria". JAMA. 246 (13): 1440–1. PMID 6790738.
- ↑ 9.0 9.1 Kartono F, Lee EW, Lanum D, Pham L, Maibach HI (2007). "Crusted Norwegian scabies in an adult with Langerhans cell histiocytosis: mishaps leading to systemic chemotherapy". Arch Dermatol. 143 (5): 626–8. doi:10.1001/archderm.143.5.626. PMID 17515513.
- ↑ 10.0 10.1 Wong SS, Woo PC, Yuen KY (2005). "Unusual laboratory findings in a case of Norwegian scabies provided a clue to diagnosis". J. Clin. Microbiol. 43 (5): 2542–4. doi:10.1128/JCM.43.5.2542-2544.2005. PMC 1153733. PMID 15872307.
- ↑ 11.0 11.1 Lin S, Farber J, Lado L (2009). "A case report of crusted scabies with methicillin-resistant Staphylococcus aureus bacteremia". J Am Geriatr Soc. 57 (9): 1713–4. doi:10.1111/j.1532-5415.2009.02412.x. PMID 19895437.
- ↑ 12.0 12.1 12.2 12.3 12.4 Chosidow O (2006). "Clinical practices. Scabies". N. Engl. J. Med. 354 (16): 1718–27. doi:10.1056/NEJMcp052784. PMID 16625010.
- ↑ 13.0 13.1 Arlian LG (1989). "Biology, host relations, and epidemiology of Sarcoptes scabiei". Annu. Rev. Entomol. 34: 139–61. doi:10.1146/annurev.en.34.010189.001035. PMID 2494934.
- ↑ Walton SF, Holt DC, Currie BJ, Kemp DJ (2004). "Scabies: new future for a neglected disease". Adv. Parasitol. 57: 309–76. doi:10.1016/S0065-308X(04)57005-7. PMID 15504541.
- ↑ Fain A (1978). "Epidemiological problems of scabies". Int. J. Dermatol. 17 (1): 20–30. PMID 415012.
- ↑ Arlian LG, Runyan RA, Estes SA (1984). "Cross infestivity of Sarcoptes scabiei". J. Am. Acad. Dermatol. 10 (6): 979–86. PMID 6736342.
- ↑ 17.00 17.01 17.02 17.03 17.04 17.05 17.06 17.07 17.08 17.09 Romani L, Steer AC, Whitfeld MJ, Kaldor JM (2015). "Prevalence of scabies and impetigo worldwide: a systematic review". Lancet Infect Dis. 15 (8): 960–7. doi:10.1016/S1473-3099(15)00132-2. PMID 26088526.
- ↑ Arlian LG, Runyan RA, Achar S, Estes SA (1984). "Survival and infectivity of Sarcoptes scabiei var. canis and var. hominis". J. Am. Acad. Dermatol. 11 (2 Pt 1): 210–5. PMID 6434601.
- ↑ 19.0 19.1 Roberts LJ, Huffam SE, Walton SF, Currie BJ (2005). "Crusted scabies: clinical and immunological findings in seventy-eight patients and a review of the literature". J. Infect. 50 (5): 375–81. doi:10.1016/j.jinf.2004.08.033. PMID 15907543.
- ↑ 20.0 20.1 Arlian LG, Morgan MS, Estes SA, Walton SF, Kemp DJ, Currie BJ (2004). "Circulating IgE in patients with ordinary and crusted scabies". J. Med. Entomol. 41 (1): 74–7. PMID 14989349.
- ↑ Feldmeier H, Singh Chhatwal G, Guerra H (2005). "Pyoderma, group A streptococci and parasitic skin diseases -- a dangerous relationship". Trop. Med. Int. Health. 10 (8): 713–6. doi:10.1111/j.1365-3156.2005.01457.x. PMID 16045456.
- ↑ Bastian HM, Lindgren AM, Alarcón GS (1997). "Scabies mimicking systemic lupus erythematosus". Am. J. Med. 102 (3): 305–6. doi:10.1016/S0002-9343(99)80272-1. PMID 9217603.
- ↑ Brar BK, Pall A, Gupta RR (2003). "Bullous scabies mimicking bullous pemphigoid". J. Dermatol. 30 (9): 694–6. PMID 14578561.
- ↑ Burch JM, Krol A, Weston WL (2004). "Sarcoptes scabiei infestation misdiagnosed and treated as Langerhans cell histiocytosis". Pediatr Dermatol. 21 (1): 58–62. PMID 14871329.
- ↑ Mauleón-Fernandez C, Sáez-de-Ocariz M, Rodríguez-Jurado R, Durán-McKinster C, Orozco-Covarrubias L, Ruiz-Maldonado R (2005). "Nodular scabies mimicking urticaria pigmentosa in an infant". Clin. Exp. Dermatol. 30 (5): 595–6. doi:10.1111/j.1365-2230.2005.01832.x. PMID 16045712.
- ↑ Duran C, Tamayo L, de la Luz Orozco M, Ruiz-Maldonado R (1993). "Scabies of the scalp mimicking seborrheic dermatitis in immunocompromised patients". Pediatr Dermatol. 10 (2): 136–8. PMID 8346105.
- ↑ Gach JE, Heagerty A (2000). "Crusted scabies looking like psoriasis". Lancet. 356 (9230): 650. PMID 10968439.
- ↑ 28.0 28.1 28.2 28.3 28.4 28.5 28.6 28.7 Anderson KL, Strowd LC (2017). "Epidemiology, Diagnosis, and Treatment of Scabies in a Dermatology Office". J Am Board Fam Med. 30 (1): 78–84. doi:10.3122/jabfm.2017.01.160190. PMID 28062820.
- ↑ Hengge UR, Currie BJ, Jäger G, Lupi O, Schwartz RA (2006). "Scabies: a ubiquitous neglected skin disease". Lancet Infect Dis. 6 (12): 769–79. doi:10.1016/S1473-3099(06)70654-5. PMID 17123897.
- ↑ 30.0 30.1 Hay RJ, Steer AC, Engelman D, Walton S (2012). "Scabies in the developing world--its prevalence, complications, and management". Clin. Microbiol. Infect. 18 (4): 313–23. doi:10.1111/j.1469-0691.2012.03798.x. PMID 22429456.
- ↑ Burkhart CG, Burkhart CN, Burkhart KM (2000). "An epidemiologic and therapeutic reassessment of scabies". Cutis. 65 (4): 233–40. PMID 10795086.
- ↑ Kristensen JK (1991). "Scabies and Pyoderma in Lilongwe, Malawi. Prevalence and seasonal fluctuation". Int. J. Dermatol. 30 (10): 699–702. PMID 1955222.
- ↑ Estrada B (2003). "Ectoparasitic infestations in homeless children". Semin Pediatr Infect Dis. 14 (1): 20–4. doi:10.1053/spid.2003.127213. PMID 12748918.
- ↑ Currie BJ, Connors CM, Krause VL (1994). "Scabies programs in aboriginal communities". Med. J. Aust. 161 (10): 636–7. PMID 7968739.
- ↑ Terry BC, Kanjah F, Sahr F, Kortequee S, Dukulay I, Gbakima AA (2001). "Sarcoptes scabiei infestation among children in a displacement camp in Sierra Leone". Public Health. 115 (3): 208–11. doi:10.1038/sj/ph/1900748. PMID 11429717.
- ↑ Andrews JR, Tonkin SL (1989). "Scabies and pediculosis in Tokelau Island children in New Zealand". J R Soc Health. 109 (6): 199–203. PMID 2513405.
- ↑ 37.0 37.1 Heukelbach J, Wilcke T, Winter B, Feldmeier H (2005). "Epidemiology and morbidity of scabies and pediculosis capitis in resource-poor communities in Brazil". Br. J. Dermatol. 153 (1): 150–6. doi:10.1111/j.1365-2133.2005.06591.x. PMID 16029341.
- ↑ U.S. Preventive Services Task Forces https://www.uspreventiveservicestaskforce.org/BrowseRec/Search?s=scabies. Accessed on Jan 25, 2017.
- ↑ 39.0 39.1 Engelman D, Kiang K, Chosidow O, McCarthy J, Fuller C, Lammie P, Hay R, Steer A (2013). "Toward the global control of human scabies: introducing the International Alliance for the Control of Scabies". PLoS Negl Trop Dis. 7 (8): e2167. doi:10.1371/journal.pntd.0002167. PMC 3738445. PMID 23951369.
- ↑ Chakrabarti A (1985). "Some epidemiological aspects of animal scabies in human population". Int J Zoonoses. 12 (1): 39–52. PMID 4055268.
- ↑ Burgess I (1994). "Sarcoptes scabiei and scabies". Adv. Parasitol. 33: 235–92. PMID 8122567.
- ↑ Steer AC, Jenney AW, Kado J, Batzloff MR, La Vincente S, Waqatakirewa L, Mulholland EK, Carapetis JR (2009). "High burden of impetigo and scabies in a tropical country". PLoS Negl Trop Dis. 3 (6): e467. doi:10.1371/journal.pntd.0000467. PMC 2694270. PMID 19547749.
- ↑ Lawrence G, Leafasia J, Sheridan J, Hills S, Wate J, Wate C, Montgomery J, Pandeya N, Purdie D (2005). "Control of scabies, skin sores and haematuria in children in the Solomon Islands: another role for ivermectin". Bull. World Health Organ. 83 (1): 34–42. doi:/S0042-96862005000100012 Check
|doi=value (help). PMC 2623469. PMID 15682247. - ↑ http://picasaweb.google.com/mcmumbi/USMLEIIImages
- ↑ 45.00 45.01 45.02 45.03 45.04 45.05 45.06 45.07 45.08 45.09 45.10 45.11 45.12 45.13 45.14 "Dermatology Atlas".
- ↑ Jayaraj R, Hales B, Viberg L, Pizzuto S, Holt D, Rolland JM, O'Hehir RE, Currie BJ, Walton SF (2011). "A diagnostic test for scabies: IgE specificity for a recombinant allergen of Sarcoptes scabiei". Diagn. Microbiol. Infect. Dis. 71 (4): 403–7. doi:10.1016/j.diagmicrobio.2011.09.007. PMID 22018936.
- ↑ 47.0 47.1 Johnston G, Sladden M (2005). "Scabies: diagnosis and treatment". BMJ. 331 (7517): 619–22. doi:10.1136/bmj.331.7517.619. PMC 1215558. PMID 16166133.
- ↑ Hicks MI, Elston DM (2009). "Scabies". Dermatol Ther. 22 (4): 279–92. doi:10.1111/j.1529-8019.2009.01243.x. PMID 19580575.
- ↑ Workowski, Kimberly A.; Bolan, Gail A. (2015-06-05). "Sexually transmitted diseases treatment guidelines, 2015". MMWR. Recommendations and reports: Morbidity and mortality weekly report. Recommendations and reports / Centers for Disease Control. 64 (RR-03): 1–137. ISSN 1545-8601. PMID 26042815.
- ↑ Strong M, Johnstone P (2007). "Interventions for treating scabies". Cochrane Database Syst Rev (3): CD000320. doi:10.1002/14651858.CD000320.pub2. PMID 17636630.
- ↑ Thomas J, Peterson GM, Walton SF, Carson CF, Naunton M, Baby KE (2015). "Scabies: an ancient global disease with a need for new therapies". BMC Infect. Dis. 15: 250. doi:10.1186/s12879-015-0983-z. PMC 4487193. PMID 26123073.
- ↑ Goldust M, Rezaee E, Hemayat S (2012). "Treatment of scabies: Comparison of permethrin 5% versus ivermectin". J. Dermatol. 39 (6): 545–7. doi:10.1111/j.1346-8138.2011.01481.x. PMID 22385121.
- ↑ Usha V, Gopalakrishnan Nair TV (2000). "A comparative study of oral ivermectin and topical permethrin cream in the treatment of scabies". J. Am. Acad. Dermatol. 42 (2 Pt 1): 236–40. doi:10.1016/S0190-9622(00)90131-2. PMID 10642678.
- ↑ Elston DM (2002). "Controversies concerning the treatment of lice and scabies". J. Am. Acad. Dermatol. 46 (5): 794–6. PMID 12004328.
 KSF
KSF
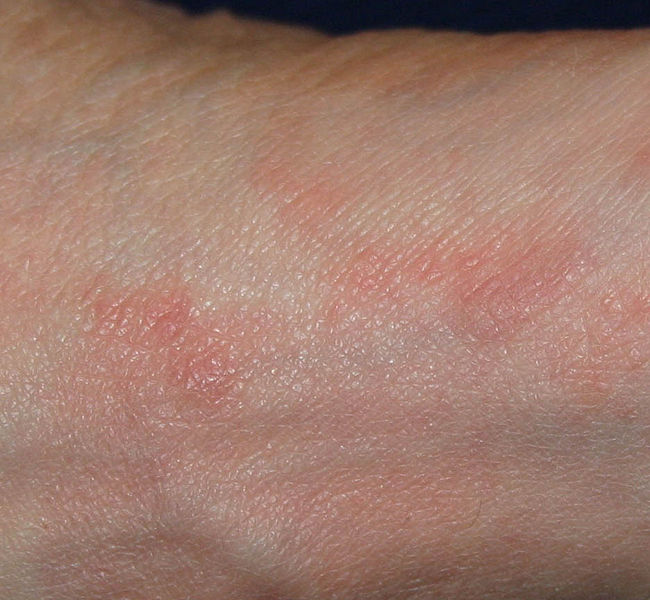



![Scabies (common location in ventral wrist) [44]](https://www.wikidoc.org/images/7/75/Scabies_%28common_location_is_ventral_wrist%29.jpg)

![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/b/b2/Norwegian_scabies25.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/1/15/Norwegian_scabies26.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/9/92/Norwegian_scabies41.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/7/73/Norwegian_scabies42.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/e/ef/Norwegian_scabies43.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/e/e3/Norwegian_scabies44.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/2/25/Norwegian_scabies45.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/4/4c/Norwegian_scabies01.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/8/83/Norwegian_scabies02.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/4/48/Norwegian_scabies15.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/2/2a/Norwegian_scabies16.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/9/94/Norwegian_scabies21.jpg)






![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/b/bd/Norwegian_scabies08.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/6/61/Norwegian_scabies09.jpg)
![Norwegian scabies. http://www.atlasdermatologico.com.br/ Adapted from Dermatology Atlas.[45]](https://www.wikidoc.org/images/e/e8/Norwegian_scabies10.jpg)





