Medicinal plants
 From Wikipedia - Reading time: 30 min
From Wikipedia - Reading time: 30 min


Medicinal plants, also called medicinal herbs, have been discovered and used in traditional medicine practices since prehistoric times. Plants synthesize hundreds of chemical compounds for various functions, including defense and protection against insects, fungi, diseases, against parasites[2] and herbivorous mammals.[3]
The earliest historical records of herbs are found from the Sumerian civilization, where hundreds of medicinal plants including opium are listed on clay tablets, c. 3000 BC. The Ebers Papyrus from ancient Egypt, c. 1550 BC, describes over 850 plant medicines. The Greek physician Dioscorides, who worked in the Roman army, documented over 1000 recipes for medicines using over 600 medicinal plants in De materia medica, c. 60 AD; this formed the basis of pharmacopoeias for some 1500 years. Drug research sometimes makes use of ethnobotany to search for pharmacologically active substances, and this approach has yielded hundreds of useful compounds. These include the common drugs aspirin, digoxin, quinine, and opium. The compounds found in plants are diverse, with most in four biochemical classes: alkaloids, glycosides, polyphenols, and terpenes. Few of these are scientifically confirmed as medicines or used in conventional medicine.
Medicinal plants are widely used as folk medicine in non-industrialized societies, mainly because they are readily available and cheaper than modern medicines. In many countries, there is little regulation of traditional medicine, but the World Health Organization coordinates a network to encourage safe and rational use. The botanical herbal market has been criticized for being poorly regulated and containing placebo and pseudoscience products with no scientific research to support their medical claims.[4] Medicinal plants face both general threats, such as climate change and habitat destruction, and the specific threat of over-collection to meet market demand.[4]
History
[edit]
Prehistoric times
[edit]Plants, including many now used as culinary herbs and spices, have been used as medicines, not necessarily effectively, from prehistoric times. Spices have been used partly to counter food spoilage bacteria, especially in hot climates,[6][7] and especially in meat dishes that spoil more readily.[8] Angiosperms (flowering plants) were the original source of most plant medicines.[9] Human settlements are often surrounded by weeds used as herbal medicines, such as nettle, dandelion and chickweed.[10][11] Humans were not alone in using herbs: some animals, such as non-human primates, monarch butterflies and sheep ingest plants when they are ill.[12]
Samples from prehistoric burial sites indicate that Paleolithic peoples consumed plants. For instance, a 60,000-year-old Neanderthal burial site, "Shanidar IV", in northern Iraq yielded pollen from eight plant species.[13] At Taforalt cave, Morocco, 15,000-year-old remains of ephedra were found inside a tomb, indicating its possible role in funeral rites.[14] A mushroom found in the personal effects of Ötzi the Iceman, whose body was frozen in the Ötztal Alps for more than 5,000 years, may have been used against whipworm.[15]
Ancient times
[edit]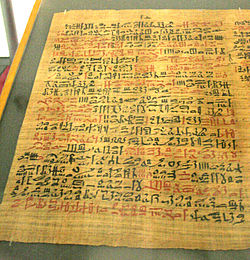
In ancient Sumeria, hundreds of medicinal plants including myrrh and opium are listed on clay tablets from around 3000 BC. The ancient Egyptian Ebers Papyrus lists over 800 plant medicines such as aloe, cannabis, castor bean, garlic, juniper, and mandrake.[16][17]
In antiquity, various cultures across Europe, including the Romans, Celts, and Nordic peoples, also practiced herbal medicine as a significant component of their healing traditions.
The Romans had a rich tradition of herbal medicine, drawing upon knowledge inherited from the Greeks and expanding upon it. Notable works include those of Pedanius Dioscorides, whose "De Materia Medica" served as a comprehensive guide to medicinal plants and remained influential for centuries.[18] Additionally, Pliny the Elder's "Naturalis Historia" contains valuable insights into Roman medical plant practices [19]
Among the Celtic peoples of ancient Europe, herbalism played a vital role in both medicine and spirituality. Druids, the religious leaders of the Celts, were reputed to possess deep knowledge of plants and their medicinal properties. Although written records are scarce, archaeological evidence, such as the discovery of medicinal plants at Celtic sites, provides insight into their herbal practices [20]
In the Nordic regions, including Scandinavia and parts of Germany, herbal medicine was also prevalent in ancient times. The Norse sagas and Eddic poetry often mention the use of herbs for healing purposes. Additionally, archaeological findings, such as the remains of medicinal plants in Viking-age graves, attest to the importance of herbal remedies in Nordic culture [21]
From ancient times to the present, Ayurvedic medicine as documented in the Atharva Veda, the Rig Veda and the Sushruta Samhita has used hundreds of herbs and spices, such as turmeric, which contains curcumin.[22] The Chinese pharmacopoeia, the Shennong Ben Cao Jing records plant medicines such as chaulmoogra for leprosy, ephedra, and hemp.[23] This was expanded in the Tang dynasty Yaoxing Lun.[24] In the fourth century BC, Aristotle's pupil Theophrastus wrote the first systematic botany text, Historia plantarum.[25] In around 60 AD, the Greek physician Pedanius Dioscorides, working for the Roman army, documented over 1000 recipes for medicines using over 600 medicinal plants in De materia medica. The book remained the authoritative reference on herbalism for over 1500 years, into the seventeenth century.[5]
Middle Ages
[edit]
During the Middle Ages, herbalism continued to flourish across Europe, with distinct traditions emerging in various regions, often influenced by cultural, religious, indigenous, and geographical factors.
In the Early Middle Ages, Benedictine monasteries preserved medical knowledge in Europe, translating and copying classical texts and maintaining herb gardens.[26][27] Hildegard of Bingen wrote Causae et Curae ("Causes and Cures") on medicine.[28]
In France, herbalism thrived alongside the practice of medieval medicine, which combined elements of Ancient Greek and Roman traditions. Catholic monastic orders played a significant role in preserving and expanding herbal knowledge. Manuscripts like the "Tractatus de Herbis" from the 15th century depict French herbal remedies and their uses.[29] Monasteries and convents served as centers of learning, where monks and nuns cultivated medicinal gardens. Likewise, in Italy, herbalism flourished with contribution Italian physicians like Matthaeus Platearius who compiled herbal manuscripts, such as the "Circa Instans," which served as practical guides for herbal remedies.[30]
In the Iberian Peninsula, the regions of the North remained independent during the period of Islamic occupation, and retained their traditional and indigenous medical practices. Galicia and Asturias, possessed a rich herbal heritage shaped by its Celtic and Roman influences. The Galician people were known for their strong connection to the land and nature and preserved botanical knowledge, with healers, known as "curandeiros" or "meigas," who relied on local plants for healing purposes [31] The Asturian landscape, characterized by lush forests and mountainous terrain, provided a rich source of medicinal herbs used in traditional healing practices, with "yerbatos," who possessed extensive knowledge of local plants and their medicinal properties [32] Barcelona, located in the Catalonia region of northeastern Spain, was a hub of cultural exchange during the Middle Ages, fostering the preservation and dissemination of medical knowledge. Catalan herbalists, known as "herbolarios," compiled manuscripts detailing the properties and uses of medicinal plants found in the region. The University of Barcelona, founded in 1450, played a pivotal role in advancing herbal medicine through its botanical gardens and academic pursuits.[33]
In Scotland and England, herbalism was deeply rooted in folk traditions and influenced by Celtic, Anglo-Saxon, and Norse practices. Herbal knowledge was passed down through generations, often by wise women known as "cunning folk." The "Physicians of Myddfai," a Welsh herbal manuscript from the 13th century, reflects the blending of Celtic and Christian beliefs in herbal medicine.[34]
In the Islamic Golden Age, scholars translated many classical Greek texts including Dioscorides into Arabic, adding their own commentaries.[35] Herbalism flourished in the Islamic world, particularly in Baghdad and in Al-Andalus. Among many works on medicinal plants, Abulcasis (936–1013) of Cordoba wrote The Book of Simples, and Ibn al-Baitar (1197–1248) recorded hundreds of medicinal herbs such as Aconitum, nux vomica, and tamarind in his Corpus of Simples.[36] Avicenna included many plants in his 1025 The Canon of Medicine.[37] Abu-Rayhan Biruni,[38] Ibn Zuhr,[39] Peter of Spain, and John of St Amand wrote further pharmacopoeias.[40]
Early Modern
[edit]
The Early Modern period saw the flourishing of illustrated herbals across Europe, starting with the 1526 Grete Herball. John Gerard wrote his famous The Herball or General History of Plants in 1597, based on Rembert Dodoens, and Nicholas Culpeper published his The English Physician Enlarged.[41] Many new plant medicines arrived in Europe as products of Early Modern exploration and the resulting Columbian Exchange, in which livestock, crops and technologies were transferred between the Old World and the Americas in the 15th and 16th centuries. Medicinal herbs arriving in the Americas included garlic, ginger, and turmeric; coffee, tobacco and coca travelled in the other direction.[42][43] In Mexico, the sixteenth century Badianus Manuscript described medicinal plants available in Central America.[44]
19th and 20th centuries
[edit]The place of plants in medicine was radically altered in the 19th century by the application of chemical analysis. Alkaloids were isolated from a succession of medicinal plants, starting with morphine from the poppy in 1806, and soon followed by ipecacuanha and strychnos in 1817, quinine from the cinchona tree, and then many others. As chemistry progressed, additional classes of potentially active substances were discovered in plants. Commercial extraction of purified alkaloids including morphine began at Merck in 1826. Synthesis of a substance first discovered in a medicinal plant began with salicylic acid in 1853. Around the end of the 19th century, the mood of pharmacy turned against medicinal plants, as enzymes often modified the active ingredients when whole plants were dried, and alkaloids and glycosides purified from plant material started to be preferred. Drug discovery from plants continued to be important through the 20th century and into the 21st, with important anti-cancer drugs from yew and Madagascar periwinkle.[45][46][47]
Context
[edit]Medicinal plants are used with the intention of maintaining health, to be administered for a specific condition, or both, whether in modern medicine or in traditional medicine.[4][48] The Food and Agriculture Organization estimated in 2002 that over 50,000 medicinal plants are used across the world.[49] The Royal Botanic Gardens, Kew more conservatively estimated in 2016 that 17,810 plant species have a medicinal use, out of some 30,000 plants for which a use of any kind is documented.[50]
In modern medicine, around a quarter[a] of the drugs prescribed to patients are derived from medicinal plants, and they are rigorously tested.[48][51] In other systems of medicine, medicinal plants may constitute the majority of what are often informal attempted treatments, not tested scientifically.[52] The World Health Organization estimates, without reliable data, that some 80 percent of the world's population depends mainly on traditional medicine (including but not limited to plants); perhaps some two billion people are largely reliant on medicinal plants.[48][51] The use of plant-based materials including herbal or natural health products with supposed health benefits, is increasing in developed countries.[53] This brings attendant risks of toxicity and other effects on human health, despite the safe image of herbal remedies.[53] Herbal medicines have been in use since long before modern medicine existed; there was and often still is little or no knowledge of the pharmacological basis of their actions, if any, or of their safety. The World Health Organization formulated a policy on traditional medicine in 1991, and since then has published guidelines for them, with a series of monographs on widely used herbal medicines.[54][55]
Medicinal plants may provide three main kinds of benefit: health benefits to the people who consume them as medicines; financial benefits to people who harvest, process, and distribute them for sale; and society-wide benefits, such as job opportunities, taxation income, and a healthier labour force.[48] However, development of plants or extracts having potential medicinal uses is blunted by weak scientific evidence, poor practices in the process of drug development, and insufficient financing.[4][56]
Trade
[edit]The markets for medicinal and aromatic plants are grouped in manufacturing categories of pharmaceuticals and dietary supplements, food and beverages, personal care products and cosmetics, with the pharmaceutical and supplement category accounting for about 60% of the total.[57] As of 2023 by one estimate, the global market was US$68 billion per year, growing by 10-20% annually.[57]
China and India are the leading producers of natural products, and are also the leading exporters and domestic consumers.[57] Major importers include the United States, the European Union, and Japan.[57]
Phytochemical basis
[edit]All plants produce chemical compounds which give them an evolutionary advantage, such as defending against herbivores or, in the example of salicylic acid, as a hormone in plant defenses.[58][59] These phytochemicals have potential for use as drugs,[60] and the content and known pharmacological activity of these substances in medicinal plants is the scientific basis for their use in modern medicine, if scientifically confirmed.[4] For instance, daffodils (Narcissus) contain nine groups of alkaloids including galantamine, licensed for use against Alzheimer's disease. The alkaloids are bitter-tasting and toxic, and concentrated in the parts of the plant such as the stem most likely to be eaten by herbivores; they may also protect against parasites.[61][62][63]
Modern knowledge of medicinal plants is being systematised in the Medicinal Plant Transcriptomics Database, which by 2011 provided a sequence reference for the transcriptome of some thirty species.[64] Major classes of plant phytochemicals are described below, with examples of plants that contain them.[9][55][65][66][67]
Alkaloids
[edit]Alkaloids are bitter-tasting chemicals, very widespread in nature, and often toxic, found in many medicinal plants.[68] There are several classes with different modes of action as drugs, both recreational and pharmaceutical. Medicines of different classes include atropine, scopolamine, and hyoscyamine (all from nightshade),[69] the traditional medicine berberine (from plants such as Berberis and Mahonia),[b] caffeine (Coffea), cocaine (Coca), ephedrine (Ephedra), morphine (opium poppy), nicotine (tobacco),[c] reserpine (Rauvolfia serpentina), quinidine and quinine (Cinchona), vincamine (Vinca minor), and vincristine (Catharanthus roseus).[67][72]
-
The alkaloid nicotine from tobacco binds directly to the body's Nicotinic acetylcholine receptors, accounting for its pharmacological effects.[73]
-
Deadly nightshade, Atropa belladonna, yields tropane alkaloids including atropine, scopolamine and hyoscyamine.[69]
Glycosides
[edit]Anthraquinone glycosides are found in medicinal plants such as rhubarb, cascara, and Alexandrian senna.[74][75] Plant-based laxatives made from such plants include senna,[76] rhubarb[77] and Aloe.[67]
The cardiac glycosides are powerful drugs from medicinal plants including foxglove and lily of the valley. They include digoxin and digitoxin which support the beating of the heart, and act as diuretics.[58]
-
Senna alexandrina, containing anthraquinone glycosides, has been used as a laxative for millennia.[76]
-
The foxglove, Digitalis purpurea, contains digoxin, a cardiac glycoside. The plant was used on heart conditions long before the glycoside was identified.[58][78]
Polyphenols
[edit]Polyphenols of several classes are widespread in plants, having diverse roles in defenses against plant diseases and predators.[58] They include hormone-mimicking phytoestrogens and astringent tannins.[67][79] Plants containing phytoestrogens have been administered for centuries for gynecological disorders, such as fertility, menstrual, and menopausal problems.[80] Among these plants are Pueraria mirifica,[81] kudzu,[82] angelica,[83] fennel, and anise.[84]
Many polyphenolic extracts, such as from grape seeds, olives or maritime pine bark, are sold as dietary supplements and cosmetics without proof or legal health claims for medicinal effects.[85] In Ayurveda, the astringent rind of the pomegranate, containing polyphenols called punicalagins, is used as a medicine, with no scientific proof of efficacy.[85][86]
-
Angelica, containing phytoestrogens, has long been used for gynaecological disorders.
Terpenes
[edit]Terpenes and terpenoids of many kinds are found in a variety of medicinal plants,[88] and in resinous plants such as the conifers. They are strongly aromatic and serve to repel herbivores. Their scent makes them useful in essential oils, whether for perfumes such as rose and lavender, or for aromatherapy.[67][89][90] Some have medicinal uses: for example, thymol is an antiseptic and was once used as a vermifuge (anti-worm medicine).[91]
-
The essential oil of common thyme (Thymus vulgaris), contains the monoterpene thymol, an antiseptic and antifungal.[91]
In practice
[edit]
Cultivation
[edit]Medicinal plants demand intensive management. Different species each require their own distinct conditions of cultivation. The World Health Organization recommends the use of rotation to minimise problems with pests and plant diseases. Cultivation may be traditional or may make use of conservation agriculture practices to maintain organic matter in the soil and to conserve water, for example with no-till farming systems.[92] In many medicinal and aromatic plants, plant characteristics vary widely with soil type and cropping strategy, so care is required to obtain satisfactory yields.[93]
Preparation
[edit]
Medicinal plants are often tough and fibrous, requiring some form of preparation to make them convenient to administer. According to the Institute for Traditional Medicine, common methods for the preparation of herbal medicines include decoction, powdering, and extraction with alcohol, in each case yielding a mixture of substances. Decoction involves crushing and then boiling the plant material in water to produce a liquid extract that can be taken orally or applied topically.[94] Powdering involves drying the plant material and then crushing it to yield a powder that can be compressed into tablets. Alcohol extraction involves soaking the plant material in cold wine or distilled spirit to form a tincture.[95]
Traditional poultices were made by boiling medicinal plants, wrapping them in a cloth, and applying the resulting parcel externally to the affected part of the body.[96]
When modern medicine has identified a drug in a medicinal plant, commercial quantities of the drug may either be synthesised or extracted from plant material, yielding a pure chemical.[45] Extraction can be practical when the compound in question is complex.[97]
Usage
[edit]
Plant medicines are in wide use around the world.[98] In most of the developing world, especially in rural areas, local traditional medicine, including herbalism, is the only source of health care for people, while in the developed world, alternative medicine including use of dietary supplements is marketed aggressively using the claims of traditional medicine. As of 2015, most products made from medicinal plants had not been tested for their safety and efficacy, and products that were marketed in developed economies and provided in the undeveloped world by traditional healers were of uneven quality, sometimes containing dangerous contaminants.[99] Traditional Chinese medicine makes use of a wide variety of plants, among other materials and techniques.[100] Researchers from Kew Gardens found 104 species used for diabetes in Central America, of which seven had been identified in at least three separate studies.[101][102] The Yanomami of the Brazilian Amazon, assisted by researchers, have described 101 plant species used for traditional medicines.[103][104]
Drugs derived from plants including opiates, cocaine and cannabis have both medical and recreational uses. Different countries have at various times made use of illegal drugs, partly on the basis of the risks involved in taking psychoactive drugs.[105]
Effectiveness
[edit]
Plant medicines have often not been tested systematically, but have come into use informally over the centuries. By 2007, clinical trials had demonstrated potentially useful activity in nearly 16% of herbal extracts; there was limited in vitro or in vivo evidence for roughly half the extracts; there was only phytochemical evidence for around 20%; 0.5% were allergenic or toxic; and some 12% had basically never been studied scientifically.[55] Cancer Research UK caution that there is no reliable evidence for the effectiveness of herbal remedies for cancer.[106]
A 2012 phylogenetic study built a family tree down to genus level using 20,000 species to compare the medicinal plants of three regions, Nepal, New Zealand and the Cape of South Africa. It discovered that the species used traditionally to treat the same types of condition belonged to the same groups of plants in all three regions, giving a "strong phylogenetic signal".[107] Since many plants that yield pharmaceutical drugs belong to just these groups, and the groups were independently used in three different world regions, the results were taken to mean 1) that these plant groups do have potential for medicinal efficacy, 2) that undefined pharmacological activity is associated with use in traditional medicine, and 3) that the use of a phylogenetic groups for possible plant medicines in one region may predict their use in the other regions.[107]
Regulation
[edit]
The World Health Organization (WHO) has been coordinating a network called the International Regulatory Cooperation for Herbal Medicines to try to improve the quality of medical products made from medicinal plants and the claims made for them.[108] In 2015, only around 20% of countries had well-functioning regulatory agencies, while 30% had none, and around half had limited regulatory capacity.[99] In India, where Ayurveda has been practised for centuries, herbal remedies are the responsibility of a government department, AYUSH, under the Ministry of Health & Family Welfare.[109]
WHO has set out a strategy for traditional medicines[110] with four objectives: to integrate them as policy into national healthcare systems; to provide knowledge and guidance on their safety, efficacy, and quality; to increase their availability and affordability; and to promote their rational, therapeutically sound usage.[110] WHO notes in the strategy that countries are experiencing seven challenges to such implementation, namely in developing and enforcing policy; in integration; in safety and quality, especially in assessment of products and qualification of practitioners; in controlling advertising; in research and development; in education and training; and in the sharing of information.[110]
Drug discovery
[edit]
The pharmaceutical industry has roots in the apothecary shops of Europe in the 1800s, where pharmacists provided local traditional medicines to customers, which included extracts like morphine, quinine, and strychnine.[111] Therapeutically important drugs like camptothecin (from Camptotheca acuminata, used in traditional Chinese medicine) and taxol (from the Pacific yew, Taxus brevifolia) were derived from medicinal plants.[112][45] The Vinca alkaloids vincristine and vinblastine, used as anti-cancer drugs, were discovered in the 1950s from the Madagascar periwinkle, Catharanthus roseus.[113]
Hundreds of compounds have been identified using ethnobotany, investigating plants used by indigenous peoples for possible medical applications.[114] Some important phytochemicals, including curcumin, epigallocatechin gallate, genistein and resveratrol are pan-assay interference compounds, meaning that in vitro studies of their activity often provide unreliable data. As a result, phytochemicals have frequently proven unsuitable as the lead substances in drug discovery.[115][116] In the United States over the period 1999 to 2012, despite several hundred applications for new drug status, only two botanical drug candidates had sufficient evidence of medicinal value to be approved by the Food and Drug Administration.[4]
The pharmaceutical industry has remained interested in mining traditional uses of medicinal plants in its drug discovery efforts.[45] Of the 1073 small-molecule drugs approved in the period 1981 to 2010, over half were either directly derived from or inspired by natural substances.[45][117] Among cancer treatments, of 185 small-molecule drugs approved in the period from 1981 to 2019, 65% were derived from or inspired by natural substances.[118]
Safety
[edit]
Plant medicines can cause adverse effects and even death, whether by side-effects of their active substances, by adulteration or contamination, by overdose, or by inappropriate prescription. Many such effects are known, while others remain to be explored scientifically. There is no reason to presume that because a product comes from nature it must be safe: the existence of powerful natural poisons like atropine and nicotine shows this to be untrue. Further, the high standards applied to conventional medicines do not always apply to plant medicines, and dose can vary widely depending on the growth conditions of plants: older plants may be much more toxic than young ones, for instance.[120][121][122][123][124][125]
Plant extracts may interact with conventional drugs, both because they may provide an increased dose of similar compounds, and because some phytochemicals interfere with the body's systems that metabolise drugs in the liver including the cytochrome P450 system, making the drugs last longer in the body and have a cumulative effect.[126] Plant medicines can be dangerous during pregnancy.[127] Since plants may contain many different substances, plant extracts may have complex effects on the human body.[6]
Quality, advertising, and labelling
[edit]Herbal medicine and dietary supplement products have been criticized as not having sufficient standards or scientific evidence to confirm their contents, safety, and presumed efficacy.[128][129][130][131] Companies often make false claims about their herbal products promising health benefits that aren't backed by evidence to generate more sales. The market for dietary supplements and nutraceuticals grew by 5% during the COVID-19 pandemic, which led to the United States taking action to stop the deceptive marketing of herbal products to combat the virus.[132][133]
Threats
[edit]Where medicinal plants are harvested from the wild rather than cultivated, they are subject to both general and specific threats. General threats include climate change and habitat loss to development and agriculture. A specific threat is over-collection to meet rising demand for medicines.[134] A case in point was the pressure on wild populations of the Pacific yew soon after news of taxol's effectiveness became public.[45] The threat from over-collection could be addressed by cultivation of some medicinal plants, or by a system of certification to make wild harvesting sustainable.[134] A report in 2020 by the Royal Botanic Gardens, Kew identifies 723 medicinal plants as being at risk of extinction, caused partly by over-collection.[135][118]
See also
[edit]- Australian Phytochemical Survey
- Ethnomedicine
- European Directive on Traditional Herbal Medicinal Products
- Plant Resources of Tropical Africa
Notes
[edit]- ^ Farnsworth states that this figure was based on prescriptions from American community pharmacies between 1959 and 1980.[51]
- ^ Berberine is the main active component of an ancient Chinese herb Coptis chinensis French, which has been administered for what Yin and colleagues state is "diabetes" for thousands of years, although with no sound evidence of efficacy.[70]
- ^ Tobacco has "probably been responsible for more deaths than any other herb", but it was used as a medicine in the societies encountered by Columbus and was considered a panacea in Europe. It is no longer accepted as medicinal.[71]
References
[edit]- ^ Lichterman BL (2004). "Aspirin: The Story of a Wonder Drug". British Medical Journal. 329 (7479): 1408. doi:10.1136/bmj.329.7479.1408. PMC 535471.
- ^ François G, Steenackers T, Assi LA, et al. (1999). "Vismione H and structurally related anthranoid compounds of natural and synthetic origin as promising drugs against the human malaria parasite Plasmodium falciparum: structure-activity relationships". Parasitology Research. 85 (7): 582–588 https://doi.org/10.1007/s004360050598. doi:10.1007/s004360050598.
- ^ Gershenzon J, Ullah C (January 2022). "Plants protect themselves from herbivores by optimizing the distribution of chemical defenses". Proc Natl Acad Sci USA. 119 (4). Bibcode:2022PNAS..11920277G. doi:10.1073/pnas.2120277119. PMC 8794845. PMID 35084361.
- ^ a b c d e f Ahn K (2017). "The worldwide trend of using botanical drugs and strategies for developing global drugs". BMB Reports. 50 (3): 111–116. doi:10.5483/BMBRep.2017.50.3.221. PMC 5422022. PMID 27998396.
- ^ a b Collins M (2000). Medieval Herbals: The Illustrative Traditions. University of Toronto Press. p. 32. ISBN 978-0-8020-8313-5.
- ^ a b Tapsell, L. C., Hemphill, I., Cobiac, L., et al. (August 2006). "Health benefits of herbs and spices: the past, the present, the future". Med. J. Aust. 185 (4 Suppl): S4–24. doi:10.5694/j.1326-5377.2006.tb00548.x. hdl:2440/22802. PMID 17022438. S2CID 9769230. Archived from the original on 31 October 2020. Retrieved 27 August 2020.
- ^ Billing J, Sherman PW (March 1998). "Antimicrobial functions of spices: why some like it hot". Quarterly Review of Biology. 73 (1): 3–49. doi:10.1086/420058. PMID 9586227. S2CID 22420170.
- ^ Sherman PW, Hash GA (May 2001). "Why vegetable recipes are not very spicy". Evolution and Human Behavior. 22 (3): 147–163. doi:10.1016/S1090-5138(00)00068-4. PMID 11384883.
- ^ a b "Angiosperms: Division Magnoliophyta: General Features". Encyclopædia Britannica (volume 13, 15th edition). 1993. p. 609.
- ^ Stepp JR (June 2004). "The role of weeds as sources of pharmaceuticals". Journal of Ethnopharmacology. 92 (2–3): 163–166. doi:10.1016/j.jep.2004.03.002. PMID 15137997.
- ^ Stepp JR, Moerman DE (April 2001). "The importance of weeds in ethnopharmacology". Journal of Ethnopharmacology. 75 (1): 19–23. doi:10.1016/S0378-8741(00)00385-8. PMID 11282438.
- ^ Sumner, Judith (2000). The Natural History of Medicinal Plants. Timber Press. p. 16. ISBN 978-0-88192-483-1.
- ^ Solecki RS (November 1975). "Shanidar IV, a Neanderthal Flower Burial in Northern Iraq". Science. 190 (4217): 880–881. Bibcode:1975Sci...190..880S. doi:10.1126/science.190.4217.880. S2CID 71625677.
- ^ Morales J, Carrión Marco Y, Cooper JH, et al. (2 November 2024). "Late pleistocene exploitation of Ephedra in a funerary context in Morocco". Scientific Reports. 14 (1): 26443. doi:10.1038/s41598-024-77785-w. ISSN 2045-2322. PMC 11531600. PMID 39488593.
{{cite journal}}: CS1 maint: overridden setting (link) - ^ Capasso, L. (December 1998). "5300 years ago, the Ice Man used natural laxatives and antibiotics". Lancet. 352 (9143): 1864. doi:10.1016/S0140-6736(05)79939-6. PMID 9851424. S2CID 40027370.
- ^ a b Sumner J (2000). The Natural History of Medicinal Plants. Timber Press. p. 17. ISBN 978-0-88192-483-1.
- ^ Petrovska 2012, pp. 1–5.
- ^ Osbaldeston, Tess Anne. Dioscorides: De Materia Medica. Olms-Weidmann, 2000
- ^ Pliny the Elder. Natural History. Harvard University Press, 1938-1963
- ^ Ross, Anne. Pagan Celtic Britain: Studies in Iconography and Tradition. Constable, 1967
- ^ Wills, Tarrin. "Herbal Medicine in the Viking Age." Viking Magazine, vol. 80, no. 3, 2017, pp. 22–27.
- ^ Dwivedi G, Dwivedi S (2007). History of Medicine: Sushruta – the Clinician – Teacher par Excellence (PDF). National Informatics Centre. Archived from the original (PDF) on 10 October 2008. Retrieved 8 October 2008.
- ^ Sumner J (2000). The Natural History of Medicinal Plants. Timber Press. p. 18. ISBN 978-0-88192-483-1.
- ^ Wu JN (2005). An Illustrated Chinese Materia Medica. Oxford University Press. p. 6. ISBN 978-0-19-514017-0.
- ^ Grene M (2004). The philosophy of biology: an episodic history. Cambridge University Press. p. 11. ISBN 978-0-521-64380-1.
- ^ Arsdall AV (2002). Medieval Herbal Remedies: The Old English Herbarium and Anglo-Saxon Medicine. Psychology Press. pp. 70–71. ISBN 978-0-415-93849-5.
- ^ Mills FA (2000). "Botany". In Johnston, William M. (ed.). Encyclopedia of Monasticism: M-Z. Taylor & Francis. p. 179. ISBN 978-1-57958-090-2.
- ^ Ramos-e-Silva Marcia (1999). "Saint Hildegard Von Bingen (1098–1179) "The Light Of Her People And Of Her Time"". International Journal of Dermatology. 38 (4): 315–320. doi:10.1046/j.1365-4362.1999.00617.x. PMID 10321953. S2CID 13404562.
- ^ Givens, Jean A. "The Tractatus de Herbis: A Thirteenth-Century Herbal." The British Library, 1982.
- ^ Givens, Jean A. "The Tractatus de Herbis: A Thirteenth-Century Herbal." The British Library, 1982
- ^ Fernández, Marta. "The Herbalist in Galicia." Ethnobotany Research and Applications, vol. 8, 2010, pp. 263–277.
- ^ Díaz-Puente, José Manuel, et al. "Traditional Medicine in Asturias (Northern Spain)." Journal of Ethnopharmacology, vol. 45, no. 2, 1995, pp. 67–74.
- ^ Vallès, Joan. "Botany and Medicine in Medieval Barcelona." Dynamis, vol. 19, 1999, pp. 349–377.
- ^ Lloyd, Robert, editor. "The Physicians of Myddfai." The Welsh MSS. Society, 1861.
- ^ Castleman M (2001). The New Healing Herbs. Rodale. p. 15. ISBN 978-1-57954-304-4.; Collins M (2000). Medieval Herbals: The Illustrative Traditions. University of Toronto Press. p. 115. ISBN 978-0-8020-8313-5.; "Pharmaceutics and Alchemy". US National Library of Medicine. Archived from the original on 5 January 2017. Retrieved 26 January 2017.; Fahd T. Botany and agriculture. p. 815., in Rashed R, Morelon R (1996). Encyclopedia of the History of Arabic Science: Astronomy-Theoretical and applied, v.2 Mathematics and the physical sciences; v.3 Technology, alchemy and life sciences. Routledge. ISBN 978-0-415-02063-3.
- ^ Castleman M (2001). The New Healing Herbs. Rodale. p. 15. ISBN 978-1-57954-304-4.
- ^ Jacquart D (2008). "Islamic Pharmacology in the Middle Ages: Theories and Substances". European Review. 16 (2): 219–227 [223]. doi:10.1017/S1062798708000215.
- ^ Kujundzić, E., Masić, I. (1999). "[Al-Biruni--a universal scientist]". Med. Arh. (in Croatian). 53 (2): 117–120. PMID 10386051.
- ^ Krek M (1979). "The Enigma of the First Arabic Book Printed from Movable Type". Journal of Near Eastern Studies. 38 (3): 203–212. doi:10.1086/372742. S2CID 162374182.
- ^ Brater, D. Craig, Daly, Walter J. (2000). "Clinical pharmacology in the Middle Ages: Principles that presage the 21st century". Clinical Pharmacology & Therapeutics. 67 (5): 447–450 [448–449]. doi:10.1067/mcp.2000.106465. PMID 10824622. S2CID 45980791.
- ^ a b Singer C (1923). "Herbals". The Edinburgh Review. 237: 95–112.
- ^ Nunn N, Qian N (2010). "The Columbian Exchange: A History of Disease, Food, and Ideas". Journal of Economic Perspectives. 24 (2): 163–188. CiteSeerX 10.1.1.232.9242. doi:10.1257/jep.24.2.163. JSTOR 25703506.
- ^ Heywood VH (2012). "The role of New World biodiversity in the transformation of Mediterranean landscapes and culture" (PDF). Bocconea. 24: 69–93. Archived from the original (PDF) on 27 February 2017. Retrieved 26 February 2017.
- ^ Gimmel Millie (2008). "Reading Medicine In The Codex De La Cruz Badiano". Journal of the History of Ideas. 69 (2): 169–192. doi:10.1353/jhi.2008.0017. PMID 19127831. S2CID 46457797.
- ^ a b c d e f Atanasov AG, Waltenberger B, Pferschy-Wenzig EM, et al. (December 2015). "Discovery and resupply of pharmacologically active plant-derived natural products: A review". Biotechnology Advances. 33 (8): 1582–1614. doi:10.1016/j.biotechadv.2015.08.001. PMC 4748402. PMID 26281720.
- ^ Petrovska BB (2012). "Historical review of medicinal plants' usage". Pharmacognosy Reviews. 6 (11): 1–5. doi:10.4103/0973-7847.95849. PMC 3358962. PMID 22654398.
- ^ Price, J. R., Lamberton, J. A., Culvenor, C.C.J (1992), "The Australian Phytochemical Survey: historical aspects of the CSIRO search for new drugs in Australian plants. Historical Records of Australian Science, 9(4), 335–356", Historical Records of Australian Science, 9 (4), Australian Academy of Science: 335–356, doi:10.1071/hr9930940335, archived from the original on 21 January 2022, retrieved 2 April 2022
- ^ a b c d Smith-Hall, C., Larsen, H.O., Pouliot, M. (2012). "People, plants and health: a conceptual framework for assessing changes in medicinal plant consumption". J Ethnobiol Ethnomed. 8: 43. doi:10.1186/1746-4269-8-43. PMC 3549945. PMID 23148504.
- ^ Schippmann U, Leaman DJ, Cunningham AB (12 October 2002). "Impact of Cultivation and Gathering of Medicinal Plants on Biodiversity: Global Trends and Issues 2. Some Figures to start with ..." Biodiversity and the Ecosystem Approach in Agriculture, Forestry and Fisheries. Satellite event on the occasion of the Ninth Regular Session of the Commission on Genetic Resources for Food and Agriculture. Rome, 12–13 October 2002. Inter-Departmental Working Group on Biological Diversity for Food and Agriculture. Rome. Food and Agriculture Organization. Archived from the original on 24 July 2017. Retrieved 25 September 2017.
- ^ "State of the World's Plants Report - 2016" (PDF). Royal Botanic Gardens, Kew. 2016. Archived from the original (PDF) on 19 September 2017. Retrieved 25 September 2017.
- ^ a b c Farnsworth NR, Akerele O, Bingel AS, et al. (1985). "Medicinal plants in therapy". Bulletin of the World Health Organization. 63 (6): 965–981. PMC 2536466. PMID 3879679.
- ^ Tilburt JC, Kaptchuk TJ (August 2008). "Herbal medicine research and global health: an ethical analysis". Bulletin of the World Health Organization. 86 (8): 577–656. doi:10.2471/BLT.07.042820. PMC 2649468. PMID 18797616. Archived from the original on 24 January 2010. Retrieved 22 September 2017.
- ^ a b Ekor M (2013). "The growing use of herbal medicines: issues relating to adverse reactions and challenges in monitoring safety". Frontiers in Pharmacology. 4 (3): 202–4. doi:10.3389/fphar.2013.00177. PMC 3887317. PMID 24454289.
- ^ Singh A (2016). Regulatory and Pharmacological Basis of Ayurvedic Formulations. CRC Press. pp. 4–5. ISBN 978-1-4987-5096-7.
- ^ a b c Cravotto G, Boffa L, Genzini L, et al. (February 2010). "Phytotherapeutics: an evaluation of the potential of 1000 plants". Journal of Clinical Pharmacy and Therapeutics. 35 (1): 11–48. doi:10.1111/j.1365-2710.2009.01096.x. PMID 20175810. S2CID 29427595.
- ^ Berida T, Adekunle Y, Dada-Adegbola H, et al. (May 2024). "Plant antibacterials: The challenges and opportunities". Heliyon. 10 (10): e31145. doi:10.1016/j.heliyon.2024.e31145. PMC 11128932. PMID 38803958.
- ^ a b c d Zamani S, Fathi M, Ebadi M, et al. (2025). "Global trade of medicinal and aromatic plants. A review". Journal of Agriculture and Food Research. 21: 101910.
- ^ a b c d e "Active Plant Ingredients Used for Medicinal Purposes". United States Department of Agriculture. Archived from the original on 12 July 2018. Retrieved 18 February 2017.
Below are several examples of active plant ingredients that provide medicinal plant uses for humans.
- ^ Hayat, S., Ahmad, A. (2007). Salicylic Acid – A Plant Hormone. Springer Science and Business Media. ISBN 978-1-4020-5183-8.
- ^ Kai Lamottke, Christophe Ripoll, Robert Walczak (2011), "The roots of innovation", European Biopharmaceutical Review, vol. 15, pp. 52-56 https://www.researchgate.net/publication/260943788_The_Roots_of_Innovation
{{citation}}: CS1 maint: multiple names: authors list (link) - ^ Bastida J, Lavilla R, Viladomat FV (2006). "Chemical and Biological Aspects of Narcissus Alkaloids". In Cordell GA (ed.). The Alkaloids: Chemistry and Biology. Vol. 63. pp. 87–179. doi:10.1016/S1099-4831(06)63003-4. ISBN 978-0-12-469563-4. PMC 7118783. PMID 17133715.
- ^ "Galantamine". Drugs.com. 2017. Archived from the original on 14 October 2018. Retrieved 17 March 2018.
- ^ Birks J (2006). Birks JS (ed.). "Cholinesterase inhibitors for Alzheimer's disease". The Cochrane Database of Systematic Reviews. 2016 (1): CD005593. doi:10.1002/14651858.CD005593. PMC 9006343. PMID 16437532.
- ^ Soejarto DD (1 March 2011). "Transcriptome Characterization, Sequencing, And Assembly Of Medicinal Plants Relevant To Human Health". University of Illinois at Chicago. Archived from the original on 20 April 2017. Retrieved 26 January 2017.
- ^ Meskin, Mark S. (2002). Phytochemicals in Nutrition and Health. CRC Press. p. 123. ISBN 978-1-58716-083-7.
- ^ Springbob, Karen, Kutchan, Toni M. (2009). "Introduction to the different classes of natural products". In Lanzotti, Virginia (ed.). Plant-Derived Natural Products: Synthesis, Function, and Application. Springer. p. 3. ISBN 978-0-387-85497-7.
- ^ a b c d e f Elumalai A, Eswariah MC (2012). "Herbalism - A Review" (PDF). International Journal of Phytotherapy. 2 (2): 96–105. Archived from the original (PDF) on 17 February 2017. Retrieved 17 February 2017.
- ^ Aniszewski, Tadeusz (2007). Alkaloids – secrets of life. Amsterdam: Elsevier. p. 182. ISBN 978-0-444-52736-3.
- ^ a b "Atropa Belladonna" (PDF). The European Agency for the Evaluation of Medicinal Products. 1998. Archived (PDF) from the original on 17 April 2018. Retrieved 26 February 2017.
- ^ Yin J, Xing H, Ye J (May 2008). "Efficacy of Berberine in Patients with Type 2 Diabetes". Metabolism. 57 (5): 712–717. doi:10.1016/j.metabol.2008.01.013. PMC 2410097. PMID 18442638.
- ^ Charlton A (June 2004). "Medicinal uses of tobacco in history". Journal of the Royal Society of Medicine. 97 (6): 292–296. doi:10.1177/014107680409700614. PMC 1079499. PMID 15173337.
- ^ Gremigni P, et al. (2003). "The interaction of phosphorus and potassium with seed alkaloid concentrations, yield and mineral content in narrow-leafed lupin (Lupinus angustifolius L.)". Plant and Soil. 253 (2): 413–427. doi:10.1023/A:1024828131581. JSTOR 24121197. S2CID 25434984.
- ^ "Nicotinic acetylcholine receptors: Introduction". IUPHAR Database. International Union of Basic and Clinical Pharmacology. Archived from the original on 29 June 2017. Retrieved 26 February 2017.
- ^ Wang, Zhe, Ma, Pei, He, Chunnian, et al. (2013). "Evaluation of the content variation of anthraquinone glycosides in rhubarb by UPLC-PDA". Chemistry Central Journal. 7 (1): 43–56. doi:10.1186/1752-153X-7-170. PMC 3854541. PMID 24160332.
- ^ Chan K, Lin T (2009). Treatments used in complementary and alternative medicine. Side Effects of Drugs Annual. Vol. 31. pp. 745–756. doi:10.1016/S0378-6080(09)03148-1. ISBN 978-0-444-53294-7.
- ^ a b Hietala, P., Marvola, M., Parviainen, T., et al. (August 1987). "Laxative potency and acute toxicity of some anthraquinone derivatives, senna extracts and fractions of senna extracts". Pharmacology & Toxicology. 61 (2): 153–6. doi:10.1111/j.1600-0773.1987.tb01794.x. PMID 3671329.
- ^ Akolkar, Praful (27 December 2012). "Pharmacognosy of Rhubarb". PharmaXChange.info. Archived from the original on 26 June 2015. Retrieved 2 February 2017.
- ^ "Digitalis purpurea. Cardiac Glycoside". Texas A&M University. Archived from the original on 2 July 2018. Retrieved 26 February 2017.
The man credited with the introduction of digitalis into the practice of medicine was William Withering.
- ^ Da Silva C, et al. (2013). "The High Polyphenol Content of Grapevine Cultivar Tannat Berries Is Conferred Primarily by Genes That Are Not Shared with the Reference Genome". The Plant Cell. 25 (12): 4777–4788. doi:10.1105/tpc.113.118810. JSTOR 43190600. PMC 3903987. PMID 24319081.
- ^ Muller-Schwarze D (2006). Chemical Ecology of Vertebrates. Cambridge University Press. p. 287. ISBN 978-0-521-36377-8.
- ^ Lee, Y. S., Park J. S., Cho S. D., et al. (December 2002). "Requirement of metabolic activation for estrogenic activity of Pueraria mirifica". Journal of Veterinary Science. 3 (4): 273–277. CiteSeerX 10.1.1.617.1507. doi:10.4142/jvs.2002.3.4.273. PMID 12819377. Archived from the original on 19 April 2019. Retrieved 19 April 2019.
- ^ Delmonte, P., Rader, J. I. (2006). "Analysis of isoflavones in foods and dietary supplements". Journal of AOAC International. 89 (4): 1138–46. doi:10.1093/jaoac/89.4.1138. PMID 16915857.
- ^ Brown D, Walton NJ (1999). Chemicals from Plants: Perspectives on Plant Secondary Products. World Scientific Publishing. pp. 21, 141. ISBN 978-981-02-2773-9.
- ^ Albert-Puleo, M. (December 1980). "Fennel and anise as estrogenic agents". Journal of Ethnopharmacology. 2 (4): 337–44. doi:10.1016/S0378-8741(80)81015-4. PMID 6999244.
- ^ a b European Food Safety Authority (2010). "Scientific Opinion on the substantiation of health claims related to various food(s)/food constituent(s) and protection of cells from premature aging, antioxidant activity, antioxidant content and antioxidant properties, and protection of DNA, proteins and lipids from oxidative damage pursuant to Article 13(1) of Regulation (EC) No 1924/20061". EFSA Journal. 8 (2): 1489. doi:10.2903/j.efsa.2010.1489.
- ^ Jindal, K. K., Sharma, R. C. (2004). Recent trends in horticulture in the Himalayas. Indus Publishing. ISBN 978-81-7387-162-7.
- ^ Turner, J. V., Agatonovic-Kustrin, S., Glass, B. D. (August 2007). "Molecular aspects of phytoestrogen selective binding at estrogen receptors". Journal of Pharmaceutical Sciences. 96 (8): 1879–85. doi:10.1002/jps.20987. PMID 17518366.
- ^ Wiart C (2014). "Terpenes". Lead Compounds from Medicinal Plants for the Treatment of Neurodegenerative Diseases. Elsevier Inc. pp. 189–284. doi:10.1016/C2011-0-09611-4. ISBN 978-0-12-398373-2.
- ^ Tchen TT (1965). "The Biosynthesis of Steroids, Terpenes and Acetogenins". American Scientist. 53 (4): 499A – 500A. JSTOR 27836252.
- ^ Singsaas EL (2000). "Terpenes and the Thermotolerance of Photosynthesis". New Phytologist. 146 (1): 1–2. doi:10.1046/j.1469-8137.2000.00626.x. JSTOR 2588737.
- ^ a b c "Thymol (CID=6989)". NIH. Archived from the original on 12 July 2018. Retrieved 26 February 2017.
THYMOL is a phenol obtained from thyme oil or other volatile oils used as a stabilizer in pharmaceutical preparations, and as an antiseptic (antibacterial or antifungal) agent. It was formerly used as a vermifuge.
- ^ "WHO Guidelines on Good Agricultural and Collection Practices (GACP) for Medicinal Plants". World Health Organization. 2003. Archived from the original on 20 October 2009. Retrieved 26 February 2017.
- ^ Carrubba, A., Scalenghe, R. (2012). "Scent of Mare Nostrum ― Medicinal and Aromatic Plants (MAPs) in Mediterranean soils". Journal of the Science of Food and Agriculture. 92 (6): 1150–1170. doi:10.1002/jsfa.5630. PMID 22419102.
- ^ Yang Y (2010). "Theories and concepts in the composition of Chinese herbal formulas". Chinese Herbal Formulas. Elsevier Ltd.: 1–34. doi:10.1016/B978-0-7020-3132-8.00006-2. ISBN 9780702031328. Retrieved 18 April 2020.
- ^ Dharmananda S (May 1997). "The Methods of Preparation of Herb Formulas: Decoctions, Dried Decoctions, Powders, Pills, Tablets, and Tinctures". Institute of Traditional Medicine, Portland, Oregon. Archived from the original on 4 October 2017. Retrieved 27 September 2017.
- ^ Mount T (20 April 2015). "9 weird medieval medicines". British Broadcasting Corporation. Archived from the original on 28 September 2017. Retrieved 27 September 2017.
- ^ Pezzuto JM (January 1997). "Plant-derived anticancer agents". Biochemical Pharmacology. 53 (2): 121–133. doi:10.1016/S0006-2952(96)00654-5. PMID 9037244.
- ^ "Traditional Medicine. Fact Sheet No. 134". World Health Organization. May 2003. Archived from the original on 27 July 2008. Retrieved 26 February 2017.
- ^ a b Chan M (19 August 2015). "WHO Director-General addresses traditional medicine forum". WHO. Archived from the original on 22 August 2015.
- ^ "Traditional Chinese Medicine: In Depth (D428)". NIH. April 2009. Archived from the original on 4 April 2017. Retrieved 26 February 2017.
- ^ Giovannini P. "Managing diabetes with medicinal plants". Kew Gardens. Archived from the original on 3 October 2017. Retrieved 3 October 2017.
- ^ Giovannini P, Howes MJ, Edwards SE (2016). "Medicinal plants used in the traditional management of diabetes and its sequelae in Central America: A review". Journal of Ethnopharmacology. 184: 58–71. doi:10.1016/j.jep.2016.02.034. PMID 26924564. S2CID 22639191. Archived from the original on 7 June 2022. Retrieved 27 August 2020.
- ^ Milliken W (2015). "Medicinal knowledge in the Amazon". Kew Gardens. Archived from the original on 3 October 2017. Retrieved 3 October 2017.
- ^ Yanomami, M. I., Yanomami, E., Albert, B., et al. (2014). Hwërɨ mamotima thëpë ã oni. Manual dos remedios tradicionais Yanomami [Manual of Traditional Yanomami Medicines]. São Paulo: Hutukara/Instituto Socioambiental.
- ^ "Scoring drugs. A new study suggests alcohol is more harmful than heroin or crack". The Economist. 2 November 2010. Archived from the original on 28 January 2018. Retrieved 26 February 2017.
"Drug harms in the UK: a multi-criteria decision analysis", by David Nutt, Leslie King and Lawrence Phillips, on behalf of the Independent Scientific Committee on Drugs. The Lancet.
- ^ "Herbal medicine". Cancer Research UK. Archived from the original on 29 May 2019. Retrieved 7 July 2019.
There is no reliable evidence from human studies that herbal remedies can treat, prevent or cure any type of cancer. Some clinical trials seem to show that certain Chinese herbs may help people to live longer, might reduce side effects, and help to prevent cancer from coming back. This is especially when combined with conventional treatment.
- ^ a b Saslis-Lagoudakis CH, Savolainen V, Williamson EM, et al. (2012). "Phylogenies reveal predictive power of traditional medicine in bioprospecting". Proceedings of the National Academy of Sciences. 109 (39): 15835–40. Bibcode:2012PNAS..10915835S. doi:10.1073/pnas.1202242109. PMC 3465383. PMID 22984175.
- ^ "International Regulatory Cooperation for Herbal Medicines (IRCH)". World Health Organization. Archived from the original on 1 September 2013. Retrieved 2 October 2017.
- ^ Kala CP, Sajwan BS (2007). "Revitalizing Indian systems of herbal medicine by the National Medicinal Plants Board through institutional networking and capacity building". Current Science. 93 (6): 797–806. JSTOR 24099124.
- ^ a b c World Health Organization (2013). WHO Traditional Medicine Strategy 2014-2023 (PDF). World Health Organization. ISBN 978-92-4-150609-0. Archived (PDF) from the original on 18 November 2017. Retrieved 3 October 2017.
- ^ "Emergence of Pharmaceutical Science and Industry: 1870-1930". Chemical & Engineering News. Vol. 83, no. 25. 20 June 2005. Archived from the original on 10 November 2018. Retrieved 2 October 2017.
- ^ Heinrich M, Bremner P (March 2006). "Ethnobotany and ethnopharmacy--their role for anti-cancer drug development". Current Drug Targets. 7 (3): 239–245. doi:10.2174/138945006776054988. PMID 16515525.
- ^ Moudi M, Go R, Yien CY, et al. (November 2013). "Vinca Alkaloids". International Journal of Preventive Medicine. 4 (11): 1231–1235. PMC 3883245. PMID 24404355.
- ^ Fabricant, D. S., Farnsworth, N. R. (March 2001). "The value of plants used in traditional medicine for drug discovery". Environ. Health Perspect. 109 (Suppl 1): 69–75. doi:10.1289/ehp.01109s169. PMC 1240543. PMID 11250806.
- ^ Baell J, Walters MA (24 September 2014). "Chemistry: Chemical con artists foil drug discovery". Nature. 513 (7519): 481–483. Bibcode:2014Natur.513..481B. doi:10.1038/513481a. PMID 25254460.
- ^ Dahlin JL, Walters MA (July 2014). "The essential roles of chemistry in high-throughput screening triage". Future Medicinal Chemistry. 6 (11): 1265–90. doi:10.4155/fmc.14.60. PMC 4465542. PMID 25163000.
- ^ Newman DJ, Cragg GM (8 February 2012). "Natural Products As Sources of New Drugs over the 30 Years from 1981 to 2010". Journal of Natural Products. 75 (3): 311–35. doi:10.1021/np200906s. PMC 3721181. PMID 22316239.
- ^ a b "State of the World's Plants and Fungi 2020" (PDF). Royal Botanic Gardens, Kew. 2020. Archived (PDF) from the original on 5 October 2020. Retrieved 30 September 2020.
- ^ Freye E (2010). "Toxicity of Datura Stramonium". Pharmacology and Abuse of Cocaine, Amphetamines, Ecstasy and Related Designer Drugs. Springer. pp. 217–218. doi:10.1007/978-90-481-2448-0_34. ISBN 978-90-481-2447-3.
- ^ Ernst E (1998). "Harmless Herbs? A Review of the Recent Literature" (PDF). The American Journal of Medicine. 104 (2): 170–178. doi:10.1016/S0002-9343(97)00397-5. PMID 9528737. Archived from the original (PDF) on 5 November 2019. Retrieved 28 November 2013.
- ^ Talalay P (2001). "The importance of using scientific principles in the development of medicinal agents from plants". Academic Medicine. 76 (3): 238–47. doi:10.1097/00001888-200103000-00010. PMID 11242573.
- ^ Elvin-Lewis M (2001). "Should we be concerned about herbal remedies". Journal of Ethnopharmacology. 75 (2–3): 141–164. doi:10.1016/S0378-8741(00)00394-9. PMID 11297844.
- ^ Vickers, A. J. (2007). "Which botanicals or other unconventional anticancer agents should we take to clinical trial?". J Soc Integr Oncol. 5 (3): 125–9. PMC 2590766. PMID 17761132.
- ^ Ernst, E. (2007). "Herbal medicines: balancing benefits and risks". Dietary Supplements and Health. Novartis Foundation Symposia. Vol. 282. Novartis Foundation Symposium. pp. 154–67, discussion 167–72, 212–8. doi:10.1002/9780470319444.ch11. ISBN 978-0-470-31944-4. PMID 17913230.
- ^ Pinn G (November 2001). "Adverse effects associated with herbal medicine". Aust Fam Physician. 30 (11): 1070–5. PMID 11759460.
- ^ Nekvindová J, Anzenbacher P (July 2007). "Interactions of food and dietary supplements with drug metabolising cytochrome P450 enzymes". Ceska Slov Farm. 56 (4): 165–73. PMID 17969314.
- ^ Born D, Barron ML (May 2005). "Herb use in pregnancy: what nurses should know". MCN Am J Matern Child Nurs. 30 (3): 201–6. doi:10.1097/00005721-200505000-00009. PMID 15867682. S2CID 35882289.
- ^ Barrett, Stephen (23 November 2013). "The herbal minefield". Quackwatch. Archived from the original on 18 August 2018. Retrieved 17 November 2017.
- ^ Zhang J, Wider B, Shang H, et al. (2012). "Quality of herbal medicines: Challenges and solutions". Complementary Therapies in Medicine. 20 (1–2): 100–106. doi:10.1016/j.ctim.2011.09.004. PMID 22305255.
- ^ Morris CA, Avorn J (2003). "Internet marketing of herbal products". JAMA. 290 (11): 1505–9. doi:10.1001/jama.290.11.1505. PMID 13129992.
- ^ Coghlan ML, Haile J, Houston J, et al. (2012). "Deep Sequencing of Plant and Animal DNA Contained within Traditional Chinese Medicines Reveals Legality Issues and Health Safety Concerns". PLOS Genetics. 8 (4): e1002657. doi:10.1371/journal.pgen.1002657. PMC 3325194. PMID 22511890.
- ^ Lordan R (2021). "Dietary supplements and nutraceuticals market growth during the coronavirus pandemic - implications for consumers and regulatory oversight". Pharmanutrition. 18. Elsevier Public Health Emergency Collection: 100282. doi:10.1016/j.phanu.2021.100282. PMC 8416287. PMID 34513589.
- ^ "United States Files Enforcement Action to Stop Deceptive Marketing of Herbal Tea Product Advertised as Covid-19 Treatment". United States Department of Justice. Department of Justice. 3 March 2022. Archived from the original on 3 October 2022. Retrieved 3 October 2022.
- ^ a b Kling J (2016). "Protecting medicine's wild pharmacy". Nature Plants. 2 (5): 16064. doi:10.1038/nplants.2016.64. PMID 27243657. S2CID 7246069.
- ^ Briggs H (30 September 2020). "Two-fifths of plants at risk of extinction, says report". BBC. Archived from the original on 29 September 2020. Retrieved 30 September 2020.
 KSF
KSF![The opium poppy Papaver somniferum is the source of the alkaloids morphine and codeine.[67]](https://upload.wikimedia.org/wikipedia/commons/thumb/8/87/Opium_poppy.jpg/250px-Opium_poppy.jpg)
![The alkaloid nicotine from tobacco binds directly to the body's Nicotinic acetylcholine receptors, accounting for its pharmacological effects.[73]](https://upload.wikimedia.org/wikipedia/commons/thumb/7/70/Nicotine.svg/250px-Nicotine.svg.png)
![Deadly nightshade, Atropa belladonna, yields tropane alkaloids including atropine, scopolamine and hyoscyamine.[69]](https://upload.wikimedia.org/wikipedia/commons/thumb/b/b7/Atropa_belladonna_-_K%C3%B6hler%E2%80%93s_Medizinal-Pflanzen-018.jpg/120px-Atropa_belladonna_-_K%C3%B6hler%E2%80%93s_Medizinal-Pflanzen-018.jpg)
![Senna alexandrina, containing anthraquinone glycosides, has been used as a laxative for millennia.[76]](https://upload.wikimedia.org/wikipedia/commons/thumb/6/61/Senna_alexandrina_Mill.-Cassia_angustifolia_L._%28Senna_Plant%29.jpg/250px-Senna_alexandrina_Mill.-Cassia_angustifolia_L._%28Senna_Plant%29.jpg)
![The foxglove, Digitalis purpurea, contains digoxin, a cardiac glycoside. The plant was used on heart conditions long before the glycoside was identified.[58][78]](https://upload.wikimedia.org/wikipedia/commons/thumb/7/74/Digitalis_purpurea2.jpg/120px-Digitalis_purpurea2.jpg)
![Digoxin is used to treat atrial fibrillation, atrial flutter and sometimes heart failure.[58]](https://upload.wikimedia.org/wikipedia/commons/thumb/4/4d/Digoxin.svg/250px-Digoxin.svg.png)

![Polyphenols include phytoestrogens (top and middle), mimics of animal estrogen (bottom).[87]](https://upload.wikimedia.org/wikipedia/commons/thumb/1/11/Phytoestrogens2.png/250px-Phytoestrogens2.png)
![The essential oil of common thyme (Thymus vulgaris), contains the monoterpene thymol, an antiseptic and antifungal.[91]](https://upload.wikimedia.org/wikipedia/commons/thumb/f/fe/Thymian.jpg/250px-Thymian.jpg)
![Thymol is one of many terpenes found in plants.[91]](https://upload.wikimedia.org/wikipedia/commons/thumb/5/5d/Thymol2.svg/120px-Thymol2.svg.png)