Vaccine
 From Wikidoc - Reading time: 12 min
From Wikidoc - Reading time: 12 min
|
WikiDoc Resources for Vaccine |
|
Articles |
|---|
|
Most recent articles on Vaccine |
|
Media |
|
Evidence Based Medicine |
|
Clinical Trials |
|
Ongoing Trials on Vaccine at Clinical Trials.gov Clinical Trials on Vaccine at Google
|
|
Guidelines / Policies / Govt |
|
US National Guidelines Clearinghouse on Vaccine
|
|
Books |
|
News |
|
Commentary |
|
Definitions |
|
Patient Resources / Community |
|
Directions to Hospitals Treating Vaccine Risk calculators and risk factors for Vaccine
|
|
Healthcare Provider Resources |
|
Causes & Risk Factors for Vaccine |
|
Continuing Medical Education (CME) |
|
International |
|
|
|
Business |
|
Experimental / Informatics |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [1]
A vaccine is an antigenic preparation used to establish immunity to a disease. The term derives from Edward Jenner's use of cowpox ("vacca" means cow in Latin), which, when administered to humans, provided them protection against smallpox, the work which Louis Pasteur and others carried on. Vaccines are based on the concept of variolation originating in China, in which a person is deliberately infected with a weak form of smallpox. Jenner realized that milkmaids who had contact with cowpox did not get smallpox. The process of distributing and administrating vaccines is referred to as vaccination. Since vaccination was much safer, smallpox inoculation fell into disuse and was eventually banned in England in 1840.
Vaccines can be prophylactic (e.g. to prevent or ameliorate the effects of a future infection by any natural or "wild" pathogen), or therapeutic (e.g. vaccines against cancer are also being investigated; see cancer vaccine).
Types of vaccines
[edit | edit source]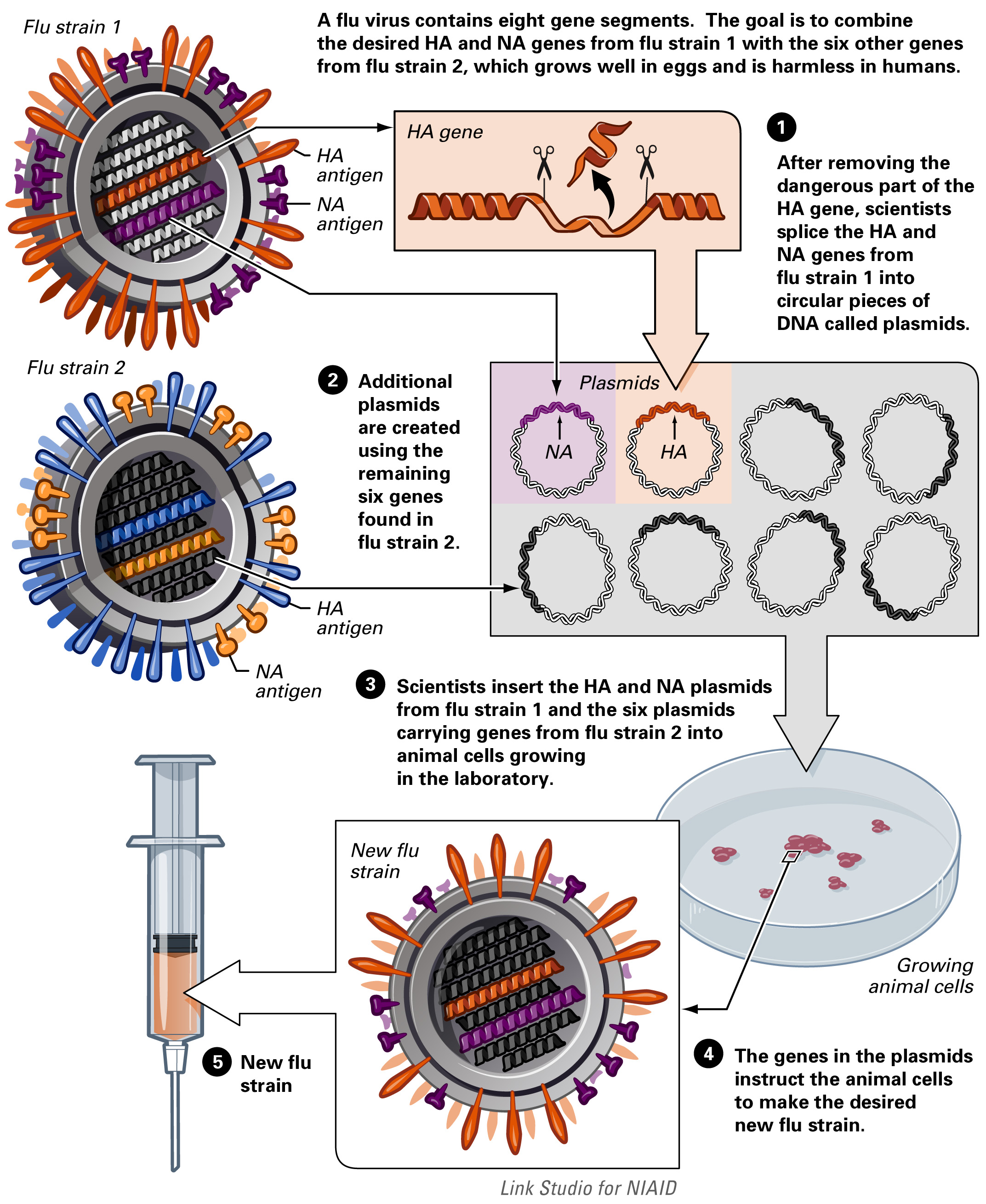
Vaccines may be dead or inactivated organisms or purified products derived from them.
There are four types of traditional vaccines[2]:
- Vaccines containing killed microorganisms - these are previously virulent micro-organisms that have been killed with chemicals or heat. Examples are vaccines against flu, cholera, bubonic plague, and hepatitis A.
- Vaccines containing live, attenuated microorganisms - these are live micro-organisms that have been cultivated under conditions that disable their virulent properties. They typically provoke more durable immunological responses and are the preferred type for healthy adults. Examples include yellow fever, measles, rubella, and mumps.
- Toxoids - these are inactivated toxic compounds from micro-organisms in cases where these (rather than the micro-organism itself) cause illness. Examples of toxoid-based vaccines include tetanus and diphtheria.
- Subunit - rather than introducing an inactivated or attenuated micro-organism to an immune system, a fragment of it can create an immune response. Characteristic examples include the subunit vaccine against HBV that is composed of only the surface proteins of the virus (produced in yeast) and the virus like particle (VLP) vaccine against Human Papillomavirus (HPV) that is composed of the viral major capsid protein.
The live tuberculosis vaccine is not the contagious strain, but a related strain called "BCG"; it is used in the United States very infrequently.
A number of innovative vaccines are also in development and in use:
- Conjugate - certain bacteria have polysaccharide outer coats that are poorly immunogenic. By linking these outer coats to proteins (e.g. toxins), the immune system can be led to recognize the polysaccharide as if it were a protein antigen. This approach is used in the Haemophilus influenzae type B vaccine.
- Recombinant Vector - by combining the physiology of one micro-organism and the DNA of the other, immunity can be created against diseases that have complex infection processes
- DNA vaccination - in recent years a new type of vaccine, created from an infectious agent's DNA called DNA vaccination, has been developed. It works by insertion (and expression, triggering immune system recognition) into human or animal cells, of viral or bacterial DNA. Some cells of the immune system that recognize the proteins expressed will mount an attack against these proteins and cells expressing them. Because these cells live for a very long time, if the pathogen that normally expresses these proteins is encountered at a later time, they will be attacked instantly by the immune system. One advantage of DNA vaccines is that they are very easy to produce and store. As of 2006, DNA vaccination is still experimental, but shows some promising results.
Note that while most vaccines are created using inactivated or attenuated compounds from micro-organisms, synthetic vaccines are composed mainly or wholly of synthetic peptides, carbohydrates or antigens. Some viral vaccines have been developed by use of cell lines derived from aborted fetuses ( http://www.lifecanada.org/html/science/Vaccines/ABriefHistoryofHumanDiploidCellStrains.pdf )
Developing immunity
[edit | edit source]The immune system recognizes vaccine agents as foreign, destroys them, and 'remembers' them. When the virulent version of an agent comes along, the immune system is thus prepared to respond, by (1) neutralizing the target agent before it can enter cells, and (2) by recognizing and destroying infected cells before that agent can multiply to vast numbers.
Vaccines have contributed to the eradication of smallpox, one of the most contagious and deadly diseases known to man. Other diseases such as rubella, polio, measles, mumps, chickenpox, and typhoid are nowhere near as common as they were just a hundred years ago. As long as the vast majority of people are vaccinated, it is much more difficult for an outbreak of disease to occur, let alone spread. This effect is called herd immunity. Polio, which is transmitted only between humans, is targeted by an extensive eradication campaign that has seen endemic polio restricted to only parts of four countries.[3] The difficulty of reaching all children, however, has caused the eradication date to be missed twice by 2006.
Vaccination schedule
[edit | edit source]- Main article: Vaccination schedule
- See also: Vaccination policy
In order to provide best protection, children are recommended to receive vaccinations as soon as their immune systems are sufficiently developed to respond to particular vaccines, with additional 'booster' shots often required to achieve 'full immunity'. This has led to the development of complex vaccination schedules. In the United States, the Advisory Committee on Immunization Practices, which recommends schedule additions for the Center for Disease Control, recommends routine vaccination of children against: hepatitis A, hepatitis B, polio, mumps, measles, rubella, diphtheria, pertussis, tetanus, HiB, chicken pox, rotavirus, influenza, meningococcal disease and pneumonia. The large number of vaccines and boosters recommended (up to 24 injections by age two) has led to problems with achieving full compliance. In order to combat declining compliance rates, various notification systems have been instituted and a number of combination injections are now marketed (e.g., Prevnar and ProQuad vaccines), which provide protection against multiple diseases.
Besides recommendations for infant vaccination boosters, many specific vaccines are recommended for repeated injections throughout life -- most commonly for measles, tetanus, influenza, and pneumonia. Pregnant women are often screened for continued resistance to rubella. In 2006, a vaccine was introduced against shingles, a disease caused by the chicken pox virus, which usually affects the elderly. Vaccine recommendations for the elderly concentrate on pneumonia and influenza, which are more deadly to that group.
Vaccine controversies
[edit | edit source]Opposition to vaccination, from a wide array of vaccine critics, has existed since the earliest vaccination campaigns: [4].
A number of vaccines, including those given to very young children, have contained thiomersal, a preservative that metabolizes into ethylmercury. It has been used in some influenza, DTP (diphtheria, tetanus and pertussis) vaccine formulations. Since 1997, use of thimerosal has been gradually diminishing in western industrialized countries after recommendations by medical authorities, but trace amounts of thimerosal remain in many vaccines and in some vaccines, thimerosal has not yet been phased out despite recommendations. Some states in USA have enacted laws banning the use of thimerosal in childhood vaccines.
In the late 1990s, controversy over vaccines escalated in both the US and the United Kingdom when a study, published in the respected journal Lancet, by Dr. Andrew Wakefield suggested a possible link between bowel disorders, autism and the MMR vaccine, and urged further research.[1] His report garnered significant media attention, leading to a drop in the uptake of the MMR vaccine in the United Kingdom and some other countries. In response to the controversies, a number of studies with larger sample sizes were conducted, and failed to confirm the findings.[5] [6]. In 2004, 10 of the 13 authors of the original Wakefield study retracted the paper's "interpretation", or conclusion, section, which had claimed: "Interpretation. We identified associated gastrointestinal disease and developmental regression in a group of previously normal children, which was generally associated in time with possible environmental triggers." The retraction of this claim stated that the data were insufficient to establish a causal link between MMR vaccine and autism.[7] Wakefield was later found to have received £435,000 in fees from trial lawyers attempting to show the vaccine was dangerous [8] [9]. Also in 2004, the United States' Institute of Medicine reported that evidence "favors rejection" of any link between vaccines containing thimerosal, or MMR, and the development of autism [10].
In 2004 and 2005, England and Wales experienced an increase in the incidence of mumps infections among adolescents and young adults. The age group affected were too old to have received the routine MMR immunisations around the time the paper by Wakefield et al was published, and too young to have contracted natural mumps as a child, and thus to achieve a herd immunity effect. With the decline in mumps that followed the introduction of the MMR vaccine, these individuals had not been exposed to the disease, but still had no immunity, either natural or vaccine induced. Therefore, as immunization rates declined following the controversy and the disease re-emerged, they were susceptible to infection. [11] [12]. This and similar examples indicate the importance of:
- careful modelling to anticipate the impact that an immunisation campaign will have on the epidemiology of the disease in the medium to long term
- ongoing surveillance for the relevant disease following introduction of a new vaccine and
- maintaining high immunisation rates, even when a disease has become rare.
There is opposition to any type of vaccination from some sectors of the community, particularly those who favor 'alternative' health care. Some skeptics claim that mass immunization is a eugenics program. Naturopaths and other alternative health care practitioners sometimes offer their own, alternative treatments to conventional vaccination.
In Australia, a massive increase in vaccination rates was observed when the federal government made certain benefits (such as the universal 'Family Allowance' welfare payments for parents of children) dependent on vaccination. As well, children were not allowed into school unless they were either vaccinated or their parents completed a statutory declaration refusing to immunize them, after discussion with a doctor, and other bureaucracy. (Similar school-entry vaccination regulations have been in place in some parts of Canada for several years.) It became easier and cheaper to vaccinate one's children than not to. When faced with the annoyance, many more casual objectors simply gave in.
Another vaccination controversy concerns smallpox. Since it has been eradicated, some suggest that the stores of smallpox virus should be destroyed. In an article on Newswise [13] both sides debate the issue: "The destruction of remaining smallpox virus stocks is an overdue step forward for public health and security that will dramatically reduce the possibility that this scourge will kill again, either by accident or design, argues Edward Hammond of The Sunshine Project, an organisation seeking international consensus against biological weapons."
"But John Agwunobi of the US Department of Health and Human Services believes that clandestine stocks almost certainly exist and that destroying the virus would be “irreversible and short sighted.” [14]
Efficacy of vaccines
[edit | edit source]Vaccines do not guarantee complete protection from a disease. Sometimes this is because the host's immune system simply doesn't respond adequately or at all. This may be due to a lowered immunity in general (diabetes, steroid use, HIV infection) or because the host's immune system does not have a B-cell capable of generating antibodies to that antigen.
Even if the host develops antibodies, the human immune system is not perfect and in any case the immune system might still not be able to defeat the infection.
Adjuvants are typically used to boost immune response. Adjuvants are sometimes called the dirty little secret of vaccines [15] in the scientific community, as not much is known about how adjuvants work. Most often aluminium adjuvants are used, but adjuvants like squalene are also used in some vaccines and more vaccines with squalene and phosphate adjuvants are being tested. The efficacy or performance of the vaccine is dependent on a number of factors:
- the disease itself (for some diseases vaccination performs better than for other diseases)
- the strain of vaccine (some vaccinations are for different strains of the disease) [16]
- whether one kept to the timetable for the vaccinations (see Vaccination schedule)
- some individuals are 'non-responders' to certain vaccines, meaning that they do not generate antibodies even after being vaccinated correctly
- other factors such as ethnicity or genetic predisposition
When a vaccinated individual does develop the disease vaccinated against, the disease is likely to be milder than without vaccination.
Economics of vaccine development
[edit | edit source]One challenge in vaccine development is economic: many of the diseases most demanding a vaccine, including HIV, malaria and tuberculosis, exist principally in poor countries. Although some contend pharmaceutical firms and biotech companies have little incentive to develop vaccines for these diseases, because there is little revenue potential, the number of vaccines actually administered has risen dramatically in recent decades. This increase, particularly in the number of different vaccines administered to children before entry into schools may be due to government mandates, rather than economic incentive. Most vaccine development to date has relied on 'push' funding by government and non-profit organizations, of government agencies, universities and non-profit organizations.
Many researchers and policymakers are calling for a different approach, using 'pull' mechanisms to motivate industry. Mechanisms such as prizes, tax credits, or advance market commitments could ensure a financial return to firms that successfully developed a HIV vaccine. If the policy were well-designed, it might also ensure people have access to a vaccine if and when it is developed.
Statistics from the government agencies of the U.S., the British Commonwealth and the U.K. show that between the 1800s and the time various vaccines were introduced, the incidences of the diseases for which vaccines were provided were reduced by 70%-90%. For some, this prompts the question as to whether the reduction in the morbidity and mortality due to these diseases is owed to improved sewage systems, food refrigeration, improved home and work environments, and the introduction of antibiotics, all of which occurred during the same period.
Preservatives
[edit | edit source]In order to extend shelf life and reduce production and storage costs, thimerosal, a preservative containing about 49% of a form of mercury called ethylmercury, was used routinely until recent years.[17] Thimerosal has been phased out in the U.S. in all but a few flu vaccines [18] (it has been phased out earlier in other countries, e.g. Denmark in 1992), but may be used in stages of manufacture. Parents wishing to avoid this preservative, most common in multi-dose containers of influenza vaccine, may specifically ask for thimerosal-free alternatives that contain only trace amounts.[19]
A study published in the September 2007 New England Journal of Medicine reported no causal association between early exposure to mercury from thimerosal-containing vaccines and neurological problems by the age of 7 to 10 years old.[2]
Vaccines for nonhumans
[edit | edit source]See also
[edit | edit source]References
[edit | edit source]- ↑ Wakefield A, Murch S, Anthony A; et al. (1998). "Ileal-lymphoid-nodular hyperplasia, non-specific colitis, and pervasive developmental disorder in children". Lancet. 351 (9103): 637–41. doi:10.1016/S0140-6736(97)11096-0. PMID 9500320. Retrieved 2007-09-05.
- ↑ William W. Thompson, Ph.D.; et al. (2007). "Early Thimerosal Exposure and Neuropsychological Outcomes at 7 to 10 years". New England Journal of Medicine. 357 (13): 1281–1292.
Additional Resources
[edit | edit source]- AAPPublications.org - 'Thimerosal and the Occurrence of Autism: Negative Ecological Evidence From Danish Population-Based Data' Pediatrics, Vol 112, No 3, September 2003 (Denmark study on autism rates)
- BMJJournals.com - 'Comparative efficacy of three mumps vaccines', Matthias Schlegel, Joseph J. Osterwalder, Renato L. Galeazzi, Pietro J. Vernazza, British Medical Journal' Vol 319, No 352, August 7, 1999
- UNT.edu - Congressional Research Service (CRS) Reports regarding vaccines University of North Texas
- Vaccine Information.org - 'Vaccine Information for the Public and Health Professionals: Information about vaccine preventable diseases', Immunization Action Coalition
- SI.edu - 'History of Vaccines', Smithsonian Institute
- cdc.gov - Mercury and Vaccines (Thimerosal) from the CDC
- dissidentvoice.org - 'Bush Puppets Push for New Law to Protect Drug Companies', Dissident Voice
- Expert Review of Vaccines. Peer-reviewed journal published by Future Science Group
- Vaccination of Humans Encyclopedia of Life Sciences: Wiley Interscience. January 2006.
- Vaccination Encyclopedia of Life Sciences: Wiley Interscience. September 2005.
- Leiva R. A brief history of human diploid cell strains. Natl Cathol Bioeth Q. 2006 Autumn;6(3):443-51 http://www.lifecanada.org/html/science/Vaccines/ABriefHistoryofHumanDiploidCellStrains.pdf
External links
[edit | edit source]General
[edit | edit source]- Vaccines: Types and development - University of Arizona
- Vaccines Licensed for Immunization and Distribution in the US
- Website for Arthur Allen's 2007 book, "Vaccine, the Controversial History of Medicine's Greatest Lifesaver" (WW Norton)
- Vaccine news, information, and commentary from the University of Pennsylvania Center for Bioethics
Vaccine proponent views
[edit | edit source]- CGDev.org -'Vaccines for Development' (updated regularly), Center for Global Development
- ClearlyExplained.com - 'Vaccines', Richard Conan-Davies, BSc Dip Ed (October 22, 2001)
- NIH.gov - 'Immunization' ('conventional' opinion on vaccines), National Institute of Health
- TownHall.com - 'Don't believe the childhood vaccine fearmongers', Michael Fumento (June 30, 2005)
Vaccine safety critical views
[edit | edit source]- Template:McGrawHillAnimation
- MacroBiotic.net - 'A Short History of Vaccines'
- IOM.edu (pdf) - 'Before the Institute of Medicine' (statement on link between thimerosol and autism), US Congressman Dave Weldon, MD, (February 9, 2004)
- Liberty-Page.com - 'Bad Medicine: Or...How government interference in the vaccine market causes shortages, intellectual stagnation and death.'
- NoVaccine.com - 'The World Association for Vaccine Education' (WAVE), Dan Schultz, DC
- [20] Immunisation Awareness Society (IAS) New Zealand
- [21] Think Twice Global vaccine institute
- [22] Vaccination Liberation
Template:Vaccines Template:Major Drug Groups
ca:Vacuna cs:Vakcína da:Vaccination de:Impfstoff eo:Vakcino fa:واکسن ko:백신 id:Vaksin it:Vaccino he:חיסון nl:Vaccin no:Vaksine nn:Vaksine simple:Vaccination sk:Očkovanie sl:Cepivo fi:Rokotus sv:Vaccination te:టీకా th:วัคซีน
 KSF
KSF