Viral hemorrhagic fever primary prevention
 From Wikidoc - Reading time: 11 min
From Wikidoc - Reading time: 11 min
|
Viral hemorrhagic fever Microchapters |
|
Diagnosis |
|---|
|
Treatment |
|
Case Studies |
|
Viral hemorrhagic fever primary prevention On the Web |
|
American Roentgen Ray Society Images of Viral hemorrhagic fever primary prevention |
|
Risk calculators and risk factors for Viral hemorrhagic fever primary prevention |
Editor-In-Chief: C. Michael Gibson, M.S., M.D. [7]
Primary Prevention[edit | edit source]
With the exception of yellow fever and Argentine hemorrhagic fever, for which vaccines have been developed, no vaccines exist that can protect against these diseases. Therefore, prevention efforts must concentrate on avoiding contact with host species. If prevention methods fail and a case of VHF does occur, efforts should focus on preventing further transmission from person to person, if the virus can be transmitted in this way.Because many of the hosts that carry hemorrhagic fever viruses are rodents, disease prevention efforts include
Controlling rodent populations[edit | edit source]
- Discouraging rodents from entering or living in homes or workplaces.
- Encouraging safe cleanup of rodent nests and droppings.
- For hemorrhagic fever viruses spread by arthropod vectors, prevention efforts often focus on community-wide insect and arthropod control. In addition, people are encouraged to use insect repellant, proper clothing, bednets, window screens, and other insect barriers to avoid being bitten.
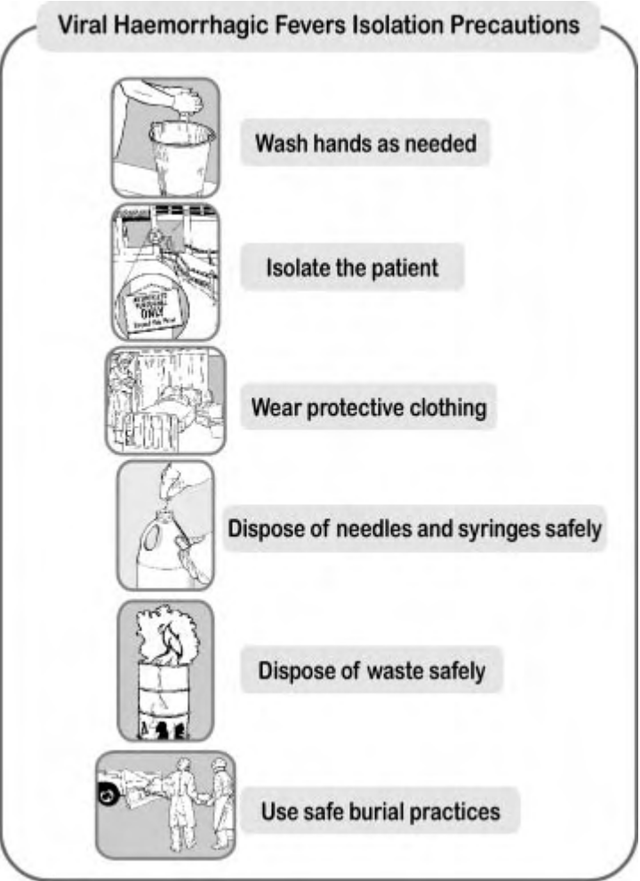
For those hemorrhagic fever viruses that can be transmitted from one person to another, avoiding close physical contact with infected people and their body fluids is the most important way of controlling the spread of disease. Barrier nursing or infection control techniques include isolating infected individuals and wearing protective clothing. Other infection control recommendations include proper use, disinfection, and disposal of instruments and equipment used in treating or caring for patients with VHF, such as needles and thermometers.
Specimen Handling[edit | edit source]
- Alert laboratory staff to the nature of the specimens prior to sending them to the clinical laboratory. Specimens should remain in the custody of designated laboratory personnel until testing is completed. Due to the potential risks associated with handling infectious materials, laboratory testing should be limited to the minimum necessary for essential diagnostic evaluation and patient care.
- While obtaining clinical laboratory specimens from the patient, use infection control precautions for patient care outlined in this document. Place specimens in sealed plastic bags, then transport them in a clearly labeled, durable, leak-proof container directly to the specimen handling area of the laboratory. Care should be taken not to contaminate the external surfaces of containers.
- Process clinical specimens in a class II biological safety cabinet following biosafety level 3 practices. If possible, pretreat serum used in laboratory tests with the combination of heat-inactivation at 56° C and polyethylene glycol p-tert-octylphenyl ether (Triton(®) X-100)*; treatment with 10 uL of 10% Triton(®) X-100 per 1 mL of serum for 1 hour reduces the titer of hemorrhagic fever viruses in serum, although 100% efficacy in inactivating these viruses should not be assumed. For tests in which the validity is affected by the presence of a detergent in the serum, heat inactivation alone may be of some benefit in reducing infectivity.
- Blood smears (e.g., for malaria) are not infectious for VHF after fixation in solvents.
- Attempts to isolate or cultivate the virus should not be part of routine clinical laboratory diagnosis when VHF is suspected. If such procedures are done on specimens where VHF is suspected, biosafety level 4 facilities and procedures are required.
- Routine cleaning and disinfecting procedures can be used for automated analyzers; analyzers should be disinfected after use as recommended by the manufacturer or with a 500 parts per million solution (1:100 dilution) of sodium hypochlorite (1/4 cup of household bleach to 1 gallon water).
Environmental Infection Control Procedures[edit | edit source]
- Environmental surfaces or inanimate objects contaminated with blood, other body fluids, secretions, or excretions should be cleaned and disinfected using standard procedures (See See: Guideline for Environmental Infection Control in Healthcare Facilities).
- Disinfection can be accomplished using a U.S. Environmental Protection Agency (EPA)-registered hospital disinfectant or a 1:100 dilution of household bleach (1/4 cup bleach to 1 gallon water). For grossly soiled surfaces, (e.g., vomitus or stool), use a 1:10 dilution of household bleach.
- Soiled linens should be placed in clearly labeled leak-proof bags at the site of use, transported directly to the laundry area, and laundered following routine healthcare laundry procedures.
- Liquid medical waste such as feces and vomitus can be disposed of in the sanitary sewer following local sewage disposal requirements (www.cdc.gov/ncidod/hip/enviro/guide.htm). Care should be taken to avoid splashing when disposing of these materials.
- When discarding solid medical waste (e.g., needles, syringes, and tubing) contaminated with blood or other body fluids from VHF patients, contain the waste with minimal agitation during handling. Properly contained wastes should be managed according to existing local and state regulations for ensuring health and environmental safety during medical waste treatment and disposal. On-site treatment of the waste in an incinerator or a gravity-displacement autoclave for decontamination purposes will help to minimize handling of contaminated waste. Alternatively, off-site medical waste treatment resources may be used. ===Standard Precautions===
- The use of standard precautions is recommended with all patients in a healthcare environment.[1] This includes a minimum level of standard precautions for use with all people regardless of their infection status, routine handwashing practices, safe handling and disposal of used needles and syringes, and intensifying standard precautions. It also includes VHF isolation precautions when needed
- Limited supplies and resources may prevent a health facility from using all the standard precautions all the time. However, health facilities should establish and maintain a basic, practical level of standard precautions that can be used routinely with patients in their health facility. This requires a source of clean water, routine handwashing before and after any contact with a person who has fever, and safe handling and disposal of sharp instruments and equipment.
- Washing hands with soap and water eliminates microorganisms from the skin and hands. This provides some protection against transmission of VHF and other diseases. This requires at least cake soap cut into small pieces, soap dishes with openings that allow water to drain away, running water or a bucket kept full with clean water, a bucket for collecting rinse water and a ladle for dipping, if running water is not available, and one-use towels.
- The handwashing technique that is recommended is to place a piece of soap in the palm of one hand, wash the opposite hand and forearm, rub the surfaces vigorously for at least 10 seconds, move soap to the opposite hand and repeat, use clean water to rinse both hands and then the forearms, dry the hands and forearms with a clean one-use towel, or let rinsed hands and forearms air-dry.
- Reusable needles and syringes are not recommended. If reusable needles and syringes are used, clean, disinfect and sterilize them before reuse. Needles and syringes used with VHF patients require special care. Cleaning staff should wear two pairs of gloves when handling needles and syringes used with any patient with a known or suspected VHF.
Handling Suspected Cases[edit | edit source]
- In an outbreak situation, several cases occur around the same time. They may be grouped together, and there may be person-to-person transmission. An initial diagnosis of a VHF can be made based on the signs and symptoms of the specific VHF.
- Suspecting a VHF during a non-outbreak situation in a single case is more difficult. The early symptoms of a VHF include high fever and headache. These are also symptoms for many infections seen at the health facility. Most people who present with fever do not have a VHF. Their fever is more often caused by malaria, typhoid fever, dysentery, severe bacterial infection or other fever-producing illnesses usually seen in the area.
- The health worker probably will not suspect a VHF until more severe signs develop and the patient does not respond to recommended treatment for other illnesses. However, health workers should be aware of the possibility of VHF in a non-outbreak situation. As soon as a VHF is suspected, VHF isolation precautions should begin. This will help reduce the number of people exposed to the VHF.
- Isolating the VHF patient will restrict patient access to health facility staff trained to use VHF isolation precautions. Establish a barrier between the VHF patient and uninfected patients, other health facility staff, and visitors.

- Patients who are hospitalized or treated in an outpatient healthcare setting should be placed in a private room and Standard, Contact, and Droplet Precautions should be initiated. Patients with respiratory symptoms also should wear a face mask to contain respiratory droplets prior to placement in their hospital or examination room and during transport.
- Caretakers should use barrier precautions to prevent skin or mucous membrane exposure of the eyes, nose, and mouth with patient blood, other body fluids, secretions (including respiratory droplets), or excretions. All persons entering the patient's room should wear gloves and gowns to prevent contact with items or environmental surfaces that may be soiled. In addition, face shields or surgical masks and eye protection (e.g., goggles or eyeglasses with side shields) should be worn by persons coming within approximately 3 feet of the patient.
- Additional barriers may be needed depending on the likelihood and magnitude of contact with body fluids. For example, if copious amounts of blood, other body fluids, vomit, or feces are present in the environment, plastic apron, leg, and shoe coverings also may be needed.
- Nonessential staff and visitors should be restricted from entering the room of patients with suspected VHF. Maintain a log of persons entering the patient’s room.
- Before exiting the room of a patient with suspected VHF, safely remove and dispose of all protective gear, and clean and disinfect shoes that are soiled with body fluids as described in the section on environmental infection control below.
- To prevent percutaneous injuries, needles and other sharps should be used and disposed of in accordance with recommendations for Standard Precautions.
- If the patient requires a surgical or obstetric procedure, consult your state health department and CDC regarding appropriate precautions for these invasive procedures.
- Although transmission by the airborne route has not been established, hospitals may choose to use Airborne Precautions for patients with suspected VHF who have severe pulmonary involvement or who undergo procedures that stimulate coughing and promote the generation of aerosols (e.g. aerosolized or nebulized medication administration, diagnostic sputum induction, bronchoscopy, airway suctioning, endotracheal intubation, positive pressure ventilation via face mask [e.g., biphasic intermittent positive airway pressure ventilation, continuous positive airway pressure ventilation], and high-frequency oscillatory ventilation) to prevent possible exposure to airborne particles that may contain virus.
- When a VHF case is suspected in the health facility, the following protective clothing should be worn in the isolation area:
- A scrub suit or inner layer of clothing (an old shirt and trousers brought from home)
- A pair of thin gloves
- Rubber boots or overshoes (only if the floor is soiled)
- A gown or outer layer of clothing (surgical or disposable gown with long sleeves and cuffs)
- A plastic apron worn over both layers of clothes
- A second pair of thin or thick gloves. Wearing a second pair of gloves provides an added measure of safety during patient care and when handling contaminated supplies
- A HEPA-filter (high-efficiency particulate air respirator) or other biosafety mask (or surgical mask if HEPA-filter or other biosafety mask is not available)
- Cotton head covering
- Clear eyeglasses or non-fogging goggles
- When protective clothing is not available or is in short supply, adaptations must be made and used
Putting On[edit | edit source]
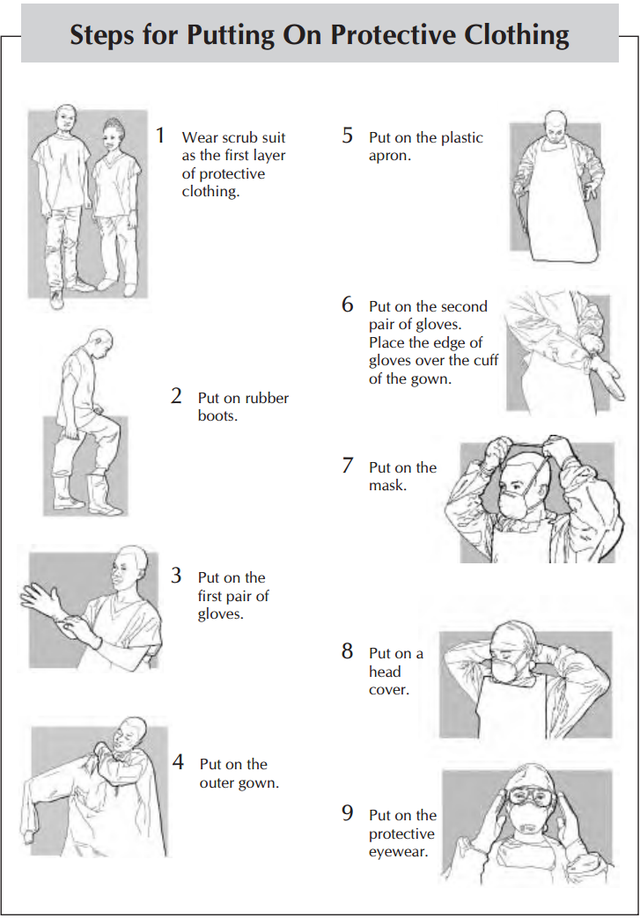
- There are specific recommendation regarding the putting on of protective clothing including:
- Before entering the changing room, remove jewelry, wallets and other valuables.
- Remove street clothes and hang them on a hook. Put on the scrub suit or set of old clothes.
- Enter the changing room.
- Put on rubber boots. Put on each boot and tuck the trouser leg inside the boot. If overboots are used, tape the top of the boot to the leg with plastic tape. This will help prevent spills from running inside the boots.
- Put on the first pair of gloves. Look at your hands for cut or broken skin. If the skin is cut or broken, refrain from direct patient contact. Put on one glove at a time. :* If the scrub suit or set of old clothes has long sleeves, place the edge of each glove under the cuff. When only one pair of gloves is worn, place the edge of the glove over the cuff or gown. If gloves are not available, use plastic bags. Put on one layer now. Attach and close the first layer with tape or elastic bands
- Put on the outer gown. Pick up the gown from the inside. This is especially important if the gown is being reused
- Put on the plastic or rubber apron.
- Put on the second pair of gloves
- Put on the mask and head cover
- Put on the protective eyewear. Attach the eyeglasses or goggles behind the head with string or cord to prevent the eyewear from falling off.
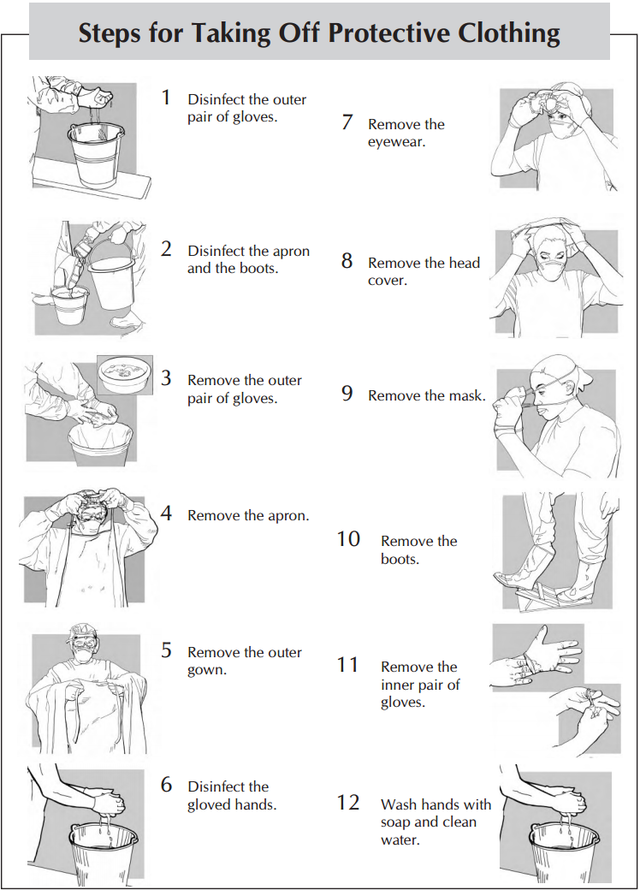
Taking off[edit | edit source]
- There are also specific recommendations regarding the removal of protective clothing including:
- Disinfect the outer pair of gloves, wash the gloved hands in soap and water, dip the gloved hands in 1:100 bleach solution (see below) for one minute
- Disinfect the apron. Spray or wipe it with 1:100 bleach solution.
- Disinfect the boots. Use a sprayer containing 1:100 bleach solution to spray boots or hold the foot over a pan or basin and ask another health worker to pour 1:100 bleach solution over the boots or step into a shallow pan containing 1:100 bleach solution and wipe boots on a bleach-drenched cloth
- Remove the outer pair of gloves
- Remove the apron and outer gown
- Disinfect the gloved hands after contact with apron and outer gown.
- Remove the eyewear, head cover and mask.
- Remove the boots. Place a towel that has been soaked in 1:100 bleach solution on the floor for health facility staff to stand on when removing boots
- Remove the inner pair of gloves.
- Remove inner layer of clothes and dress in street clothes.
- Wash hands with soap and clean water before leaving the changing room.
Handling Equipments[edit | edit source]
- Disinfection kills almost all bacteria, fungi, viruses, and protozoa. It reduces the number of microorganisms to make equipment and surfaces safer for use. When VHF is suspected in the health facility, all medical, nursing, laboratory and cleaning staff should disinfect:
- Hands and skin after contact with a VHF patient or infectious body fluids.
- Gloved hands after contact with each VHF patient or after contact with infectious body fluids (when gloves cannot be changed).
- Thermometers, stethoscopes and other medical instruments after use with each VHF patient.
- Spills of infectious body fluids on the walls and floors.
- Patient excreta and containers contaminated by patient excreta.
- Reusable supplies such as protective clothing and patient bedding.
- Used needles and syringes.
Bleach Preparation[edit | edit source]
- Two strengths of solution are recommended.
- 1:10 bleach solution is a strong solution used to disinfect excreta and bodies. It is also used to prepare the 1:100 bleach solution.
- 1:100 bleach solution is used to disinfect surfaces, medical equipment, patient bedding, reusable protective clothing before it is laundered, rising gloves between contact with each patient, rinsing gloves, apron and boots before leaving the patient's room, disinfecting contaminated waste for disposal.
- The dilutions mentioned pertain to a starting concentration of 5% active chlorine, so the 1:10 solution is 0.5% and the 1:100 is 0.05%.
- These solutions must be prepared new each day as they lose their strength after 24 hours.
Waste Disposal[edit | edit source]
- Direct, unprotected contact during disposal of infectious waste can result in accidental transmission of VHF. For this reason, all contaminated waste produced in the care of the VHF patient must be disposed of safely. All non-reusable items should be destroyed so they cannot be used again. Burning should be carried out at least daily.
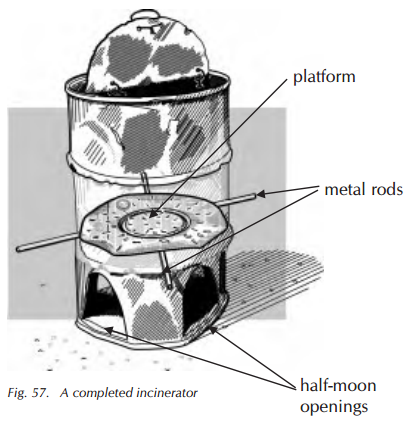
Prevention Lassa Fever CDC.png[5][2] - Liquid waste, including patient excreta, can be disposed of in an isolated latrine or toilet set aside for VHF cases. Burning is the recommended method for disposal of other VHF-contaminated waste. A safe and inexpensive disposal system can be made by using an incinerator or a pit for burning. Use fuel to accelerate the burning and ensure that all waste is completely destroyed.
Burial Practice[edit | edit source]
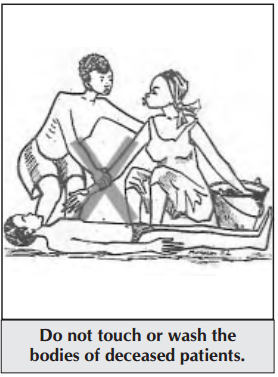
- There is risk of transmission in the health facility when a VHF patient dies because the bodies and body fluids of deceased VHF patients remain contagious for several days after death. Family and community members are also at risk if burial practices involve touching and washing the body.
- Burial should take place as soon as possible after the body is prepared in the health facility. Health facility staff should prepare the body safely and instruct families on what is and is not safe.
- To prepare the body, protective clothing is recommended per usually with a second pair of thick rubber gloves. The body and the area around it is sprayed with 1:10 bleach solution. The body is placed in a “body bag” (mortuary sack) and it is closed securely. The body bag is sprayed with 1:10 bleach solution. The body is then transported to the burial site as soon as possible. Any person who must touch or carry the body during transport should wear the same protective clothing as is worn in the isolation area. The grave should be at least 2 meters deep. Viewing the body is not possible and the burial ceremony should be limited to family only. The interior of the vehicle where the body was carried should be rinsed with 1:10 bleach solution.
Community Education[edit | edit source]
- Community education and involvement is an important part of the prevention of the spread of VHF
References[edit | edit source]
 KSF
KSF