COVID-19 pandemic in the United States
 From Wikipedia - Reading time: 92 min
From Wikipedia - Reading time: 92 min
| COVID-19 pandemic in the United States | |
|---|---|
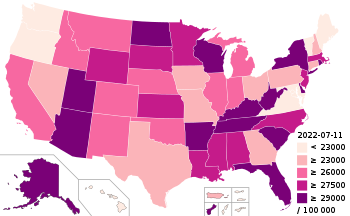 COVID-19 cases per 100,000 people by state, as of July 11, 2022 | |
| Disease | COVID-19 |
| Virus strain | SARS-CoV-2 |
| Location | United States |
| First outbreak | Wuhan, Hubei, China[1] |
| Arrival date | January 13, 2020[2] (5 years, 2 weeks and 3 days ago) Public health emergency: January 31, 2020 – May 11, 2023 (3 years, 3 months, 1 week and 4 days) |
| Confirmed cases | 103,436,829[3] |
| Suspected cases‡ | 146,585,169 (CDC estimate in September 2021)[4] |
| Recovered |
|
Deaths |
|
| Fatality rate | 1.17% |
| Vaccinations | |
| Government website | |
| CDC | |
| ‡Suspected cases have not been confirmed by laboratory tests as being due to this strain, although some other strains may have been ruled out. | |

On December 31, 2019, China announced the discovery of a cluster of pneumonia cases in Wuhan. The first American case was reported on January 20,[9] and Health and Human Services Secretary Alex Azar declared a public health emergency on January 31.[10] Restrictions were placed on flights arriving from China,[11][12] but the initial U.S. response to the pandemic was otherwise slow in terms of preparing the healthcare system, stopping other travel, and testing.[13][14][15][a][17] The first known American deaths occurred in February[18] and in late February President Donald Trump proposed allocating $2.5 billion to fight the outbreak. Instead, Congress approved $8.3 billion with only Senator Rand Paul and two House representatives (Andy Biggs and Ken Buck) voting against, and Trump signed the bill, the Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020, on March 6.[19] Trump declared a national emergency on March 13.[20] The government also purchased large quantities of medical equipment, invoking the Defense Production Act of 1950 to assist.[21] By mid-April, disaster declarations were made by all states and territories as they all had increasing cases. A second wave of infections began in June, following relaxed restrictions in several states, leading to daily cases surpassing 60,000. By mid-October, a third surge of cases began; there were over 200,000 new daily cases during parts of December 2020 and January 2021.[22][23]
COVID-19 vaccines became available in December 2020, under emergency use, beginning the national vaccination program, with the first vaccine officially approved by the Food and Drug Administration (FDA) on August 23, 2021.[24] Studies have shown them to be highly protective against severe illness, hospitalization, and death. In comparison with fully vaccinated people, the CDC found that those who were unvaccinated were from 5 to nearly 30 times more likely to become either infected or hospitalized. There has nonetheless been some vaccine hesitancy for various reasons, although side effects are rare.[25][26] There were also numerous reports that unvaccinated COVID-19 patients strained the capacity of hospitals throughout the country, forcing many to turn away patients with life-threatening diseases.
A fourth rise in infections began in March 2021 amidst the rise of the Alpha variant, a more easily transmissible variant first detected in the United Kingdom. That was followed by a rise of the Delta variant, an even more infectious mutation first detected in India, leading to increased efforts to ensure safety. The January 2022 emergence of the Omicron variant, which was first discovered in South Africa, led to record highs in hospitalizations and cases in early 2022, with as many as 1.5 million new infections reported in a single day.[27] By the end of 2022, an estimated 77.5% of Americans had had COVID-19 at least once, according to the CDC.[28]
State and local responses to the pandemic during the public health emergency included the requirement to wear a face mask in specified situations (mask mandates), prohibition and cancellation of large-scale gatherings (including festivals and sporting events), stay-at-home orders, and school closures.[29] Disproportionate numbers of cases were observed among Black and Latino populations,[30][31][32] as well as elevated levels of vaccine hesitancy,[33][34] and there was a sharp increase in reported incidents of xenophobia and racism against Asian Americans.[35][36] Clusters of infections and deaths occurred in many areas.[b] The COVID-19 pandemic also saw the emergence of misinformation and conspiracy theories,[39] and highlighted weaknesses in the U.S. public health system.[17][40][41]
In the United States, there have been 103,436,829[3] confirmed cases of COVID-19 with 1,212,505[3] confirmed deaths, the most of any country, and the 17th highest per capita worldwide.[42] The COVID-19 pandemic ranks as the deadliest disaster in the country's history.[43] It was the third-leading cause of death in the U.S. in 2020, behind heart disease and cancer.[44] From 2019 to 2020, U.S. life expectancy dropped by three years for Hispanic and Latino Americans, 2.9 years for African Americans, and 1.2 years for White Americans.[45] In 2021, U.S. deaths due to COVID-19 rose,[46] and life expectancy fell.[47]
Timeline
[edit]December 2019 to April 2020
[edit]In November 2019, COVID-19 infections had first broken out in Wuhan, China.[48][49] China publicly reported the cluster on December 31, 2019.[50] After China confirmed that the cluster of infections was caused by a novel infectious coronavirus[50] on January 7, 2020, the CDC issued an official health advisory the following day.[51] On January 20, the World Health Organization (WHO) and China both confirmed that human-to-human transmission had occurred.[52] The CDC immediately activated its Emergency operations center (EOC) to respond to the outbreak in China.[53] Also, the first report of a COVID-19 case in the U.S. was publicly reported,[50] though the All of Us study (released in 2021) showed five states already had cases weeks earlier.[54] After other cases were reported, on January 30, the WHO declared a Public health emergency of international concern (PHEIC) – its highest level of alarm[55] – warning that "all countries should be prepared for containment."[56][57][e] The same day, the CDC confirmed the first person-to-person case in the U.S.[59] The next day, the country declared a public health emergency.[60] Although by that date there were only seven known cases in the U.S., the HHS and CDC reported that there was a likelihood of further cases appearing in the country.[60]
The Trump administration evacuated American nationals from Wuhan in January.[61] On February 2, the U.S. enacted travel restrictions to and from China.[12] On February 6, the earliest confirmed American death with COVID-19 (that of a 57-year-old woman) occurred in Santa Clara County, California. The CDC did not report its confirmation until April 21,[62] by which point nine other COVID-19 deaths had occurred in Santa Clara County.[63] The virus had been circulating undetected at least since early January and possibly as early as November.[64]
On February 25, the CDC warned the American public for the first time to prepare for a local outbreak.[65][66] The next day, New York City saw the sickening of its "patient zero", Manhattan attorney Lawrence Garbuz, then thought to be the first community-acquired case.[67][68][69] Another case known as "patient zero" in Los Angeles is a man named Gregg Garfield, who spent 64 days in the Burbank Hospital, on a ventilator for 30 days, with a 1% chance to live. Contracting the virus from a ski trip, Garfield was able to return to the slopes, although with some fingers and toes amputated.[70]
In February, Vice President Mike Pence took over for HHS Secretary Alex Azar as chair of the White House Coronavirus Task Force, with Trump saying, "We are very, very ready for this, for anything, whether it's going to be a breakout of larger proportions, or whether we're at that very low level."[71] In late February Trump proposed allocating $2.5 billion to fight the outbreak, but Congress instead approved $8.3 billion with only Senator Rand Paul and Representatives Andy Biggs and Ken Buck voting against, and Trump signed the bill on March 6.[19]

By March 11, the virus had spread to 110 countries, and the WHO officially declared a pandemic.[29] The CDC had already warned that large numbers of people needing hospital care could overload the healthcare system, which would lead to otherwise preventable deaths.[72][73] Director of the National Institute of Allergy and Infectious Diseases Anthony Fauci said the mortality from COVID-19 was ten times higher than the common flu.[74] By March 12, diagnosed cases of COVID-19 in the U.S. exceeded a thousand.[75] Trump declared a national emergency on March 13.[20] On March 16, the White House advised against any gatherings of more than ten people.[76] Three days later, the United States Department of State advised U.S. citizens to avoid all international travel.[77]
By the middle of March, all fifty states were able to perform tests with a doctor's approval, either from the CDC or from commercial labs. However, the number of available test kits remained limited.[78] As cases began spreading throughout the nation, federal and state agencies began taking urgent steps to prepare for a surge of hospital patients. Among the actions was establishing additional places for patients in case hospitals became overwhelmed.[79]
Throughout March and early April, several state, city, and county governments imposed "stay at home" quarantines on their populations to stem the spread of the virus.[80] By March 26, The New York Times data showed the United States to have the highest number of known cases of any country.[81] By March 27, the country had reported over 100,000 cases.[82] On April 2, at President Trump's direction, the Centers for Medicare & Medicaid Services (CMS) and CDC ordered additional preventive guidelines to the long-term care facility industry.[83] On April 11, the U.S. death toll became the highest in the world when the number of deaths reached 20,000, surpassing that of Italy.[84] On April 19, the CMS added new regulations requiring nursing homes to inform residents, their families and representatives, of COVID-19 cases in their facilities.[85] On April 28, the total number of confirmed cases across the country surpassed 1 million.[86]
May to August 2020
[edit]By May 27, less than four months after the pandemic reached the U.S., 100,000 Americans had died with COVID-19.[87] State economic reopenings and lack of widespread mask orders resulted in a sharp rise in cases across most of the continental U.S. outside of the Northeast.[88] A study conducted in May 2020 indicated that the true number of COVID-19 cases in the United States was much higher than the number of confirmed cases with some locations having 6–24 times higher infections, which was further confirmed by a later population-wide serosurvey.[89][90][91]
On July 6, the United States Department of State announced the country's withdrawal from WHO effective July 6, 2021.[92] On July 10, the CDC adopted the Infection Fatality Ratio (IFR), "the number of individuals who die of the disease among all infected individuals (symptomatic and asymptomatic)", as a new metric for disease severity.[93] In July, US PIRG and 150 health professionals sent a letter asking the federal government to "shut it down now, and start over".[94] In July and early August, requests multiplied, with a number of experts asking for lockdowns of "six to eight weeks"[95] that they believed would restore the country by October 1, in time to reopen schools and have an in-person election.[96]
In August, over 400,000 people attended the 80th Sturgis Motorcycle Rally in Sturgis, South Dakota, and from there, at least 300 people in more than 20 states were infected.[97] The CDC followed up with a report on the associated 51 confirmed primary event-associated cases, 21 secondary cases, and five tertiary cases in the neighboring state of Minnesota, where one attendee died of COVID-19.[98] The U.S. passed five million COVID-19 cases by August 8.[99]
September to December 2020
[edit]On September 22, the U.S. passed 200,000 deaths, according to data from Johns Hopkins University.[100] In early October, an unprecedented series of high-profile U.S. political figures and staffers announced they had tested positive for COVID-19.[101][102] On October 2, Trump announced on Twitter that both he and the First Lady had tested positive for COVID-19 and would immediately quarantine.[103][102] Trump was given an experimental Regeneron product with two monoclonal antibodies[104][f] and taken to Walter Reed National Military Medical Center,[106] where he was given remdesivir and dexamethasone.[107]
USA Today studied the aftermath of presidential election campaigning, recognizing that causation was impossible to determine. Among their findings, cases increased 35 percent compared to 14 percent for the state after a Trump rally in Beltrami County, Minnesota. One case was traced to a Joe Biden rally in Duluth, Minnesota.[108]
On November 9, President-elect Biden's transition team announced his COVID-19 Advisory Board.[109] On the same day, the total number of cases had surpassed ten million[110] while the total had risen by over a million in the ten days prior, averaging 102,300 new cases per day.[111] Pfizer also announced that its COVID-19 vaccine may be up to ninety percent effective.[112][113] In November, the Trump administration reached an agreement with a number of retail outlets, including pharmacies and supermarkets, to make the COVID-19 vaccine free once available.[114]
In spite of recommendations by the government not to travel, more than 2 million people flew on airlines during the Thanksgiving period.[115] On December 8, the U.S. passed 15 million cases, with about one out of every 22 Americans having tested positive since the pandemic began.[116] On December 14, the U.S. passed 300,000 deaths, representing an average of more than 961 deaths per day since the first known death on February 6. More than 50,000 deaths were reported in the past month, with an average of 2,403 daily deaths occurring in the past week.[117]
On December 24, following concerns over a probably more easily transmissible new SARS-CoV-2 variant from the United Kingdom, later called Alpha, the CDC announced testing requirements for American passengers traveling from the UK, to be administered within 72 hours, starting on December 28.[118][119] On December 29, the U.S. reported the first case of this variant in Colorado. The patient had no travel history, leading the CDC to say, "Given the small fraction of US infections that have been sequenced, the variant could already be in the United States without having been detected."[120]
January to April 2021
[edit]
On January 1, 2021, the U.S. passed 20 million cases, representing an increase of more than a million over the past week and 10 million in less than two months.[121][122] On January 6, the CDC announced that it had found at least 52 confirmed cases of the Alpha variant, and it also stressed that there could already be more cases in the country.[123] In the following days, more cases of the variant were reported in other states, leading former CDC director Tom Frieden to express his concerns that the U.S. will soon face "close to a worst-case scenario".[124] It was believed the variant had been present in the U.S. since October.[125]
On January 19, the U.S. passed 400,000 deaths, just five weeks after the country passed 300,000 deaths.[126] On January 22, the U.S. passed 25 million cases, with one of every 13 Americans testing positive for COVID-19.[127] On January 29, a nationwide requirement for use of face masks on public transit and other forms of public transportation was issued by the CDC and the federal Transportation Security Administration, to go into effect on February 1.[128][129] (Subsequently, extended, the federal mask mandate for public transportation remains in effect in April 2022.)[129][130]
On February 22, the U.S. passed 500,000 deaths, just five weeks after the country passed 400,000 deaths.[131] By March 5, more than 2,750 cases of COVID-19 variants were detected in 47 states; Washington, D.C.; and Puerto Rico.[132] In the first prime time address of his presidency, on March 11, Biden announced his plan to push states to make vaccines available to all adults by May 1, with the aim of making small gatherings possible by July 4.[133] On March 24, the U.S. passed 30 million cases, just as a number of states began to expand the eligibility age for COVID-19 vaccines.[134] Experts began warning against public relaxation of COVID-19 mitigation measures as vaccines continue to be administered, with CDC director Rochelle Walensky, warning of a new rise in cases.[135]
By April 7, the Alpha variant had become the dominant COVID-19 strain in the U.S.[136] On April 12, the U.S. reported its first cases of a new "double mutant" SARS-CoV-2 variant from India, later called Delta, in California.[137] By April 25, the country's seven-day average of new infections was reported to be decreasing, but concerns were raised about drops in vaccine demand in certain parts of the U.S., which were attributed to vaccine hesitancy.[138][139][140] On April 29, the CDC estimated that roughly 35% of the U.S. population had been infected with the virus as of March 2021, about four times higher than the official reported numbers.[141]
May to August 2021
[edit]On May 4, Biden announced a new goal of having 70 percent of all adults in the U.S. receive at least one COVID-19 vaccine shot by July 4, along with steps to vaccinate teenagers and more inaccessible populations.[142] The country ultimately did not reach that goal, with only 67 percent of the overall adult population having done so by July 4.[143] On May 6, a study by the Institute for Health Metrics and Evaluation estimated that the true COVID-19 death toll in the U.S. was more than 900,000 people.[144] On May 9, Dr. Fauci confirmed that the U.S. death toll was likely undercounted.[145]
On May 13, the CDC changed its guidance and said that fully vaccinated individuals do not need to wear masks in most situations.[146] Some states ended their mask mandates shortly after, while others maintained the mandate. The CDC was criticized for the confusion resulting from the announcement, as it did not remove existing state and local mandates. The guidance also did not remove the federal mask mandate on public transportation.[147] On June 15, the U.S. passed 600,000 deaths, though the number of daily deaths had decreased due to vaccination efforts.[148]
By June, COVID-19 cases rose again, especially in Arkansas, Nevada, Missouri, and Wyoming. The rising numbers were believed to be attributable to the Delta variant.[149] By July 7, the Delta variant had surpassed the Alpha variant to become the dominant COVID-19 strain in the U.S., according to CDC data.[150] By August the Delta variant accounted for 99 percent of all cases and was found to double the risk of hospitalization for those not yet vaccinated.[151]
On August 1, the U.S. passed 35 million cases.[152] By early and mid-August, hospitals in some states with low vaccination rates began to exceed capacity.[153] One-quarter of the U.S. population resides in eight states—Alabama, Arkansas, Florida, Georgia, Louisiana, Mississippi, Nevada, and Texas—but, by mid-August, these states together had a half of COVID-19 hospitalizations in the nation.[154] By the end of the month, the ICUs of five of those—Alabama, Arkansas, Florida, Georgia, and Texas—were over 90% full.[155]
September to November 2021
[edit]On September 8, the U.S. passed 40 million cases.[156] By September 15, one in every 500 Americans had died from COVID-19.[157] By September 20, COVID-19 had killed over 675,000 Americans, the estimated number of American deaths from the Spanish flu in 1918. As a result, COVID-19 became the deadliest respiratory pandemic in recent American history.[158] The Associated Press called the new numbers a "colossal tragedy" because, despite a century of advances in science, the country failed to take full advantage of vaccines.[159] On October 1, the U.S. passed 700,000 deaths.[160] On October 18, the U.S. passed 45 million cases.[161] On November 26, Biden announced that the U.S. will restrict travel from South Africa and seven other African countries due to concerns over a new variant from the area, called Omicron.[162]
December 2021 to March 2022
[edit]At the beginning of January 2022, the number of cases per day exceeded 1 million.[163] As of February 1, fatality rates were 63% higher in the U.S. than other large wealthy countries, due in part to far lower vaccination rates compared to those countries.[164] On March 9, the Biden administration advised Congress of a lack of funding for testing, therapeutics and vaccines, but Republicans continued to block new spending on the pandemic so Democrats removed an emergency aid package from a proposed spending bill.[165] On March 20, Dr. Anthony S. Fauci warned of an "uptick" in cases like Europe had seen recently, stating the U.S. should "be prepared for the possibility that we might get another variant".[166]
April to June 2022
[edit]In April 2022, it was reported by CNN that COVID-19 numbers reached pandemic lows across the US, resulting in many testing sites closing their doors. With testing sites seeing as low as single digits per day, Director of Public Health Services Division of the Haywood County Health and Human Services Agency in North Carolina Sarah Henderson suggested that she expected most counties to see closures soon, if they had not already. "We were seeing an excess of 100 patients at our testing site in the first few days [of January], which doesn't sound like a lot, but our community is very small," Henderson said. "The last couple of weeks, we have seen single digits every day. I certainly won't speak for other counties, but I think we're probably heading in that direction where if they're not closing down, they're decreasing hours and staff."[167]
On April 18, 2022, the federal transportation mask mandate, which had been extended to May 3 by the Biden administration on the advice of the CDC, was ended nationwide by U.S. District Judge Kathryn Kimball Mizelle, a Trump-appointed federal judge in Florida.[168] The Justice Department challenged the ruling several days later, yet masks remained optional on airplanes, buses, and subway systems, except when required by local mandates.[169]
The first annual National COVID Week of Remembrance & Action was held from April 24–30, with mayors and other political officials declaring the week of remembrance in their respective jurisdictions as part of a national movement led by a collection of COVID advocacy groups.[170][171] According to data compiled by NBC News, the U.S. death toll reached 1 million on May 4, 2022, the largest-recorded death toll in any single country, followed by Brazil, with about 660,000 deaths.[172] The White House confirmed the 1 million mark with a presidential proclamation on May 12, ordering flags to be flown at half-staff at all federal facilities through sundown on May 16.[173]
In June, the United States concluded the approval process for the vaccination of children under five years of age, with the first vaccines expected to be administered on June 21.[174] On June 12, the U.S. dropped COVID testing requirements for inbound international air travelers, while vaccination requirements largely remained in place for inbound travelers using any mode of cross-border transportation.[175]
July to September 2022
[edit]The number of cases for the months of January through June 2022 was about 2.4 times the number for the same period in 2021, and the number of COVID-attributed deaths likewise averaged 0.74 times the number in 2021.[163] Nonetheless, as of July 14, only 21 states have active COVID-19 emergency orders in place,[176] and there are no state-level mask requirements still in force.[177]
The number of cases for July and August 2022 was 3,672,358 and 3,154,320, respectively, with 11,963 and 15,943 COVID-attributed deaths, respectively. The totals for these two months reflect about 1.6 times the number of cases and 0.81 times the number of deaths from the same months in 2021.[163]
On September 18, 2022, in an appearance on 60 Minutes, president Joe Biden declared his belief that the COVID-19 pandemic was "over" in the United States.[178][179] This assessment met some debate in the medical community: at the time, the United States had roughly 400 deaths from the disease per day, and when extrapolated to 150,000 per year is three times the fatality rate of a bad flu season.[180]
The number of cases for the months of July through September 2022 was about 0.86 times the number for the same period in 2021, and the number of COVID-attributed deaths likewise averaged 0.42 times the number for the same period in 2021.[163]
October to December 2022
[edit]In October, new variants BQ.1 and BQ.1.1 from the dominant BA.5 appeared to be spreading quickly, but comprised only a small proportion of overall variants. Although variant XBB was of concern internationally, it was rare in the United States.[181] Recommendations for receiving vaccination booster shots are mixed: while populations at risk of severe disease and death should stay up-to-date, healthy, middle-aged-and-younger populations are rarely at risk of severe illness, and most have adequate immunity. Although the newest bivalent boosters target the recent BA.4 and BA.5 variants and their risks are low, some experts recommend new strategies to develop vaccines with broader effectiveness.[182]
In a survey of vaccination booster intake (after completing a primary series), about 15% reported receiving the updated booster. The rates varied racially with 19% among White, non-Hispanic people, about 11% among Hispanic people, and about 7% among non-Hispanic American Indians, Alaska Native people, Black people, and those of multiple races, leading to concerns of vaccination access inequity.[183]
In the months leading up to November, deaths from COVID-19 substantially decreased, attributed to high levels of population immunity (through vaccination or prior infection), and improvements in early treatment for patients at risk for severe disease. The CDC recommended vaccinations, treatments for immunocompromised individuals and to reduce severity of the disease, and continuing to wear masks in public.[184] Nonetheless, Dr. Anthony Fauci stated that the Biden administration felt that there was "enough community protection that we're not going to see a repeat of what we saw last year at this time," referring to the emergence of the Omicron variant.[185]
A study of vaccine effectiveness found that U.S.-authorized bivalent mRNA boosters administered to those having already received 2 to 4 monovalent vaccinations provided significant additional protection against symptomatic SARS-CoV-2.[186] Concerns of a surge in Beijing caused the Biden administration to require U.S. visitors from China, Hong Kong, and Macau to provide proof of COVID-19 negative test results.[187] At the end of the year, the CDC reported that the COVID Omicron XBB.1.5 variant became much more prevalent and represented about 41% of new cases in the U.S. Scientists at Columbia University warned that the rise of subvariants could "result in a surge of breakthrough infections as well as re-infections."[188]
January to March 2023
[edit]On January 11, 2023, the Biden administration decided to renew the COVID-19 public health emergency amid a winter surge of cases related to highly transmissible Omicron subvariants. With relief measures such as automatic Medicaid re-enrollment being decoupled from the emergency declaration, some commentators believed this signaled the final extension of the emergency declaration.[189]
Although some states had already ended emergency SNAP benefits enacted during the pandemic, the USDA announced that emergency allotments for the remaining 32 states, the District of Columbia, Guam, and the U.S. Virgin Islands would end after the February 2023 distribution. Leaders of some anti-hunger organizations believed that the end of the $95-per-month additional benefit would strain local food pantries and food banks.[190] South Carolina, which ended emergency food grants after the January 2023 distribution, and the 17 other states which terminated pandemic food supplements prior to the federal end date were all states with Republican-controlled state legislatures.[191]
On January 31, 2023, President Biden announced the end to the COVID-19 emergency declarations by May 11, 2023.[192] By February 23, eighteen states had already cut payments for more than 10 million people, and Congress had decided to end the program early, exchanging additional benefits for a new permanent program that provides extra money to low-income families to replace school meals during the summer.[193]
April to June 2023
[edit]On April 10, 2023, President Biden signed into law a resolution terminating the national emergency, effective immediately.[194][195] This national emergency was separate from the public health emergency, which remained in effect until May 11, 2023.[194]
July to September 2023
[edit]A late-summer wave of COVID-19 cases, as reflected by tests at pharmacies and healthcare settings, marked the first US surge of infections since the end of the public health emergency. Wastewater testing initially indicated that the uptick in cases was only a third the size of the previous summer's surge, yet data from Walgreens showed the first week of August having the largest number of positive cases since May 2021.[196][197]
Hospitals across the United States reported a 24% rise in hospitalizations during the first two weeks of August and wastewater testing showed increased cases in the West and Northeast. With the pandemic legally declared over earlier in 2023, schools and workplaces responded to outbreaks differently, with many schools seeking to be more judicious about when to keep students home from school. The film studio Lionsgate, however, briefly reinstated a mask mandate following an outbreak, as did Morris Brown College, which also reinstated temperature checks and a restriction on large events for two weeks, at the beginning of the fall 2023 semester.[198] As more schools launched their fall semesters in late August and early September, high positivity rates among students and staff led to temporary in-person learning suspensions across three school districts in Texas and Tennessee, driven by district-level decisions rather than state authorities.[199]
With hospitalizations in excess of 20,000 for the first time since the end of the public health emergency, the federal government restarted the national free COVID test delivery program on September 25, 2023, enabling the delivery of four free COVID-19 tests per mailing address at a time when many insurance providers had begun to drop coverage of COVID tests.[200] The program, entering its fifth round of distributions with the fall 2023 initiative, was suspended in May 2023 to preserve supplies yet Health Secretary Xavier Becerra stated that the stockpile had been replenished and that the program would continue through the holiday season, and beyond, if cases continued to rise. Some of the newly mailed tests would show expired dates on their packaging but would remain valid for testing since the FDA had recently extended the expiration dates of a variety of tests.[201]
October to December 2023
[edit]Upon entering the first winter season of the post-pandemic period, some health facilities in California, New York, Massachusetts, and Illinois began to reinstate mask mandates for staff and visitors, due to increased rates of infection amid what had become an annual winter milieu of COVID, flu, and RSV.[202] New York City Health and Hospitals resumed its mandate shortly after Christmas, with the additional goal of minimizing staffing shortages throughout the healthcare system.[203]
January to March 2024
[edit]In January 2024, wastewater data showed that U.S. infections had reached their second-highest recorded level, surpassed only by the initial Omicron wave in January 2022.[204]
Due to a 38% rise in COVID-related hospitalizations in December, rapidly rising RSV infections, and similarly trending flu cases, the city of Saint Louis reinstated a mask mandate for city employees which would have started on January 5. Missouri's Republican governor, a staunch opponent of mask mandates, pressured the city to cancel the mandate less than 24 hours after it had been issued, with the city also revising its previous data on RSV and flu infections.[205]
Meanwhile, the New York City Fire Department instituted a more targeted municipal employee mandate on January 12, which required only firetruck and ambulance personnel to be masked, specifically while rendering pre-hospital patient care. This followed a renewed mask mandate which went into effect at all New York City Health + Hospitals on January 1.[206]
On January 9, in a bid to avoid school and workplace disruptions amid the post-pandemic winter surge, California health officials shortened the recommended period of isolation to one day for infected individuals who exhibit only mild symptoms.[207] On March 1, 2024, the CDC followed suit and shortened its recommended isolation period to one day after being fever-free without the aid of medications, which was the same recommendation provided for influenza and respiratory syncytial virus. The CDC still recommended enhanced precautions, such as wearing a mask and limiting close contact with others, for five days.[208]
Responses
[edit]On January 28, 2020, the CDC updated its China travel recommendations to level 3, its highest alert.[209] On February 8, the WHO's director-general announced that a team of international experts had been assembled to travel to China and he hoped officials from the CDC would also be part of that mission.[210][211] In January, Boeing announced a donation of 250,000 medical masks to help address China's supply shortages.[212] On February 7, the State Department said it had facilitated the transportation of nearly eighteen tons of medical supplies to China, including masks, gowns, gauze, respirators, and other vital materials.[213] On the same day, U.S. Secretary of State Pompeo announced a $100 million pledge to China and other countries to assist with their fights against the virus.[214]
Contact tracing is a tool to control transmission rates during the reopening process. Some states like Texas and Arizona opted to proceed with reopening without adequate contact tracing programs in place. Health experts have expressed concerns about training and hiring enough personnel to reduce transmission. Privacy concerns have prevented measures such as those imposed in South Korea where authorities used cellphone tracking and credit card details to locate and test thousands of nightclub patrons when new cases began emerging.[215] Funding for contact tracing is thought to be insufficient, and even better-funded states have faced challenges getting in touch with contacts. Congress allocated $631 million for state and local health surveillance programs, but the Johns Hopkins Center for Health Security estimates that $3.6 billion will be needed. The cost rises with the number of infections, and contact tracing is easier to implement when the infection count is lower. Health officials are also worried that low-income communities will fall further behind in contact tracing efforts which "may also be hobbled by long-standing distrust among minorities of public health officials".[216] As of July 1, 2020, only four states were using contact tracing apps as part of their state-level strategies to control transmission. The apps document digital encounters between smartphones, so the users will automatically be notified if someone they had contact with has tested positive. Public health officials in California claim that most of the functionality could be duplicated by using text, chat, email, and phone communications.[217]
In the United States, remdesivir is indicated for use in adults and adolescents (aged twelve years and older with body weight at least 40 kilograms (88 lb)) for the treatment of COVID-19 requiring hospitalization.[218] The FDA issued an emergency use authorization (EUA) for the combination of baricitinib with remdesivir, for the treatment of suspected or laboratory confirmed COVID-19 in hospitalized people two years of age or older requiring supplemental oxygen, invasive mechanical ventilation, or extracorporeal membrane oxygenation (ECMO).[219] In early March, President Trump directed the FDA to test certain medications to discover if they had the potential to treat COVID-19 patients.[220] Among those were chloroquine and hydroxychloroquine, which have been successfully used to treat malaria for over fifty years. A small test in France by researcher Didier Raoult had given positive results, although the study was criticized for design flaws, small sample size, and the fact that it was published before peer review.[221] On March 28, the FDA issued an Emergency Use Authorization (EUA) which allowed certain hospitalized COVID-19 patients to be treated with hydroxychloroquine or chloroquine.[222][220][223][224] On June 15, the FDA revoked the EUA for hydroxychloroquine and chloroquine as potential treatments for COVID-19, saying the available evidence showed "no benefit for decreasing the likelihood of death or speeding recovery".[225] However, Trump continued to promote the use of hydroxychloroquine for COVID-19 through July.[226]
From early 2020, more than 70 companies worldwide (with five or six operating primarily in the U.S.) began vaccine research.[227][228] In preparation for large-scale production, Congress set aside more than $3.5 billion for this purpose as part of the CARES Act.[229][228] On November 20, 2020, the Pfizer–BioNTech partnership submitted a request for emergency use authorization for its vaccine to the Food and Drug Administration (FDA),[230][231] which was granted on December 11.[232][233] On December 18, 2020, the FDA granted the Moderna vaccine emergency use authorization,[234][235] which Moderna had requested on November 30, 2020.[236][237] Starting on December 14, 2020, the first doses of COVID-19 vaccine were administered.[238]
Polling showed a significant partisan divide regarding the outbreak.[239] In February 2020, similar numbers of Democrats and Republicans believed COVID-19 was "a real threat": 70% and 72%, respectively. By mid-March 2020, 76% of Democrats viewed COVID-19 as "a real threat", while only 40% of Republicans agreed.[240] In mid-March, various polls found Democrats were more likely than Republicans to believe "the worst was yet to come" (79–40%), to believe their lives would change in a major way due to the outbreak (56–26%),[241] and to take certain precautions against the virus (83–53%).[242] The CDC was the most trusted source of information about the outbreak (85%), followed by the WHO (77%), state and local government officials (70–71%), the news media (47%), and Trump (46%).[242] A May 2020 poll concluded that 54% of people in the U.S. felt the federal government was doing a poor job in stopping the spread of COVID-19 in the country. 57% felt the federal government was not doing enough to address the limited availability of COVID-19 testing. 58% felt the federal government was not doing enough to prevent a second wave of COVID-19 cases later in 2020.[243] In September 2020, the Pew Research Center found that the global image of the United States had suffered in many foreign nations. In some nations, the United States' favorability rating had reached a record low since Pew began collecting this data nearly twenty years earlier. Across thirteen different nations, a median of fifteen percent of respondents rated the U.S. response to the pandemic positively.[244]
Impacts
[edit]Economic
[edit]
The pandemic, along with the resultant stock market crash and other impacts, led a recession in the United States following the economic cycle peak in February 2020.[245] The economy contracted 4.8 percent from January through March 2020,[246] and the unemployment rate rose to 14.7 percent in April.[247] The total healthcare costs of treating the epidemic could be anywhere from $34 billion to $251 billion according to analysis presented by The New York Times.[248] A study by economists Austan Goolsbee and Chad Syverson indicated that most economic impact due to consumer behavior changes was prior to mandated lockdowns.[249] During the second quarter of 2020, the U.S. economy suffered its largest drop on record, with GDP falling at an annualized rate of 32.9 percent. As of June 2020, the U.S. economy was over ten percent smaller than it was in December 2019.[250]

In September, Bain & Company reported on the tumultuous changes in consumer behavior before and during the pandemic. Potentially permanently, they found acceleration towards e-commerce, online primary healthcare, livestreamed gym workouts, and moviegoing via subscription television. Concurrent searches for both low-cost and premium products, and a shift to safety over sustainability, occurred alongside rescinded bans and taxes on single-use plastics, and losses of three to seven years of gains in out-of-home foodservice.[251] OpenTable estimated in May that 25 percent of American restaurants would close their doors permanently.[252]
The economic impact and mass unemployment caused by the COVID-19 pandemic raised fears of a mass eviction crisis,[253][254][255][256] with an analysis by the Aspen Institute indicating 30–40 million are at risk for eviction by the end of 2020.[257][258][needs update] According to a report by Yelp, about sixty percent of U.S. businesses that have closed since the start of the pandemic will stay shut permanently.[259]
| Variable | Feb | Mar | Apr | May | June | July | Aug | Sep | Oct | Nov |
|---|---|---|---|---|---|---|---|---|---|---|
| Jobs, level (000s)[260] | 152,463 | 151,090 | 130,303 | 133,002 | 137,802 | 139,582 | 140,914 | 141,720 | 142,373 | 142,629 |
| Jobs, monthly change (000s)[260] | 251 | −1,373 | −20,787 | 2,699 | 4,800 | 1,780 | 1,371 | 661 | 653 | 256 |
| Unemployment rate %[261] | 3.5% | 4.4% | 14.7% | 13.3% | 11.1% | 10.2% | 8.4% | 7.9% | 6.9% | 6.7% |
| Number unemployed (millions)[262] | 5.8 | 7.1 | 23.1 | 21.0 | 17.8 | 16.3 | 13.6 | 12.6 | 11.1 | 10.7 |
| Employment to population ratio %, age 25–54[263] | 80.5% | 79.6% | 69.7% | 71.4% | 73.5% | 73.8% | 75.3% | 75.0% | 76.0% | 76.0% |
| Inflation rate % (CPI-All)[264] | 2.3% | 1.5% | 0.4% | 0.2% | 0.7% | 1.0% | TBD | TBD | TBD | TBD |
| Stock market S&P 500 (avg. level)[265] | 3,277 | 2,652 | 2,762 | 2,920 | 3,105 | 3,230 | 3,392 | 3,380 | 3,270 | 3,694 |
| Debt held by public ($ trillion)[266] | 17.4 | 17.7 | 19.1 | 19.9 | 20.5 | 20.6 | 20.8 | 21.0 | 21.2 | 21.3 |
Social
[edit]The pandemic has had far-reaching consequences beyond the disease itself and efforts to contain it, including political, cultural, and social implications.
From the earliest days of the pandemic, there were reported incidents of xenophobia and racism against Asian Americans.[36] During the first year, an ad-hoc organization called Stop AAPI Hate received 3,795 reports of racism against Asian Americans and Pacific Islanders.[267]
Disproportionate numbers of cases have been observed among Black and Latino populations.[30][31][32] Of four studies published in September 2020, three found clear disparities due to race and the fourth found slightly better survival rates for Hispanics and Blacks.[268] As of September 15, 2020, Blacks had COVID-19 mortality rates more than twice as high as the rate for Whites and Asians, who have the lowest rates.[269] CNN reported in May 2020 that the Navajo Nation had the highest rate of infection in the United States.[270] In June 2021, the CDC confirmed these numbers, reporting that American Indian or Alaska Native, Non-Hispanic persons had the highest rates of both hospitalizations and deaths, while Hispanic and Latino persons suffered the highest rates of COVID compared to White persons. However, the CDC noted that only 61% of case reports included race and ethnicity data, which could result in inaccurate estimates of the relative risk among groups.[271] Additionally, a study published by the New England Journal of Medicine in July 2020 revealed that the effect of stress and weathering on minority groups decreases their stamina against COVID.[272]
From 2019 to 2020, in the United States, the life expectancy of a Hispanic American decreased three years, for an African American 2.9 years, and for a White American 1.2 years.[45] The COVID Tracking Project[273] published data revealing that people of color were contracting and dying from COVID-19 at higher rates than Whites. An NPR analysis of April–September 2020 data from the COVID Tracking Project found that Black people's share of COVID-19 deaths across the United States was 1.5 times greater (in some states 2.5 times greater) than their share of the U.S. population. Similarly, Hispanics and Latinos were disproportionately infected in 45 states and had a disproportionate share of the deaths in 19 states. Native American and Alaskan Native cases and deaths were disproportionally high in at least 21 states and, in some, as much as five times more than average. White non-Hispanics died at a lower rate than their share of the population in 36 states and D.C.[274]
Life expectancy continued to fall from 2020 to 2021.[47][275]
By April 2020, closed schools affected more than 55 million students.[276] Higher education was also impacted in a variety of different ways.[277][278]
Elections
[edit]The pandemic prompted calls from voting rights groups and some Democratic Party leaders to expand mail-in voting, while Republican leaders generally opposed the change. Some states were unable to agree on changes, resulting in lawsuits. Responding to Democratic proposals for nationwide mail-in voting as part of a COVID-19 relief law, President Trump said "you'd never have a Republican elected in this country again" despite evidence the change would not favor any particular group.[279] Trump called mail-in voting "corrupt" and said voters should be required to show up in person, even though, as reporters pointed out, he had himself voted by mail in the last Florida primary.[280] Though mail-in vote fraud is slightly higher than in-person voter fraud, both instances are rare, and mail-in voting can be made more secure by disallowing third parties to collect ballots and providing free drop-off locations or prepaid postage.[281]
High COVID-19 fatalities at the state and county level correlated with a drop in expressed support for the election of Republicans, including the reelection of Trump, according to a study published in Science Advances that compared opinions in January–February 2020 with opinions in June 2020.[282]
Hospital care crisis
[edit]This article needs to be updated. The reason given is: Information needed regarding 2022. (January 2022) |
The impact of the COVID-19 pandemic on hospitals became severe for some hospital systems of the United States in the spring of 2020, a few months after the COVID-19 pandemic began. Some had started to run out of beds, along with having shortages of nurses and doctors. By November 2020, with 13 million cases so far, hospitals throughout the country had been overwhelmed with record numbers of COVID-19 patients. Nursing students had to fill in on an emergency basis, and field hospitals were set up to handle the overflow.
At the beginning of 2021, cases had reached a peak, forcing some hospitals to periodically close their doors because they were overwhelmed with COVID-19 patients. In some places, as hospital space filled up, ambulances often waited hours to deliver patients. In addition, patients already admitted might get discharged earlier than usual to make room for others more severely ill. By early September, at least seven states had called in their National Guard to help overworked hospitals, including Oregon, Idaho, Montana, Kentucky, Tennessee, Georgia, and South Carolina.
The summer of 2021 saw another surge due to the new Delta variant of the virus. As a result, health care in U.S. hospitals was severely affected and led to crisis standards of care. Many hospitals were thereby unable to offer adequate medical care as a result of tight resources. For example, one hospital system in Oregon had to cancel or delay hundreds of surgeries as of mid-August. Hospitals also began seeing younger patients. And some experts found that the Delta variant was often more severe among younger age groups, whose vaccination rates were lower.
States like California saw over ten times more cases than they had just a few months earlier. By mid-August 2021, nearly all states experienced double-digit growth in COVID-19 hospitalizations. Some, like Washington, had a 34% increase of patients over a single week in September. At various medical centers, ICUs had reached capacity, forcing doctors to postpone routine surgeries. In addition, countless hospitals were also short of beds and nurses, making care and response times a lot slower. It meant that patients might wait in the ER for many hours. While some hospitals with no more capacity had to find alternate medical facilities in other states, often hundreds of miles away.
Emergency medical services in the United States also experienced a significant labor shortage, lengthening the time it took some patients to be transported to a hospital.Vaccination campaign
[edit]The US map below is for the percent of people of all ages who received all doses prescribed by the initial COVID-19 vaccination protocol. Two of the three COVID-19 vaccines used in the U.S. require two shots to be fully vaccinated. The other vaccine requires only one shot. Booster doses are recommended too.[283][284]

Timeline graph of doses administered
[edit]| Timeline of daily COVID-19 vaccine doses administered in the US.[285] |
 |
| See the latest date on the timeline at the bottom. |
Background to various vaccines
[edit]The COVID-19 vaccination campaign in the United States is an ongoing mass immunization campaign for the COVID-19 pandemic in the United States. The Food and Drug Administration (FDA) first granted emergency use authorization to the Pfizer–BioNTech vaccine on December 10, 2020,[286] and mass vaccinations began four days later. The Moderna vaccine was granted emergency use authorization on December 17, 2020,[287] and the Janssen (Johnson & Johnson) vaccine was granted emergency use authorization on February 27, 2021.[288] It was not until April 19, 2021, that all U.S. states had opened vaccine eligibility to residents aged 16 and over.[289] On May 10, 2021, the FDA approved the Pfizer-BioNTech vaccine for adolescents aged 12 to 15.[290] On August 23, 2021, the FDA granted full approval to the Pfizer–BioNTech vaccine for individuals aged 16 and over.[291]
The U.S. government began the campaign under the presidency of Donald Trump with Operation Warp Speed, a public–private partnership to expedite the development and manufacturing of COVID-19 vaccines. Joe Biden became the new President of the United States on January 20, 2021. Biden had an immediate goal of administering 100 million vaccine doses within his first hundred days in office, and signed an executive order which increased supplies for vaccination.[292][293][294] This goal was met on March 19, 2021.[295] On March 25, 2021, he announced he would increase the goal to 200 million within his first 100 days in office.[296] This goal was reached on April 21, 2021.[297]
By July 4, 2021, 67% of the United States' adult population had received at least one dose, just short of a goal of 70%. This goal was met on August 2, 2021. While vaccines have helped significantly reduce the number of new COVID-19 infections nationwide, states with below-average vaccination rates began to see increasing numbers of cases credited to the highly infectious Delta variant by July 2021, which led to an increased push by organizations and companies to begin imposing de facto mandates for their employees be vaccinated for COVID-19.
On September 9, 2021, President Biden announced plans by the federal government to use executive orders and emergency temporary standards enforced by OSHA to mandate the vaccination of all federal branch employees, and require that all companies with more than 100 employees regularly test all employees who are not yet fully vaccinated for COVID-19.[298] On January 26, 2022, OSHA withdrew the vaccine mandate for companies with more than 100 employees due to a ruling from the Supreme Court of the United States that blocked the mandate.[299][300]
As of November 2022, according to The Commonwealth Fund, COVID-19 vaccination in the United States has prevented an additional 3.2 million deaths, an additional 18.5 million hospitalizations, and an additional 120 million infections from COVID-19. Vaccination has also prevented an additional $899.4 billion in healthcare costs.[301] According to a June 2022 study published in The Lancet, COVID-19 vaccination in the United States prevented an additional 1.9 million deaths from December 8, 2020, to December 8, 2021.[302][303] According to a July 2022 study published in JAMA Network Open, COVID-19 vaccination in the United States prevented an additional 235,000 deaths, an additional 1.6 million hospitalizations, and an additional 27 million infections from December 1, 2020, to September 30, 2021.[304]Vaccine mandates
[edit]By August 2021, more than 800 colleges and universities, over 200 health care companies and dozens of states, local governments and school districts, had some type of vaccination requirements.[305] President Biden appealed to public organizations and private companies to require employees to be vaccinated, which companies are now legally allowed to do.[306]
Until August to September 2021, many companies were giving bonuses for getting vaccinated.[307] Nonetheless, nearly 2,000 private hospitals and health systems had previously issued vaccine mandates. Many companies outside health care did the same, such as United Airlines, Tyson Foods, and Walmart among them. Washington state had already required vaccines for all state employees and contractors.[307] With the new Delta variant spreading infections more quickly due to its higher transmissibility, companies including Facebook, Google, and Salesforce, have already issued employee vaccine mandates.[308]
According to a USA Today poll from August 2021, 68% supported a business's right to refuse service to unvaccinated customers, and 62% supported employer's right to mandate vaccinations to its employees. In the same poll, 72% also felt that mandating masks was "a matter of health and safety" and should not be considered an infringement of personal liberty.[309]
Effectiveness of COVID-19 vaccines
[edit]

Evidence from vaccine use during the pandemic shows vaccination can reduce infection and is most effective at preventing severe COVID-19 symptoms and death, but is less good at preventing mild COVID-19. Efficacy wanes over time but can be maintained with boosters.[312] In 2021, the CDC reported that unvaccinated people were 10 times more likely to be hospitalized and 11 times more likely to die than fully vaccinated people.[313][314]
The CDC reported that vaccine effectiveness fell from 91% against Alpha to 66% against Delta.[315] One expert stated that "those who are infected following vaccination are still not getting sick and not dying like was happening before vaccination."[316] By late August 2021, the Delta variant accounted for 99 percent of U.S. cases and was found to double the risk of severe illness and hospitalization for those not yet vaccinated.[317]
In November 2021, a study by the ECDC estimated that 470,000 lives over the age of 60 had been saved since the start of the vaccination roll-out in the European region.[318] According to a June 2022 study, COVID‑19 vaccines prevented an additional 14.4 to 19.8 million deaths in 185 countries and territories from 8 December 2020 to 8 December 2021.[319]
On 10 December 2021, the UK Health Security Agency reported that early data indicated a 20- to 40-fold reduction in neutralizing activity for Omicron by sera from Pfizer 2-dose vaccinees relative to earlier strains. After a booster dose (usually with an mRNA vaccine),[320] vaccine effectiveness against symptomatic disease was at 70%–75%, and the effectiveness against severe disease was expected to be higher.[321]
According to early December 2021 CDC data, "unvaccinated adults were about 97 times more likely to die from COVID-19 than fully vaccinated people who had received boosters".[322]
A meta-analysis looking into COVID-19 vaccine differences in immunosuppressed individuals found that people with a weakened immune system are less able to produce neutralizing antibodies. For example, organ transplant recipients need three vaccines to achieve seroconversion.[323] A study on the serologic response to mRNA vaccines among patients with lymphoma, leukemia, and myeloma found that one-quarter of patients did not produce measurable antibodies, varying by cancer type.[324]
In February 2023, a systematic review in The Lancet said that the protection afforded by infection was comparable to that from vaccination, albeit with an increased risk of severe illness and death from the disease of an initial infection.[325]
A January 2024 study by the CDC found that staying up to date on the vaccines could reduce the risk of strokes, blood clots and heart attacks related to COVID-19 in people aged 65 years or older or with a condition that makes them more vulnerable to said conditions.[326][327]Transition to later phases
[edit]On February 17, 2022, Governor Gavin Newsom announced a formal shift toward endemic management of COVID-19 in California, saying "we are moving past the crisis phase into a phase where we will work to live with this virus".[328]
During his State of the Union Address on March 1, 2022, Biden stated that "because of the progress we've made, because of your resilience and the tools we have, tonight I can say we are moving forward safely, back to more normal routines." However, he also stated that the federal government would "never just accept living with COVID-19", explaining that it would "continue to combat the virus as we do other diseases." The White House released a new action plan the next day, which included plans to make COVID-19 antiviral medication available for free to high-risk patients at testing locations such as pharmacies and clinics, funding in support of vigilance and preparedness in the event of new surges and variants, preventing the closure of schools and businesses, and ensuring global vaccine distribution.[329][330]
On April 26, 2022, Fauci said that the United States is "out of the pandemic phase"[331] and the following day, stated that "we're really in a transitional phase...into hopefully a more controlled phase and endemicity", but further clarified that "the world is still in a pandemic...we are still experiencing a pandemic" and the United States could still see new waves of infection. Fauci's comments follow a report from the CDC indicating that the United States has a much higher level of collective immunity at this time, due to the Omicron variant.[332]
On May 16, 2022, Joseph Wendelken, a spokesman for the Rhode Island Department of Health stated that COVID-19 is now "an endemic disease" and said "we should expect moderate increases and decreases in our COVID-19 levels over the coming months".[333] In an interview with 60 Minutes aired on September 18, 2022, Joe Biden declared that the pandemic stage of COVID-19 was over in the United States.[334]
Preparations made after previous outbreaks
[edit]The United States has experienced pandemics and epidemics throughout its history, including the 1918 Spanish flu, the 1957 Asian flu, and the 1968 Hong Kong flu pandemics.[335][336][337] In the most recent pandemic prior to COVID-19, the 2009 swine flu pandemic took the lives of more than 12,000 Americans and hospitalized another 270,000 over the course of approximately a year.[335]
According to the Global Health Security Index, an American-British assessment which ranks the health security capabilities in 195 countries, the U.S. was the "most prepared" nation in 2020.[338][339] In September 2019, the Trump administration terminated United States Agency for International Development's PREDICT program, a $200 million epidemiological research program initiated in 2009 to provide early warning of pandemics abroad.[340][341] The program trained scientists in sixty foreign laboratories to detect and respond to viruses that have the potential to cause pandemics. One such laboratory was the Wuhan lab that first identified the virus that causes COVID-19. After revival in April 2020, the program was given two 6-month extensions to help fight COVID-19 in the U.S. and other countries.[342][343]
Statistics
[edit]The CDC publishes official numbers of COVID-19 cases in the United States. The CDC estimates that, between February 2020 and September 2021, only 1 in 1.3 COVID-19 deaths were attributed to COVID-19.[344] The true COVID-19 death toll in the United States would therefore be higher than official reports, as modeled by a paper published in The Lancet Regional Health – Americas.[345] One way to estimate COVID-19 deaths that includes unconfirmed cases is to use the excess mortality, which is the overall number of deaths that exceed what would normally be expected.[346] From March 1, 2020, through the end of 2020, there were 522,368 excess deaths in the United States, or 22.9% more deaths than would have been expected in that time period.[347]
In February 2020, at the beginning of the pandemic, a shortage of tests made it impossible to confirm all possible COVID-19 cases[348] and resulting deaths, so the early numbers were likely undercounts.[349][350][351][352]See also
[edit]- COVID-19 pandemic by country and territory
- COVID-19 pandemic in North America
- Misinformation related to the COVID-19 pandemic
- United States House Select Subcommittee on the Coronavirus Crisis
Notes
[edit]- ^ A lack of mass testing obscured the extent of the outbreak.[16]
- ^ Examples of areas in which clusters occurred include urban areas, nursing homes, long-term care facilities, group homes for the intellectually disabled,[37] detention centers (including prisons), meatpacking plants, churches, and navy ships.[38]
- ^ This chart only includes deaths. Data for the current day may be incomplete.
- ^ This chart only includes lab-confirmed cases and deaths. Not all states report recoveries. Data for the current day may be incomplete.
- ^ The editorial board for The Wall Street Journal suggested the world may have been "better prepared" had the PHEIC been declared a week sooner, when the virus had spread to other countries.[58]
- ^ In a news release, Sean Conley, physician to President Trump, incorrectly identified Regeneron's monoclonal antibody product as polyclonal.[105]
References
[edit]- ^ Sheikh K, Rabin RC (March 10, 2020). "The Coronavirus: What Scientists Have Learned So Far". The New York Times. Retrieved March 24, 2020.
- ^ "Second Travel-related Case of 2019 Novel Coronavirus Detected in United States". U.S. Centers for Disease Control and Prevention (CDC).
Second Travel-related Case of 2019 Novel Coronavirus Detected in United States: The patient returned to the U.S. from Wuhan on January 13, 2020
- ^ a b c d e f Mathieu E, Ritchie H, Rodés-Guirao L, Appel C, Giattino C, Hasell J, et al. (2020–2024). "Coronavirus Pandemic (COVID-19)". Our World in Data. Retrieved January 28, 2025.
- ^ "Estimated COVID-19 Burden". U.S. Centers for Disease Control and Prevention (CDC). July 27, 2021.
- ^ "U.S. recovered COVID-19 cases". Worldometer. Frequently updated.
- ^ "COVID Data Tracker". CDC. U.S. Centers for Disease Control and Prevention (CDC). August 10, 2024. Retrieved August 18, 2024.
- ^ "The pandemic's true death toll". The Economist. January 25, 2022. Archived from the original on February 8, 2024. Retrieved January 25, 2022.
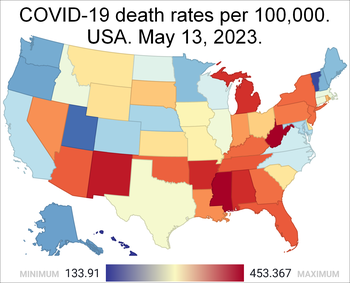
- ^ COVID-19 Deaths per 100K. U.S. News & World Report. Run your cursor over the map to see the dates and data for each state. "The data on this page is courtesy of USAFacts – a nonprofit, nonpartisan civic initiative – and includes information from the Centers for Disease Control and Prevention and state and local health departments. See a detailed methodology at the USAFacts website."
- ^ Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. (March 5, 2020). "First Case of 2019 Novel Coronavirus in the United States". New England Journal of Medicine. 382 (10): 929–936. doi:10.1056/NEJMoa2001191. ISSN 0028-4793. PMC 7092802. PMID 32004427.
- ^ "Proclamation on Declaring a National Emergency Concerning the Novel Coronavirus Disease (COVID-19) Outbreak". The White House. March 13, 2020.
- ^ Aubrey A (January 31, 2020). "Trump Declares Coronavirus A Public Health Emergency And Restricts Travel From China". NPR. Retrieved March 18, 2020.
'Foreign nationals other than immediate family of U.S. citizens and permanent residents who have traveled in China in the last 14 days will be denied entry into United States,' Azar said.
- ^ a b Robertson L (April 15, 2020). "Trump's Snowballing China Travel Claim". FactCheck.org. Retrieved April 29, 2020.
... effective February 2.
- ^ Lemire J, Miller Z, Colvin J, Alonso-Zaldivar R (April 12, 2020). "Signs missed and steps slowed in Trump's pandemic response". Associated Press. Retrieved April 28, 2020.
- ^ Pilkington E, McCarthy T (March 28, 2020). "The missing six weeks: how Trump failed the biggest test of his life". The Guardian. ISSN 0261-3077. Retrieved March 28, 2020.
- ^ Ollstein AM (April 14, 2020). "Trump halts funding to World Health Organization". Politico. ISSN 2381-1595. Wikidata Q104180080. Retrieved April 28, 2020.
- ^ Whoriskey P, Satija N (March 16, 2020). "How U.S. coronavirus testing stalled: Flawed tests, red tape and resistance to using the millions of tests produced by the WHO". The Washington Post. Retrieved March 18, 2020.
- ^ a b Banco E. "Inside America's Covid-reporting breakdown". Politico. Retrieved May 9, 2022.
- ^ https://www.npr.org/sections/coronavirus-live-updates/2020/04/22/840836618/1st-known-u-s-covid-19-death-was-on-feb-6-a-post-mortem-test-reveals [bare URL]
- ^ a b "Trump signs $8.3B bill to combat coronavirus outbreak in US". AP News. March 6, 2020.
- ^ a b "COVID-19 Emergency Declaration | FEMA.gov". www.fema.gov. March 14, 2020.
- ^ Watson K (March 27, 2020). "Trump invokes Defense Production Act to require GM to produce ventilators". CBS News. Retrieved April 24, 2020.
- ^ "COVID-19 Cases Are Skyrocketing, But Deaths Are Flat – So Far. These 5 Charts Explain Why". Time. Retrieved February 25, 2021.
- ^ "COVID Data Tracker". U.S. Centers for Disease Control and Prevention (CDC). March 28, 2020. Retrieved September 21, 2021.
- ^ FDA Approves First COVID-19 Vaccine. U.S. Food and Drug Administration (FDA). August 23, 2021. Retrieved October 16, 2021.
- ^ "Fauci: Polio would still exist in US if 'false information' being spread now existed decades ago", ABC News, July 20, 2021
- ^ Stieg C (July 6, 2021). "Dr. Fauci: Where to expect new Covid surges in the U.S.—and what it means for mask-wearing, other restrictions". CNBC. Retrieved July 11, 2021.
- ^ Rattner N (January 11, 2022). "U.S. sets fresh records for Covid hospitalizations and cases with 1.5 million new infections". CNBC. Retrieved January 12, 2022.
- ^ Vlachou M (July 4, 2023). "CDC Estimates How Many Americans Hadn't Had COVID By End Of 2022". HuffPost. Retrieved July 4, 2023.
- ^ a b Deb S, Cacciola S, Stein M (March 11, 2020). "Sports Leagues Bar Fans and Cancel Games Amid Coronavirus Outbreak". The New York Times. ISSN 0362-4331. Archived from the original on March 11, 2020. Retrieved March 12, 2020.
- ^ a b Godoy M (May 30, 2020). "What Do Coronavirus Racial Disparities Look Like State By State?". NPR.
- ^ a b Karson K, Scanlan Q (May 22, 2020). "Black Americans and Latinos nearly 3 times as likely to know someone who died of COVID-19: Poll". ABC News.
- ^ a b "States tracking COVID-19 race and ethnicity data". American Medical Association. July 28, 2020. Retrieved July 31, 2020.
- ^ Beleche T, et al. (May 2021). "COVID-19 Vaccine Hesitancy: Demographic Factors, Geographic Patterns, and Changes Over Time" (PDF). Assistant Secretary for Planning and Evaluation, US HHS. Retrieved August 9, 2021.
- ^ Livingston C (April 8, 2021). "Black Americans' Vaccine Hesitancy is Grounded in More Than Mistrust". Duke University. Retrieved August 9, 2021.
- ^ "New report finds 169 percent surge in anti-Asian hate crimes during the first quarter". NBC News. April 28, 2021. Retrieved December 27, 2021.
- ^ a b Tavernise S, Oppel RA Jr (March 23, 2020). "Spit On, Yelled At, Attacked: Chinese-Americans Fear for Their Safety". The New York Times. Archived from the original on March 23, 2020. Retrieved March 23, 2020.
- ^ "COVID-19 Infections And Deaths Are Higher Among Those With Intellectual Disabilities". NPR.
- ^ "U.S. Navy Policies Battling COVID-19 Rely Heavily On Isolation". NPR.
- ^ Douglas KM (February 2021). "COVID-19 conspiracy theories". Group Processes & Intergroup Relations. 24 (2): 270–275. doi:10.1177/1368430220982068. ISSN 1368-4302. S2CID 232132806.
- ^ Butcher L (November 17, 2020). "Pandemic puts all eyes on public health". Knowable Magazine. doi:10.1146/knowable-111720-1. Retrieved March 2, 2022.
- ^ Nuwer R (June 13, 2022). "Universal Health Care Could Have Saved More Than 330,000 U.S. Lives during COVID". Scientific American. Retrieved June 22, 2022.
- ^ "Mortality Analyses". Johns Hopkins University. Retrieved December 17, 2020.
- ^ "COVID-19 surpasses 1918 flu as deadliest pandemic in U.S. history". National Geographic. September 21, 2021.
- ^ Stobbe M (December 21, 2020). "US deaths in 2020 top 3 million, by far most ever counted". Associated Press.
- ^ a b Bosman J, Kasakove S, Victor D (July 21, 2021). "U.S. Life Expectancy Plunged in 2020, Especially for Black and Hispanic Americans". The New York Times. Archived from the original on December 28, 2021. Retrieved July 21, 2021.
- ^ Shapiro E, Pereira I, Deliso M (October 6, 2021). "COVID-19 live updates: More Americans died of COVID this year than all of 2020". ABC News. Retrieved October 6, 2021.
- ^ a b Bernstein L (December 22, 2022). "U.S. life expectancy continued to fall in 2021 as covid, drug deaths surged". The Washington Post. Retrieved December 22, 2022.
- ^ Margolin J, Meek JG (April 8, 2020). "Intelligence report warned of coronavirus crisis as early as November: Sources". ABC News. Retrieved December 6, 2020.
- ^ Diaz J (December 1, 2020). "Coronavirus Was In U.S. Weeks Earlier Than Previously Known, Study Says". NPR. Retrieved December 1, 2020.
- ^ a b c Holshue ML, DeBolt C, Lindquist S, Lofy KH, Wiesman J, Bruce H, et al. (March 2020). "First Case of 2019 Novel Coronavirus in the United States". New England Journal of Medicine. 382 (10): 929–936. doi:10.1056/NEJMoa2001191. PMC 7092802. PMID 32004427.
- ^ "Outbreak of Pneumonia of Unknown Etiology (PUE) in Wuhan, China". CDC. January 8, 2020.
- ^ Kuo L (January 21, 2020). "China confirms human-to-human transmission of coronavirus". The Guardian. Retrieved April 19, 2020.
- ^ "CDC Emergency Operations Center Activations". CDC. January 20, 2020.
- ^ Althoff KN, Schlueter DJ, Anton-Culver H, Cherry J, Denny JC, Thomsen I, et al. (June 2021). "Antibodies to SARS-CoV-2 in All of Us Research Program Participants, January 2-March 18, 2020". Clinical Infectious Diseases. 74 (4): 584–590. doi:10.1093/cid/ciab519. PMC 8384413. PMID 34128970.
- ^ "Timeline: WHO's COVID-19 response". World Health Organization. Retrieved September 11, 2020.
- ^ Boseley S (January 30, 2020). "WHO declares coronavirus a global health emergency". The Guardian. Retrieved March 30, 2020.
- ^ Kennedy M (January 30, 2020). "WHO Declares Coronavirus Outbreak A Global Health Emergency". NPR. Retrieved April 19, 2020.
- ^ "World Health Coronavirus Disinformation". The Wall Street Journal. April 5, 2020. Archived from the original on April 9, 2020. Retrieved April 29, 2020.
- ^ Wayland M (January 30, 2020). "Trump says coronavirus outbreak is 'all under control' and a 'very small problem' in US". CNBC (NBCUniversal). Retrieved September 11, 2020.
- ^ a b "US declares public health emergency from coronavirus". The Boston Globe. February 1, 2020.
- ^ Diamond D (January 28, 2021). "U.S. handling of American evacuees from Wuhan increased coronavirus risks, watchdog finds". The Washington Post. Archived from the original on February 7, 2021. Retrieved February 9, 2021.
- ^ Moon S (April 24, 2020). "A seemingly healthy woman's sudden death is now the first known US coronavirus-related fatality". CNN. Retrieved May 25, 2020.
- ^ Debolt D (April 25, 2020). "29 people had flu-like symptoms when they died in Santa Clara County. Nine tested positive for coronavirus". The Mercury News. Retrieved December 30, 2020.
- ^ Melinek J (May 1, 2020). "When Did COVID-19 Arrive and Could We Have Spotted It Earlier?". MedPage Today. Retrieved May 7, 2020.
- ^ Taylor M (March 23, 2020). "Exclusive: U.S. axed CDC expert job in China months before virus outbreak". Reuters. Retrieved March 24, 2020.
- ^ Schuchat A (May 2020). "Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24 – April 21, 2020" (PDF). MMWR. Morbidity and Mortality Weekly Report. 69 (18): 551–556. doi:10.15585/mmwr.mm6918e2. PMC 7737947. PMID 32379733.
- ^ "Lawrence Garbuz, New York's First Known COVID-19 Case, Reveals What He Learned About Attorney Well-Being From the Virus". New York State Bar Association. August 11, 2020.
- ^ Brody L (March 6, 2021). "Covid-19's 'Patient Zero' in New York: What Life Is Like for the New Rochelle Lawyer". The Wall Street Journal.
- ^ "New York area's 'patient zero' says coronavirus 'wasn't on my mind' when he got sick". NBC News. May 11, 2020.
- ^ "'I'm back in action,' One of the first Americans who contracted COVID-19 speaks about his recovery". March 13, 2021.
- ^ Santucci J (February 27, 2020). "What we know about the White House coronavirus task force now that Mike Pence is in charge". USA Today. Retrieved November 26, 2020.
- ^ "Coronavirus Disease 2019 (COVID-19) Situation Summary". U.S. Centers for Disease Control and Prevention (CDC). March 7, 2020. Retrieved March 7, 2020.
- ^ "Coronavirus Has Become a Pandemic, W.H.O. Says". The New York Times. March 11, 2020. Archived from the original on March 11, 2020.
- ^ "Dr. Anthony Fauci addresses COVID-19 mortality rate". C-SPAN. March 11, 2020. Retrieved September 30, 2020.
- ^ Taylor A, Armus T (March 11, 2020). "Live updates: As U.S. coronavirus cases top 1,000, mixed signs of recovery in China, South Korea". The Washington Post. Retrieved March 11, 2020.
- ^ Liptak K (March 16, 2020). "White House advises public to avoid groups of more than 10, asks people to stay away from bars and restaurants". CNN. Retrieved March 18, 2020.
- ^ "Global Level 4 Health Advisory – Do Not Travel". travel.state.gov. Archived from the original on August 3, 2020. Retrieved March 20, 2020.
- ^ "The 4 Key Reasons the U.S. Is So Behind on Coronavirus Testing". The Atlantic. March 15, 2020.
- ^ "They were supposed to build stages for Coachella. Now they're building coronavirus triage tents". Los Angeles Times. March 30, 2020.
- ^ Norwood C (April 3, 2020). "Most states have issued stay-at-home orders, but enforcement varies widely". PBS NewsHour. Retrieved April 9, 2020.
- ^ McNeil DG Jr (March 26, 2020). "The U.S. Now Leads the World in Confirmed Coronavirus Cases". The New York Times. Retrieved March 26, 2022.
- ^ Chan C, Shumaker L, Maler S (March 28, 2020). "Confirmed coronavirus cases in U.S. reach 100,000: Reuters tally". Reuters. Retrieved March 28, 2020.
- ^ "Trump wants masks on all nursing home workers, temperature checks for all, and separate COVID-19 units". McKnight's Long-term Care News. April 3, 2020.
- ^ "U.S. coronavirus deaths top 20,000, highest in world exceeding Italy: Reuters tally". Reuters. April 11, 2020. Retrieved May 1, 2020.
- ^ "Trump Administration Announces New Nursing Homes COVID-19 Transparency Effort". Centers for Medicare & Medicaid Services. April 19, 2020.
- ^ Steve Almasy, Christina Maxouris, Nicole Chavez. "US coronavirus cases surpass 1 million and the death toll is greater than US losses in Vietnam War". CNN. Retrieved April 29, 2020.
- ^ Fisher M (May 27, 2020). "U.S. coronavirus death toll surpasses 100,000, exposing nation's vulnerabilities". The Washington Post. Retrieved July 23, 2020.
- ^ Farzan AN, et al. (June 11, 2020). "U.S. surpasses 2 million coronavirus cases". The Washington Post. Retrieved July 23, 2020.
- ^ Joseph A (July 21, 2020). "Actual Covid-19 case count could be 6 to 24 times higher than official estimates, CDC study shows". statnews. Stat. Retrieved January 26, 2021.
- ^ Havers FP, Reed C, Lim T, Montgomery JM, Klena JD, Hall AJ, et al. (July 2020). "Seroprevalence of Antibodies to SARS-CoV-2 in 10 Sites in the United States, March 23-May 12, 2020". JAMA Internal Medicine. 180 (12): 1576. doi:10.1001/jamainternmed.2020.4130. ISSN 2168-6106. PMID 32692365.
- ^ DeVille T. "Almost 17 million U.S. coronavirus cases were not detected during first half of 2020, study led by UMBC graduate finds". The Baltimore Sun. Retrieved March 19, 2021.
- ^ "Briefing on the U.S. Government's Next Steps With Regard to Withdrawal From the World Health Organization". US Department of State. September 2, 2020. Retrieved November 26, 2020.
- ^ "COVID-19 Pandemic Planning Scenarios" (PDF). CDC. July 10, 2020. Retrieved September 29, 2020.
- ^ Durkee A (July 24, 2020). "Medical Experts Tell Government: 'Shut It Down Now, And Start Over'". Forbes Media. Retrieved July 25, 2020.
- ^ Board E (August 8, 2020). "America Could Control the Pandemic by October. Let's Get to It". The New York Times. Archived from the original on August 8, 2020. Retrieved August 8, 2020.
- ^ Rivers C, Martin E, Watson C, Schoch-Spana M, Cicero A, Inglesby T (2020). "Resetting Our Response: Changes Needed in the US Approach to COVID-19". Baltimore, MD: Johns Hopkins Center for Health Security. and Benito M (July 23, 2020). "Back to normal by October? Dr. Hotez sends the White House a national, unified coronavirus plan". KHOU-TV. and Osterholm MT, Kashkari N (August 7, 2020). "Here's How to Crush the Virus Until Vaccines Arrive". The New York Times. Archived from the original on August 7, 2020. and Slavitt A (August 4, 2020). "Joe Biden is the national reset we need on COVID-19, but he's more than 75,000 lives away". USA Today. and Branswell H (August 10, 2020). "Winter is coming: Why America's window of opportunity to beat back Covid-19 is closing". STAT. Retrieved August 11, 2020.
- ^ Walker M, Healy J (November 6, 2020). "A Motorcycle Rally in a Pandemic? 'We Kind of Knew What Was Going to Happen'". The New York Times. Archived from the original on November 6, 2020. Retrieved November 7, 2020.
- ^ Firestone MJ, Wienkes H, Garfin J, Wang X, Vilen K, Smith KE, et al. (November 2020). "COVID-19 Outbreak Associated with a 10-Day Motorcycle Rally in a Neighboring State – Minnesota, August–September 2020" (PDF). MMWR Morb Mortal Wkly Rep. 69 (47): 1771–1776. doi:10.15585/mmwr.mm6947e1. PMC 8022865. PMID 33237891. S2CID 227176504.
- ^ Craft D (August 8, 2020). "U.S. sets record as coronavirus cases top 5 million". Reuters. Retrieved September 25, 2020.
- ^ Chappel B (September 22, 2020). "'Enormous And Tragic': U.S. Has Lost More Than 200,000 People To COVID-19". NPR. Retrieved September 22, 2020.
- ^ Haberman M, Shear MD (October 1, 2020). "Trump Says He'll Begin 'Quarantine Process' After Hope Hicks Tests Positive for Coronavirus". The New York Times. ISSN 0362-4331. Archived from the original on October 2, 2020. Retrieved October 3, 2020.
- ^ a b Moreno JE (October 2, 2020). "White House wanted to keep Hope Hicks's positive COVID-19 test private: report". The Hill. Retrieved October 3, 2020.
- ^ Dawsey J, Itkowitz C. "Trump says he and first lady have tested positive for coronavirus". The Washington Post. ISSN 0190-8286. Retrieved October 2, 2020.
- ^ Manke K (October 6, 2020). "Trump's COVID-19 treatments suggest severe illness, UC Berkeley expert says". UC Berkeley News. Retrieved October 7, 2020.
- ^ "Memorandum From Trump's Doctor on COVID-19 Treatment". U.S. News & World Report. Associated Press. October 2, 2020. Retrieved October 8, 2020. and Cohen J (October 5, 2020). "Update: Here's what is known about Trump's COVID-19 treatment". Science. doi:10.1126/science.abf0974. S2CID 225114036.
- ^ Liptak K (October 3, 2020). "Trump taken to Walter Reed medical center and will be hospitalized 'for the next few days'". CNN. Retrieved February 24, 2021.
- ^ Cha AE, Goldstein A (October 4, 2020). "Prospect of Trump's early hospital discharge mystifies doctors". The Washington Post. Retrieved October 5, 2020.
- ^ Mansfield E, Salman J, Voyles Pulver D (October 22, 2020). "Trump's campaign made stops nationwide. Coronavirus cases surged in his wake in at least five places". USA Today. Retrieved October 26, 2020.
- ^ Facher L (November 9, 2020). "Biden transition team unveils members of Covid-19 task force". Stat. Retrieved November 9, 2020.
- ^ Wang C (November 9, 2020). "U.S. coronavirus cases cross 10 million as outbreaks spike across the nation". CNBC. Retrieved November 9, 2020.
- ^ "10 Million People Have Tested Positive for Coronavirus in the United States". Time. Retrieved November 9, 2020.
- ^ "Pfizer says COVID-19 vaccine is looking 90% effective". Associated Press. November 9, 2020. Retrieved November 9, 2020.
- ^ Thomas K, Gelles D, Zimmer C (November 9, 2020). "Pfizer's Early Data Shows Vaccine Is More Than 90% Effective". The New York Times. ISSN 0362-4331. Archived from the original on November 9, 2020. Retrieved November 9, 2020.
- ^ Alonso-Zalidivar R (November 12, 2020). "Feds announce COVID-19 vaccine agreement with drug stores". Associated Press. Retrieved November 18, 2020.
- ^ O'Brien M (November 23, 2020). "Many Americans flying for Thanksgiving despite CDC pleas". The Republican. Archived from the original on February 6, 2021. Retrieved November 27, 2020.
- ^ Bacon J, Aspegren E, Hauck G (December 8, 2020). "Coronavirus updates: Joe Biden pledges to deliver 100M doses in 100 days; US reaches 15M infections; Ohio-State Michigan football game off". USA Today. Retrieved December 8, 2020.
- ^ Yan H (December 14, 2020). "Covid-19 now kills more than 1 American every minute. And the rate keeps accelerating as the death toll tops 300,000". CNN. Retrieved December 14, 2020.
- ^ Murphy M (December 24, 2020). "U.S. to require all air passengers arriving from U.K. to test negative for COVID-19". MarketWatch. Retrieved December 24, 2020.
- ^ Tufekci Z (December 31, 2020). "The Mutated Virus Is a Ticking Time Bomb". The Atlantic. Retrieved January 5, 2021.
- ^ "US reports its first known case of new UK Covid variant". The Guardian. December 29, 2020. Retrieved December 30, 2020.
- ^ Cohen L (January 1, 2021). "U.S. surpasses 20 million cases of coronavirus on first day of 2021". CBS News. Retrieved January 1, 2021.
- ^ Lim D (January 1, 2021). "U.S. coronavirus cases eclipse 20 million". Politico. Retrieved January 1, 2021.
- ^ Nedelman M (January 6, 2021). "CDC has found more than 50 US cases of coronavirus variant first identified in UK". CNN. Retrieved January 7, 2021.
- ^ Reimann N (January 8, 2021). "'Close To A Worst-Case Scenario' – Former CDC Director Issues 'Horrifying' Outlook For New Covid Strain". Forbes. Retrieved January 12, 2021.
- ^ Geddes L, Holpuch A (January 1, 2021). "New coronavirus variant may have been in US since October". The Guardian. Retrieved February 4, 2021.
- ^ Stone W (January 19, 2021). "As Death Rate Accelerates, U.S. Records 400,000 Lives Lost To The Coronavirus". NPR. Retrieved January 23, 2021.
- ^ Tompkins L (January 22, 2021). "U.S. coronavirus cases top 25 million". The New York Times. Archived from the original on December 28, 2021. Retrieved January 23, 2021.
- ^ Montague Z (January 30, 2021). "The C.D.C. Issues Mask Mandate for Domestic Travel". The New York Times. Retrieved April 14, 2022.
- ^ a b "Federal Mask Requirement for Transit". Federal Transit Administration. Archived from the original on January 4, 2022. Retrieved January 11, 2022.
- ^ Murphy H (April 13, 2022). "The C.D.C. extends the mask mandate on planes and public transit another two weeks". The New York Times. Retrieved April 14, 2022.
- ^ Huang P (February 22, 2021). "'A Loss To The Whole Society': U.S. COVID-19 Death Toll Reaches 500,000". NPR. Retrieved February 23, 2021.
- ^ Yeung J, McKeehan B. "More than 2,750 cases of coronavirus variants reported in the US". CNN. Retrieved March 5, 2021.
- ^ Sullivan S. "Biden directs states to make all adults eligible for vaccine by May 1". The Washington Post. ISSN 0190-8286. Retrieved March 12, 2021.
- ^ Maan A (March 24, 2021). "U.S. COVID-19 cases top 30 million as states race to vaccinate". Reuters. Retrieved March 24, 2021.
- ^ Cullinane S (March 27, 2021). "Record Covid-19 vaccinations don't mean it's time to relax, officials say". CNN. Retrieved March 27, 2021.
- ^ Haslett C (April 7, 2021). "UK variant has become most dominant COVID strain in US, CDC says". ABC News. Retrieved April 11, 2021.
- ^ Haseltine WA (April 12, 2021). "An Indian SARS-CoV-2 Variant Lands In California. More Danger Ahead?". Forbes. USA. Retrieved April 20, 2021.
- ^ Maxouris C (April 25, 2021). "Some parts of the US are more vulnerable to another hit by coronavirus. Here's why". CNN. Retrieved April 25, 2021.
- ^ Maxouris C (April 18, 2021). "Covid-19 vaccine demand is slowing in parts of the US. Now an uphill battle starts to get more shots into arms". CNN. Retrieved April 25, 2021.
- ^ Savidge M, Barajas A, Waldrop T (April 23, 2021). "Vaccine hesitancy in Hinds County, Mississippi, is a story shared elsewhere". CNN. Retrieved April 25, 2021.
- ^ Nedelman M (April 29, 2021). "More than a third of the US has been infected with Covid-19, CDC estimates". CNN.
- ^ Groppe M (May 4, 2021). "Biden's new goal: 70% of adults at least partially vaccinated by July 4". USA Today. Retrieved May 4, 2021.
- ^ Bebinger M, Farmer B (July 5, 2021). "As COVID Vaccinations Slow, Parts Of The U.S. Remain Far Behind 70% Goal". NPR. Retrieved July 5, 2021.
- ^ Sullivan B (May 6, 2021). "New Study Estimates More Than 900,000 People Have Died Of COVID-19 In U.S." NPR. Retrieved May 11, 2021.
- ^ Bowden J (May 9, 2021). "Fauci: 'No doubt' US has undercounted COVID-19 deaths". The Hill. Retrieved May 11, 2021.
- ^ Lovelace B Jr (May 13, 2021). "CDC says fully vaccinated people don't need to wear face masks indoors or outdoors in most settings". CNBC. Retrieved May 26, 2021.
- ^ Bursztynsky J (May 16, 2021). "CDC director defends telling fully vaccinated they can go without masks amid confusion in states, cities". CNBC. Retrieved May 26, 2021.
- ^ Har J, Kunzelman M (June 15, 2021). "US COVID-19 deaths hit 600,000, equal to yearly cancer toll". Associated Press. Retrieved June 16, 2021.
- ^ Soucheray S (June 29, 2021). "US COVID-19 cases rise, likely due to Delta variant". CIDRAP. Retrieved July 11, 2021.
- ^ Lovelace B Jr (July 7, 2021). "CDC data shows highly transmissible delta variant is now the dominant Covid strain in the U.S." CNBC. Retrieved July 11, 2021.
- ^ "Among the unvaccinated, Delta variant more than doubles risk of hospitalization", Los Angeles Times, August 28, 2021
- ^ Johnson A (August 1, 2021). "U.S. passes 35 million Covid cases as California tops 4 million". NBC News. Retrieved August 4, 2021.
- ^ Musumeci N, Davis C (August 9, 2021). "There are only 8 ICU beds available in the entire state of Arkansas as COVID-19 spikes". Yahoo! News. Retrieved August 9, 2021.
- ^ Caldwell T (August 13, 2021). "These 8 states make up half of US Covid-19 hospitalizations. And the surge among the unvaccinated is overwhelming health care workers". CNN. Retrieved August 13, 2021.
- ^ Holcombe M (August 31, 2021). "These 5 states have less than 10% of ICU beds left as Covid-19 overwhelms hospitals". CNN. Retrieved August 31, 2021.
- ^ Mundell E (September 8, 2021). "U.S. COVID-19 Cases Now Top 40 Million". U.S. News & World Report. Retrieved September 15, 2021.
- ^ Holcombe M (September 15, 2021). "1 in 500 US residents has died of Covid-19". CNN. Retrieved September 15, 2021.
- ^ Lovelace B Jr (September 20, 2021). "Covid is officially America's deadliest pandemic as U.S. fatalities surpass 1918 flu estimates". CNBC. Retrieved September 20, 2021.
- ^ Johnson CK (September 20, 2021). "COVID has killed about as many Americans as the 1918-19 flu". Associated Press. Retrieved September 20, 2021.
- ^ Ahluwalia S, Priya M L (October 1, 2021). "U.S. COVID-19 death toll hits 700,000". Reuters. Retrieved October 1, 2021.
- ^ Dugan K (October 18, 2021). "Coronavirus: Total US COVID-19 cases top 45 million as death toll surpasses 725,000". KIRO-TV. Retrieved October 23, 2021.
- ^ Collins K (November 26, 2021). "Biden restricts travel from South Africa and seven other countries starting Monday". CNN. Retrieved November 26, 2021.
- ^ a b c d "NY Times COVID 19 Dataset". NY Times COVID 19 Data. The New York Times. Retrieved March 19, 2021.
- ^ Benjamin Mueller, Eleanor Lutz (February 1, 2022). "U.S. Has Far Higher Covid Death Rate Than Other Wealthy Countries". The New York Times. Retrieved March 22, 2022.
- ^ Sheryl Gay Stolberg, Madeleine Ngo (March 9, 2022). "Uncertainty for Biden's Covid Plan After Aid Is Dropped From Spending Bill". The New York Times. Retrieved March 22, 2022.
- ^ Christina Jewett (March 20, 2022). "Fauci predicts an uptick in U.S. cases, saying it is not yet time to 'declare victory.'". The New York Times. Retrieved March 22, 2022.
- ^ "With fewer cases and less demand, many Covid-19 testing sites are shutting down". CNN. April 11, 2022.
- ^ Legaspi A (April 18, 2022). "Trump-Appointed Judge Deemed 'Not Qualified' by Bar Association Voids Mask Mandate on Planes, Other Travel". Rolling Stone. Archived from the original on April 18, 2022. Retrieved May 7, 2022.
- ^ Cameron M (April 21, 2022). "CDC Launches Appeal of Mask Mandate Decision". Business Traveler USA. Archived from the original on May 7, 2022. Retrieved May 7, 2022.
- ^ Salant J (April 27, 2022). "N.J. families of COVID victims push Congress to prevent a repeat pandemic". NJ.com. NJ Advance Media. Archived from the original on May 7, 2022. Retrieved May 7, 2022.
- ^ Cantu Trevino M (May 1, 2022). "Families gather for National Week of COVID Remembrance". Alice Echo-News Journal. Archived from the original on May 7, 2022. Retrieved May 7, 2022.
- ^ Chuck E, Siemaszko C (May 4, 2022). "Covid's toll in the U.S. reaches a once unfathomable number: 1 million deaths". NBC News. Archived from the original on May 4, 2022. Retrieved May 7, 2022.
- ^ "A Proclamation on Remembering the 1,000,000 Americans Lost to COVID-19". White House Briefing Room. May 12, 2022. Archived from the original on May 12, 2022. Retrieved May 13, 2022.
- ^ Tin A (June 9, 2022). "Here's when the White House says parents could start scheduling COVID vaccines for kids under 5". CBS News. Archived from the original on June 9, 2022. Retrieved June 10, 2022.
- ^ "Covid: US to drop test requirement for air travellers". BBC News. June 10, 2022. Archived from the original on June 10, 2022. Retrieved June 10, 2022.
- ^ "State emergency health orders during the coronavirus (COVID-19) pandemic, 2021-2022". BallotPedia. Retrieved July 14, 2022.
- ^ "State-level mask requirements in response to the coronavirus (COVID-19) pandemic, 2020-2022". BallotPedia. Retrieved July 14, 2022.
- ^ President Joe Biden: The 2022 60 Minutes Interview. Retrieved September 21, 2022 – via YouTube.
- ^ Liptak Kate Sullivan, Jamie Gumbrecht, Allie Malloy, Kevin (September 18, 2022). "Biden: 'The pandemic is over'". CNN. Retrieved September 20, 2022.
{{cite web}}: CS1 maint: multiple names: authors list (link) - ^ Berger E (September 24, 2022). "Biden's claim that Covid pandemic is over sparks debate among experts". The Guardian. Retrieved September 24, 2022.
- ^ "Monitoring Variants". Centers for Disease Control and Prevention. CDC. October 21, 2022. Retrieved December 12, 2022.
- ^ Mandavilli A (November 19, 2022). "Will Covid Boosters Prevent Another Wave? Scientists Aren't So Sure". The New York Times. Retrieved December 12, 2022.
- ^ "Improving COVID-19 Vaccine Equity". Centers for Disease Control and Prevention. CDC. October 28, 2022. Retrieved December 12, 2022.
- ^ "Update on COVID-19–Related Deaths". Centers for Disease Control and Prevention. CDC. November 18, 2022. Retrieved December 12, 2022.
- ^ LaFraniere S, Mueller B (November 22, 2022). "A Year After the Omicron Surge, Officials See a Reduced Covid Threat This Winter". The New York Times. Retrieved December 12, 2022.
- ^ Link-Gelles R, Allison Avrich Ciesla, Katherine E. Fleming-Dutra, Zachary R. Smith, Amadea Britton, Ryan E. Wiegand, et al. (November 22, 2022). "Effectiveness of Bivalent mRNA Vaccines in Preventing Symptomatic SARS-CoV-2 Infection — Increasing Community Access to Testing Program, United States, September–November 2022". MMWR. Morbidity and Mortality Weekly Report. 71 (48). CDC: 1526–1530. doi:10.15585/mmwr.mm7148e1. PMC 9721148. PMID 36454688. Retrieved December 12, 2022.
- ^ Stolberg SG, Mueller B (December 28, 2022). "US to Require Negative Covid Tests for Travelers From China". The New York Times. Retrieved January 6, 2023.
- ^ Kimball S (December 30, 2022). "Highly immune evasive omicron XBB.1.5 variant is quickly becoming dominant in U.S. as it doubles weekly". CNBC. Retrieved January 6, 2023.
- ^ Klein B, Luhby T (January 11, 2023). "Biden administration renews Covid-19 public health emergency". CNN. Archived from the original on January 12, 2023. Retrieved January 12, 2023.
- ^ Habeshian S (January 28, 2023). "SNAP benefits returning to pre-COVID amounts in February". Axios. Archived from the original on January 29, 2023. Retrieved January 29, 2023.
- ^ "2022 State Senate Elections Map". 270 to Win. Archived from the original on December 2, 2022. Retrieved January 29, 2023.
- ^ Staff Writer (January 31, 2023). "U.S. to end COVID-19 emergency declarations on May 11". Reuters. Retrieved January 31, 2023.
- ^ ALECCIA J (February 23, 2023). "US ending extra help for groceries that started during COVID". ABC News.
- ^ a b Richards Z (April 10, 2023). "Biden signs bill ending Covid national emergency". NBC News. Retrieved April 11, 2023.
- ^ "Bill Signed: H.J.Res. 7". The White House. whitehouse.gov. April 10, 2023. Retrieved April 10, 2023.
On Monday, April 10, 2023, the President signed into law: H.J.Res. 7, which terminates the national emergency related to the COVID-19 pandemic.
- ^ Goodman B, McPhillips D (July 28, 2023). "Your summer cold could be Covid-19, as the nation goes into a late summer wave". CNN. Archived from the original on July 29, 2023. Retrieved July 29, 2023.
- ^ Lee BY (August 8, 2023). "Walgreens Shows Highest Covid-19 Test Positivity Levels Since May 2021". Forbes. Archived from the original on August 9, 2023. Retrieved August 8, 2023.
- ^ Bosman J (August 28, 2023). "Not Over Yet: Late-Summer Covid Wave Brings Warning of More to Come". The New York Times. Archived from the original on August 28, 2023. Retrieved August 28, 2023.
- ^ Lonas L, Choi J (September 5, 2023). "COVID-19 raises anxiety at start of new school year". The Hill. Archived from the original on September 5, 2023. Retrieved September 5, 2023.
- ^ Tyko K (September 25, 2023). "Free COVID tests from government available again". Axios. Retrieved September 25, 2023.
- ^ Nazzaro M (September 25, 2023). "How to order free COVID test kits". The Hill. Archived from the original on September 25, 2023. Retrieved September 25, 2023.
- ^ Brooks B (January 4, 2024). "Mask mandates return at some US hospitals as COVID, flu jump". Reuters. Archived from the original on January 4, 2024. Retrieved January 4, 2024.
- ^ Propper D (January 3, 2024). "Mask mandates back at NYC hospitals as COVID and flu cases increase". New York Post. Archived from the original on January 4, 2024. Retrieved January 4, 2024.
- ^ Prater E (January 5, 2024). "Highly mutated COVID variant 'Pirola' JN.1 is fueling the pandemic's second highest U.S. wave—and it's still growing". Fortune. Archived from the original on January 6, 2024. Retrieved January 7, 2024.
- ^ Huguelet A (January 7, 2024). "St. Louis backs off mask mandate for city workers". St. Louis Post-Dispatch. Archived from the original on January 7, 2024. Retrieved January 8, 2024.
- ^ Edelman S (January 13, 2024). "FDNY orders all first-responders to mask up amid spike in contagious diseases". New York Post. Archived from the original on January 13, 2024. Retrieved January 15, 2024.
- ^ Palm I (January 18, 2024). "California health officials shorten COVID isolation period to 1 day". KTLA. Archived from the original on January 19, 2024. Retrieved January 19, 2024.
- ^ Mandavilli A (March 1, 2024). "C.D.C. Shortens Isolation Period for People With Covid". The New York Times. Archived from the original on March 1, 2024. Retrieved March 11, 2024.
- ^ Farber M (January 28, 2020). "China spurned CDC offer to send a team to help contain coronavirus: US Health Secretary". Fox News.
- ^ Allyn B (February 8, 2020). "China's Coronavirus Death Toll Surpasses SARS Pandemic". NPR. Retrieved August 12, 2020.
- ^ "C.D.C. and W.H.O. Offers to Help China Have Been Ignored for Weeks". The New York Times. February 7, 2020. Archived from the original on February 7, 2020.
- ^ "Boeing donating 250,000 medical masks to battle coronavirus in China". KOMO-TV. January 29, 2020.
- ^ "The United States Announces Assistance To Combat the Novel Coronavirus". U.S. Dept. of State. February 7, 2020.
- ^ Guzman J (February 7, 2020). "US pledges $100 million to help fight coronavirus in China". The Hill. Retrieved April 11, 2020.
- ^ "Contact tracing may help avoid another lockdown. Can it work in the U.S.?". May 29, 2020.
- ^ Cunningham PW (June 15, 2020). "Analysis | The Health 202: U.S. isn't ready for the contact tracing it needs to stem the coronavirus". The Washington Post.
- ^ "New Contact Tracing Apps Need Access To Users' Private Data To Control Spread Of COVID-19". KPIX-TV. July 1, 2020. Retrieved July 7, 2020.
- ^ Commissioner Oo (October 22, 2020). "FDA Approves First Treatment for COVID-19". US Food and Drug Administration (FDA). Retrieved December 1, 2020.
- ^ "Coronavirus (COVID-19) Update: FDA Authorizes Drug Combination for Treatment of COVID-19". US Food and Drug Administration (FDA). November 23, 2020. Retrieved December 1, 2020.
- ^ a b "U.S. Moves to Expand Array of Drug Therapies Deployed Against Coronavirus". The Wall Street Journal. March 19, 2020.
- ^ Braun E (March 30, 2020). "In France, controversial doctor stirs coronavirus debate". Politico. Retrieved September 2, 2020.
- ^ "Coronavirus (COVID-19) Update: Daily Roundup March 30, 2020". US Food and Drug Administration (FDA). March 30, 2020. Retrieved September 2, 2020.
- ^ Koppock K (March 13, 2020). "FDA Announces Two Drugs Given 'Compassionate Use' Status in Treating COVID-19". Pharmacy Times. Archived from the original on April 3, 2020. Retrieved April 25, 2020.
- ^ Wise J (March 30, 2020). "FDA issues emergency-use authorization for anti-malaria drugs amid coronavirus outbreak". The Hill. Retrieved March 30, 2020.
- ^ Research Cf (June 26, 2020). "FDA cautions against use of hydroxychloroquine or chloroquine for COVID-19 outside of the hospital setting or a clinical trial due to risk of heart rhythm problems". US Food and Drug Administration (FDA).
- ^ Gittleson B, Phelps J, Cathey L (July 28, 2020). "Trump doubles down on defense of hydroxychloroquine to treat COVID-19 despite efficacy concerns". ABC News. Retrieved September 2, 2020.
- ^ "COVID-19 (coronavirus) vaccine: Get the facts". Mayo Clinic. April 22, 2020.
- ^ a b Gottlieb S (April 26, 2020). "America Needs to Win the Coronavirus Vaccine Race". The Wall Street Journal.
- ^ "Guide to the Cares Act". United States Senate Committee on Small Business and Entrepreneurship. Retrieved August 15, 2020.
- ^ Pfizer and BioNTech to Submit Emergency Use Authorization Request Today to the U.S. FDA for COVID-19 Vaccine. Pfizer. November 20, 2020. Retrieved November 20, 2020.
- ^ Park A (November 20, 2020). "Exclusive: Pfizer CEO Discusses Submitting the First COVID-19 Vaccine Clearance Request to the FDA". Time. Retrieved November 20, 2020.
- ^
 This article incorporates text from this source, which is in the public domain: FDA Takes Key Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for First COVID-19 Vaccine. US Food and Drug Administration (FDA). December 11, 2020. Retrieved December 11, 2020.
This article incorporates text from this source, which is in the public domain: FDA Takes Key Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for First COVID-19 Vaccine. US Food and Drug Administration (FDA). December 11, 2020. Retrieved December 11, 2020.
- ^ Oliver SE, Gargano JW, Marin M, Wallace M, Curran KG, Chamberland M, et al. (December 2020). "The Advisory Committee on Immunization Practices' Interim Recommendation for Use of Pfizer–BioNTech COVID-19 Vaccine – United States, December 2020" (PDF). MMWR Morb Mortal Wkly Rep. 69 (50): 1922–1924. doi:10.15585/mmwr.mm6950e2. PMC 7745957. PMID 33332292.
- ^
 This article incorporates text from this source, which is in the public domain: FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine. US Food and Drug Administration (FDA). Retrieved December 18, 2020.
This article incorporates text from this source, which is in the public domain: FDA Takes Additional Action in Fight Against COVID-19 By Issuing Emergency Use Authorization for Second COVID-19 Vaccine. US Food and Drug Administration (FDA). Retrieved December 18, 2020.
- ^ Oliver SE, Gargano JW, Marin M, Wallace M, Curran KG, Chamberland M, et al. (December 2020). "The Advisory Committee on Immunization Practices' Interim Recommendation for Use of Moderna COVID-19 Vaccine – United States, December 2020" (PDF). MMWR. Morbidity and Mortality Weekly Report. 69 (5152): 1653–1656. doi:10.15585/mmwr.mm695152e1. PMC 9191904. PMID 33382675. S2CID 229945697.
- ^ "Moderna Applies for Emergency F.D.A. Approval for Its Coronavirus Vaccine". The New York Times. November 30, 2020. Archived from the original on November 30, 2020. Retrieved November 30, 2020.
- ^ Moderna Announces Primary Efficacy Analysis in Phase 3 COVE Study for Its COVID-19 Vaccine Candidate and Filing Today with U.S. FDA for Emergency Use Authorization. Moderna, Inc. November 30, 2020. Archived from the original on November 30, 2020. Retrieved November 30, 2020.
- ^ Pereira I (December 14, 2020). "US administers 1st doses of Pfizer coronavirus vaccine". ABC News. Retrieved March 6, 2021.
- ^ Aleem Z (March 15, 2020). "A new poll shows a startling partisan divide on the dangers of the coronavirus". Vox.
- ^ Allyn B, Sprunt B (March 17, 2020). "Poll: As Coronavirus Spreads, Fewer Americans See Pandemic As A Real Threat". NPR. Retrieved March 25, 2020.
- ^ Murray M (March 15, 2020). "Sixty percent believe worst is yet to come for the U.S. in coronavirus pandemic; Public attitudes about the coronavirus response are split along partisan lines in a new NBC News/Wall Street Journal poll". NBC News.
- ^ a b Weissmann J (March 17, 2020). "Democrats Are Being Much, Much More Careful About the Coronavirus Than Republicans". Slate.
- ^ Agiesta J (May 12, 2020). "CNN Poll: Negative ratings for government handling of coronavirus persist". CNN. Retrieved May 13, 2020.
- ^ Wike R, Fetterolf J, Mordecai M (September 15, 2020). "U.S. Image Plummets Internationally as Most Say Country Has Handled Coronavirus Badly". Pew Research Center. Retrieved September 26, 2020.
- ^ "Determination of the February 2020 Peak in US Economic Activity". National Bureau of Economic Research. June 8, 2020.
- ^ Long H (April 29, 2020). "U.S. economy shrank 4.8 percent in first quarter, the biggest decline since the Great Recession". The Washington Post. Retrieved April 29, 2020.
- ^ Long H (May 8, 2020). "U.S. unemployment rate soars to 14.7 percent, the worst since the Depression era". The Washington Post. Retrieved May 8, 2020.
- ^ Abelson R (March 28, 2020). "Coronavirus May Add Billions to the Nation's Health Care Bill". The New York Times. Archived from the original on March 28, 2020. Retrieved April 1, 2020.
- ^ Goolsbee A (2021). "Fear, Lockdown, and Diversion: Comparing Drivers of Pandemic Economic Decline 2020". Journal of Public Economics. 193. Becker Friedman Institute for Research in Economics: 104311. doi:10.1016/j.jpubeco.2020.104311. PMC 7687454. PMID 33262548. Retrieved June 23, 2020.
- ^ Tapee A (July 31, 2020). "US economy posts its worst drop on record". CNN. Retrieved August 19, 2020.
- ^ Faelli F, Rovit S, Apps C, Johns L (September 23, 2020). "Shaping the Consumer of the Future". Bain & Company. Retrieved October 3, 2020.
- ^ Rummler O (May 14, 2020). "OpenTable forecasts 25% of U.S. restaurants to shutter permanently". Axios Media. Retrieved October 4, 2020.
- ^ "43 million Americans at risk of eviction as relief programs and moratorium expire: "It's a nightmare"". CBS News. July 31, 2020.
- ^ "32% of Americans had outstanding housing payments at the beginning of August". CNBC. August 6, 2020.
- ^ "'A Homeless Pandemic' Looms As 30 Million Are At Risk Of Eviction". NPR. August 10, 2020.
- ^ Ivanova I (November 27, 2020). "Nearly 19 million Americans could lose their homes when eviction limits expire Dec. 31". CBS News. Retrieved December 7, 2020.
- ^ "As Stimulus Talks Stalemate, New Report Finds 40 Million Americans Could Be At Risk Of Eviction". Forbes. August 7, 2020.
- ^ "Millions of Americans at risk of eviction after moratorium expired". Fox Business. August 12, 2020.
- ^ "Yelp data shows 60% of business closures due to the coronavirus pandemic are now permanent". CNBC. September 16, 2020.
- ^ a b US Bureau of Labor Statistics (January 1, 1939). "All Employees: Total Nonfarm Payrolls". FRED, Federal Reserve Bank of St. Louis. Retrieved June 4, 2019.
- ^ US Bureau of Labor Statistics (January 1, 1948). "Civilian Unemployment Rate". FRED, Federal Reserve Bank of St. Louis. Retrieved June 4, 2019.
- ^ US Bureau of Labor Statistics (January 1, 1948). "Unemployment level". FRED, Federal Reserve Bank of St. Louis. Retrieved June 20, 2020.
- ^ US Bureau of Labor Statistics (January 1, 1948). "Employment-Population Ration 25-54 Yrs". FRED, Federal Reserve Bank of St. Louis. Retrieved June 22, 2020.
- ^ US Bureau of Labor Statistics (January 1, 1947). "Consumer Price Index for All Urban Consumers: All Items". FRED, Federal Reserve Bank of St. Louis. Retrieved June 4, 2019.
- ^ "S&P 500". fred.stlouisfed.org. June 3, 2019. Retrieved June 4, 2019.
- ^ "The Debt to the Penny and Who Holds It". treasury.gov. June 10, 2021. Retrieved June 10, 2021.
- ^ Fang M (March 16, 2021). "There Have Been Nearly 4,000 Incidents Of Anti-Asian Racism In The Last Year". HuffPost. Retrieved March 16, 2021.
- ^ Van Beusekom M (September 25, 2020). "Studies spotlight COVID racial health disparities, similarities". CIDRAP – Center for Infectious Disease Research and Policy, University of Minnesota. Retrieved September 27, 2020.
- ^ "The color of coronavirus: COVID-19 deaths by race and ethnicity in the U.S." APM Research Lab: American Public Media. Retrieved September 28, 2020.
- ^ Hollie Silverman, Konstantin Toropin, Sara Sidner, Leslie Perrot. "Navajo Nation surpasses New York state for the highest Covid-19 infection rate in the US". CNN. Retrieved May 28, 2020.
- ^ "Cases, Data, and Surveillance". U.S. Centers for Disease Control and Prevention (CDC). February 11, 2020. Retrieved July 15, 2021.
- ^ Chowkwanyun M, Reed AL (July 2020). "Racial Health Disparities and Covid-19 – Caution and Context". New England Journal of Medicine. 383 (3): 201–3. doi:10.1056/NEJMp2012910. ISSN 0028-4793. PMID 32374952. S2CID 218534431.
- ^ "The COVID Racial Data Tracker". The COVID Tracking Project (The Atlantic Monthly Group). Retrieved September 28, 2020.
- ^ Wood D (September 23, 2020). "As Pandemic Deaths Add Up, Racial Disparities Persist – And In Some Cases Worsen". NPR. Retrieved September 27, 2020.
- ^ "New Report Confirms U.S. Life Expectancy has Declined to Lowest Level Since 1996". cdc.gov. December 20, 2022. Retrieved December 22, 2022.
- ^ "Map: Coronavirus and School Closures". Education Week. Editorial Projects in Education. March 7, 2020. Retrieved April 23, 2020.
- ^ "Higher Education Responses to Coronavirus (COVID-19)". www.ncsl.org. Retrieved March 30, 2024.
- ^ Dutta T, Agley J (March 18, 2024). "College leadership decisions and experiences during the COVID-19 pandemic: an elite interview study". Journal of American College Health: 1–11. doi:10.1080/07448481.2024.2328139. ISSN 0744-8481. PMID 38498604.
- ^ Panetta G (March 30, 2020). "Trump baselessly claimed that expanding voting access would lead to a Republican never being elected in America again". Business Insider.
- ^ Samuels B (April 7, 2020). "Trump defends his mail-in ballot after calling vote-by-mail 'corrupt'". The Hill. Archived from the original on February 26, 2021.
- ^ Parks M (April 7, 2020). "Fact Check: Is Mail Ballot Fraud As Rampant As President Trump Says It Is?". NPR.
- ^ Warshaw C, Vavreck L, Baxter-King R (October 2020). "Fatalities from COVID-19 are reducing Americans' support for Republicans at every level of federal office". Science Advances. 6 (44): eabd8564. Bibcode:2020SciA....6.8564W. doi:10.1126/sciadv.abd8564. ISSN 2375-2548. PMC 7608793. PMID 33127688.
- ^ CDC COVID Data Tracker: Vaccinations in the US. View: People. Show: Fully Vaccinated. Population: Total Population. Resulting map will be labeled: "Percent of People Fully Vaccinated Reported to the CDC by State/Territory and for Select Federal Entities for the Total Population". Hover or click on locations for more data.
- ^ U.S. COVID-19 vaccine tracker: See your state's progress. From the Mayo Clinic. Hover on the states on the map at the source page for exact numbers for the fully vaccinated. Click on the "data sources" link in the first paragraph to see that the data is from the Centers for Disease Control and Prevention.
- ^ Timeline of daily COVID-19 vaccine doses administered in the US. Click on the chart tab. Then click the download tab, and then the SVG link to get the SVG file. The table tab has a table of the data by date. The sources tab says the data is from the COVID-19 Data Repository by the Center for Systems Science and Engineering (CSSE) at Johns Hopkins University. The graph on the chart tab at the source is interactive and provides more detail. For example, run your cursor over the graph to see the date and the number vaccinated that day. The actual number may be higher or lower since a rolling 7-day average is used.
- ^ Thomas K, Weiland N, LaFraniere S (December 10, 2020). "F.D.A. Advisory Panel Gives Green Light to Pfizer Vaccine". The New York Times.
- ^ Lovelace B Jr (December 19, 2020). "FDA approves second Covid vaccine for emergency use as it clears Moderna's for U.S. distribution". CNBC.
- ^ Machemer T. "FDA Approves Johnson & Johnson Vaccine, Another Valuable Tool Against Covid-19". Smithsonian Magazine.
- ^ Anthes E, Ngo M, Sullivan E (May 30, 2021) [2021-04-19]. "Adults in all U.S. states are now eligible for vaccination, hitting Biden's target. Half have had at least one dose". The New York Times. Archived from the original on September 13, 2024. Retrieved October 9, 2024.
- ^ Johnson CY (May 10, 2021). "FDA authorizes Pfizer coronavirus vaccine for adolescents 12 to 15 years old". The Washington Post. Retrieved May 10, 2021 – via MSN.
- ^ Lovelace B Jr (August 23, 2021). "FDA grants full approval to Pfizer-BioNTech's Covid shot, clearing path to more vaccine mandates". CNBC. Retrieved August 23, 2021.
- ^ Klein B, Stracqualursi V, Sullivan K (January 21, 2021). "Biden unveils Covid-19 plan based on 'science not politics' as he signs new initiatives". CNN. Retrieved March 12, 2021.
- ^ "COVID-19: US president Joe Biden signs 10 executive orders to curb spread of coronavirus". Sky News. Retrieved March 12, 2021.
- ^ "100 Million Shots In 100 Days: Is Biden's COVID-19 Vaccination Goal Achievable?". NPR. Retrieved March 12, 2021.
- ^ "Biden Eyes New Goal After US Clears 100M Shots Since Jan. 20". HuffPost. March 20, 2021.
- ^ Mangan D, Lovelace B Jr (March 25, 2021). "Biden sets new Covid vaccine goal of 200 million shots within his first 100 days: 'I believe we can do it'". CNBC. Retrieved March 27, 2021.
- ^ Pettypiece S, Shabad R (April 21, 2021). "'We did it': Biden celebrates U.S. hitting milestone of 200 million doses in his first 100 days". NBCNews.com. Retrieved April 22, 2021.
- ^ "Biden announces sweeping vaccine mandates affecting millions of workers". NBC News. September 13, 2021. Archived from the original on September 13, 2021. Retrieved January 27, 2022.
- ^ "Federal Register :: COVID-19 Vaccination and Testing; Emergency Temporary Standard". Federal Register. January 27, 2022. Archived from the original on January 27, 2022. Retrieved January 27, 2022.
- ^ "21A244 National Federation of Independent Business v. OSHA (01/13/2022)" (PDF). Supreme Count. Archived from the original (PDF) on January 13, 2022. Retrieved January 27, 2022.
- ^ Fitzpatrick MC, Moghadas SM, Pandey A, Galvani AP (December 13, 2022). "Two Years of U.S. COVID-19 Vaccines Have Prevented Millions of Hospitalizations and Deaths". commonwealthfund.org. doi:10.26099/whsf-fp90. Retrieved August 7, 2023.
- ^ Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC (June 23, 2022). "Global impact of the first year of COVID-19 vaccination: a mathematical modelling study". The Lancet Infectious Diseases. 22 (9): 1293–1302. doi:10.1016/s1473-3099(22)00320-6. ISSN 1473-3099. PMC 9225255. PMID 35753318.
- ^ "COVID-19 vaccines saved nearly 20 million lives in a year, study says". CBS News. June 24, 2022. Retrieved June 27, 2022.
- ^ Steele MK, Couture A, Reed C, Iuliano D, Whitaker M, Fast H, et al. (July 6, 2022). "Estimated Number of COVID-19 Infections, Hospitalizations, and Deaths Prevented Among Vaccinated Persons in the US, December 2020 to September 2021". JAMA Network Open. 5 (7): e2220385. doi:10.1001/jamanetworkopen.2022.20385. ISSN 2574-3805. PMC 9260489. PMID 35793085.
- ^ "COVID vaccination progress: Only 1 in 5 say they won't get a jab; White House says pace of shots accelerating". USA Today. August 31, 2021.
- ^ "Biden calls on private companies to issue vaccine requirements". NBC News. August 23, 2021.
- ^ a b "Employers Want You To Get Vaccinated. This One Is Offering A $1,000 Bonus." NPR. August 17, 2021.
- ^ Abril D (August 19, 2021). "As delta variant spreads, some companies with vaccine mandates deploy tech to verify records". The Washington Post. Retrieved October 16, 2021.
- ^ "Most Americans Now Support Mask And Vaccination Mandates. Which Companies Will Follow Their Lead?". Fortune. August 23, 2021.
- ^ a b Leonhardt D (March 11, 2024). "The Fourth Anniversary of the Covid Pandemic". The New York Times. Archived from the original on March 11, 2024. "Data excludes Alaska. Sources: C.D.C. Wonder; Edison Research. (Chart) By The New York Times. Source credits chart to Ashley Wu.
- ^ "Data on COVID-19 mortality by vaccination status". Our World in Data (CDC data). April 2023. Archived from the original on October 16, 2023.
Data source: Centers for Disease Control and Prevention, Vaccine Breakthrough/Surveillance and Analytics Team.
- ^ Yang ZR, Jiang YW, Li FX, Liu D, Lin TF, Zhao ZY, et al. (April 2023). "Efficacy of SARS-CoV-2 vaccines and the dose-response relationship with three major antibodies: a systematic review and meta-analysis of randomised controlled trials". The Lancet. Microbe. 4 (4): e236 – e246. doi:10.1016/S2666-5247(22)00390-1. PMC 9974155. PMID 36868258.
- ^ Holcombe M, Waldrop T (September 11, 2021). "CDC study: Unvaccinated 11 times more likely to die from Covid-19". CNN. Retrieved September 11, 2021.
- ^ Scobie HM, Johnson AG, Suthar AB, Severson R, Alden NB, Balter S, et al. (September 2021). "Monitoring Incidence of COVID-19 Cases, Hospitalizations, and Deaths, by Vaccination Status - 13 U.S. Jurisdictions, April 4-July 17, 2021" (PDF). MMWR. Morbidity and Mortality Weekly Report. 70 (37): 1284–1290. doi:10.15585/mmwr.mm7037e1. PMC 8445374. PMID 34529637.
- ^ Fowlkes A, Gaglani M, Groover K, Thiese MS, Tyner H, Ellingson K (August 2021). "Effectiveness of COVID-19 Vaccines in Preventing SARS-CoV-2 Infection Among Frontline Workers Before and During B.1.617.2 (Delta) Variant Predominance - Eight U.S. Locations, December 2020-August 2021" (PDF). MMWR. Morbidity and Mortality Weekly Report. 70 (34): 1167–1169. doi:10.15585/mmwr.mm7034e4. PMC 8389394. PMID 34437521.
- ^ Schreiber M, Chayka K, Chayka K, Beyerstein L, Beyerstein L, Wilson J, et al. (July 1, 2021). "The Delta Covid Variant's Urgent Message for America". The New Republic. ISSN 0028-6583. Archived from the original on August 28, 2021. Retrieved October 28, 2021.
- ^ "Among the unvaccinated, Delta variant more than doubles risk of hospitalization". Los Angeles Times. August 28, 2021. Archived from the original on November 8, 2021.
- ^ "WHO/ECDC: Nearly half a million lives saved by COVID-19 vaccination in less than a year". November 25, 2021.
- ^ Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC (June 2022). "Global impact of the first year of COVID-19 vaccination: a mathematical modelling study". The Lancet Infectious Diseases. 22 (9): 1293–1302. doi:10.1016/s1473-3099(22)00320-6. PMC 9225255. PMID 35753318.
- ^ "Coronavirus (COVID-19) booster vaccine". NHS. Government Digital Service. September 17, 2021. Retrieved December 11, 2021.
- ^ SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 31 (PDF) (Briefing). Public Health England. December 10, 2021. pp. 3–5, 20–22. GOV-10645. Archived (PDF) from the original on December 18, 2021. Retrieved December 10, 2021.
- ^ Gore D (February 9, 2022). "Latest CDC Data: Unvaccinated Adults 97 Times More Likely to Die from COVID-19 Than Boosted Adults". FactCheck.org. Retrieved February 11, 2022.
- ^ Lee AR, Wong SY, Chai LY, Lee SC, Lee MX, Muthiah MD, et al. (March 2022). "Efficacy of covid-19 vaccines in immunocompromised patients: systematic review and meta-analysis". BMJ. 376: e068632. doi:10.1136/bmj-2021-068632. PMC 8889026. PMID 35236664.
- ^ Greenberger LM, Saltzman LA, Senefeld JW, Johnson PW, DeGennaro LJ, Nichols GL (August 2021). "Antibody response to SARS-CoV-2 vaccines in patients with hematologic malignancies". Cancer Cell. 39 (8): 1031–1033. doi:10.1016/j.ccell.2021.07.012. PMC 8295014. PMID 34331856.
- ^ Stein C, Nassereldine H, Sorensen RJ, Amlag JO, Bisignano C, Byrne S, et al. (February 2023). "Past SARS-CoV-2 infection protection against re-infection: a systematic review and meta-analysis". The Lancet. 401 (10379): 833–842. doi:10.1016/S0140-6736(22)02465-5. ISSN 0140-6736. PMC 9998097. PMID 36930674.
- ^ Payne AB (2024). "Effectiveness of Bivalent mRNA COVID-19 Vaccines in Preventing COVID-19–Related Thromboembolic Events Among Medicare Enrollees Aged ≥65 Years and Those with End Stage Renal Disease — United States, September 2022–March 2023". MMWR. Morbidity and Mortality Weekly Report. 73 (1): 16–23. doi:10.15585/mmwr.mm7301a4. ISSN 0149-2195. PMC 10794061. PMID 38206877. Archived from the original on January 14, 2024. Retrieved January 14, 2024.
- ^ Mole B (January 12, 2024). "COVID shots protect against COVID-related strokes, heart attacks, study finds". Ars Technica. Archived from the original on January 14, 2024. Retrieved January 14, 2024.
- ^ The Associated Press (February 18, 2022). "California adopts nation's first endemic virus policy". NPR. Retrieved June 8, 2022.
- ^ "Biden says Americans can 'remove their masks,' resume pre-Covid work, life routines". NBC News. March 2, 2022. Retrieved March 2, 2022.
- ^ Keith T (March 2, 2022). "The White House has a new plan for COVID-19 aimed at getting things back to normal". NPR. Retrieved March 2, 2022.
- ^ "Dr. Fauci on why the U.S. Is 'out of the pandemic phase'". PBS NewsHour. April 26, 2022.
- ^ Achenbach J (April 27, 2022). "Fauci says U.S. is out of coronavirus 'pandemic phase'". The Washington Post. Retrieved May 21, 2022.
- ^ "'COVID-19 is back in Rhode Island,' Central Falls health strategist warns". The Boston Globe.
- ^ Pelley S (September 18, 2022). "President Joe Biden: The 2022 60 Minutes Interview". CBS News. Retrieved September 19, 2022.
- ^ a b Miguel K (February 28, 2020). "Here's a look at some of history's worst pandemics that have killed millions". KGO-TV. Retrieved March 22, 2020.
- ^ Lileks J (March 18, 2020). "How the news media played down the pandemics of yore, from Spanish flu to Swine flu". Star Tribune. Retrieved March 22, 2020.
- ^ Brown J (March 3, 2020). "The Coronavirus Is No 1918 Pandemic". The Atlantic. Retrieved March 22, 2020.
- ^ "These are the countries best prepared for health emergencies". World Economic Forum. February 12, 2020.
- ^ Maizland L, Nayeem T, Kumar A (March 24, 2020). "What a Global Health Survey Found Months Before the Coronavirus Pandemic". Council on Foreign Relations.
- ^ Cohen Z (April 10, 2020). "Trump administration shuttered pandemic monitoring program, then scrambled to extend it". CNN. Retrieved July 10, 2020.
- ^ McNeil DG Jr (October 25, 2019). "Scientists Were Hunting for the Next Ebola. Now the U.S. Has Cut Off Their Funding". The New York Times. Retrieved July 11, 2020.
- ^ Baumgaertner E, Rainey J (April 2, 2020). "Trump administration ended pandemic early-warning program to detect coronaviruses". Los Angeles Times. Retrieved May 30, 2020.
- ^ McNeil DG Jr, Kaplan T (August 30, 2020). "U.S. Will Revive Global Virus-Hunting Effort Ended Last Year". The New York Times. Retrieved October 21, 2020.
- ^ "Cases, Data, and Surveillance". Centers for Disease Control and Prevention. February 11, 2020. Retrieved December 19, 2021.
- ^ Iuliano AD, Chang HH, Patel NN, Threlkel R, Kniss K, Reich J, et al. (July 13, 2021). "Estimating Under-recognized COVID-19 Deaths, United States, March 2020-May 2021 using an Excess Mortality Modelling Approach". The Lancet Regional Health – Americas. 1: 100019. doi:10.1016/j.lana.2021.100019. ISSN 2667-193X. PMC 8275579. PMID 34386789.
- ^ "Excess Deaths Associated with COVID-19". Centers for Disease Control and Prevention—National Center for Health Statistics. Retrieved July 21, 2020.
- ^ Woolf SH, Chapman DA, Sabo RT (April 2, 2021). "Excess Deaths From COVID-19 and Other Causes in the US, March 1, 2020, to January 2, 2021". JAMA. 325 (17): 1786–1789. doi:10.1001/jama.2021.5199. PMC 8019132. PMID 33797550. S2CID 232763669.
- ^ Multiple sources:
- Eastwood J, Overberg P, Barry R (April 4, 2020). "Why We Don't Know How Many Americans Are Infected With Coronavirus—and Might Never Know". The Wall Street Journal.
- "Lack of testing clouds virus picture on the North Coast | Coronavirus". The Astorian. April 8, 2020. Retrieved April 27, 2020.
- Bosman J (April 11, 2020). "Official Counts Understate the U.S. Coronavirus Death Toll—The New York Times". The New York Times. Retrieved April 27, 2020.
- "US coronavirus map: Tracking the United States outbreak". USA Today. January 28, 2020. Retrieved April 27, 2020.
- Roberts JJ (April 3, 2020). "Can the private sector provide better coronavirus data? Experts are skeptical". Fortune. Retrieved April 10, 2020.
Confirmed coronavirus cases in the U.S. crossed 200,000 on Thursday, but experts agree the actual number of infected people is much higher. The lack of reliable data—a persistent problem since the pandemic began—has made it impossible to determine the actual size of the outbreak, hampering the U.S. response.
- Myer R, Madrigal A (April 16, 2020). "A New Statistic Reveals Why America's COVID-19 Numbers Are Flat". The Atlantic. Retrieved April 19, 2020.
- ^ Kliff S, Bosman J (April 5, 2020). "Official Counts Understate the U.S. Coronavirus Death Toll". The New York Times. Retrieved April 5, 2020.
- ^ Abdelmalek M, Margolin J, Katersky A, David E (April 7, 2020). "Coronavirus death toll in US likely worse than numbers say". ABC News. Retrieved April 10, 2020.
- ^ Brown E, Reinhard B, Davis AC (April 5, 2020). "Coronavirus death toll: Americans are almost certainly dying of covid-19 but being left out of the official count". The Washington Post. Retrieved April 10, 2020.
- ^ Swan J, Baker S (May 6, 2020). "Trump and some top aides question the accuracy of virus death toll". Axios.
Further reading
[edit]- The Covid Crisis Group (April 25, 2023). Lessons from the Covid War: An Investigative Report. PublicAffairs. ISBN 978-1-5417-0380-3.
Contributors: Danielle Allen • John M. Barry • John Bridgeland • Michael Callahan • Nicholas A. Christakis • Doug Criscitello • Charity Dean • Victor Dzau • Gary Edson • Ezekiel Emanuel • Ruth Faden • Baruch Fischhoff • Margaret "Peggy" Hamburg • Melissa Harvey • Richard Hatchett • David Heymann • Kendall Hoyt • Andrew Kilianski • James Lawler • Alexander J. Lazar • James Le Duc • Marc Lipsitch • Anup Malani • Monique K. Mansoura • Mark McClellan • Carter Mecher • Michael Osterholm • David A. Relman • Robert Rodriguez • Carl Schramm • Emily Silverman • Kristin Urquiza • Rajeev Venkayya • Philip Zelikow
[1]
External links
[edit]- COVID-19 Therapeutics Locator at Administration for Strategic Preparedness and Response.
- COVID-19 at Centers for Disease Control and Prevention (CDC).
- The Covid Tracking Project.
- Coverage of federal response. C-SPAN.
- Covid Historical data at Johns Hopkins University & Medicine.
- Coronavirus disease (COVID-19) advice for the public: Mythbusters at World Health Organization (WHO).
- [Covid in the U.S.: Latest Maps, Case and Death Counts - The New York Times Coronavirus in the U.S.: Latest Map and Case Count] The New York Times.
- "As states start to reopen, here's where people are going". The Washington Post. May 29, 2020.
- "How the Virus Won". The New York Times. June 24, 2020.
- v:COVID-19/All-cause deaths/United States
- ^
- Washington Post Live (April 25, 2023). "Transcript: Global Health: Lessons from the Pandemic with Philip Zelikow and Charity Dean". The Washington Post. Retrieved April 26, 2023.
Dan Diamond; Charity Dean; Philip Zelikow;
- Washington Post Live (April 25, 2023). "Audio: Lessons learned from U.S. COVID-19 response". The Washington Post. Retrieved April 26, 2023.
Dan Diamond; Charity Dean; Philip Zelikow;
- Washington Post Live (April 25, 2023). "Video: Lessons learned from U.S. COVID-19 response". YouTube. Retrieved April 26, 2023.
Dan Diamond; Charity Dean; Philip Zelikow;
- Diamond D (April 25, 2023). "Review | Experts trace flawed U.S. covid response and how to fix it". The Washington Post. Retrieved April 26, 2023.
- Washington Post Live (April 25, 2023). "Transcript: Global Health: Lessons from the Pandemic with Philip Zelikow and Charity Dean". The Washington Post. Retrieved April 26, 2023.
 KSF
KSF