Antibiotic use in livestock
 From Wikipedia - Reading time: 45 min
From Wikipedia - Reading time: 45 min

The use of antibiotics in the husbandry of livestock includes treatment when ill (therapeutic), treatment of a group of animals when at least one is diagnosed with clinical infection (metaphylaxis[1]), and preventative treatment (prophylaxis). Antibiotics are an important tool to treat animal as well as human disease, safeguard animal health and welfare, and support food safety.[2] However, used irresponsibly, this may lead to antibiotic resistance which may impact human, animal and environmental health.[3][4][5][6]
While levels of use vary dramatically from country to country, for example some Northern European countries use very low quantities to treat animals compared with humans,[7][8] worldwide an estimated 73% of antimicrobials (mainly antibiotics) are consumed by farm animals.[9] Furthermore, a 2015 study also estimates that global agricultural antibiotic usage will increase by 67% from 2010 to 2030, mainly from increases in use in developing BRIC countries.[10]
Increased antibiotic use is a matter of concern as antibiotic resistance is considered to be a serious threat to human and animal welfare in the future, and growing levels of antibiotics or antibiotic-resistant bacteria in the environment could increase the numbers of drug-resistant infections in both.[11] Bacterial diseases are a leading cause of death and a future without effective antibiotics would fundamentally change the way modern human as well as veterinary medicine is practised.[11][12][13]
Legislation and other curbs on antibiotic use in farm animals are now being introduced across the globe.[14][15][16] In 2017, the World Health Organization strongly suggested reducing antibiotic use in animals used in the food industry.[17] The use of antibiotics for growth promotion purposes was banned in the European Union from 2006,[18] and the use of sub-therapeutic doses of medically important antibiotics in animal feed and water[19] to promote growth and improve feed efficiency became illegal in the United States on 1 January 2017, through regulatory change enacted by the Food and Drug Administration (FDA), which sought voluntary compliance from drug manufacturers to re-label their antibiotics.[20][21]
History
[edit]The 2018 book 'Pharming animals: a global history of antibiotics in food production (1935–2017)'[22] summarises the central role antibiotics have played in agriculture: "Since their advent during the 1930s, antibiotics have not only had a dramatic impact on human medicine, but also on food production. On farms, whaling and fishing fleets as well as in processing plants and aquaculture operations, antibiotics were used to treat and prevent disease, increase feed conversion, and preserve food. Their rapid diffusion into nearly all areas of food production and processing was initially viewed as a story of progress on both sides of the Iron Curtain."[22][citation needed]
To retrace, while natural antibiotics or antibacterials were known to ancient man, antibiotics came to the fore during World War II to help treat war time casualties. It is recorded that antibiotics were first used in farming towards the end of the war, in the form of intra-mammary penicillin preparations to treat bovine mastitis.[23] At that time, milk was seen as an agricultural product which was highly susceptible to bacterial contamination, and farmers welcomed the opportunity to 'purify' their produce for the safety of consumers; it was only later that concern switched from the bacterial load of the product to the residues that might result from untimely or unregulated treatment.[24]
The use of antibiotics to treat and prevent disease has followed a similar path to that used in human medicine in terms of therapeutic and metaphylactic[1] applications to treat and manage disease and improve population health, and the application of case-by-case strategic preventative treatments when animals are deemed at particular risk. However, in the late 1940s, studies examining the supplementation of B12 in chicks' diets found that B12 produced from the fermentation of Streptomyces aureofaciens, an antibiotic for use in human medicine, produced a better weight gain for chicks than B12 supplied from other sources, and a reduced amount of feed to bring the birds to market weight.[25] Further studies on other livestock species showed a similar improved growth and feed efficiency effect with the result that as the cost of antibiotics came down, they were increasingly included at low ('sub-therapeutic') levels in livestock feed as a means of increasing production of affordable animal protein to meet the needs of a rapidly-expanding post-war population.[23] This development coincided with an increase in the scale of individual farms and the level of confinement of the animals on them, and so routine preventative antibiotic treatments became the most cost-effective means of treating the anticipated disease that could sometimes arise as a result.[23] Veterinary medicine increasingly embraced the therapeutic, metaphylactic and strategic preventative use of antibiotics to treat disease. The routine use of antibiotics for growth stimulation and disease prevention also grew.[citation needed]
Antibiotic usage in the UK has been banned since 2006 – however in 2017, 73% of all antibiotics sold globally were used in animals for food production.[26]
Growth stimulation
[edit]In 1910 in the United States, a meat shortage resulted in protests and boycotts.[27][28] After this and other shortages, the public demanded government research into stabilization of food supplies.[27] Since the 1900s, livestock production on United States farms has had to rear larger quantities of animals over a short period of time to meet new consumer demands. It was discovered in the 1940s that feeding subtherapeutic levels of antibiotics improved feed efficiency and accelerated animal growth.[29] Following this discovery, American Cyanamid published research establishing the practice of using antibiotic growth promoters.[27] By 2001, this practice had grown so much that a report by the Union of Concerned Scientists found that nearly 90% of the total use of antimicrobials in the United States was for non-therapeutic purposes in agricultural production.[30] Certain antibiotics, when given in low, subtherapeutic doses, are known to improve feed conversion efficiency (more output, such as muscle or milk, for a given amount of feed) and may promote greater growth, most likely by affecting gut flora.[31] The drugs listed below can be used to increase feed conversion ratio and weight gain, but are not legally allowed to be used for such purposes any longer in the United States. Some drugs listed below are ionophores, which are coccidiostats and not classified as antibiotics in many countries; they have not been shown to increase risk of antibiotic-resistant infections in humans.[citation needed]
| Antibiotic Growth Promoters historically used in Livestock Production in some countries | ||||
|---|---|---|---|---|
| Drug | Class | Livestock | ||
| Bacitracin | Peptide | Beef cattle, chickens, swine, and turkeys; promotes egg production in chickens[32][33] | ||
| Bambermycin | Beef cattle, chickens, swine, and turkeys.[32][33] | |||
| Carbadox | Swine[32] | |||
| Colistin | Swine[34] | |||
| Laidlomycin | Beef cattle[32] | |||
| Lasalocid | Ionophore | Beef cattle[32][33] | ||
| Lincomycin | Chickens and swine[32] | |||
| Monensin | Ionophore | Beef cattle and sheep; promotes milk production in dairy cows[32][33] | ||
| Neomycin/ Oxytetracycline | Beef cattle, chickens, swine, and turkeys[32] | |||
| Penicillin | Chickens, swine, and turkeys[32] | |||
| Roxarsone | Chickens and turkeys[32] | |||
| Salinomycin | Ionophore | |||
| Tylosin | Chickens and swine[32] | |||
| Virginiamycin | Peptide | Beef cattle, chickens, swine, turkeys[32][33] | ||
The practice of using antibiotics for growth stimulation has been deemed problematic for these following reasons:[35]
- It is the largest use of antimicrobials worldwide
- Subtherapeutic use of antibiotics results in bacterial resistance
- Every important class of antibiotics are being used in this way, making every class less effective
- The bacteria being changed harm humans
Antibiotic resistance
[edit]Genetic Basis of Antibiotic Resistance
[edit]Antibiotic resistance is a subset of antimicrobial resistance (AMR) through with bacteria develop mechanisms to withstand insults such as antibiotics which are meant to kill.[36] AMR refers to resistance by all microbes including viruses, fungi, parasites and bacteria to medicine .[37] This is a growing matter of concern as antibiotic resistance is considered to be a serious future threat to human welfare.[11] AMR is increasing in both developed and developing countries. If this trend continues without adequate intervention, the result may be infectious disease with no cure and vaccines.[38]
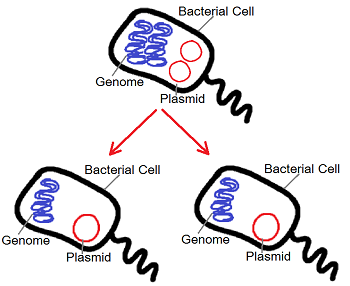
Bacteria from the same ecological niche as antibiotic-producing organisms have evolved ancient mechanisms to withstand the effect of the harmful antibiotics. Bacteria are still able to thrive in the presence of many environmental treats, including antibiotics. This unique ability is referred to as genetic plasticity.[39] Bacteria have two mechanism by which their genetics information can be altered to make them more resistant to treats - either by the mutation of their genes or by the acquisition of foreign DNA, which code for resistant genes.[39] The latter being the most important cause of antibiotic-resistant strains of bacteria in animals and humans. Bacteria may acquire these foreign genes through three processes: transformation, transduction and conjugation.[39]
Transformation is the process by which bacteria acquire naked DNA from the environment.[39] In transduction, bacteria acquire DNA from viruses via bacteriophages.[39] Conjugation is the direct transfer of DNA through cell-to-cell contact which is often mediated by plasmids.[39] Conjugative plasmids carry a number of beneficial gene and enable bacteria to exchange them among themselves to improve survival against antibiotics. This contributes to multi-drug resistant bacteria.[40]
Antibiotic resistance also occurs naturally, as it is a bacterium's response to any threat. Antibiotic-resistant bacteria have been found in pristine environments unrelated to human activity such as in the frozen and uncovered remains of woolly mammoths,[41] in the polar ice caps[42] and in isolated caves deep underground.[43] Antibiotic resistance can occurs if the bioavailability of antibiotics are too low to inhibit bacterial growth, which can trigger cellular responses in the bacteria that allow them to survive. These bacteria can then reproduce and spread their antibiotic-resistant genes to other generations, increasing their prevalence and ultimately leading to infections that cannot be healed by antibiotics.[44]
High priority antibiotics
[edit]The World Health Organization (WHO) published a revised list in 2019 of 'Critically Important Antimicrobials for Human Medicine, 6th revision'[45] with the intent that it be used "as a reference to help formulate and prioritise risk assessment and risk management strategies for containing antimicrobial resistance due to human and non-human antimicrobial use to help preserve the effectiveness of currently available antimicrobials. It lists its Highest Priority Critically Important Antimicrobials as: 3rd, 4th and 5th generation cephalosporins, glycopeptides, macrolides and ketolides, polymyxins including colistin, and quinolones including fluoroqinolones.[citation needed]
The European Medicines Agency (EMA) Antimicrobial Advice Ad Hoc Expert Group (AMEG) also published an updated categorisation[46] of different antibiotics in veterinary medicine by the antibiotic resistance risk to humans of using them alongside the need to treat disease in animals for health and welfare reasons. The categorisation specifically focuses on the situation in Europe. Category A ('Avoid') antibiotics are designated as 'not appropriate for use in food producing animals'. Category B ('Restrict') products, also known as Highest Priority Critically Important Antibiotics, are only to be used as a last resort. These include quinolones (such as fluoroquinolones), 3rd and 4th generation cephalosporins, and polymyxins, including colistin. A new intermediate Category C ('Caution') has been created for antibiotics which should be used when there is no available product in Category D ('Prudence') that would be clinically effective. Category C includes macrolides and aminoglycosides, with the exception of spectinomycin, which remains in Category D.[citation needed]
Evidence for the transfer of macrolide-resistant microorganisms from animals to humans has been scant,[47][48] and most evidence shows that pathogens of concern in human populations originated in humans and are maintained there, with rare cases of transference to humans. Macrolides are also extremely useful in the effective treatment of some Mycoplasma species in poultry, Lawsonia in pigs, respiratory tract infections in cattle and in some circumstances, lameness in sheep.[46]
Sources of antibiotic resistance
[edit]Summary
[edit]While the human medical use of antibiotics is the main source of antibiotic resistant infections in humans,[49][50][51] it is known that humans can acquire antibiotic resistance genes from a variety of animal sources, including farm animals, pets and wildlife.[52][53][54][55] Three potential mechanisms by which agricultural antibiotic use could lead to human disease have been identified as: 1 - direct infection with resistant bacteria from an animal source; 2 - breaches in the species barrier followed by sustained transmission in humans of resistant strains arising in livestock; 3 - transfer of resistance genes from agriculture into human pathogens.[56] While there is evidence of transmission of resistance from animals to humans in all three cases, either the scale is limited or causality is hard to establish. As Chang et al. (2014)[56] state: "The topic of agricultural antibiotic use is complex. As we noted ... many believe that agricultural antibiotics have become a critical threat to human health. While the concern is not unwarranted, the extent of the problem may be exaggerated. There is no evidence that agriculture is 'largely to blame' for the increase in resistant strains and we should not be distracted from finding adequate ways to ensure appropriate antibiotic use in all settings, the most important of which being clinical medicine."
Direct contact with animals
[edit]In terms of direct infection with resistant bacteria from an animals source, studies have shown that direct contact with livestock can lead to the spread of antibiotic-resistant bacteria. The risk appears greatest in those handling or managing livestock, for example in a study where resistant bacteria were monitored in farm labourers and neighbours after chickens receiving an antibiotic in their feed.[57] Manure may also contain antibiotic-resistant Staphylococcus aureus bacteria which can infect humans.[58][59] In 2017, the WHO included methicillin-resistant S. aureus (MRSA) in its priority list of 12 antibiotic-resistant bacteria, urging the need to search for new and more effective antibiotics against it. There also has been an increase in the number of bacterial pathogens resistant to multiple antimicrobial agents, including MRSA, which have recently emerged into different lineages. Some of them are associated with livestock and on-farm companion animals that are then able to be transmitted to humans, also called livestock-associated methicillin-resistant Staphylococcus aureus (LA-MRSA). These new lineages can be found on soft tissues of livestock workers, for example in their noses. A study looked at the association between exposure to livestock and the occurrence of LA-MRSA infection and observed that LA-MRSA infection was 9.64 times as likely to be found among livestock workers and veterinarians compared to their unexposed families and community members, showing that exposure to livestock significantly increases the risk of developing MRSA infection.[60][61] Although total numbers colonised by LA-MRSA remain low, and fewer still develop infection,[62][63] the condition is nonetheless rising in prevalence, difficult to treat, and has become a public health concern.[64] For companion animals without farm contact information about MRSA is still limited. Therefore, AMR surveillance should be extended, especially since antimicrobial use limitations for livestock are often extended to pets without further justification.[65]
Foodborne antibiotic resistance
[edit]Another way humans can be exposed to antibiotic-resistant bacteria is by pathogens on food.[66] In particular, If resistant bacteria are ingested by humans via food and then colonise the gut, they can cause infections which are unpleasant enough in themselves, but can be even harder to treat if they are serious enough to require antibiotic treatment but are also resistant to commonly-used antibiotics.[54][67] Campylobacter, Salmonella, E. coli and Listeria species are the most common foodborne bacteria.[68] Salmonella and Campylobacter alone account for over 400,000 Americans becoming sick from antibiotic-resistant infections every year.[69][70] Dairy products, ground minced beef and poultry are among the most common foods that can harbour pathogens both resistant and susceptible to antibiotics,[71] and surveillance of retail meats such as turkey, chicken, pork and beef have found Enterobacteriaceae. While some studies have established connections between antibiotic resistant infections and food-producing animals,[72][73] others have struggled to establish causal links, even when examining plasmid-mediated resistance.[74][75][76][77] Standard precautions such as pasteurising, or preparing and cooking meat properly, food preservation methods, and effective hand washing can help eliminate, decrease, or prevent spread of and infection from these and other potentially harmful bacteria.[78]
Other sources of resistance
[edit]As well as via food, E. coli from a variety of sources can also cause urinary and bloodstream infections. While one study suggests a large proportion of resistant E. coli isolates causing bloodstream infections in people could emanate from livestock produced for food,[79] other studies have since contradicted this, finding little commonality between resistance genes from livestock sources and those found in human infections, even when examining plasmid-mediated resistance.[76][80][81]
The use of antibiotics in livestock also has the potential to introduce antibiotic-resistant bacteria to humans via environmental exposure or inhalation of airborne bacteria. Antibiotics given to livestock in sub-therapeutic concentrations to stimulate growth when there is no diagnosis of disease – a practice still permitted in some countries – may kill some, but not all, of the bacterial organisms in the animal, possibly leaving those that are naturally antibiotic-resistant in the environment. Hence the practice of using antibiotics for growth stimulation could result in selection for resistance.[82][83] Antibiotics are not fully digested and processed in the animal or human gut, therefore, an estimated 40–90% of the antibiotics ingested are excreted in urine and/or faeces.[84][85] This means that as well as finding antibiotics in human sewage and animal manure, both can also contain antibiotic-resistant bacteria which have developed in vivo or in the environment. When animal manures are stored inadequately or applied as fertiliser, this can then spread bacteria to crops and into run-off water.[4][84] Antibiotics have been found in small amounts in crops grown in fertilised fields,[86] and detected in runoff from animal waste-fertilised land.[87] Composting has been shown to reduce the presence of various antibiotics by 20–99%,[84] but one study found that chlortetracycline, an antibiotic used in livestock feed in China, degraded at different rates dependent on the animal it was fed to, and that manure composting was not sufficient to ensure the microbial degradation of the antibiotic.[88]
Public Health Impact and Antimicrobial Resistance
The widespread use of antibiotics in livestock is closely linked to the growing threat of antimicrobial resistance (AMR) in humans. When animals are routinely administered antibiotics—particularly for growth promotion or disease prevention—resistant bacteria can develop. These bacteria may spread to humans through several pathways, including the food supply, direct animal contact, and environmental contamination, such as water runoff from farms.
Transmission through foodborne routes is considered especially significant in industrialized countries. Pathogens like Salmonella enterica, Campylobacter jejuni, Campylobacter coli, and Yersinia enterocolitica are typically transmitted via contaminated food. For other resistant bacteria, such as methicillin-resistant Staphylococcus aureus (MRSA), direct contact between humans and animals is the primary mode of transmission.[89]
Additionally, bacteria and antibiotic residues from food-animal production are widely dispersed into the environment, primarily through manure. This environmental contamination affects local microbial communities and wildlife, turning both into potential reservoirs for resistance. These environmental sources can, in turn, reintroduce resistant bacteria back into human and animal populations.
Global health experts have increasingly warned of the serious consequences of AMR. According to Dame Sally Davies, the United Kingdom's Special Envoy on Antimicrobial Resistance, more than 1.2 million people die each year from drug-resistant infections, with antibiotic use in animal agriculture being a significant contributing factor. The Review on Antimicrobial Resistance, chaired by Jim O’Neill, projected that without bold policies, annual deaths from AMR could rise to 10 million by 2050—surpassing current cancer mortality.[90]
The World Health Organization (WHO) supports these projections, estimating that AMR could lead to 10 million deaths annually by 2050 if no action is taken.[91] Currently, at least 700,000 people die each year from drug-resistant infections, including approximately 230,000 deaths from multidrug-resistant tuberculosis.[92] In addition to the health burden, the economic impact of uncontrolled AMR could rival that of the 2008–2009 global financial crisis [93]
Recognizing the interconnectedness of human, animal, and environmental health, the WHO and other international bodies emphasize the need for a coordinated "One Health" approach to mitigate the spread of antimicrobial resistance. This strategy calls for global cooperation across sectors to improve antibiotic stewardship, strengthen surveillance systems, and promote sustainable alternatives to antibiotic use in agriculture.
Global positions on antibiotic use in farm animals
[edit]In 2017, the World Health Organization (WHO) recommended reducing antibiotic use in animals used in the food industry. Due to the increasing risk of antibiotic resistant bacteria, the WHO strongly suggested restrictions on antibiotics being used for growth promotion and antibiotics used on healthy animals. Animals that require antibiotics should be treated with antibiotics that pose the smallest risk to human health.[17] HSBC also produced a report in October 2018 warning that the use of antibiotics in meat production could have "devastating" consequences for humans. It noted that many dairy and meat producers in Asia and the Americas had an economic incentive to continue high usage of antibiotics, particularly in crowded or unsanitary living conditions.[94]
However, the World Organisation for Animal Health has acknowledged the need to protect antibiotics but argued against a total ban on antibiotic use in animal production.[95] A total ban on antibiotics might drastically reduce protein supply in some parts of the world,[96] and when use of antibiotics is reduced or eliminated in livestock through legislation or voluntarily, both animal health and welfare and economic impacts can be negatively affected.[97][98] For example, experiences from farms where antibiotic use has been cut back or eliminated in the interests of meeting a consumer demand for 'antibiotic-free' or 'reared without antibiotics' produce have been shown to have a detrimental effect on animal health and welfare.[99][100][101] When antibiotics are used sub-therapeutically (for animal performance, increased growth, and improved feed efficiency), then the costs of meat, eggs, and other animal products are lowered.[102] One big argument against the restriction of antibiotic use is the potential economic hardship that would result for producers of livestock and poultry that could also result in higher cost for consumers. In a study analysing the economic cost of the FDA restricting all antibiotic use in animal livestock, it was estimated that the restriction would cost consumers approximately $1.2 billion to $2.5 billion per year.[102] In order to determine the overall economic impact of restricting antibiotic use, the financial cost must be weighed against the health benefits to the population. Since it is difficult to estimate the value of potential health benefits, the study concluded that the complete economic impact of restricting antibiotic use has not yet been determined.[102]
Although quantifying health benefits may be difficult, the economic impact of antibiotic restriction in animals can also be evaluated through the economic impact of antibiotic resistance in humans, which is a significant outcome of antibiotic use in animals. The World Health Organization identifies antibiotic resistance as a contributor to longer hospital stays and higher medical costs.[103] When infections can no longer be treated by typical first-line antibiotics, more expensive medications are required for treatment. When illness duration is extended by antibiotics resistance, the increased health care costs create a larger economic burden for families and societies.[103] The Center for Infectious Disease Research and Policy estimates approximately $2.2 billion in antibiotic resistance- related healthcare costs each year.[104] So while restricting antibiotics in animals causes a significant economic burden, the outcome of antibiotic resistance in humans that is perpetuated by antibiotic use in animals carries comparable economic burdens.[citation needed]
Use and regulation by country
[edit]

The use of medicines to treat disease in food-producing animals is regulated in nearly all countries, although some countries prescription-control their antibiotics, meaning only qualified veterinary surgeons can prescribe and in some cases dispense them.[105] Historically, the restrictions have existed to prevent contamination of mainly meat, milk, eggs and honey with chemicals that are in any way harmful to humans. Treating a sick animal with medicines may lead the animal product containing some of those medicines when the animal is slaughtered, milked, lays eggs or produces honey, unless withdrawal periods are adhered to which stipulate a period of time to ensure the medicines have left the animal's system sufficiently to avoid any risk.[106] Scientific experiments provide data for each medicine in each application, showing how long it is present in the body of an animal and what the animal's body does to metabolise the medicine. By the use of 'drug withdrawal periods' before slaughter or the use of milk or eggs from treated animals, veterinarians and animal owners ensure that the meat, milk and eggs is safe and free of any contamination.[107] However, some countries have also banned or heavily controlled routine use of antibiotics for growth stimulation or the preventative control of disease arising from deficiencies in management or facilities. This is not over concerns about residues, but about the growth of antibiotic resistance.
Brazil
[edit]Brazil is the world's largest exporter of beef. The government regulates antibiotic use in the cattle production industry.[108] The beef cattle industry in Brazil is based on grass-fed animals in which the Nellore breed predominates. The volume of antimicrobials used is not officially published in Brazil. Case studies conducted on farms in Brazil are the only way to get estimates and data of antimicrobial use. National Action Plan on Antimicrobial Resistance in Agriculture was set in place to contain the rise in antimicrobial resistance and limit the use of antibiotics in livestock production. Not all antimicrobials are banned in Brazil; treatment for therapeutic, metaphylactic, and prophylactic reasons are allowed.[109]
Canada
[edit]Because of concerns about antibiotics residues getting into the milk or meat of cattle, the Canadian Food Inspection Agency (CFIA) enforces standards which protect consumers by ensuring that foods produced will not contain antibiotics at a level which will cause harm to consumers. In Canada the veterinary drug regulation consists of two federal government agencies, namely Health Canada and the CFIA, which are responsible for implementing and enforcing the Food and Drugs Act. Testing samples for drug residues include three methods: monitoring, surveillance, and compliance. There are Swab Test On Premises (STOP) procedures to detect antibiotic residues in kidney tissues.[110]
China
[edit]China produces and consumes the most antibiotics of all countries.[111] Antibiotic use has been measured by checking the water near factory farms in China[112][113] as well as through animal faeces.[114] It was calculated that 38.5 million kg (or 84.9 million lbs) of antibiotics were used in China's swine and poultry production in 2012.[115] The abuse of antibiotics caused severe pollution of soil and surface water in Northern China.[116]
In 2012, U.S. News & World Report described the Chinese government's regulation of antibiotics in livestock production as "weak".[117]
On the UK 5-Year Antimicrobial Resistance (AMR) Strategy 2013–2018, the importance of addressing AMR negative effects on animal health has been considered as same as human health. Several scientific partnerships with low-middle income countries would be established.[118] UK-China Newton fund has started to build multi-discipline collaboration cross the border to stop the increasing global burden caused by AMR.[119] To achieve the goal of citizen public health and food safety, "The National action Plan on Controlling Antibiotic-Resistance Bacteria on animal origins (2016–2020)" has been published by Ministry of Agriculture and Rural Affairs of People's Republic of China since 2017. This plan is fully integrated with the concept of one health. It covers not only the research and development, but also social context.
European Union
[edit]
In 1999, the European Union (EU) implemented an antibiotic resistance monitoring program and a plan to phase out antibiotic use for the purposes of growth promotion by 2006.[120] The European Union banned the use of antibiotics as growth agents starting on 1 January 2006 with Regulation (EC) No 1831/2003.[121] In Germany, 1,734 tons of antimicrobial agents were used for animals in 2011 compared with 800 tons for humans.[122] Sweden was the first country to ban all use of antibiotics as growth promoters in 1986 and played a big role in the EU-wide ban on antimicrobial use by extensive lobbying after joining EU in 1995.[123][124] Another strategy actively applied in Sweden is prudent usage of antibiotics by performing individual rather than group treatment (on average more than 90% of treatment is individual with tablets, injectables or intramammaries).[125] Denmark started cutting down drastically in 1994, now using 60% less.[126] In the Netherlands, the use of antibiotics to treat diseases increased after the ban on its use for growth purposes in 2006.[127]
In 2011, the European Parliament voted for a non-binding resolution that called for the end of the preventative use of antibiotics in livestock.[128]
A revised regulation on veterinary medicinal products, proposed in procedure 2014/0257/COD, proposed limiting the use of antibiotics in prophylaxis and metaphylaxis. An agreement on the regulation between the Council of the European Union and the European Parliament was confirmed on 13 June 2018,[129][130] and the new Veterinary Medicines Regulation (Regulation (EU) 2019/6) is due to come into effect on 28 January 2022.[131]
India
[edit]In 2011 the Indian government proposed a "National policy for containment of antimicrobial resistance".[132] Other policies set schedules for requiring that food producing animals not be given antibiotics for a certain amount of time before their food goes to market.[133][134] A study released by Centre for Science and Environment (CSE) on 30 July 2014 found antibiotic residues in chicken. This study claims that Indians are developing resistance to antibiotics – and hence falling prey to a host of otherwise curable ailments. Some of this resistance might be due to large-scale unregulated use of antibiotics in the poultry industry. CSE finds that India has not set any limits for antibiotic residues in chicken and says that India will have to implement a comprehensive set of regulations including banning of antibiotic use as growth promoters in the poultry industry. Not doing this will put lives of people at risk.[135]
New Zealand
[edit]In 1999 the New Zealand government issued a statement that they would not then ban the use of antibiotics in livestock production.[136] In 2007 ABC Online reported on antibiotic use in chicken production in New Zealand.[137] In 2017, New Zealand published a new action plan to address the ongoing concern of antimicrobial resistance (AMR). The action plan outlined five objectives with each objective looking both at AMR in humans and AMR in agriculture.[138] Compared to other countries, New Zealand has a very low prevalence of AMR in animals and plants. This is due to their low use of antibiotics in animal treatment.[139]
South Korea
[edit]In 1998 some researchers reported use in livestock production was a factor in the high prevalence of antibiotic-resistant bacteria in Korea.[140] In 2007 The Korea Times noted that Korea has relatively high usage of antibiotics in livestock production.[141] In 2011, the Korean government banned the use of antibiotics as growth promoters in livestock.[142]
United Kingdom
[edit]As with other countries in Europe, use of antibiotics for growth promotion was banned in 2006.[18] Less than one third of all antibiotics sold in the UK are now estimated to be used to treat or prevent disease in farmed animals, following a revision to the 2017 sales data published by the UK Government's Veterinary Medicines Directorate.[143][144] Furthermore, 2018 sales data[145] estimated use at 29.5 mg antibiotics per kg of animal at time of treatment during that year. This represents a 53% reduction in sales of antibiotics to treat food-producing animals over five years.[146] The reduction has largely been achieved without legislation, and has been credited to voluntary industry action coordinated by the Responsible Use of Medicines in Agriculture (RUMA) Alliance[147] through a 'Targets Task Force' comprising a prominent veterinary surgeon and farmer from each livestock enterprise.[148] A European comparison of 2017 sales data found the UK had the fifth lowest sales in Europe during that year, with 2018 comparisons due to be released towards the end of 2020.[7]
While sales data give an overview of levels of use, products are often licensed for use in many species and therefore it is not possible to determine levels of use in different species without more specific usage data from each sector. In 2011, British Poultry Council members, representing 90% of the UK poultry meat industry, formed a stewardship programme that started recording antibiotics used to treat birds in the poultry meat sector in 2012. The first report was published in 2016 and reported a 44% reduction in antibiotic use between 2012 and 2015.[149] Since then, the organisation has produced three further reports, with the 2019 report confirming that the sector is maintaining reductions of over 80% in total use since it started its stewardship group, as well as reducing use of Highest Priority Critically Important Antibiotics by over 80% by stopping use of 3rd and 4th generation cephalosporins in 2012 and colistin in 2016, and only using macrolides and fluoroquinolones as a last resort. Preventative use of antibiotics has also stopped.[citation needed]
As many products are licensed for use in poultry and pigs, the increasing transparency around use in the UK poultry meat sector motivated the UK pig sector to set up a stewardship programme in 2016[150] through the National Pig Association. In 2017, an electronic Medicine Book for pigs (eMB-Pigs) was launched by levy body Agriculture and Horticulture Development Board.[151] eMB-Pigs provides a centralised electronic version of the existing paper or electronic medicine book kept on farms, and allows pig producers to record and quantify their individual use of medicines for easy review with the veterinary surgeon, at the same time as capturing use on each farm so that data can be collated to provide national usage figures. After it became a requirement of Red Tractor farm assurance for pigs[152] that annual, aggregated records of antibiotic use must be logged on the eMB system, data released May 2018 showed that according to records covering 87% of the UK slaughter pig population, antibiotic use had halved between 2015 and 2017,[153] Data for 2018 confirms that overall antibiotic use in the UK pig sector fell further, by 60% from the estimated 2015 figure,[154] to 110 mg/kg. Use of Highest Priority Critically Important Antibiotics also fell to 0.06 mg/kg,[155] a reduction of 95% from 2015, with use of colistin almost nil.
Factors such as levels of infectious disease domestically or internationally, weather and vaccine availability can all affect antibiotic use.[156] For example, the Scottish salmon farming sector worked with Government and researchers to introduce a vaccine for the disease Furunculosis (Aeromonas salmonicida) in 1994, which significantly reduced the need for antibiotic treatments,[157] but the trout sector is still without an effective vaccine for this disease. Lack of data can also make it difficult for farmers to know they compare with their peers or what they need to focus on, a particular problem for the sheep and cattle sectors in the UK, which are in the process of trying to set up their own electronic medicines hub to capture data.[156]
United States
[edit]In 1970 the FDA first recommended that antibiotic use in livestock be limited but set no actual regulations governing this recommendation.[19] By 2001, the Union of Concerned Scientists estimated that more than 70% of the antibiotics consumed in the US were given to food animals (for example, chickens, pigs, and cattle), in the absence of disease.[158][159]
In 2004 the Government Accountability Office (GAO) heavily critiqued the FDA for not collecting enough information and data on antibiotic use in factory farms. From this, the GAO concluded the FDA did not have enough information to create effective policy changes regarding antibiotic use. In response, the FDA said more research was being conducted and voluntary efforts within the industry would solve the problem of antibiotic resistance.[160] However, by 2011, a total of 13.6 million kg (30 million lb) of antimicrobials were sold for use in food-producing animals in the United States,[161] which represented 80% of all antibiotics sold or distributed in the United States.[162]
In March 2012, the United States District Court for the Southern District of New York, ruling in an action brought by the Natural Resources Defense Council and others, ordered the FDA to revoke approvals for the use of antibiotics in livestock that violated FDA regulations.[163] On 11 April 2012 the FDA announced a voluntary program to phase out unsupervised use of drugs as feed additives and convert approved over-the-counter uses for antibiotics to prescription use only, requiring veterinarian supervision of their use and a prescription.[164][165] In December 2013, the FDA announced the commencement of these steps to phase out the use of antibiotics for the purposes of promoting livestock growth.[158][166]
In 2015, the FDA approved a new Veterinary Feed Directive (VFD), an updated guideline giving instructions to pharmaceutical companies, veterinarians and producers about how to administer necessary drugs through the animal's feed and water.[167] Around the same time, the FDA published a report of antibiotics sold or distributed for food-producing animals which found that between 2009 and 2013, just over 60% were "medically important" drugs also used in humans;[161] the rest were from drug classes like ionophores, which are not used in human medicine.[168] Following this, the FDA asked drug companies to voluntarily edit its labels to exclude growth promotion as an indication for antibiotic usage. It subsequently reports that "Under Guidance for Industry (GFI) #213, which went into effect January 1, 2017, antibiotics that are important for human medicine can no longer be used for growth promotion or feed efficiency in cows, pigs, chickens, turkeys, and other food animals."[169] These new 2017 guidelines for instance prohibited using a drug off-label for non-therapeutic purposes, which would make using the re-labeled drug for growth enhancement illegal. In addition, some drugs were reclassified from 'Over the Counter' (OTC) to 'Veterinary Feed Directive' (VFD); VFD drugs require a veterinarian's authorization before they can be delivered in feed.[20][21][167][170] As a result, the FDA reported a 33% decrease from 2016 to 2017 in domestic sales of medically important antibiotics for use in livestock. Despite this progress, the Natural Resources Defense Council (NRDC) remains concerned that sales of antibiotics to the beef and pork industries remain elevated in 2017 compared with the poultry industries, and their use could still primarily be for preventing diseases in healthy animals, which further increases the threat on antibiotic resistance.[171] However, the FDA policy remains the same as it stated in 2013:[167]
The key aspect of FDA's strategy is the request that animal drug sponsors (those who own the right to market the product) voluntarily work with FDA to revise the approved use conditions for their medically important antimicrobial drug products to remove production uses (such as growth enhancement or feed efficiency), and bring the remaining therapeutic uses under veterinary oversight. Once manufacturers voluntarily make these changes, products can no longer be used for production purposes and therapeutic use of these products would require veterinary oversight.
Because of concerns about antibiotics residues getting into the milk or meat of cattle, in the United States, the government requires a withdraw period for any animal treated with antibiotics before it can be slaughtered, to allow residue to exit the animal.[172]
Some grocery stores have policies about antibiotic use in the animal whose produce they sell. In response to consumer concerns about the use of antibiotics in poultry, Perdue removed all human antibiotics from its feed in 2007 and launched the Harvestland brand, under which it sold products that met the requirements for an "antibiotic-free" label. In 2012 in the United States advocacy organization Consumers Union organized a petition asking the store Trader Joe's to discontinue the sale of meat produced with antibiotics.
- Gore, Al (2013). "The Reinvention of Life and Death: Antibiotics before Swine". The Future: Six Drivers of Global Change (First ed.). New York: Random House. pp. 227 and citation on 475. ISBN 9780812992946.
- Hurd, Scott (26 June 2012). "Commentary: 'Meat without Drugs' could be inhumane". Bovine Veterinarian. Retrieved 27 August 2013.
All peer-reviewed scientific risk assessments have demonstrated a negligible risk of human health harm due to livestock antibiotic use.
- Greenaway, Twilight (20 June 2012). "Your meat on drugs: Will grocery stores cut out antibiotics?". Grist. Retrieved 27 August 2013. By 2014, Perdue had also phased out ionophores from its hatchery and began using "antibiotic free" labels on some products,[173] and by 2015, 52% of the company's chickens were raised without the use of any type of antibiotics.[174]
The CDC and FDA do not now support the use of antibiotics for growth promotion because of evidence suggesting that antibiotics used for growth promotion purposes could lead to the development of resistant bacteria.[69] In addition to this, The Pew Charitable Trusts has stated that "hundreds of scientific studies conducted over four decades demonstrate that feeding low doses of antibiotics to livestock breeds antibiotic-resistant superbugs that can infect people".[175] The FDA, the U.S. Department of Agriculture and the Centers for Disease Control and Prevention have all testified before Congress that there is a definitive link between the routine, non-therapeutic use of antibiotics in food animal production and the challenge of antibiotic resistance in humans."[176] However, the National Pork Board, a government-owned corporation of the United States, has said: "The vast majority of producers use (antibiotics) appropriately."[177] In 2011 the National Pork Producers Council, an American trade association, also said, "Not only is there no scientific study linking antibiotic use in food animals to antibiotic resistance in humans, as the US pork industry has continually pointed out, but there isn't even adequate data to conduct a study."[178] The statement was issued in response to a United States Government Accountability Office report that asserts: "Antibiotic use in food animals contributes to the emergence of resistant bacteria that may affect humans".[160]
It is difficult to set up a comprehensive surveillance system for measuring rates of change in antibiotic resistance.[179] The US Government Accountability Office published a report in 2011 stating that government and commercial agencies had not been collecting sufficient data to make a decision about best practices.[160] There is also no regulatory agency in the United States that systematically collects detailed data on antibiotic use in humans and animals, which means it is not clear which antibiotics are prescribed for which purpose and at what time. While this may be lacking at a regulatory level, the US poultry meat sector has been working on the issue of data collection itself, and has now reported comparative data showing significant reductions in antibiotic use.[180] Among the highlights in the report[181] was a 95% decrease in in-feed tetracycline use in broiler chicks from 2013 to 2017, a 67% reduction in in-feed use of tetracycline in turkeys, and a 42% drop in hatchery use of gentamicin in turkey poults. This is an encouraging sign; the 53% overall reduction in antibiotic use seen in the UK between 2013 and 2018[145][146] was initiated from a voluntary stewardship programme developed by the UK poultry meat sector.[149]
Research into alternatives
[edit]
Increasing concern due to the emergence of antibiotic-resistant bacteria has led researchers to look for alternatives to using antibiotics in livestock.[182]
Probiotics, cultures of a single bacteria strain or mixture of different strains, are being studied in livestock as a production enhancer.[183]
Prebiotics are non-digestible carbohydrates. The carbohydrates are mainly made up of oligosaccharides which are short chains of monosaccharides. The two most commonly studied prebiotics are fructooligosaccharides (FOS) and mannanoligosaccharides (MOS). FOS has been studied for use in chicken feed. MOS works as a competitive binding site, as bacteria bind to it rather than the intestine and are carried out.[184]
Bacteriophages are able to infect most bacteria and are easily found in most environments colonized by bacteria, and have been studied as well.[182]
In another study it was found that using probiotics, competitive exclusion, enzymes, immunomodulators and organic acids prevents the spread of bacteria and can all be used in place of antibiotics.[185] Another research team was able to use bacteriocins, antimicrobial peptides and bacteriophages in the control of bacterial infections.[186] While further research is needed in this field, alternative methods have been identified in effectively controlling bacterial infections in animals.
Other alternatives include preventative approaches to keep the animals healthier and so reduce the need for antibiotics. These include improving the living conditions for animals, stimulating natural immunity through better nutrition, increasing biosecurity, implementing better management and hygiene practices, and ensuring better use of vaccination.[96]
See also
[edit]- Antibiotic misuse
- Antimicrobial resistance
- Antibiotics in poultry farming in America
- Subtherapeutic antibiotic use in swine
- Antibiotic prophylaxis
- List of antibiotic-resistant bacteria
References
[edit]- ^ a b Bousquet-Melou, Alain; Ferran, Aude; Toutain, Pierre-Louis (May 2010). "Prophylaxis & Metaphylaxis in Veterinary Antimicrobial Therapy". Conference: 5th International Conference on Antimicrobial Agents in Veterinary Medicine (AAVM)At: Tel Aviv, Israel – via ResearchGate.
- ^ British Veterinary Association, London (May 2019). "BVA policy position on the responsible use of antimicrobials in food producing animals" (PDF). Retrieved 22 March 2020.
- ^ Massé, Daniel; Saady, Noori; Gilbert, Yan (4 April 2014). "Potential of Biological Processes to Eliminate Antibiotics in Livestock Manure: An Overview". Animals. 4 (2): 146–163. doi:10.3390/ani4020146. PMC 4494381. PMID 26480034. S2CID 1312176.
- ^ a b Sarmah, Ajit K.; Meyer, Michael T.; Boxall, Alistair B. A. (1 October 2006). "A global perspective on the use, sales, exposure pathways, occurrence, fate and effects of veterinary antibiotics (VAs) in the environment". Chemosphere. 65 (5): 725–759. Bibcode:2006Chmsp..65..725S. doi:10.1016/j.chemosphere.2006.03.026. PMID 16677683.
- ^ Kumar, Kuldip; C. Gupta, Satish; Chander, Yogesh; Singh, Ashok K. (1 January 2005). "Antibiotic Use in Agriculture and Its Impact on the Terrestrial Environment". Advances in Agronomy. 87: 1–54. doi:10.1016/S0065-2113(05)87001-4. ISBN 9780120007851.
- ^ Boeckel, Thomas P. Van; Glennon, Emma E.; Chen, Dora; Gilbert, Marius; Robinson, Timothy P.; Grenfell, Bryan T.; Levin, Simon A.; Bonhoeffer, Sebastian; Laxminarayan, Ramanan (29 September 2017). "Reducing antimicrobial use in food animals". Science. 357 (6358): 1350–1352. Bibcode:2017Sci...357.1350V. doi:10.1126/science.aao1495. PMC 6510296. PMID 28963240. S2CID 206662316.
- ^ a b ESVAC (European Medicines Agency) (October 2019). "Sales of veterinary antimicrobial agents in 31 European countries in 2017: Trends from 2010 to 2017" (PDF). Retrieved 22 March 2020.
- ^ Torrella, Kenny (8 January 2023). "Big Meat just can't quit antibiotics". Vox. Retrieved 23 January 2023.
- ^ Boeckel, Thomas P. Van; Pires, João; Silvester, Reshma; Zhao, Cheng; Song, Julia; Criscuolo, Nicola G.; Gilbert, Marius; Bonhoeffer, Sebastian; Laxminarayan, Ramanan (20 September 2019). "Global trends in antimicrobial resistance in animals in low- and middle-income countries" (PDF). Science. 365 (6459): eaaw1944. doi:10.1126/science.aaw1944. ISSN 0036-8075. PMID 31604207. S2CID 202699175.
- ^ Van Boeckel, Thomas P.; Brower, Charles; Gilbert, Marius; Grenfell, Bryan T.; Levin, Simon A.; Robinson, Timothy P.; Teillant, Aude; Laxminarayan, Ramanan (2015). "Global trends in antimicrobial use in food animals". Proceedings of the National Academy of Sciences. 112 (18): 5649–5654. Bibcode:2015PNAS..112.5649V. doi:10.1073/pnas.1503141112. PMC 4426470. PMID 25792457. S2CID 3861749.
- ^ a b c Bush, Karen; Courvalin, Patrice; Dantas, Gautam; Davies, Julian; Eisenstein, Barry; Huovinen, Pentti; Jacoby, George A.; Kishony, Roy; Kreiswirth, Barry N.; Kutter, Elizabeth; Lerner, Stephen A.; Levy, Stuart; Lewis, Kim; Lomovskaya, Olga; Miller, Jeffrey H.; Mobashery, Shahriar; Piddock, Laura J. V.; Projan, Steven; Thomas, Christopher M.; Tomasz, Alexander; Tulkens, Paul M.; Walsh, Timothy R.; Watson, James D.; Witkowski, Jan; Witte, Wolfgang; Wright, Gerry; Yeh, Pamela; Zgurskaya, Helen I. (2 November 2011). "Tackling antibiotic resistance". Nature Reviews Microbiology. 9 (12): 894–896. doi:10.1038/nrmicro2693. PMC 4206945. PMID 22048738. S2CID 4048235.
- ^ Tang, Karen L; Caffrey, Niamh P; Nóbrega, Diego; Cork, Susan C; Ronksley, Paul C; Barkema, Herman W; Polachek, Alicia J; Ganshorn, Heather; Sharma, Nishan; Kellner, James D; Ghali, William A (November 2017). "Restricting the use of antibiotics in food-producing animals and its associations with antibiotic resistance in food-producing animals and human beings: a systematic review and meta-analysis". The Lancet Planetary Health. 1 (8): e316 – e327. doi:10.1016/S2542-5196(17)30141-9. PMC 5785333. PMID 29387833.
- ^ Shallcross, Laura J.; Howard, Simon J.; Fowler, Tom; Davies, Sally C. (5 June 2015). "Tackling the threat of antimicrobial resistance: from policy to sustainable action". Philosophical Transactions of the Royal Society B: Biological Sciences. 370 (1670): 20140082. doi:10.1098/rstb.2014.0082. PMC 4424432. PMID 25918440. S2CID 39361030.
- ^ European Medicines Agency (4 September 2019). "Implementation of the new Veterinary Medicines Regulation in the EU".
- ^ OECD, Paris (May 2019). "Working Party on Agricultural Policies and Markets: Antibiotic Use and Antibiotic Resistance in Food Producing Animals in China". Retrieved 22 March 2020.
- ^ US Food & Drug Administration (July 2019). "Timeline of FDA Action on Antimicrobial Resistance". Food and Drug Administration. Retrieved 22 March 2020.
- ^ a b "WHO guidelines on use of medically important antimicrobials in food-producing animals" (PDF).
- ^ a b European Commission, Brussels (December 2005). "Ban on antibiotics as growth promoters in animal feed enters into effect".
- ^ a b "The Judicious Use of Medically Important Antimicrobial Drugs in Food-Producing Animals" (PDF). Guidance for Industry (#209). 2012. Archived from the original (PDF) on 3 July 2010.
- ^ a b "Veterinary Feed Directive (VFD) Basics". AVMA. Archived from the original on 15 April 2017. Retrieved 14 March 2017.
- ^ a b University of Nebraska, Lincoln (October 2015). "Veterinary Feed Directive Questions and Answers". UNL Beef. Retrieved 14 March 2017.
- ^ a b Kirchelle, Claas (7 August 2018). "Pharming animals: a global history of antibiotics in food production (1935–2017)". Palgrave Communications. 4. doi:10.1057/s41599-018-0152-2. S2CID 51934013.
- ^ a b c Gustafson, R. H.; Bowen, R. E. (1997). "Antibiotic use in animal agriculture". Journal of Applied Microbiology. 83 (5): 531–541. doi:10.1046/j.1365-2672.1997.00280.x. ISSN 1365-2672. PMID 9418018. S2CID 38409567.
- ^ SMITH-HOWARD, KENDRA (2010). "Antibiotics and Agricultural Change: Purifying Milk and Protecting Health in the Postwar Era". Agricultural History. 84 (3): 327–351. doi:10.3098/ah.2010.84.3.327. ISSN 0002-1482. JSTOR 27868996.
- ^ Stokstad, ELR; Jukes, TH; Pierce, J; Page, AC Jr.; Franklin, AL (1949). "The multiple nature of the animal protein factor". Journal of Biological Chemistry. 180 (2): 647–654. doi:10.1016/S0021-9258(18)56683-7. PMID 18135798 – via CAB Direct.
- ^ Balogun, Bukky; Sutherland, Nikki; Coe, Sarah. "The use of antibiotics on healthy farm animals and antimicrobial resistance - House of Commons Library".
- ^ a b c Ogle, Maureen (3 September 2013). "Riots, Rage and Resistance: A Brief History of How Antibiotics Arrived on the Farm". Scientific American. Retrieved 5 November 2013.
- ^ Reported locally in these:
- "To Become Vegetarians", Mansfield (O.) News, 17 January 1910, p2
- "150,000 at Cleveland Stop the Use of Meat" Syracuse Herald-Journal, 25 January 1910, p1
- "Boycott on Meat is Rapidly Spreading; Men Who Are Blamed For High Price", Atlanta Constitution, 25 January 1910, p1
- ^ Flores-Tejeida, L.B; Soto-Zarazua, G.M; Guevara-Gonzalez, R.G; Escamilla-Garcia, A.; Gomez-Soto, J.G (2018). "A review of hot and sweet pepper added in animal nutrition: Alternative against the use of antibiotics". 2018 XIV International Engineering Congress (CONIIN). pp. 1–6. doi:10.1109/CONIIN.2018.8489822. ISBN 978-1-5386-7018-7. S2CID 52986242.
- ^ "Hogging It!: Estimates of Antimicrobial Abuse in Livestock". Union of Concerned Scientists. 2001.
- ^ Reinhardt, Christopher. "Antimicrobial Feed Additives". Merck Veterinary Manual.
- ^ a b c d e f g h i j k l Allen, Heather K.; Stanton, Thad B. (1 January 2014). "Altered egos: antibiotic effects on food animal microbiomes". Annual Review of Microbiology. 68: 297–315. doi:10.1146/annurev-micro-091213-113052. ISSN 1545-3251. PMID 25002091.
- ^ a b c d e Reinhardt, Christopher D. (2012), "Antimicrobial Feed Additives", in Aiello, Susan E.; Moses, Michael A. (eds.), Merck Veterinary Manual, Merck & Co. and Merial
- ^ Schoenmakers, Kevin (21 October 2020). "How China is getting its farmers to kick their antibiotics habit". Nature. Retrieved 2 August 2021.
- ^ Silbergeld, E. K.; Graham, J.; Price, L. B. (2008). "Industrial Food Animal Production, Antimicrobial Resistance, and Human Health". Annual Review of Public Health. 29: 151–169. doi:10.1146/annurev.publhealth.29.020907.090904. PMID 18348709.
- ^ Habboush, Yacob; Guzman, Nilmarie (2025), "Antibiotic Resistance", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 30020649, retrieved 23 March 2025
- ^ "Antimicrobial resistance". www.who.int. Retrieved 23 March 2025.
- ^ "Drug-Resistant Infections: A Threat to Our Economic Future". World Bank. Retrieved 23 March 2025.
- ^ a b c d e f Munita, Jose M.; Arias, Cesar A. (April 2016). "Mechanisms of Antibiotic Resistance". Microbiology Spectrum. 4 (2). doi:10.1128/microbiolspec.VMBF-0016-2015. ISSN 2165-0497. PMC 4888801. PMID 27227291.
- ^ Bennett, P M (March 2008). "Plasmid encoded antibiotic resistance: acquisition and transfer of antibiotic resistance genes in bacteria: Plasmid-encoded antibiotic resistance". British Journal of Pharmacology. 153 (S1): S347 – S357. doi:10.1038/sj.bjp.0707607. PMC 2268074. PMID 18193080.
- ^ Perry, Julie; Waglechner, Nicholas; Wright, Gerard (June 2016). "The Prehistory of Antibiotic Resistance". Cold Spring Harbor Perspectives in Medicine. 6 (6): a025197. doi:10.1101/cshperspect.a025197. PMC 4888810. PMID 27252395.
- ^ Nesme, Joseph; Cecillon, Sebastien; Delmont, Tom; Monier, Jean-Michel; Vogel, Timothy; Simonet, Pascal (May 2014). "Large-Scale Metagenomic-Based Study of Antibiotic Resistance in the Environment". Current Biology. 24 (10): 1096–100. Bibcode:2014CBio...24.1096N. doi:10.1016/j.cub.2014.03.036. PMID 24814145. S2CID 15550895.
- ^ Bhullar, K; Waglechner, N; Pawlowski, A; Koteva, K; Banks, ED; Johnston, MD; Barton, HA; Wright, GD (2012). "Antibiotic resistance is prevalent in an isolated cave microbiome". PLOS ONE. 7 (4): e34953. Bibcode:2012PLoSO...734953B. doi:10.1371/journal.pone.0034953. PMC 3324550. PMID 22509370.
- ^ Ben, Yujie; Fu, Caixia; Hu, Min; Liu, Lei; Wong, Ming Hung; Zheng, Chunmiao (February 2019). "Human health risk assessment of antibiotic resistance associated with antibiotic residues in the environment: A review". Environmental Research. 169: 483–493. Bibcode:2019ER....169..483B. doi:10.1016/j.envres.2018.11.040. ISSN 1096-0953. PMID 30530088. S2CID 56488563.
- ^ World Health Organization (2018). "Critically Important Antimicrobials for Human Medicine, 6th Revision" (PDF). Retrieved 31 March 2020.
- ^ a b European Medicines Agency (January 2020). "Advice on impacts of using antimicrobials in animals". Retrieved 31 March 2020.
- ^ Hurd, H. Scott; Doores, Stephanie; Hayes, Dermot; Mathew, Alan; Maurer, John; Silley, Peter; Singer, Randall S.; Jones, Ronald N. (1 May 2004). "Public Health Consequences of Macrolide Use in Food Animals: A Deterministic Risk Assessment". Journal of Food Protection. 67 (5): 980–992. doi:10.4315/0362-028X-67.5.980. ISSN 0362-028X. PMID 15151237.
- ^ Hurd, H. Scott; Malladi, Sasidhar (June 2008). "A stochastic assessment of the public health risks of the use of macrolide antibiotics in food animals" (PDF). Risk Analysis. 28 (3): 695–710. Bibcode:2008RiskA..28..695H. doi:10.1111/j.1539-6924.2008.01054.x. ISSN 1539-6924. PMID 18643826. S2CID 8201863.
- ^ UK Government (10 September 2013). "UK 5 Year Antimicrobial Resistance Strategy 2013". Paragraph 2.1. Retrieved 22 March 2020.
- ^ The European Medicines Agency Committee for Medicinal Products for Veterinary Use (6 October 2016). "CVMP Strategy on Antimicrobials 2016–2020" (PDF). p. 4. Retrieved 22 March 2020.
- ^ Shea, Katherine M. (1 July 2003). "Antibiotic Resistance: What Is the Impact of Agricultural Uses of Antibiotics on Children's Health?". Pediatrics. 112 (Supplement 1): 253–258. doi:10.1542/peds.112.S1.253. ISSN 0031-4005. PMID 12837918. S2CID 8152452.
- ^ Graham, David W; Bergeron, Gilles; Bourassa, Megan W; Dickson, James; Gomes, Filomena; Howe, Adina; Kahn, Laura H; Morley, Paul S; Scott, H Morgan; Simjee, Shabbir; Singer, Randall S; Smith, Tara C; Storrs, Carina; Wittum, Thomas E (April 2019). "Complexities in understanding antimicrobial resistance across domesticated animal, human, and environmental systems". Annals of the New York Academy of Sciences. 1441 (1): 17–30. Bibcode:2019NYASA1441...17G. doi:10.1111/nyas.14036. PMC 6850694. PMID 30924539.
- ^ Marshall, Bonnie M; Levy, Stuart B (October 2011). "Food Animals and Antimicrobials: Impacts on Human Health". Clinical Microbiology Reviews. 24 (4): 718–733. doi:10.1128/CMR.00002-11. PMC 3194830. PMID 21976606.
- ^ a b Economou, Vangelis; Gousia, Panagiota (1 April 2015). "Agriculture and food animals as a source of antimicrobial-resistant bacteria". Infection and Drug Resistance. 8: 49–61. doi:10.2147/IDR.S55778. ISSN 1178-6973. PMC 4388096. PMID 25878509. S2CID 3789178.
- ^ Swartz, Morton N. (1 June 2002). "Human Diseases Caused by Foodborne Pathogens of Animal Origin". Clinical Infectious Diseases. 34 (Supplement_3): S111 – S122. doi:10.1086/340248. ISSN 1058-4838. PMID 11988881.
- ^ a b Chang, Qiuzhi; Wang, Weike; Regev-Yochay, Gili; Lipsitch, Marc; Hanage, William P. (March 2015). "Antibiotics in agriculture and the risk to human health: how worried should we be?". Evolutionary Applications. 8 (3): 240–247. Bibcode:2015EvApp...8..240C. doi:10.1111/eva.12185. PMC 4380918. PMID 25861382. S2CID 4167603.
- ^ Levy, SB; FitxGerald, GB; Macone, AB (September 1976). "Changes in intestinal flora of farm personnel after introduction of a tetracycline-supplemented feed on a farm". New England Journal of Medicine. 295 (11): 583–588. doi:10.1056/NEJM197609092951103. PMID 950974.
- ^ Zhang, Sarah (2013). "Pig-manure fertilizer linked to human MRSA infections". Nature News. doi:10.1038/nature.2013.13752.
- ^ Casey, Joan A.; Curriero, Frank C.; Cosgrove, Sara E.; Nachman, Keeve E.; Schwartz, Brian S. (25 November 2013). "High-Density Livestock Operations, Crop Field Application of Manure, and Risk of Community-Associated Methicillin-Resistant Staphylococcus aureus Infection in Pennsylvania". JAMA Internal Medicine. 173 (21): 1980–1990. doi:10.1001/jamainternmed.2013.10408. PMC 4372690. PMID 24043228.
- ^ Chen, Chen; Wu, Felicia (2018). "Livestock-Associated Methicillin-Resistant Staphylococcus Aureus (LA-MRSA) Colonization and Infection Among Livestock Workers and Veterinarians: A Systematic Review and Meta-Analysis". SSRN Electronic Journal. doi:10.2139/ssrn.3208968. ISSN 1556-5068.
- ^ Nadimpalli, M.; Rinsky, J. L.; Wing, S.; Hall, D.; Stewart, J.; Larsen, J.; Strelitz, J. (2015). "Persistence of livestock-associated antibiotic-resistant Staphylococcus aureus among industrial hog operation workers in North Carolina over 14 days". Occup Environ Med. 72 (2): 90–99. doi:10.1136/oemed-2014-102095. PMC 4316926. PMID 25200855. S2CID 8760462.
- ^ Anjum, Muna F.; Marco-Jimenez, Francisco; Duncan, Daisy; Marín, Clara; Smith, Richard P.; Evans, Sarah J. (12 September 2019). "Livestock-Associated Methicillin-Resistant Staphylococcus aureus From Animals and Animal Products in the UK". Frontiers in Microbiology. 10: 2136. doi:10.3389/fmicb.2019.02136. ISSN 1664-302X. PMC 6751287. PMID 31572341.
- ^ Risk Assessment on Methicillin-Resistant Staphylococcus aureus (MRSA), with a focus on Livestock-associated MRSA, in the UK Food Chain (Report). Food Standards Agency. February 2017. S2CID 46569353.
- ^ Livestock-associated Staphylococcus Aureus (LA-MRSA), Research topic. Retrieved from: https://www.frontiersin.org/research-topics/6689/livestock-associated-staphylococcus-aureus-la-mrsa
- ^ Feuer, Leonie; Frenzer, Stefanie Katharina; Merle, Roswitha; Leistner, Rasmus; Bäumer, Wolfgang; Bethe, Astrid; Lübke-Becker, Antina; Klein, Babette; Bartel, Alexander (15 July 2024). "Prevalence of MRSA in canine and feline clinical samples from one-third of veterinary practices in Germany from 2019-2021". The Journal of Antimicrobial Chemotherapy. 79 (9): –225. doi:10.1093/jac/dkae225. ISSN 1460-2091. PMID 39007221.
- ^ "Antibiotic Resistance Threats in the United States" (PDF). Centers for Disease Control and Prevention. Retrieved 30 December 2016.
- ^ Bortolaia V; et al. (February 2016). "Human health risks associated with antimicrobial-resistant enterococci and Staphylococcus aureus on poultry meat". Clinical Microbiology and Infection. 22 (2): 130–40. doi:10.1016/j.cmi.2015.12.003. PMID 26706616.
- ^ New South Wales Government. "Foodborne illness pathogens". Retrieved 31 March 2020.
- ^ a b CDC (10 September 2018). "Antibiotic Resistance and Food are Connected". Centers for Disease Control and Prevention. Retrieved 29 March 2019.
- ^ Center for Disease Control and Prevention (2013). Human Isolates Final Report (PDF). National Antibiotic Resistance Monitoring System: Enteric Bacteria (Report).
- ^ DeWaal, J. D.; Grooters, Susan Vaughn (May 2013). "Antibiotic Resistance in Foodborne Pathogens" (PDF). Center for Science in the Public Interest.
- ^ Angulo, F. J.; Molbak, K. (1 December 2005). "Human Health Consequences of Antimicrobial Drug-Resistant Salmonella and Other Foodborne Pathogens". Clinical Infectious Diseases. 41 (11): 1613–1620. doi:10.1086/497599. PMID 16267734.
- ^ Mølbak, Kåre; Baggesen, Dorte Lau; Aarestrup, Frank Møller; Ebbesen, Jens Munk; Engberg, Jørgen; Frydendahl, Kai; Gerner-Smidt, Peter; Petersen, Andreas Munk; Wegener, Henrik C. (4 November 1999). "An Outbreak of Multidrug-Resistant, Quinolone-Resistant Salmonella enterica Serotype Typhimurium DT104". New England Journal of Medicine. 341 (19): 1420–1425. doi:10.1056/NEJM199911043411902. PMID 10547404.
- ^ McCrackin, M. A.; Helke, Kristi L.; Galloway, Ashley M.; Poole, Ann Z.; Salgado, Cassandra D.; Marriott, Bernadette P. (2 October 2016). "Effect of Antimicrobial Use in Agricultural Animals on Drug-resistant Foodborne Campylobacteriosis in Humans: A Systematic Literature Review". Critical Reviews in Food Science and Nutrition. 56 (13): 2115–2132. doi:10.1080/10408398.2015.1119798. ISSN 1040-8398. PMID 26580432. S2CID 16481535.
- ^ Mather, A. E.; Reid, S. W. J.; Maskell, D. J.; Parkhill, J.; Fookes, M. C.; Harris, S. R.; Brown, D. J.; Coia, J. E.; Mulvey, M. R.; Gilmour, M. W.; Petrovska, L. (27 September 2013). "Distinguishable Epidemics of Multidrug-Resistant Salmonella Typhimurium DT104 in Different Hosts". Science. 341 (6153): 1514–1517. Bibcode:2013Sci...341.1514M. doi:10.1126/science.1240578. ISSN 0036-8075. PMC 4012302. PMID 24030491.
- ^ a b El Garch, Farid; de Jong, Anno; Bertrand, Xavier; Hocquet, Didier; Sauget, Marlène (2018). "mcr-1-like detection in commensal Escherichia coli and Salmonella spp. from food-producing animals at slaughter in Europe". Veterinary Microbiology. 213: 42–46. doi:10.1016/j.vetmic.2017.11.014. PMID 29292002.
- ^ Zaheer, Rahat; Cook, Shaun R.; Barbieri, Ruth; Goji, Noriko; Cameron, Andrew; Petkau, Aaron; Polo, Rodrigo Ortega; Tymensen, Lisa; Stamm, Courtney; Song, Jiming; Hannon, Sherry (2020). "Surveillance of Enterococcus spp. reveals distinct species and antimicrobial resistance diversity across a One-Health continuum". Scientific Reports. 10 (1): 3937. Bibcode:2020NatSR..10.3937Z. doi:10.1038/s41598-020-61002-5. ISSN 2045-2322. PMC 7054549. PMID 32127598.
- ^ United States Department of Agriculture (December 2016). "Cleanliness Helps Prevent Foodborne Illness". Retrieved 31 March 2020.
- ^ Vieira, Antonio R.; Collignon, Peter; Aarestrup, Frank M.; McEwen, Scott A.; Hendriksen, Rene S.; Hald, Tine; Wegener, Henrik C. (December 2011). "Association Between Antimicrobial Resistance in Escherichia coli Isolates from Food Animals and Blood Stream Isolates from Humans in Europe: An Ecological Study". Foodborne Pathogens and Disease. 8 (12): 1295–1301. doi:10.1089/fpd.2011.0950. PMID 21883007.
- ^ Dorado-García, Alejandro; Smid, Joost H.; van Pelt, Wilfrid; Bonten, Marc J. M.; Fluit, Ad C.; van den Bunt, Gerrita; Wagenaar, Jaap A.; Hordijk, Joost; Dierikx, Cindy M.; Veldman, Kees T.; de Koeijer, Aline (1 February 2018). "Molecular relatedness of ESBL/AmpC-producing Escherichia coli from humans, animals, food and the environment: a pooled analysis". Journal of Antimicrobial Chemotherapy. 73 (2): 339–347. doi:10.1093/jac/dkx397. ISSN 0305-7453. PMID 29165596. S2CID 3779506.
- ^ Ludden, Catherine; Raven, Kathy E.; Jamrozy, Dorota; Gouliouris, Theodore; Blane, Beth; Coll, Francesc; de Goffau, Marcus; Naydenova, Plamena; Horner, Carolyne; Hernandez-Garcia, Juan; Wood, Paul (22 January 2019). Sansonetti, Philippe J. (ed.). "One Health Genomic Surveillance of Escherichia coli Demonstrates Distinct Lineages and Mobile Genetic Elements in Isolates from Humans versus Livestock". mBio. 10 (1): e02693–18, /mbio/10/1/mBio.02693–18.atom. doi:10.1128/mBio.02693-18. ISSN 2150-7511. PMC 6343043. PMID 30670621.
- ^ Wegener, Henrik C. (2012). "A15 Antibiotic Resistance—Linking Human and Animal Health". In Choffnes, E.R.; Relman, D.A.; Olsen, L.; Hutton, R.; Mack, A. (eds.). Antibiotic Resistance — Linking Human And Animal Health: Improving Food Safety Through a One Health Approach Workshop Summary. Washington DC: National Academies Press. doi:10.17226/13423. ISBN 978-0-309-25937-8. PMID 23230579. NBK114485.
- ^ Wegener H (2003). "Antibiotics in animal feed and their role in resistance development". Current Opinion in Microbiology. 6 (5): 439–445. doi:10.1016/j.mib.2003.09.009. PMID 14572534.
- ^ a b c Zhang, X (2014). "Prevalence of veterinary antibiotics and antibiotic-resistant Escherichia coli in the surface water of a livestock production region in northern China". PLOS ONE. 9 (11): e111026. Bibcode:2014PLoSO...9k1026Z. doi:10.1371/journal.pone.0111026. PMC 4220964. PMID 25372873. S2CID 4154235.
- ^ Storteboom, Heather; Arabi, Mazdak; Davis, Jessica G.; Crimi, Barbara; Pruden, Amy (October 2010). "Tracking Antibiotic Resistance Genes in the South Platte River Basin Using Molecular Signatures of Urban, Agricultural, And Pristine Sources". Environmental Science & Technology. 44 (19): 7397–7404. Bibcode:2010EnST...44.7397S. doi:10.1021/es101657s. ISSN 0013-936X. PMID 20809616.
- ^ Cimitile, Matthew. "Worried about Antibiotics in Your Beef? Vegetables May Be No Better". Scientific American.
- ^ Sun, P. (2013). "Detection and quantification of ionophore antibiotics in runoff, soil and poultry litter". Journal of Chromatography A. 1312: 10–17. doi:10.1016/j.chroma.2013.08.044. PMID 24028934.
- ^ Bao, Yanyu; Zhou, Qixing; Guan, Lianzhu; Wang, Yingying (April 2009). "Depletion of chlortetracycline during composting of aged and spiked manures". Waste Management. 29 (4): 1416–1423. Bibcode:2009WaMan..29.1416B. doi:10.1016/j.wasman.2008.08.022. PMID 18954968.
- ^ Title: Antibiotic Resistance—Linking Human and Animal Health Author: H. C. Wegener Publisher: National Academies Press (US) Date: 2012 Website name: NCBI Bookshelf URL: https://www.ncbi.nlm.nih.gov/books/NBK114485/ Access date: 22 March 2025
- ^ Title: Tackling Drug-Resistant Infections Globally: Final Report and Recommendations Author: Jim O’Neill Publisher: The Review on Antimicrobial Resistance Date: May 2016 Website name: AMR Review URL: https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf Access date: 22 March 2025
- ^ World Health Organization (2019) Title: New report calls for urgent action to avert antimicrobial resistance crisis Author: World Health Organization Publisher: WHO Date: 29 April 2019 Website name: World Health Organization URL: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis Access date: 22 March 2025
- ^ World Health Organization (2019) Title: New report calls for urgent action to avert antimicrobial resistance crisis Author: World Health Organization Publisher: WHO Date: 29 April 2019 Website name: World Health Organization URL: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis Access date: 22 March 2025
- ^ World Health Organization (2019) Title: New report calls for urgent action to avert antimicrobial resistance crisis Author: World Health Organization Publisher: WHO Date: 29 April 2019 Website name: World Health Organization URL: https://www.who.int/news/item/29-04-2019-new-report-calls-for-urgent-action-to-avert-antimicrobial-resistance-crisis Access date: 22 March 2025
- ^ "One of the world's largest banks has issued an alarming warning about antibiotic resistance — with big consequences for humanity". Business Insider UK. 10 October 2018. Retrieved 13 November 2018.
- ^ "Antibiotics for livestock vital to feed world: OIE". Reuters. 11 January 2012.
- ^ a b Stop using antibiotics in healthy animals to preserve their effectiveness. (2017). Retrieved from https://www.who.int/news-room/detail/07-11-2017-stop-using-antibiotics-in-healthy-animals-to-prevent-the-spread-of-antibiotic-resistance
- ^ Karavolias, Joanna; Salois, Matthew Jude; Baker, Kristi; Watkins, Kevin (October 2018). "Raised without antibiotics: impact on animal welfare and implications for food policy". Translational Animal Science. 2 (4): 337–348. doi:10.1093/tas/txy016. PMC 7200433. PMID 32704717.
- ^ Phillips, I.; Casewell, M; Cox, T; De Groot, B; Friis, C; Jones, R; Nightingale, C; Preston, R; Waddell, J (4 December 2003). "Does the use of antibiotics in food animals pose a risk to human health? A critical review of published data". Journal of Antimicrobial Chemotherapy. 53 (1): 28–52. doi:10.1093/jac/dkg483. PMID 14657094.
- ^ Dee, S; Guzman, JE; Hanson, D; Garbes, N; Morrison, R; Amodie, D (2018). "A randomized controlled trial to evaluate performance of pigs raised in antibiotic-free or conventional production systems following challenge with porcine reproductive and respiratory syndrome virus". PLOS ONE. 13 (12): e0208430. Bibcode:2018PLoSO..1308430D. doi:10.1371/journal.pone.0208430. PMC 6283559. PMID 30521587.
- ^ Gaucher, ML; Quessy, S; Letellier, A; Boulianne, M (2015). "mpact of a drug-free 391 program on broiler chicken growth performances, gut health, Clostridium perfringens and 392 Campylobacter jejuni occurrences at the farm level". Poultry Science. 94 (8): 1791–801. doi:10.3382/ps/pev142. PMID 26047674.
- ^ Smith, JA (2011). "Experiences with drug-free broiler production". Poultry Science. 90 (11): 2670–8. doi:10.3382/ps.2010-01032. PMID 22010257.
- ^ a b c National Research Council (US) Committee on Drug Use in Food Animals (1999). "Costs of Eliminating Subtherapeutic Use of Antibiotics". The Use of Drugs in Food Animals: Benefits and Risks. National Academies Press.
- ^ a b "Antibiotic Resistance". WHO. World Health Organization. Retrieved 28 March 2019.
- ^ Dall, Chris (22 March 2018). "Price to Pay: Antibiotic-Resistant Infections Cost $2 billion a year". The Center for Infectious Disease Research and Policy.
- ^ Tang, Karen L; Caffrey, Niamh P; Nóbrega, Diego; Cork, Susan C; Ronksley, Paul C; Barkema, Herman W; Polachek, Alicia J; Ganshorn, Heather; Sharma, Nishan; Kellner, James D; Checkley, Sylvia L; Ghali, William A (August 2019). "Comparison of different approaches to antibiotic restriction in food-producing animals: stratified results from a systematic review and meta-analysis". BMJ Global Health. 2019 (4): e001710. doi:10.1136/bmjgh-2019-001710. PMC 6730577. PMID 31543995.
- ^ Veterinary Medicines Directorate (5 November 2018). "Avoiding Veterinary Residues in Food – Maintaining Consumer Confidence" (PDF). Defra (UK). Retrieved 22 March 2020.
- ^ IFAH. "Veterinary Medicines and Food Safety". Health for Animals. Archived from the original (PDF) on 7 April 2020. Retrieved 22 March 2020.
- ^ Millen, D. D.; Pacheco, R. D. L.; Meyer, P. M.; Rodrigues, P. H. M.; De Beni Arrigoni, M. (2011). "Current outlook and future perspectives of beef production in Brazil". Animal Frontiers. 1 (2): 46–52. doi:10.2527/af.2011-0017.
- ^ Antimicrobial use, resistance and economic benefits and costs to livestock producers in Brazill. OECD. 2019. pp. 8–9.
- ^ Canadian Cattlemen's Association and Beef Information Centre (2003). "Understanding Use of Antibiotic and Hormonal Substances in Beef Cattle". Nutrition Perspective. Archived from the original on 17 May 2016. Retrieved 29 October 2009.
- ^ Tatlow, Didi Kirsten (18 February 2013). "Global Health Threat Seen in Overuse of Antibiotics on Chinese Pig Farms". IHT Rendezvous. Retrieved 28 August 2013.
- ^ Wei, R.; Ge, F.; Huang, S.; Chen, M.; Wang, R. (2011). "Occurrence of veterinary antibiotics in animal wastewater and surface water around farms in Jiangsu Province, China" (PDF). Chemosphere. 82 (10): 1408–1414. Bibcode:2011Chmsp..82.1408W. doi:10.1016/j.chemosphere.2010.11.067. PMID 21159362. Archived from the original (PDF) on 17 August 2018. Retrieved 17 August 2018.
- ^ Hu, X.; Zhou, Q.; Luo, Y. (2010). "Occurrence and source analysis of typical veterinary antibiotics in manure, soil, vegetables and groundwater from organic vegetable bases, northern China". Environmental Pollution. 158 (9): 2992–2998. Bibcode:2010EPoll.158.2992H. doi:10.1016/j.envpol.2010.05.023. PMID 20580472.
- ^ Zhao, L.; Dong, Y. H.; Wang, H. (2010). "Residues of veterinary antibiotics in manures from feedlot livestock in eight provinces of China". Science of the Total Environment. 408 (5): 1069–1075. Bibcode:2010ScTEn.408.1069Z. doi:10.1016/j.scitotenv.2009.11.014. PMID 19954821.
- ^ Krishnasamy, Vikram; Otte, Joachim; Silbergeld, Ellen (28 April 2015). "Antimicrobial use in Chinese swine and broiler poultry production". Antimicrobial Resistance and Infection Control. 4 (1): 17. doi:10.1186/s13756-015-0050-y. ISSN 2047-2994. PMC 4412119. PMID 25922664. S2CID 10987316.
- ^ Mu, Quanhua; Li, Jin; Sun, Yingxue; Mao, Daqing; Wang, Qing; Yi, Luo (5 December 2014). "Occurrence of sulfonamide-, tetracycline-, plasmid-mediated quinolone- and macrolide-resistance genes in livestock feedlots in Northern China". Environmental Science and Pollution Research. 22 (6932–6940): 6932–6940. doi:10.1007/s11356-014-3905-5. PMID 25475616. S2CID 41282094.
- ^ Salamon, Maureen (11 February 2013). "China's Overuse of Antibiotics in Livestock May Threaten Human Health". health.usnews.com. Retrieved 28 August 2013.
- ^ Global and Public Health Group/10200 (24 November 2017). UK 5 Year Antimicrobial Resistance (AMR) Strategy 2013–2018: Annual progress report, 2016 (PDF) (Report).
{{cite report}}: CS1 maint: numeric names: authors list (link) - ^ Medical Research Council, M. R. C. (29 November 2018). "£4.5m from Newton Fund for collaborations that will tackle antimicrobial resistance". mrc.ukri.org. Archived from the original on 27 March 2019. Retrieved 6 December 2018.
- ^ European Union (2005). "European Commission – PRESS RELEASES – Press release – Ban on antibiotics as growth promoters in animal feed enters into effect". Retrieved 22 December 2005.
- ^ "EUR-Lex – 32003R1831 – EN – EUR-Lex". data.europa.eu.
- ^ Köper, Lydia M.; Bode, Christoph; Bender, Alice; Reimer, Inke; Heberer, Thomas; Wallmann, Jürgen (10 August 2020). Clegg, Simon (ed.). "Eight years of sales surveillance of antimicrobials for veterinary use in Germany—What are the perceptions?". PLOS ONE. 15 (8). Public Library of Science (PLoS): e0237459. Bibcode:2020PLoSO..1537459K. doi:10.1371/journal.pone.0237459. ISSN 1932-6203. PMC 7416935. PMID 32776971.
- ^ ""The Swedish experience" – a summary on the Swedish efforts towards a low and prudent use of antibiotics in animal production". SLU.SE. Retrieved 8 June 2023.
- ^ Wierup, Martin (June 2001). "The Swedish Experience of the 1986 Year Ban of Antimicrobial Growth Promoters, with Special Reference to Animal Health, Disease Prevention, Productivity, and Usage of Antimicrobials". Microbial Drug Resistance. 7 (2): 183–190. doi:10.1089/10766290152045066. ISSN 1076-6294. PMID 11442345.
- ^ Grundin, Johanna; Blanco-Penedo, Isabel; Fall, Nils; Sternberg Lewerin, Susanna (2020). "The Swedish experience" – a summary on the Swedish efforts towards a low and prudent use of antibiotics in animal production (PDF). Uppsala: SLU Framtidens djur, natur och hälsa. p. 19. ISBN 978-91-576-9745-5.
- ^ Koch, Julia (13 November 2013). "Cutting Antibiotics : Denmark Leads Way in Healthier Pig Farming". Spiegel Online. Retrieved 22 May 2014.
- ^ Cogliani, Carol; Goossens, Herman; Greko, Christina (1 January 2011). "Restricting Antimicrobial Use in Food Animals: Lessons from Europe". Microbe Magazine. 6 (6): 274–279. doi:10.1128/microbe.6.274.1. ISSN 1558-7452.
- ^ "Parliament demands smarter use of antibiotics". www.europarl.europa.eu.
- ^ "EUR-Lex – 2014_257 – EN – EUR-Lex". eur-lex.europa.eu.
- ^ "Veterinary medicines: new EU rules to enhance availability and fight against antimicrobial resistance – Consilium". www.consilium.europa.eu.
- ^ European Medicines Agency (4 September 2019). "Implementation of the new Veterinary Medicines Regulation". Retrieved 31 March 2020.
- ^ Thacker, Teena (13 April 2011). "Govt wants to limit use of antibiotics in animals – Indian Express". indianexpress.com. Retrieved 28 August 2013.
- ^ Sinha, Kounteya (25 November 2011). "New norm to curb antibiotic resistance". The Times of India. Archived from the original on 28 August 2013. Retrieved 28 August 2013.
- ^ Sinha, Kounteya (6 April 2012). "In a first, antibiotics bar on food-producing animals". The Times of India. Archived from the original on 28 August 2013. Retrieved 28 August 2013.
- ^ "Centre For Science and Environment (CSE)". 30 July 2014. Archived from the original on 15 October 2017. Retrieved 30 July 2014.
- ^ staff (7 January 1999). "NZ holds off ban on animal antibiotics – National – NZ Herald News". nzherald.co.nz. Retrieved 29 August 2013.
- ^ Williams, Robyn; Cook, Greg (11 August 2007). "Antibiotics and intensive chicken farming in New Zealand – The Science Show". abc.net.au. Retrieved 29 August 2013.
- ^ Ministry of Health and Ministry for Primary Industries. 2017. Antimicrobial Resistance: New Zealand's current situation and identified areas for action. Wellington: Ministry of Health and Ministry for Primary Industries. Retrieved from https://www.health.govt.nz/publication/antimicrobial-resistance-new-zealands-current-situation-and-identified-areas-action
- ^ Hillerton J.; Irvine C.; Bryan M.; Scott D.; Merchant S. (2016). "Use of antimicrobials for animals in New Zealand, and in comparison with other countries". New Zealand Veterinary Journal. 65 (2): 71–77. doi:10.1080/00480169.2016.1171736. PMID 27030313. S2CID 33661460.
- ^ Kim, Woo Joo; Park, Seung Chull (1998). "bacterial Resistance to Antimicrobial Agents: An Overview from Korea" (PDF). Yonsei Medical Journal. 39 (6): 488–494. doi:10.3349/ymj.1998.39.6.488. PMID 10097674. Retrieved 29 August 2013.
- ^ Won-sup, Yoon (25 June 2007). "Antibiotics in Livestock Harm Human Beings". The Korea Times. Retrieved 29 August 2013.
- ^ Flynn, Dan (7 June 2011). "South Korea Bans Antibiotics in Animal Feed". foodsafetynews.com. Retrieved 29 August 2013.
- ^ "UK One Health Report: Joint report on antibiotic use and antibiotic resistance" (PDF). 31 January 2019.
- ^ Veterinary Medicines Directorate (29 October 2019). "Erratum to UK Veterinary Antibiotic Resistance and Sales Surveillance Report UK-VARSS 2017" (PDF).
- ^ a b Veterinary Medicines Directorate (29 October 2019). "Veterinary Antimicrobial Resistance and Sales Surveillance UK-VARSS 2018".
- ^ a b Defra (29 October 2019). "Sales of veterinary antibiotics halved over the past four years". UK Government.
- ^ "Responsible Use of Medicines in Agriculture Alliance". Retrieved 22 March 2020.
- ^ "RUMA Targets Task Force". Retrieved 22 March 2020.
- ^ a b British Poultry Council (27 July 2016). "British Poultry Sector reduces antibiotic use by 44%". Retrieved 31 March 2020.
- ^ National Pig Association (2016). "NPA Pig IndustryAntibiotic Stewardship Programme" (PDF). Retrieved 31 March 2020.
- ^ Agriculture and Horticulture Development Board (AHDB) (January 2017). "e-Medicine Book (eMB-Pigs)". Retrieved 31 March 2020.
- ^ Red Tractor Assurance (2017). "Important Changes to Red Tractor Pig Membership, Spring/ Summer 2017" (PDF). Archived from the original (PDF) on 26 May 2021. Retrieved 31 March 2020.
- ^ Agriculture and Horticulture Development Board (May 2018). "UK pig industry halves antibiotic usage in two years". Retrieved 31 March 2020.
- ^ Veterinary Medicines Directorate (November 2016). "UK VARSS 2016 Highlights Report" (PDF). Retrieved 31 March 2020.
- ^ Agriculture and Horticulture Development Board (May 2019). "Pig industry antibiotic results show further reduction". Retrieved 31 March 2020.
- ^ a b Responsible Use of Medicines in Agriculture (RUMA) Alliance (October 2019). "Targets update shows further progress towards farm antibiotic goals – but with more to do". Retrieved 31 March 2020.
- ^ Scottish Government (February 2018). "Aeromonas Salmonicida". Retrieved 31 March 2020.
- ^ a b Martin Khor (18 May 2014). "Why Are Antibiotics Becoming Useless All Over the World?". The Real News. Archived from the original on 13 October 2017. Retrieved 18 May 2014.
- ^ "Executive summary from the UCS report "Hogging It: Estimates of Antimicrobial Abuse in Livestock"". Union of Concerned Scientists. January 2001.
- ^ a b c Antibiotic Resistance: Agencies Have Made Limited Progress Addressing Antibiotic Use in Animals (Report). U.S. Government Accountability Office. 7 September 2011. Retrieved 27 August 2013.
Antibiotics have saved millions of lives, but antibiotic use in food animals contributes to the emergence of resistant bacteria that may affect humans.
- ^ a b Summary Report on Antimicrobials Sold or Distributed for Use in Food-Producing Animals (PDF) (Report). FDA. 2013.[dead link]
- ^ Drug Use Review (PDF) (Report). FDA. 2012. Archived from the original (PDF) on 29 March 2015.
- ^ John Gever (23 March 2012). "FDA Told to Move on Antibiotic Use in Livestock". MedPage Today. Retrieved 24 March 2012.
- ^ Gardiner Harris (11 April 2012). "U.S. Tightens Rules on Antibiotics Use for Livestock". The New York Times. Retrieved 12 April 2012.
- ^ "FDA's Strategy on Antimicrobial Resistance — Questions and Answers". US Food and Drug Administration. 11 April 2012. Retrieved 12 April 2012.
"Judicious use" is using an antimicrobial drug appropriately and only when necessary; Based on a thorough review of the available scientific information, FDA recommends that use of medically important antimicrobial drugs in food-producing animals be limited to situations where the use of these drugs is necessary for ensuring animal health, and their use includes veterinary oversight or consultation. FDA believes that using medically important antimicrobial drugs to increase production in food-producing animals is not a judicious use.
- ^ Tavernise, Sabrina (11 December 2013). "F.D.A. to Phase Out Use of Some Antibiotics in Animals Raised for Meat". The New York Times. Retrieved 11 December 2013.
- ^ a b c Center for Veterinary Medicine, FDA (December 2013). "FDA's Strategy on Antimicrobial Resistance – Questions and Answers". Guidance for Industry. Retrieved 14 March 2017.
- ^ "Evaluating the Safety of Antimicrobial New Animal Drugs with Regard to Their Microbiological Effects on Bacteria of Human Health Concern" (PDF). Guidance for Industry (#152). 2003. Archived from the original (PDF) on 9 July 2009.
- ^ Summary Report On Antimicrobials Sold or Distributed for Use in Food-Producing Animals. (2018). US Food and Drug Administration. Retrieved from [1]
- ^ Cornell University College of Veterinary Medicine. "VFD – Veterinary Feed Directive". Retrieved 14 March 2017.
- ^ Dall C. (2018). FDA reports major drop in antibiotics for food animals. CIDRAP News. Retrieved from http://www.cidrap.umn.edu/news-perspective/2018/12/fda-reports-major-drop-antibiotics-food-animals
- ^ USDA. "Beef...from Farm to Table". Fact Sheets. Archived from the original on 24 February 2013.
- ^ Stephanie Strom (31 July 2015). "Perdue Sharply Cuts Antibiotic Use in Chickens and Jabs at Its Rivals". The New York Times. Retrieved 12 August 2015.
- ^ "Antibiotics Position Statement". Archived from the original on 28 July 2015. Retrieved 12 August 2015.
- ^ "Antibiotic Resistance and Food Animal Production: a Bibliography of Scientific Studies (1969–2012)" (PDF). The Pew Charitable Trusts. Archived from the original (PDF) on 11 August 2012.
- ^ The Pew Charitable Trusts (15 October 2012). "Pew Comments on Proposed Antibiotics Legislation". Retrieved 26 August 2013.
- ^ Couric, Katie (10 February 2010). "Animal Antibiotic Overuse Hurting Humans?". CBS News. New York City: CBS. Retrieved 29 August 2013.
- ^ *National Pork Producers Council (15 September 2011). "Nat'l Pork Producers Council Issues Statement About GAO's Report on Antibiotic Resistance". growinggeorgia.com. Retrieved 29 August 2013.
• Philpott, Tom (21 September 2011). "Meat Industry Still Denying Antibiotic Resistance". motherjones.com. Retrieved 29 August 2013. - ^ Bax, R.; Bywater, R.; Cornaglia, G.; Goossens, H.; Hunter, P.; Isham, V.; Jarlier, V.; Jones, R.; Phillips, I.; Sahm, D.; Senn, S.; Struelens, M.; Taylor, D.; White, A. (June 2001). "Surveillance of antimicrobial resistance — what, how and whither?". Clinical Microbiology and Infection. 7 (6): 316–325. doi:10.1046/j.1198-743x.2001.00239.x. PMID 11442565.
- ^ CIDRAP (August 2019). "US poultry data show big reductions in key antibiotics". Center for Infectious Disease Research and Policy, University of Minnesota. Retrieved 1 April 2020.
- ^ Singer, Randall S; Porter, Leah (August 2019). "Estimates of On-Farm Antimicrobial Usage in Broiler Chicken and Turkey Production in the United States, 2013 – 2017" (PDF). Retrieved 1 April 2020.
- ^ a b Allen H. K.; Trachsel J.; Looft T.; Casey T. A. (2014). "Finding alternatives to antibiotics". Annals of the New York Academy of Sciences. 1323 (1): 91–100. Bibcode:2014NYASA1323...91A. doi:10.1111/nyas.12468. PMID 24953233. S2CID 38772673.
- ^ Hume M. E. (2011). "Historic perspective: Prebiotics, probiotics, and other alternatives to antibiotics". Poultry Science. 90 (11): 2663–9. doi:10.3382/ps.2010-01030. PMID 22010256.
- ^ Griggs, J.P.; Jacob, J.P. (December 2005). "Alternatives to Antibiotics for Organic Poultry Production". Journal of Applied Poultry Research. 14 (4): 750–756. doi:10.1093/japr/14.4.750.
- ^ Doyle, M.E. 2001: Alternatives to Antibiotic Use for Growth Promotion in Animal Husbandry. Food Research Institute, University of Wisconsin-Madison.
- ^ Joerger R.D. (2003). "Alternatives to antibiotics: bacteriocins, antimicrobial peptides and bacteriophages". Poultry Science. 82 (4): 640–647. doi:10.1093/ps/82.4.640. PMID 12710486.
External links
[edit]- Anomaly, Jonathan (2015). "What's Wrong with Factory Farming". Public Health Ethics.
- O'Neill, Jim (2015). "Antimicrobials in Agriculture and the Environment" (PDF). The Review on Antimicrobial Resistance.
- O'Neill, Jim (2016). "Tackling Drug Resistance Globally: Final report and recommendations" (PDF)
- PBS report on antibiotics in livestock production
- Fix Food, Fix Antibiotics, a 90-second video explaining the problem of antibiotic resistance and campaigning for action
- Pew Trust campaign for restricting antibiotic use
- Antibiotic Resistance and the Use of Antibiotics in Animal Agriculture: Hearing before the Subcommittee on Health of the Committee on Energy and Commerce, House of Representatives, One Hundred Eleventh Congress, Second Session, July 14, 2010
 KSF
KSF