Neurotransmitter prodrug
 From Wikipedia - Reading time: 12 min
From Wikipedia - Reading time: 12 min
A neurotransmitter prodrug, or neurotransmitter precursor, is a drug that acts as a prodrug of a neurotransmitter. A variety of neurotransmitter prodrugs have been developed and used in medicine.[1][2] They can be useful when the neurotransmitter itself is not suitable for use as a pharmaceutical drug owing to unfavorable pharmacokinetic or physicochemical properties, for instance high susceptibility to metabolism, short elimination half-life, or lack of blood–brain barrier permeability.[1][2][3] Besides their use in medicine, neurotransmitter prodrugs have also been used as recreational drugs in some cases.[4][5]
Monoamine prodrugs
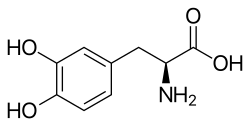
[edit]Monoamine neurotransmitter prodrugs include the catecholamine precursors and prodrugs L-phenylalanine, L-tyrosine, L-DOPA (levodopa), L-DOPS (droxidopa), dipivefrine (O,O'-dipivalylepinephrine), and dibutepinephrine,[1][3] as well as the serotonin and melatonin precursors and prodrugs L-tryptophan and L-5-hydroxytryptophan (5-HTP; oxitriptan).[6][7][8] Other dopamine prodrugs, including etilevodopa, foslevodopa, melevodopa, XP-21279, DopAmide, DA-Phen, O,O'-diacetyldopamine, O,O'-dipivaloyldopamine, docarpamine, gludopa, and gludopamine, have also been developed.[9][10][11][12][13] Dopamantine (N-adamantanoyl dopamine) is another possible attempt at a dopamine prodrug.[14][15] Other serotonin prodrugs have been developed as well, such as the renally-selective L-glutamyl-5-hydroxy-L-tryptophan (glu-5-HTP).[16][17][18]
5-HTP is additionally a prodrug of N-methylated tryptamine psychedelic trace amines, such as N-methylserotonin (NMS; norbufotenin) and bufotenin (5-hydroxy-N,N-dimethyltryptamine; 5-HO-DMT).[19][20][21][22][23] The same is also true of L-tryptophan, which is transformed into tryptamine as well as into N-methyltryptamine (NMT) and N,N-dimethyltryptamine (N,N-DMT).[20][24][25][26][27] Dependent on these transformations, both tryptophan and 5-HTP produce the head-twitch response (HTR), a behavioral proxy of psychedelic effects, at sufficiently high doses in animals.[20][28][29][21][30][19] O-Acetylbufotenine and O-pivalylbufotenine are thought to be centrally active prodrugs of the peripherally selective bufotenin.[31][32][33]
Although they are not endogenous neurotransmitter prodrugs, "false" or "substitute" neurotransmitter prodrugs, such as α-methyltryptophan and α-methyl-5-hydroxytryptophan (which are prodrugs of α-methylserotonin, a substitute neurotransmitter of serotonin), have also been developed.[34] Analogously, ibopamine and fosopamine are prodrugs of epinine (N-methyldopamine; deoxyepinephrine).[35]
GABA prodrugs
[edit]γ-Aminobutyric acid (GABA) prodrugs include progabide and tolgabide.[2][36] Picamilon has been claimed to be a prodrug of GABA, but has not actually been demonstrated to be converted into GABA.[37][38] Pivagabine was once thought to be a prodrug of GABA, but this proved not to be the case.[39]
4-Amino-1-butanol is known to be converted into GABA through the actions of aldehyde reductase (ALR) and aldehyde dehydrogenase (ALDH).[40] 4-Amino-1-butanol is to GABA as 1,4-butanediol (4-hydroxy-1-butanol; 1,4-BD) is to γ-hydroxybutyric acid (GHB) (with 1,4-BD being a well-known prodrug of GHB).[40][41] The metabolic intermediate γ-aminobutyraldehyde (GABAL) is also converted into GABA.[42][43]
GHB prodrugs
[edit]A number of γ-hydroxybutyric acid (GHB) prodrugs are known.[4] These include 1,4-butanediol (1,4-BD) and γ-butyrolactone (GBL), as well as the metabolic intermediate γ-hydroxybutyraldehyde (GHBAL).[4][5][41][44]
Acetylcholine prodrugs
[edit]Acetylcholine precursors and prodrugs like choline, phosphatidylcholine (lecithin), citicoline (CDP-choline), and choline alphoscerate (α-GPC) are known and have been researched.[45]
References
[edit]- ^ a b c Vytla D, Combs-Bachmann RE, Hussey AM, McCarron ST, McCarthy DS, Chambers JJ (May 2012). "Prodrug approaches to reduce hyperexcitation in the CNS". Adv Drug Deliv Rev. 64 (7): 666–685. doi:10.1016/j.addr.2011.11.007. PMID 22138074.
- ^ a b c Jana S, Mandlekar S, Marathe P (2010). "Prodrug design to improve pharmacokinetic and drug delivery properties: challenges to the discovery scientists". Curr Med Chem. 17 (32): 3874–3908. doi:10.2174/092986710793205426. PMID 20858214.
- ^ a b Huttunen KM, Raunio H, Rautio J (September 2011). "Prodrugs--from serendipity to rational design". Pharmacol Rev. 63 (3): 750–771. doi:10.1124/pr.110.003459. PMID 21737530.
- ^ a b c Ponce, Julio de Carvalho (2024). "The use of prodrugs as drugs of abuse". WIREs Forensic Science. 6 (3). doi:10.1002/wfs2.1514. ISSN 2573-9468.
- ^ a b Trombley TA, Capstick RA, Lindsley CW (December 2020). "DARK Classics in Chemical Neuroscience: Gamma-Hydroxybutyrate (GHB)". ACS Chem Neurosci. 11 (23): 3850–3859. doi:10.1021/acschemneuro.9b00336. PMID 31287661.
- ^ Maffei ME (December 2020). "5-Hydroxytryptophan (5-HTP): Natural Occurrence, Analysis, Biosynthesis, Biotechnology, Physiology and Toxicology". Int J Mol Sci. 22 (1): 181. doi:10.3390/ijms22010181. PMC 7796270. PMID 33375373.
- ^ Dörwald, F.Z. (2012). Lead Optimization for Medicinal Chemists: Pharmacokinetic Properties of Functional Groups and Organic Compounds. Wiley. p. 159. ISBN 978-3-527-33226-7. Retrieved 9 September 2024.
- ^ Turner EH, Loftis JM, Blackwell AD (March 2006). "Serotonin a la carte: supplementation with the serotonin precursor 5-hydroxytryptophan". Pharmacol Ther. 109 (3): 325–338. doi:10.1016/j.pharmthera.2005.06.004. PMID 16023217.
- ^ Gupta HV, Lyons KE, Pahwa R (September 2019). "Old Drugs, New Delivery Systems in Parkinson's Disease". Drugs Aging. 36 (9): 807–821. doi:10.1007/s40266-019-00682-9. PMID 31161581.
- ^ Lees A, Tolosa E, Stocchi F, Ferreira JJ, Rascol O, Antonini A, Poewe W (January 2023). "Optimizing levodopa therapy, when and how? Perspectives on the importance of delivery and the potential for an early combination approach". Expert Rev Neurother. 23 (1): 15–24. doi:10.1080/14737175.2023.2176220. hdl:10451/56313. PMID 36729395.
- ^ Cacciatore I, Ciulla M, Marinelli L, Eusepi P, Di Stefano A (April 2018). "Advances in prodrug design for Parkinson's disease". Expert Opin Drug Discov. 13 (4): 295–305. doi:10.1080/17460441.2018.1429400. PMID 29361853.
- ^ Haddad F, Sawalha M, Khawaja Y, Najjar A, Karaman R (December 2017). "Dopamine and Levodopa Prodrugs for the Treatment of Parkinson's Disease". Molecules. 23 (1): 40. doi:10.3390/molecules23010040. PMC 5943940. PMID 29295587.
- ^ Dhaneshwar SS, Sharma M, Patel V, Desai U, Bhojak J (2011). "Prodrug strategies for antihypertensives". Curr Top Med Chem. 11 (18): 2299–317. doi:10.2174/156802611797183285. PMID 21671866.
- ^ Lamoureux G, Artavia G (2010). "Use of the adamantane structure in medicinal chemistry". Current Medicinal Chemistry. 17 (26): 2967–2978. doi:10.2174/092986710792065027. PMID 20858176.
Dopamantine 4, the anti-Parkinson drug which has passed clinical trials, is also based on the ability of adamantane to change the distribution of a drug [10]. The conjugation of an adamantyl group as a "lipophilic carrier" allows poorly absorbed drugs to penetrate the BBB more readily and increase the concentration in the brain tissue.
- ^ Vernier VG, du Pont EI (1974). "Chapter 3. Antiparkinsonism Drugs". Annual Reports in Medicinal Chemistry. Vol. 9. Elsevier. pp. 19–26. doi:10.1016/s0065-7743(08)61424-4. ISBN 978-0-12-040509-1.
Carmantadine (VII, Sch 15427) is structurally related to amantadine33. It shares some of its pharmacological actions, was effective in a head-turning test34, and is in early clinical trials. Dopamantine (VIII) combined elements of both amantadine and dopamine in its structure, shares some pharmacological effects of amantadine and is in early clinical trials35.
- ^ Thorré, Katrien; Sarre, S.; Twahirwa, E.; Meeusen, R.; Ebinger, G.; Haemers, A.; Michotte, Y. (1996). "Effect of l-tryptophan, l-5-hydroxytryptophan and l-tryptophan prodrugs on the extracellular levels of 5-HT and 5-HIAA in the hippocampus of the rat using microdialysis". European Journal of Pharmaceutical Sciences. 4 (4): 247–256. doi:10.1016/0928-0987(95)00056-9.
- ^ Li Kam Wa TC, Freestone S, Samson RR, Johnston NR, Lee MR (July 1993). "A comparison of the effects of two putative 5-hydroxytryptamine renal prodrugs in normal man". Br J Clin Pharmacol. 36 (1): 19–23. doi:10.1111/j.1365-2125.1993.tb05886.x. PMC 1364549. PMID 7690583.
- ^ Li Kam Wa TC, Freestone S, Samson RR, Johnston NR, Lee MR (September 1994). "The antinatriuretic action of gamma-L-glutamyl-5-hydroxy-L-tryptophan is dependent on its decarboxylation to 5-hydroxytryptamine in normal man". Br J Clin Pharmacol. 38 (3): 265–269. doi:10.1111/j.1365-2125.1994.tb04351.x. PMC 1364799. PMID 7826829.
- ^ a b Kozlenkov, Alexey; González-Maeso, Javier (2013). "Animal Models and Hallucinogenic Drugs". The Neuroscience of Hallucinations. New York, NY: Springer New York. pp. 253–277. doi:10.1007/978-1-4614-4121-2_14. ISBN 978-1-4614-4120-5.
- ^ a b c Halberstadt AL, Geyer MA (2018). "Effect of Hallucinogens on Unconditioned Behavior". Behavioral Neurobiology of Psychedelic Drugs. Current Topics in Behavioral Neurosciences. Vol. 36. pp. 159–199. doi:10.1007/7854_2016_466. ISBN 978-3-662-55878-2. PMC 5787039. PMID 28224459.
- ^ a b Schmid CL, Bohn LM (October 2010). "Serotonin, but not N-methyltryptamines, activates the serotonin 2A receptor via a β-arrestin2/Src/Akt signaling complex in vivo". J Neurosci. 30 (40): 13513–24. doi:10.1523/JNEUROSCI.1665-10.2010. PMC 3001293. PMID 20926677.
- ^ Sapienza, Jacopo (13 October 2023). "The Key Role of Intracellular 5-HT2A Receptors: A Turning Point in Psychedelic Research?". Psychoactives. 2 (4): 287–293. doi:10.3390/psychoactives2040018. ISSN 2813-1851.
- ^ Vargas MV, Dunlap LE, Dong C, Carter SJ, Tombari RJ, Jami SA, Cameron LP, Patel SD, Hennessey JJ, Saeger HN, McCorvy JD, Gray JA, Tian L, Olson DE (February 2023). "Psychedelics promote neuroplasticity through the activation of intracellular 5-HT2A receptors". Science. 379 (6633): 700–706. Bibcode:2023Sci...379..700V. doi:10.1126/science.adf0435. PMC 10108900. PMID 36795823.
- ^ Carbonaro TM, Gatch MB (September 2016). "Neuropharmacology of N,N-dimethyltryptamine". Brain Res Bull. 126 (Pt 1): 74–88. doi:10.1016/j.brainresbull.2016.04.016. PMC 5048497. PMID 27126737.
Endogenous DMT is synthesized from the essential amino acid tryptophan, which is decarboxylated to tryptamine. Tryptamine is then transmethylated by the enzyme indolethylamine-N-methyltransferase (INMT) (using S-adenosyl methionine as a substrate), which catalyzes the addition of methyl groups resulting in the production of N-methyltryptamine (NMT) and DMT. NMT can also act as a substrate for INMT-dependent DMT biosynthesis (Barker et al., 1981).
- ^ Barker SA (2018). "N, N-Dimethyltryptamine (DMT), an Endogenous Hallucinogen: Past, Present, and Future Research to Determine Its Role and Function". Front Neurosci. 12: 536. doi:10.3389/fnins.2018.00536. PMC 6088236. PMID 30127713.
After the discovery of an indole-N-methyl transferase (INMT; Axelrod, 1961) in rat brain, researchers were soon examining whether the conversion of tryptophan (2, Figure 2) to tryptamine (TA; 3, Figure 2) could be converted to DMT in the brain and other tissues from several mammalian species. Numerous studies subsequently demonstrated the biosynthesis of DMT in mammalian tissue preparations in vitro and in vivo (Saavedra and Axelrod, 1972; Saavedra et al., 1973). In 1972, Juan Saavedra and Julius Axelrod reported that intracisternally administered TA was converted to N-methyltryptamine (NMT; 4, Figure 2) and DMT in the rat, the first demonstration of DMT's formation by brain tissue in vivo.
- ^ Cameron LP, Olson DE (October 2018). "Dark Classics in Chemical Neuroscience: N, N-Dimethyltryptamine (DMT)" (PDF). ACS Chem Neurosci. 9 (10): 2344–2357. doi:10.1021/acschemneuro.8b00101. PMID 30036036.
Like serotonin and melatonin, DMT is a product of tryptophan metabolism.25 Following tryptophan decarboxylation, tryptamine is methylated by an N-methyltransferase (i.e., INMT) with S-adenosylmethionine serving as the methyl donor. A second enzymatic methylation produces DMT (Figure 3A).26 [...] The enzyme indolethylamine N-methyltransferase (INMT) catalyzes the methylation of a variety of biogenic amines, and is responsible for converting tryptamine into DMT in mammals.140
- ^ Colosimo, Frankie A.; Borsellino, Philip; Krider, Reese I.; Marquez, Raul E.; Vida, Thomas A. (26 February 2024). "The Clinical Potential of Dimethyltryptamine: Breakthroughs into the Other Side of Mental Illness, Neurodegeneration, and Consciousness". Psychoactives. 3 (1). MDPI AG: 93–122. doi:10.3390/psychoactives3010007. ISSN 2813-1851.
The metabolism of DMT within the body begins with its synthesis. Endogenous DMT is made from tryptophan after decarboxylation transforms it into tryptamine [22,25]. Tryptamine then undergoes transmethylation mediated by indolethylamine-N-methyltransferase (INMT) with S-adenosyl methionine (SAM) as a substrate, morphing into N-methyltryptamine (NMT) and eventually producing N,N-DMT [26]. Intriguingly, INMT is distributed widely across the body, predominantly in the lungs, thyroid, and adrenal glands, with a dense presence in the anterior horn of the spinal cord. Within the cerebral domain, regions such as the uncus, medulla, amygdala, frontal cortex, fronto-parietal lobe, and temporal lobe exhibit INMT activity, primarily localized in the soma [26]. INMT transcripts are found in specific brain regions, including the cerebral cortex, pineal gland, and choroid plexus, in both rats and humans. Although the rat brain is capable of synthesizing and releasing DMT at concentrations similar to established monoamine neurotransmitters like serotonin [27], the possibility that DMT is an authentic neurotransmitter is still speculative. This issue has been controversial for decades [28] and requires the demonstration of an activity-dependent release (i.e., Ca2+-stimulated) of DMT at a synaptic cleft to be fully established in the human brain.
- ^ Schmid, Cullen L.; Bohn, Laura M. (2018). "βArrestins: Ligand-Directed Regulators of 5-HT2A Receptor Trafficking and Signaling Events". 5-HT2A Receptors in the Central Nervous System. Cham: Springer International Publishing. pp. 31–55. doi:10.1007/978-3-319-70474-6_2. ISBN 978-3-319-70472-2.
- ^ Jaster AM, de la Fuente Revenga M, González-Maeso J (July 2022). "Molecular targets of psychedelic-induced plasticity". J Neurochem. 162 (1): 80–88. doi:10.1111/jnc.15536. PMC 9068831. PMID 34741320.
- ^ Canal CE, Morgan D (2012). "Head-twitch response in rodents induced by the hallucinogen 2,5-dimethoxy-4-iodoamphetamine: a comprehensive history, a re-evaluation of mechanisms, and its utility as a model". Drug Test Anal. 4 (7–8): 556–576. doi:10.1002/dta.1333. PMC 3722587. PMID 22517680.
- ^ Glennon RA, Rosecrans JA (1982). "Indolealkylamine and phenalkylamine hallucinogens: a brief overview". Neurosci Biobehav Rev. 6 (4): 489–497. doi:10.1016/0149-7634(82)90030-6. PMID 6757811.
- ^ Nichols DE, Glennon RA (1984). "Medicinal Chemistry and Structure-Activity Relationships of Hallucinogens". In Jacobs BL (ed.). Hallucinogens: Neurochemical, Behavioral, and Clinical Perspectives. New York: Raven Press. pp. 95–142. ISBN 978-0-89004-990-7. OCLC 10324237.
- ^ Glennon RA, Rosecrans JA (1981). "Speculations on the mechanism of action of hallucinogenic indolealkylamines". Neurosci Biobehav Rev. 5 (2): 197–207. doi:10.1016/0149-7634(81)90002-6. PMID 7022271.
- ^ Sourkes TL (1991). "Alpha-methyltryptophan as a therapeutic agent". Prog Neuropsychopharmacol Biol Psychiatry. 15 (6): 935–938. doi:10.1016/0278-5846(91)90020-2. PMID 1763198.
- ^ Supuran, C.T.; Angeli, A.; Tanini, D. (2024). Advances in Prodrugs: Design and Therapeutic Applications. Elsevier. p. 296. ISBN 978-0-443-15634-2. Retrieved 13 November 2024.
- ^ Aboul-Enein MN, El-Azzouny AA, Saleh OA, Maklad YA (June 2012). "On chemical structures with potent antiepileptic/anticonvulsant profile". Mini Rev Med Chem. 12 (7): 671–700. doi:10.2174/138955712800626665. PMID 22512548.
- ^ Goldberg JS (August 2010). "Selected Gamma Aminobutyric Acid (GABA) Esters may Provide Analgesia for Some Central Pain Conditions". Perspect Medicin Chem. 4: 23–31. doi:10.4137/pmc.s5490. PMC 2918363. PMID 20703328.
- ^ Santillo MF, Sprando RL (April 2023). "Picamilon, a γ-aminobutyric acid (GABA) analogue and marketed nootropic, is inactive against 50 biological targets". Basic Clin Pharmacol Toxicol. 132 (4): 355–358. doi:10.1111/bcpt.13836. PMID 36668678.
- ^ Bianchi M, Quadro G, Mourier G, Galzigna L (1983). "Pharmacokinetics and in vitro effects of a 4-aminobutyric acid derivative with anticonvulsant action". Pharmacology. 27 (4): 237–240. doi:10.1159/000137876. PMID 6634934.
- ^ a b Storer, R. James; Ferrante, Antonio (10 October 1997). "Radiochemical Assay of Diamine Oxidase". Polyamine Protocols. Methods in Molecular Biology. Vol. 79. New Jersey: Humana Press. pp. 91–96. doi:10.1385/0-89603-448-8:91. ISBN 978-0-89603-448-8. PMID 9463822.
In biological mixtures γ-aminobutyraldehyde may be alternatively oxidized by aldehyde dehydrogenases (EC 1.2.1.3) to γ-aminobutyric acid (GABA) (11—13). The formation of 4-amino-1-butanol is also possible through reduction by aldehyde dehydrogenase and/or alcohol dehydrogenase (13,14), thus preventing cyclization. Other fates of putrescine in biological mixtures include the acetylation to acetylputrescine by an N-acetyltransferase and then oxidation by monoamine oxidase (EC 1.4.3.4) (11,17). [...] Fig 1 Fates of putrescine in biological mixtures
- ^ a b Felmlee MA, Morse BL, Morris ME (January 2021). "γ-Hydroxybutyric Acid: Pharmacokinetics, Pharmacodynamics, and Toxicology". AAPS J. 23 (1): 22. doi:10.1208/s12248-020-00543-z. PMC 8098080. PMID 33417072.
- ^ Rashmi, Deo; Zanan, Rahul; John, Sheeba; Khandagale, Kiran; Nadaf, Altafhusain (2018). "γ-Aminobutyric Acid (GABA): Biosynthesis, Role, Commercial Production, and Applications". Studies in Natural Products Chemistry. Vol. 57. Elsevier. pp. 413–452. doi:10.1016/b978-0-444-64057-4.00013-2. ISBN 978-0-444-64057-4.
Alternate pathways of GABA synthesis from putrescine and other polyamines have also been reported [207–211]. Here, γ-aminobutyraldehyde, an intermediate from polyamine degradation reaction via combined activities of diamine oxidase (DAO, E.C. 1.4.3.6) and 4-aminobutyraldehyde dehydrogenase (ABALDH), leads to the synthesis of GABA [205,212,213]. In response to abiotic stresses, GABA is also reported to be synthesized from proline via D1-pyrroline intermediate formation [47,205,214] and also by a nonenzymatic reaction [214]. However, GABA synthesis from polyamine pathways is minor in the brain, [215] although they play a significant role in the developing brain [216] and retina [217]. But GABA can be formed from putrescine in the mammalian brain [218].
- ^ Benedetti MS, Dostert P (1994). "Contribution of amine oxidases to the metabolism of xenobiotics". Drug Metab Rev. 26 (3): 507–535. doi:10.3109/03602539408998316. PMID 7924902.
MAO also catalyses the deamination of a natural brain constituent, monoacetyl-putrescine, producing y-acetylaminobutyraldehyde, which in turn participates in the formation of brain GABA [13].
- ^ Tay E, Lo WK, Murnion B (2022). "Current Insights on the Impact of Gamma-Hydroxybutyrate (GHB) Abuse". Subst Abuse Rehabil. 13: 13–23. doi:10.2147/SAR.S315720. PMC 8843350. PMID 35173515.
- ^ Parnetti L, Mignini F, Tomassoni D, Traini E, Amenta F (June 2007). "Cholinergic precursors in the treatment of cognitive impairment of vascular origin: ineffective approaches or need for re-evaluation?". J Neurol Sci. 257 (1–2): 264–269. doi:10.1016/j.jns.2007.01.043. PMID 17331541.
 KSF
KSF