The heart in mixed connective tissue disorder
 From Wikidoc - Reading time: 6 min
From Wikidoc - Reading time: 6 min
Template:WikiDoc Cardiology News Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
Associate Editor: Cafer Zorkun, M.D., Ph.D. [2]
Overview[edit | edit source]
In 1972, Sharp et al first described Mixed Connective Tissue Disorder (MCTD) as a distinct rheumatic disease with overlapping features of systemic lupus erythematosus (SLE), polymyositis (PM), and progressive systemic sclerosis (PSS) associated with antibodies to RNAse sensitive extractable nuclear antigen. When the antigen was subsequently characterized as polypeptides on the U1 ribonuclear protein component of the splicesosome (U1RNP), MCTD became the first rheumatic disease syndrome to be defined by a serologic test.[1]
In addition to its rheumatic features, Mixed Connective Tissue Disorder (MCTD) has a number of cardiac manifestations including pericarditis, pericardial effusion, myocarditis, ventricular hypertrophy, ventricular dilatation, cardiac conduction disturbances, and vascular intimal hyperplasia. [2]
In one study evaluating 38 patients with Mixed Connective Tissue Disorder (MCTD), four of the five patients who died underwent an autopsy. All four cases showed epicardial and intramural coronary intimal proliferation.[3] Interestingly, none of these patients had pathologic evidence of myocardial infarction. In fact, in the result of same study stated that there were no coronary arterial thrombi or intimal plaques to suggest evidence of atherosclerosis.
In a similar follow-up study of 14 children with Mixed Connective Tissue Disorder (MCTD), arterial intimal hyperplasia and no evidence of myocardial damage was demonstrated in the 2 hearts undergoing autopsy.[4]
From the original 25 patients with Mixed Connective Tissue Disorder (MCTD) described by Sharp et al, a 4-5 year follow-up study discovered that eight patients died but only one death was attributed to a myocardial infarction.[5]
While arterial intimal hyperplasia is well described in patients with Mixed Connective Tissue Disorder (MCTD), the progression to an acute coronary syndrome (ACS) appears to be uncommon.
Histopathological Findings[edit | edit source]
There are no specific histologic findings that aid in the diagnosis of Mixed Connective Tissue Disorder as a separate autoimmune disease. For example, nephritis in MCTD is usually indistinguishable from lupus nephritis.
-
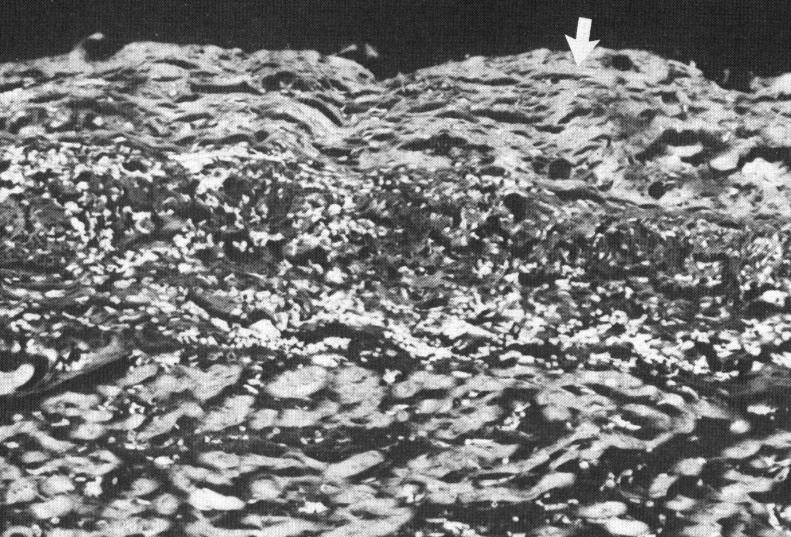
Fibrous Pericarditis in MCTD
-
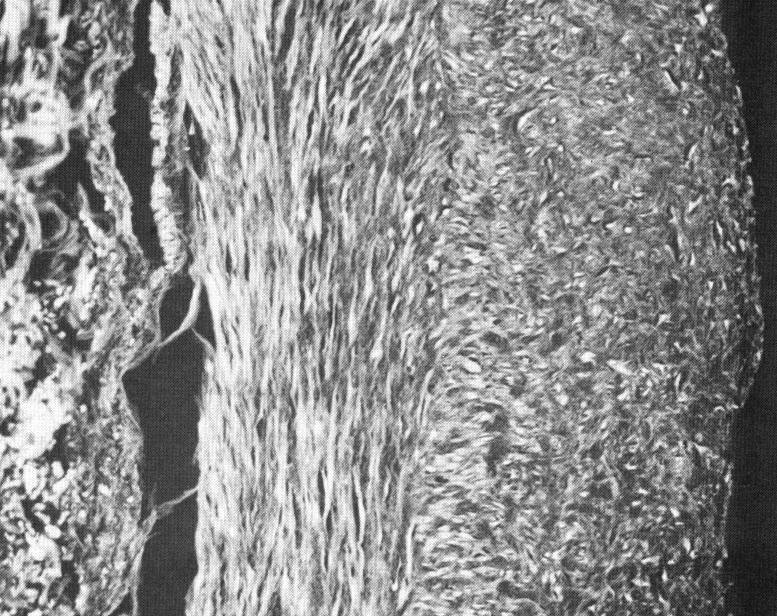
Cellular aggregates in perivascular space and adjacent myocardium
-
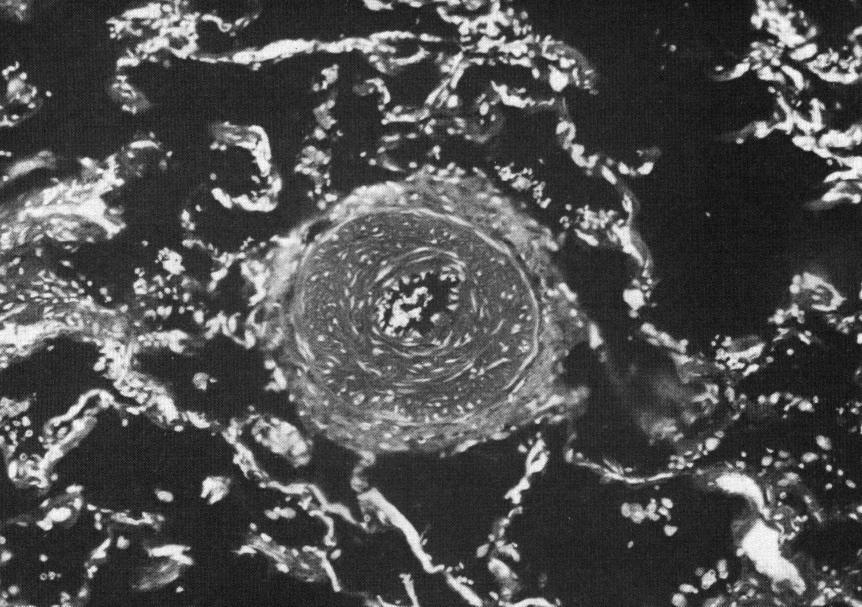
Cross Section of Intramural Coronary Artery
-
Small pulmonary artery in patient with MCTD and pulmnonary hypertension
Symptoms of MCTD[edit | edit source]
Common symptoms[edit | edit source]
- Swollen fingers or hands
Anti–U1 small nuclear RNP positive[edit | edit source]
Mixed findings[edit | edit source]
A.Systemic lupus erythematosus–like findings
- Facial erythema
- Leukopenia (<4,000/mm3) or thrombocytopenia (<100,000/mm3)
B.Progressive Systemic Sclerosis–like findings
- Pulmonary fibrosis, restrictive changes of the lung (forced vital capacity <80% of predicted), or reduced carbon monoxide diffusing capacity (<70% of predicted)
- Hypomotility or dilatation of esophagus
C.Polymyositis-like findings
- Muscle weakness
- Elevated serum level of muscle enzymes (creatine kinase)
- Myogenic pattern on electromyogram
Diagnosis of MCTD[edit | edit source]
A. Kasukawa criteria
- Presence of 1 or both common symptoms listed above
- Positive anti–U1 snRNP antibody
- Presence of 1 or more findings in at least 2 of the 3 disease categories under “mixed findings”
MCTD will be diagnosed when all 3 conditions are fulfilled.[6] [7] [8] [9] [10] [11] [12] [13] [14] [15] [16] [17]
B. Sharp criteria[18]
- Definite diagnosis requires 4 major criteria with positive anti-U1 RNP greater than 1:4000 and a negative anti-Sm Ab. U1 RNP is the specific RNP protein associated with this syndrome.
- Probable diagnosis requires either 3 major criteria or 2 major criteria (which must come from the first 3 major criteria listed) and 2 minor criteria plus an anti-U1 RNP greater than 1:1000.
- Possible diagnosis requires 3 major criteria without serologic evidence of disease or, if anti-U1 RNP is greater than 1:100, 2 major criteria or 1 major and 3 minor criteria.
- Major criteria are severe myositis, pulmonary involvement (diffusing capacity of lung for carbon monoxide 70% of normal, pulmonary hypertension, proliferating vascular lesions on lung biopsy), Raynaud phenomenon or esophageal hypomotility, swollen hands or sclerodactyly, and highest observed anti-U1 RNP (>1:10.000) with negative anti-Sm Ab.
- Minor criteria are alopecia, leukopenia (4000 WBC/mL), anemia (<10 g/dL for females, <12 g/dL for males), pleuritis, pericarditis, arthritis, trigeminal neuralgia, malar rash, thrombocytopenia (<100.000/mL), mild myositis, and history of swollen hands.
C. Alarcon-Segovia and Villareal classification and diagnostic criteria [19]
- Serologic criterion is a positive anti-RNP at a titer of 1:1600 or higher.
- Clinical criteria (at least 3) are edema of the hands, Raynaud phenomenon (i.e., 2 or 3 color changes), acrosclerosis, synovitis, and myositis (laboratory or biopsy evidence).
Cardiac Involvement in MCTD[edit | edit source]
Cardiovascular abnormalities associated with mixed connective tissue disease are rare. Presence of any of the complications listed below indicates unfavorable prognosis;
- Acute pericarditis and/or pericardial effusion,
- Intimal hyperplasia of coronary arteries,
- Perivascular and myocardial leukocytic infiltrates,
- Coronary Artery Disease: Although it is rarer, ACS may occur secondary to vascular changes and underlying CAD. The youngest patient with MCTD and ACS in literature was 18 years old. [20]
References[edit | edit source]
- ↑ Kasukawa R, Tojo T, Miyawaki S. Preliminary diagnostic criteria for classification of mixed connective tissue disease. In: Kasukawa R, Sharp GC, editors. Mixed connective tissue disease and antinuclear antibodies. Amsterdam: Elsevier; 1987. p. 41–7.
- ↑ Langley RL, Treadwell EL. Cardiac tamponade and pericardial disorders in connective tissue diseases: case report and literature review. J Natl Med Assoc 1994; 86: 149¡53.
- ↑ Alpert MA, Goldberg SH, Singsen BH, Durham JB, Sharp GC, Ahmad M, Madigan NP, Hurst DP, Sullivan WD, Cardiovascular manifestations of mixed connective tissue disease in adults. Circulation. 1983; 68:1182-1193
- ↑ Singsen BH, Bernstein BH, Kornreich HK et al.Mixed connective tissue disease in childhood.A clinical and serologic survey. J Pediatr 1977; 90: 893¡900.
- ↑ Nimelstein SH, Brody S, McShane D, Holman HR. Mixed connective tissue disease: a subsequent evaluation of the original 25 patients. Medicine 1980; 59: 239¡48.
- ↑ ACP Medicine, 2007, Dale D C, Federman D D
- ↑ Braunwald's Heart Disease 8th Ed, 2007, Libby P
- ↑ Mayo Clinic Cardiology, Concise Textbook, 3rd edition, 2007
- ↑ Hurst's The Heart, Fuster V, 11th (printed) and 12th (online) editions, 2004-2008
- ↑ NMS Medicine, 6th Edition, 2008
- ↑ Oxford Textbook of Medicine 4th edition (March 2003)
- ↑ Harris: Kelley's Textbook of Rheumatology, 7th ed. 2005
- ↑ Robbins and Cotran PATHOLOGIC BASIS OF DISEASE, 7th Edition, 2005
- ↑ Washington Manual of Medical Therapeutics, The, 32nd Edition, 2007
- ↑ Cecil Textbook of Medicine, 23rd Edition, 2007
- ↑ Harrison's Principals of Internal Medicine, 16th Edition, 2005
- ↑ Myocarditis, From Bench to Bedside, Cooper L T, 2003
- ↑ Sharp GC, Irvin WS, Tan EM, et al. Mixed connective tissue disease--an apparently distinct rheumatic disease syndrome associated with a specific antibody to an extractable nuclear antigen (ENA). Am J Med. Feb 1972;52(2):148-59. [Medline].
- ↑ Alarcon-Segovia D, Villareal M. Classification and diagnostic criteria for mixed connective tissue disease. In: Kasukawa R, Sharp GC, eds. Mixed Connective Tissue Disease and Anti-nuclear Antibodies. 1987:33-40.
- ↑ Jang J J, Olin J W, Fuster V. A teenager with mixed connective tissue disease presenting with an acute coronary syndrome. Vascular Medicine; 2004, Vol. 9 Issue 1, 31-34
Template:Diseases of the musculoskeletal system and connective tissue
 KSF
KSF