Sinus rhythm
 From Wikidoc - Reading time: 5 min
From Wikidoc - Reading time: 5 min

|
WikiDoc Resources for Sinus rhythm |
|
Articles |
|---|
|
Most recent articles on Sinus rhythm Most cited articles on Sinus rhythm |
|
Media |
|
Powerpoint slides on Sinus rhythm |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Sinus rhythm at Clinical Trials.gov Clinical Trials on Sinus rhythm at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Sinus rhythm
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Patient resources on Sinus rhythm Discussion groups on Sinus rhythm Patient Handouts on Sinus rhythm Directions to Hospitals Treating Sinus rhythm Risk calculators and risk factors for Sinus rhythm
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Sinus rhythm |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Sinus rhythm is a term used in medicine to describe the normal beating of the heart, as measured by an electrocardiogram (ECG). It has certain generic features that serve as hallmarks for comparison with normal ECGs.
ECG Structure[edit | edit source]
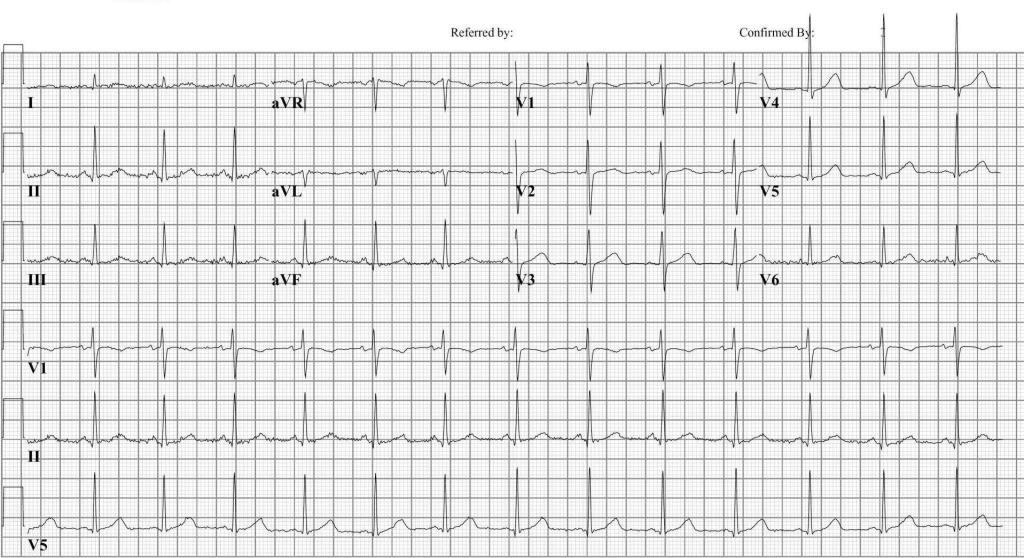
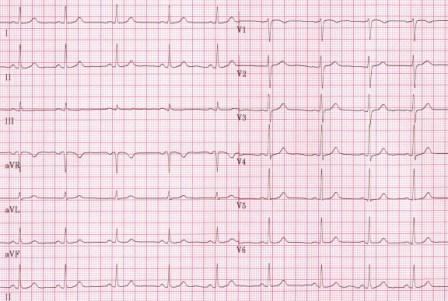
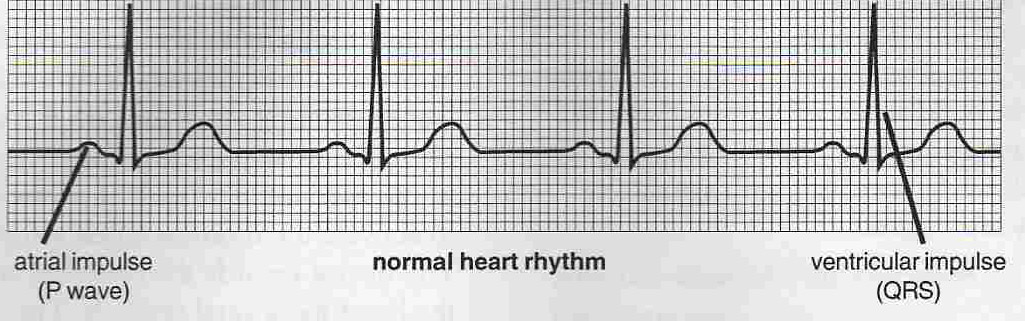
There are typically five distinct waves (identified by the letters P, Q, R, S, and T) in a single beat of the heart in sinus rhythm, and they occur in a specific order, over specific periods of time, with specific relative sizes. While there is a significant range within which variations in rhythm are considered normal, anything that deviates from sinus rhythm by more than a certain amount may be indicative of heart disease.
Sinus Rhythm on ECG[edit | edit source]
Sinus rhythm is characterized by a usual rate of anywhere between 60-100 bpm. Every QRS complex is preceded by a P wave and every P wave must be followed by a QRS (the opposite occurs if there is second or third degree AV block). The P wave morphology and axis must be normal and the PR interval will usually be 120 ms or greater.
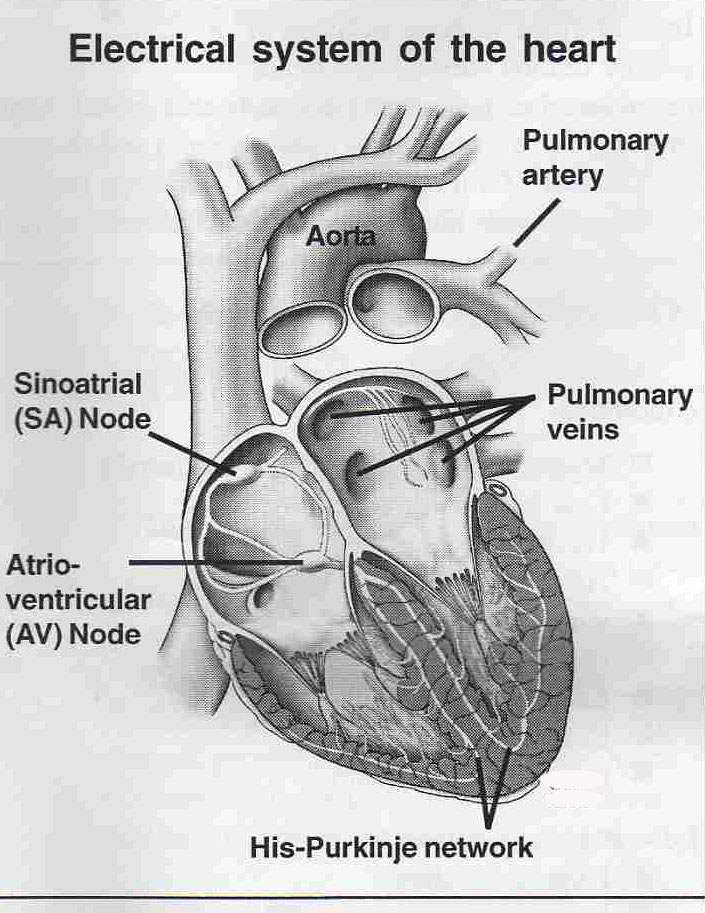
In normal sinus rhythm, electrical impulses from the SA node travel to the AV node with successful contraction of the two atria. The electrical impulses from the AV node successfully contract the ventricles. On the ECG, there are normal PQRST elements with no evidence of arrhythmia, tachycardia, or bradycardia.
Depolarization of the SA Node[edit | edit source]
In Normal Sinus Rhythm the pacemaker impulse is formed in the SA node which is located near the junction of the superior vena cava and right atrium. The impulse now spreads leftward and inferiorly through the atria (at first only in the RA, then in both RA and LA and finally only in the LA). Small fascicles of tissue which resemble conduction tissue can be demonstrated in the atria, called intra-atrial pathways which connect both atria and help organize atrial depolarization. A reasonable concept is to consider the spread of electrical stimulation through the atria as ripples on a pond with the pebble falling into the pond at the SA node and then spreading throughout the atria. Atrial depolarization inscribes the P wave on the ECG.
Depolarization of the AV Node[edit | edit source]
After depolarization of the atria, the impulse now arrives at the AV node. This is the only normal electrical connection between the atria and ventricles and serves as a safety valve to prevent too many atrial impulses from reaching the ventricles. The AV node is very complex and consists of several layers of cells having different action potentials and conduction characteristics. Since the atrial stimulus is delayed in the junctional area and there is no deplolarization of myocardium the ECG returns to the baseline as the PR segment.
Depolarization of the His Bundle and Right and Left Bundle or His Purkinje System (HPS)[edit | edit source]
Once the stimulus leaves the AV node it arrives at the His Bundle. The His bundle shortly divides into the right bundle branch and left bundle branch. The Left Bundle divides into a smaller anterior and a larger posterior radiation which fans out in the endocardial layers and meets again in the periphery as fibers of the Purkinje System. Conduction down all three major fascicles (Left anterior, Left posterior, and Right Bundle) is very rapid and is not represented on the ECG. The stimulus is then delivered to the endocardial surfaces of the RV and LV very rapidly and the myocardium depolarizes to form the QRS.
EKG Examples[edit | edit source]
 KSF
KSF