Osteopathic medicine in the United States
 From Wikipedia - Reading time: 31 min
From Wikipedia - Reading time: 31 min
| Osteopathic medicine in the United States |
|---|
| Andrew Taylor Still (founder) |
Osteopathic medicine is a branch of the medical profession in the United States that promotes the practice of science-based medicine, often referred to in this context as allopathic medicine, with a set of philosophy and principles set by its earlier form, osteopathy. Osteopathic physicians (DOs) are graduates of American osteopathic medical colleges and are licensed to practice the full scope of medicine and surgery in all 50 U.S. states. The field is distinct from osteopathic practices offered in nations outside of the U.S.—in which practitioners are generally considered neither parts of core medical staff nor of medicine itself; rather, they are considered alternative medicine practitioners. The other major branch of medicine in the United States is referred to by practitioners of osteopathic medicine as allopathic medicine.[1]
By the middle of the 20th century, the profession had moved closer to mainstream medicine. American "osteopaths" became "osteopathic medical doctors", ultimately achieving full practice rights as medical doctors in all 50 states.[2][3]
In modern medicine in the U.S., any distinction between the MD and the DO professions has eroded steadily. The training of osteopathic physicians in the United States is now virtually indistinguishable from the training of allopathic physicians (MDs).[4] Osteopathic physicians attend four years of medical school like their MD counterparts, acquiring equivalent education in medicine and surgery; DOs also attend the same graduate medical education programs (ACGME-accredited residencies and fellowships) as their MD counterparts to acquire their licenses as physicians. DOs use all conventional methods of diagnosis and treatment and practice across all specialties of medicine and surgery. Although osteopathic physicians are still trained in osteopathic manipulative treatment (OMT),[5] the modern derivative of Andrew Taylor Still's techniques,[6][7] during medical school, the majority of practicing physicians with a DO degree do not practice OMT in their daily work.[8] There are ongoing debates about the utility of maintaining separate, distinct pathways for educating physicians in the United States.[9][10]
Nomenclature
[edit]Physicians and surgeons who graduate from osteopathic medical schools are known as osteopathic physicians or osteopathic medical doctors.[3] Upon graduation, they are conferred a Doctor of Osteopathic Medicine (DO) medical degree.[11][12][13]
Osteopathic curricula in countries other than the United States differ from those in the United States. European-trained practitioners of osteopathic manipulative techniques are referred to as "osteopaths": their scope of practice excludes most medical therapies and relies more on osteopathic manipulative medicine and alternative medical modalities.[14] While it was once common for DO graduates in the United States to refer to themselves as "osteopaths", this term is now considered archaic. Those holding the DO degree are commonly referred to as "osteopathic physicians", and they learn, train in, and practice the full scope of mainstream evidence-based medicine and surgery.[15]
Demographics
[edit]
As of 2023,[update] 40 medical schools were offering DO degrees in 64 locations[17] across the United States, while there were 155 accredited MD medical schools (2021–2022).[18]
- In 1960, 13,708 physicians were graduates of the 5 osteopathic medical schools.[19]
- In 2002, there were 49,210 physicians from 19 osteopathic medical schools.[citation needed]
- Between 1980 and 2005, the number of osteopathic graduates per year increased by over 150 percent, from about 1,000 to 2,800. This number was expected to approach 5,000 by 2015.[20]
- In 2016, there were 33 colleges of osteopathic medicine in 48 locations, in 31[21] states.[22] One in four medical students in the United States in 2016 was enrolled in an osteopathic medical school.[23]
- As of 2018,[update] there were more than 145,000 osteopathic physicians and osteopathic medical students in the United States.[23]

Osteopathic physicians are not evenly distributed in the United States. States with the highest concentration of osteopathic physicians are Oklahoma, Iowa, and Michigan, where osteopathic physicians comprised 17–20% of the physician workforce in 2011.[needs update][26] The state with the greatest number of osteopathic physicians is Pennsylvania, with 8,536 DOs in active practice in 2018.[23] The states with the lowest concentrations of DOs are Washington, D.C., North Dakota, and Vermont, where only 1–3% of physicians have an osteopathic medical degree.[when?][25][26] Public awareness of osteopathic medicine likewise varies widely in different regions. In 2003, people living in Midwest states were the most likely to be familiar with osteopathic medicine.[27] In the Northeastern United States, osteopathic physicians provided more than one-third of general and family medicine patient visits between 2003 and 2004.[needs update][28][10]
Between 2010 and 2015, twelve states experienced greater than 50% growth in the number of DOs: Virginia, South Carolina, Utah, Tennessee, North Dakota, Kentucky, South Dakota, Wyoming, Oregon, North Carolina, Minnesota, and Washington.[23]
Osteopathic principles
[edit]
This article appears to contradict the article Osteopathic Oath. (August 2023) |
Osteopathic medical students take the Osteopathic Oath, similar to the Hippocratic oath, to maintain and uphold the "core principles" of osteopathic medical philosophy. Revised in 1953, and again in 2002, the core principles are:
- The body is a unit; a person is a unit of body, mind, and spirit.
- The body is capable of self-regulation, self-healing, and health maintenance.
- Structure and function are reciprocally interrelated.
- Rational treatment is based on an understanding of these principles: body unity, self-regulation, and the interrelationship of structure and function.
Contemporary osteopathic physicians practice evidence-based medicine, indistinguishable from their MD colleagues.[29]
Significance
[edit]There are different opinions on the significance of these principles. Some note that the osteopathic medical philosophy is suggestive of a kind of social movement within the field of medicine, one that promotes a more patient-centered, holistic approach to medicine, and emphasizes the role of the primary care physician within the health care system.[30][31] Others point out that there is nothing in the principles that would distinguish DO from MD training in any fundamental way. One study, published in The Journal of the American Osteopathic Association found a majority of MD medical school administrators and faculty saw nothing objectionable in the core principles listed above, and some endorse them generally as broad medical principles.[29]
History
[edit]19th century, a new movement within medicine
[edit]
Frontier physician Andrew Taylor Still, DO founded the American School of Osteopathy (now the A.T. Still University-Kirksville (Mo.) College of Osteopathic Medicine) in Kirksville, Missouri in 1892 as a radical protest against the turn-of-the-century medical system. A.T. Still believed that the conventional medical system lacked credible efficacy, was morally corrupt and treated effects rather than causes of disease.[32][33] He founded osteopathic medicine in rural Missouri at a time when medications, surgery, and other traditional therapeutic regimens often caused more harm than good. Some of the medicines commonly given to patients during this time were arsenic, castor oil, whiskey, and opium. In addition, unsanitary surgical practices often resulted in more deaths than cures.[34]
Still intended his new system of medicine to be a reformation of the existing 19th-century medical practices. He imagined that someday "rational medical therapy" would consist of the manipulation of the musculoskeletal system, surgery, and very sparingly used drugs. He invented the name "osteopathy" by blending two Greek roots osteon- for bone and -pathos for suffering to communicate his theory that disease and physiologic dysfunction were etiologically grounded in a disordered musculoskeletal system. Thus, by diagnosing and treating the musculoskeletal system, he believed that physicians could treat a variety of diseases and spare patients the negative side effects of drugs.[citation needed]

The new profession faced stiff opposition from the medical establishment at the time. The relationship of the osteopathic and medical professions was often "bitterly contentious"[16] and involved "strong efforts" by medical organizations to discredit osteopathic medicine.[35] Throughout the first half of the twentieth century, the policy of the American Medical Association labeled osteopathic medicine as a cult. The AMA Code of ethics declared it unethical for a medical physician to voluntarily associate with an osteopath.[30][36]
One notable advocate for the fledgling movement was Mark Twain. Manipulative treatments had purportedly alleviated the symptoms of his daughter Jean's epilepsy as well as Twain's own chronic bronchitis. In 1909, he spoke before the New York State Assembly at a hearing regarding the practice of osteopathy in the state. "I don't know as I cared much about these osteopaths until I heard you were going to drive them out of the state, but since I heard that I haven't been able to sleep."[citation needed] Philosophically opposed to the American Medical Association's stance that its own type of medical practice was the only legitimate one, he spoke in favor of licensing for osteopaths. Physicians from the New York County Medical Society responded with a vigorous attack on Twain, who retorted with "[t]he physicians think they are moved by regard for the best interests of the public. Isn't there a little touch of self-interest back of it all?" "... The objection is, people are curing people without a license and you are afraid it will bust up business."[37]
Following an accreditation survey in 1903, the American Osteopathic Association began requiring 3-year curricula at osteopathic medical schools.[38] In 1916, the AOA mandated all DO schools expand programs to four years.[38] In 1929, osteopathic medical schools began teaching pharmacology as a part of the curricula.[38]
1916–1966, federal recognition
[edit]| Years | Identity & Mission | |
| 1892 to 1950 | Manual medicine | |
| 1951 to 1970 | Family practice / manual therapy | |
| 1971 to present | Full service care / multispeciality orientation | |
Recognition by the US federal government was a key goal of the osteopathic medical profession in its effort to establish equivalency with its MD counterparts. Between 1916 and 1966, the profession engaged in a "long and tortuous struggle" for the right to serve as physicians and surgeons in the US Military Medical Corps. On May 3, 1966 Secretary of Defense Robert McNamara authorized the acceptance of osteopathic physicians into all the medical military services on the same basis as MDs. The first osteopathic physician to take the oath of office to serve as a military physician was Harry J. Walter.[39] The acceptance of osteopathic physicians was further solidified in 1996 when Ronald Blanck, DO was appointed to serve as Surgeon General of the Army, the only osteopathic physician to hold the post.[36]
1962, California
[edit]In the 1960s in California, the American Medical Association (AMA) spent nearly $8 million to end the practice of osteopathic medicine in the state. In 1962, Proposition 22, a statewide ballot initiative in California, eliminated the practice of osteopathic medicine in the state. The California Medical Association (CMA) issued MD degrees to all DOs in the state of California for a nominal fee. "By attending a short seminar and paying $65, a doctor of osteopathy (DO) could obtain an MD degree; 86 percent of the DOs in the state (out of a total of about 2000) chose to do so."[40] Immediately following, the AMA re-accredited the University of California at Irvine College of Osteopathic Medicine as the University of California, Irvine School of Medicine, an MD medical school. It also placed a ban on issuing physician licenses to DOs moving to California from other states.[41] However, the decision proved to be controversial. In 1974, after protests and lobbying by influential and prominent DOs, the California Supreme Court ruled in Osteopathic Physicians and Surgeons of California v. California Medical Association, that licensing of DOs in that state must be resumed.[42] Four years later, in 1978, the College of Osteopathic Medicine of the Pacific opened in Pomona, and in 1997, Touro University California opened in Vallejo. As of 2012, there were 6,368 DOs practicing in California.[43]
1969, AMA House of Delegates approval
[edit]
In 1969, the American Medical Association (AMA) approved a measure allowing qualified osteopathic physicians to be full and active members of the Association. The measure also allowed osteopathic physicians to participate in AMA-approved intern and residency programs. However, the American Osteopathic Association rejected this measure, claiming it was an attempt to eliminate the distinctiveness of osteopathic medicine. In 1970, AMA President Dwight L. Wilbur sponsored a measure in the AMA's House of Delegates permitting the AMA Board of Trustees' plan for the merger of DO and MD professions. Today, a majority of osteopathic physicians are trained alongside MDs, in residency programs governed by the ACGME, an independent board of the AMA.[46]
1993, first African-American woman to serve as dean of a US medical school
[edit]In 1993, Barbara Ross-Lee, DO, was appointed to the position of dean of the Ohio University College of Osteopathic Medicine; she was the first African-American woman to serve as the dean of a US medical school.[47] Ross-Lee now[when?] is the dean of the NYIT College of Osteopathic Medicine at Arkansas State University in Jonesboro, Arkansas. Ross-Lee is the sister of singer Diana Ross.[citation needed]
Non-discrimination policies
[edit]Recent[when?] years have seen a professional rapprochement between the two groups. DOs have been admitted to full active membership in the American Medical Association since 1969. The AMA has invited a representative of the American Osteopathic Association to sit as a voting member in the AMA legislative body, the house of delegates.[48]
2006, American Medical Student Association
[edit]In 2006, during the presidency of an osteopathic medical student, the American Medical Student Association (AMSA) adopted a policy regarding the membership rights of osteopathic medical students in their main policy document, the "Preamble, Purposes and Principles."
AMSA RECOGNIZES the equality of osteopathic and allopathic medical degrees within the organization and the healthcare community as a whole. As such, DO students shall be entitled to the same opportunities and membership rights as allopathic students.
— PPP, AMSA[49]
2007, AMA
[edit]In recent[when?] years, the largest MD organization in the US, the American Medical Association, adopted a fee non-discrimination policy discouraging differential pricing based on attendance of an MD or DO medical school.[50]
In 2006, calls for an investigation into the existence of differential fees charged for visiting DO and MD medical students at American medical schools were brought to the American Medical Association. After an internal investigation into the fee structure for visiting DO and MD medical students at MD medical schools, it was found that one institution of the 102 surveyed charged different fees for DO and MD students.[51] The house of delegates of the American Medical Association adopted resolution 809, I-05 in 2007.
Our AMA, in collaboration with the American Osteopathic Association, discourages discrimination against medical students by institutions and programs based on osteopathic or allopathic training.
— AMA policy H-295.876[50]
State licensing of practice rights
[edit]
1901–1930 1931–1966 1967–1989
In the United States, laws regulating physician licenses are governed by the states. Between 1896 and 1973, osteopathic physicians lobbied state legislatures to pass laws giving those with a DO degree the same legal privilege to practice medicine as those with an MD degree. In many states, the debate was long and protracted. Both the AOA and the AMA were heavily involved in influencing the legislative process. The first state to pass such a law was Vermont in 1896, the last was Mississippi in 1973.[41]
Current status
[edit]Education and training
[edit]According to Harrison's Principles of Internal Medicine, "the training, practice, credentialing, licensure, and reimbursement of osteopathic physicians is virtually indistinguishable from those of (MD) physicians, with 4 years of osteopathic medical school followed by specialty and subspecialty training and [board] certification."[1]
DO-granting US medical schools have curricula similar to those of MD-granting schools. Generally, the first two years are classroom-based, while the third and fourth years consist of clinical rotations through the major specialties of medicine.[52] Some schools of Osteopathic Medicine have been criticized by the osteopathic community for relying too heavily on clinical rotations with private practitioners, who may not be able to provide sufficient instruction to the rotating student.[53] Other DO-granting and MD-granting schools place their students in hospital-based clinical rotations where the attending physicians are faculty of the school, and who have a clear duty to teach medical students while treating patients.[citation needed]
Graduate medical education
[edit]
Upon graduation, most osteopathic medical physicians pursue residency training programs. Depending on state licensing laws, osteopathic medical physicians may also complete a one-year rotating internship at a hospital approved by the American Osteopathic Association (AOA).[citation needed] Osteopathic physicians may apply to residency programs accredited by the Accreditation Council for Graduate Medical Education (ACGME). The AOA ceased graduate medical education accreditation activities in 2020.[54]
Osteopathic manipulative treatment (OMT)
[edit]Within the osteopathic medical curriculum, manipulative treatment is taught as an adjunctive measure to other biomedical interventions for several disorders and diseases. However, a 2001 survey of osteopathic physicians found that more than 50% of the respondents used OMT on less than 5% of their patients. The survey follows many indicators that osteopathic physicians have become more like MD physicians in every respect —few perform OMT, and most prescribe medications or suggest surgery as the first line of treatment.[55] The American Osteopathic Association has made an effort in recent[when?] years to support scientific inquiry into the effectiveness of osteopathic manipulation as well as to encourage osteopathic physicians to consistently offer manipulative treatments to their patients. However, the number of osteopathic physicians who report consistently prescribing and performing manipulative treatment has been falling steadily. Medical historian and sociologist Norman Gevitz[30] cites poor educational quarters and few full-time OMT instructors as major factors for the decreasing interest of medical students in OMT. He describes problems with "the quality, breadth, nature, and orientation of OMM instruction," and he claims that the teaching of osteopathic medicine has not changed sufficiently over the years to meet the intellectual and practical needs of students.[29]
In their assigned readings, students learn what certain prominent DOs have to say about various somatic dysfunctions. There is often a theory or model presented that provides conjectures and putative explanations about why somatic dysfunction exists and what its significance is. Instructors spend the bulk of their time demonstrating osteopathic manipulative (OM) techniques without providing evidence that the techniques are significant and efficacious. Even worse, faculty members rarely provide instrument-based objective evidence that somatic dysfunction is present in the first place.[29]

At the same time, recent[when?] studies show an increasingly positive attitude of patients and physicians (MD and DO) toward the use of manual therapy as a valid, safe, and effective treatment modality.[56] One survey, published in the Journal of Continuing Medical Education, found that a majority of physicians (81%) and patients (76%) felt that manual manipulation (MM) was safe, and over half (56% of physicians and 59% of patients) felt that manipulation should be available in the primary care setting. Although less than half (40%) of the physicians reported any educational exposure to MM and less than one-quarter (20%) have administered MM in their practice, most (71%) respondents endorsed desiring more instruction in MM.[57] Another small study examined the interest and ability of MD residents in learning osteopathic principles and skills, including OMT. It showed that after a 1-month elective rotation, the MD residents responded favorably to the experience.[58]
Professional attitudes
[edit]In 1998, an article in The New York Times described the increasing numbers, public awareness, and mainstreaming of osteopathic medical physicians, illustrating an increasingly cooperative climate between the DO and MD professions.[30]
In 2005, during his tenure as president of the Association of American Medical Colleges, Jordan Cohen described a climate of cooperation between DO and MD practitioners:
"We now find ourselves living at a time when osteopathic and allopathic graduates are both sought after by many of the same residency programs; are in most instances both licensed by the same licensing boards; are both privileged by many of the same hospitals; and are found in appreciable numbers on the faculties of each other's medical schools".[16][59]
International practice rights
[edit]
Each country has different requirements and procedures for licensing or registering osteopathic physicians and osteopaths. The only osteopathic practitioners that the US Department of Education recognizes as physicians are graduates of osteopathic medical colleges in the United States.[60]
The Bureau on International Osteopathic Medical Education and Affairs (BIOMEA) is an independent board of the American Osteopathic Association. The BIOMEA monitors the licensing and registration practices of physicians in countries outside of the United States and advances the recognition of American-trained DOs. Towards this end, the BIOMEA works with international health organizations like the World Health Organization (WHO), the Pan American Health Organization (PAHO) as well as other groups.[61]
The procedure by which countries consider granting physician licensure to foreigners varies widely. For US-trained physicians, the ability to qualify for "unlimited practice rights" also varies according to one's degree, MD or DO.[62] Many countries recognize US-trained MDs as applicants for licensure, granting successful applicants "unlimited" practice rights. The American Osteopathic Association has lobbied the governments of other countries to recognize US-trained DOs similarly to their MD counterparts, with some success.[citation needed]
| Osteopathic Medicine and Osteopathy |
| Osteopathy in Australia and New Zealand |
| Osteopathic medicine in Canada |
| Osteopathy in Europe Osteopathy in the UK |
| Osteopathic medicine in the United States |
According to Josh Kerr of the AOA, "some countries don’t understand the differences in training between an osteopathic physician and an osteopath."[63] The American Medical Student Association strongly advocates for US-trained DO international practice rights "equal to that" of MD-qualified physicians.[49]
The International Labor Organization (ILO), an agency of the United Nations, issued a letter affirming that U.S.-trained osteopathic physicians are fully licensed physicians who prescribe medication and perform surgery. The acknowledgment draws a clear separation between American DOs, who are medical doctors, and non-physician osteopaths trained outside of the United States. Within the international standards that classify jobs to promote international comparability across occupations, U.S.-trained DOs are now categorized with all other physicians as medical doctors. This event took place in June 2018 and started a relay of events and opened doors for DO's as more countries started to understand and give full recognition to US-trained medical doctors with the D.O. degree, e.g. the Association of Medical Councils of Africa (AMCOA) approved a resolution in 2019 granting the AOA's request that AMCOA recognizes U.S.-trained DOs as fully licensed physicians with practice rights equivalent to MDs, opening its 20 member countries, which include Botswana, Gambia, Ghana, Kenya, Lesotho, Liberia, Malawi, Mauritius, Namibia, Nigeria, Rwanda, Seychelles, Sierra Leone, South Africa, South Sudan, Swaziland, Tanzania, Uganda, Zambia, and Zimbabwe to DO's.[citation needed]
In primary care
[edit]
Osteopathic physicians have historically entered primary care fields at a higher rate than their MD counterparts. Some osteopathic organizations make claims to a greater emphasis on the importance of primary care within osteopathic medicine. However, the proportion of osteopathic students choosing primary care fields, like that of their MD peers, is declining.[65] Currently,[when?] only one in five osteopathic medical students enters a family medicine residency (the largest primary care field).[needs update][66] In 2004, only 32% of osteopathic seniors planned careers in any primary care field; this percentage was down from a peak in 1996 of more than 50%.[64]
Criticism and internal debate
[edit]This section needs to be updated. (August 2023) |
This article contains too many or overly lengthy quotations. (August 2023) |
OMT
[edit]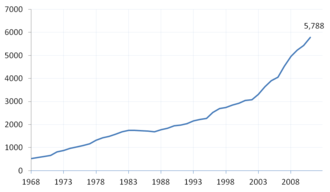
Traditional osteopathic medicine, specifically OMT, has been criticized for using techniques such as cranial and cranio-sacral manipulation. CST has been described as pseudoscience which is not backed up by any scientific evidence.[67] Medical research has found no good evidence that either CST or cranial osteopathy confers any health benefit, and they can be harmful, particularly if used on children or infants.[68][69][70] The basic assumptions of CST are challenged by some medical doctors, and practitioners produce conflicting and mutually exclusive diagnoses of the same patients.[71]
Research emphasis
[edit]Another area of criticism has been the relative lack of research and lesser emphasis on scientific inquiry at DO schools in comparison with MD schools.[72][73][74]
The inability to institutionalize research, particularly clinical research, at osteopathic institutions has, over the years, weakened the acculturation, socialization, and distinctive beliefs and practices of osteopathic students and graduates.[72]
Identity crisis
[edit]A debate exists within the osteopathic community over the feasibility of maintaining osteopathic medicine as a distinct entity within US health care.[2][29][75][76][77][78][79][80][81] J. D. Howell, author of The Paradox of Osteopathy,[40] notes claims of a "fundamental yet ineffable difference" between MD and DO qualified physicians are based on practices such as "preventive medicine and seeing patients in a sociological context" that are "widely encountered not only in osteopathic medicine but also in allopathic medicine."[82] Studies have confirmed the lack of any "philosophic concept or resultant practice behavior" that would distinguish a DO from an MD.[83][84] Howell summarizes the questions framing the debate over the future of osteopathic distinctiveness thus:
If osteopathy has become the functional equivalent of allopathy [meaning the MD profession], what is the justification for its continued existence? And if there is value in therapy that is uniquely osteopathic, why should its use be limited to osteopaths?[40]
Rapid expansion
[edit]As the number of osteopathic schools has increased, the debate over distinctiveness has often seen the leadership of the American Osteopathic Association at odds with the community of osteopathic physicians.
Within the osteopathic community, the growth is drawing attention to the identity crisis faced by [the profession]. While osteopathic leaders emphasize osteopaths' unique identity, many osteopaths would rather not draw attention to their uniqueness.[48]
The rapid expansion has raised concerns about the number of available faculty at osteopathic schools and the role that those faculty play in maintaining the integrity of the academic program of the schools. Norman Gevitz, author of the leading text on the history of osteopathic medicine, wrote in 2009,
DO schools are currently expanding their class sizes much more quickly than are their MD counterparts. Unlike MD colleges, where it is widely known that academic faculty members—fearing dilution of quality as well as the prospect of an increased teaching workload—constitute a powerful inhibiting force to expand the class size, osteopathic faculty at private osteopathic schools have traditionally had little or no input on such matters. Instead, these decisions are almost exclusively the responsibility of college administrators and their boards of trustees, who look at such expansion from an entrepreneurial as well as an educational perspective. Osteopathic medical schools can keep the cost of student body expansion relatively low compared with that of MD institutions. Although the standards of the Commission on Osteopathic College Accreditation ensure that there will be enough desks and lab spaces to accommodate all new students, they do not mandate that an osteopathic college must bear the expense of maintaining a high full-time faculty: student ratio.[38]
The president of the American Association of Colleges of Osteopathic Medicine commented on the current climate of crisis within the profession.
The simultaneous movement away from osteopathic medicine’s traditionally separate training and practice systems, when coupled with its rapid growth, has created a sense of crisis as to its future. The rapid rate of growth has raised questions as to the availability of clinical and basic science faculty and clinical resources to accommodate the increasing load of students.[52]
See also
[edit]- Comparison of MD and DO in the United States
- Doctor of Osteopathic Medicine
- List of osteopathic colleges
- Osteopathic medical schools in the United States
- Osteopathic medical associations in the United States
- Osteopathy
References
[edit]- ^ a b "Joint statement from the American Osteopathic Association and American Medical Association: AOA and AMA stand against misrepresentation of osteopathic physicians". American Medical Association. 4 November 2020. Archived from the original on 10 May 2021. Retrieved 28 May 2021.
- ^ a b c Meyer CT, Price A (April 1993). "Osteopathic medicine: a call for reform". The Journal of the American Osteopathic Association. 93 (4): 473–485. doi:10.7556/jaoa.1993.93.4.473. PMID 8267703.
- ^ a b Wu P, Siu J (2012). "A Brief Guide to Osteopathic Medicine For Students, By Students" (PDF). American Association of Colleges of Osteopathic Medicine. Archived (PDF) from the original on 15 April 2013. Retrieved 20 August 2013.
- ^ Kasper DL, Braunwald E, Fauci AS, Hauser SL, Longo DL, Jameson JL, Isselbacher KJ (2012). "Chapter 10. Complementary and Alternative Medicine". Harrison's Principles of Internal Medicine (18th ed.). New York: McGraw-Hill. ISBN 978-0-07-174889-6. Archived from the original on 2013-12-24.
- ^ Lesho EP (Nov 1999). "An overview of osteopathic medicine". Archives of Family Medicine. 8 (6): 477–484. doi:10.1001/archfami.8.6.477. PMID 10575385.[permanent dead link]
- ^ "Osteopathic Medicine". Intelihealth.com. Archived from the original on 2007-04-15. Retrieved 1 December 2007.
- ^ DiGiovanna EL, Schiowitz S, Dowling DJ (2004). An Osteopathic Approach to Diagnosis and Treatment (3rd ed.). Lippincott Williams & Wilkins. ISBN 978-0-7817-4293-1.
- ^ Healy CJ, Brockway MD, Wilde BB (January 2021). "Osteopathic manipulative treatment (OMT) use among osteopathic physicians in the United States". Journal of Osteopathic Medicine. 121 (1): 57–61. doi:10.1515/jom-2020-0013. PMID 33512391.
- ^ Cohen JJ (June 2009). "The separate osteopathic medical education pathway: isn't it time we got our acts together? Counterpoint". Academic Medicine. 84 (6): 696. doi:10.1097/ACM.0b013e3181a3ddaa. PMID 19474536.
- ^ a b Chen C, Mullan F (June 2009). "The separate osteopathic medical education pathway: uniquely addressing national needs. Point". Academic Medicine. 84 (6): 695. doi:10.1097/ACM.0b013e3181a3dd28. PMID 19474535.
- ^ Gevitz N (March 1997). "'Visible and recognized': osteopathic invisibility syndrome and the two percent solution". The Journal of the American Osteopathic Association. 97 (3): 168–170. doi:10.7556/jaoa.1997.97.3.168. PMID 9107129.
- ^ Clark RC (January 2000). "Increased awareness of osteopathic medicine is essential to the profession's survival" (Free full text). The Journal of the American Osteopathic Association. 100 (1): 6–8. PMID 10693310.[permanent dead link]
- ^ Oths KS, Hinojosa SZ (2004). "Divergences in the evolution of Osteopathy". Healing by Hand: Manual Medicine and Bonesetting in Global Perspective. Rowman Altamira. pp. 67–68. ISBN 978-0-7591-0393-1.
- ^ "The Difference Between U.S.-Trained Osteopathic Physicians and Osteopaths Trained Abroad". AACOM. Archived from the original on Aug 28, 2016. Retrieved 21 August 2016.
- ^ "Terminology for Reporting on Osteopathic Medicine". American Osteopathic Association. Archived from the original on 2013-05-14. Retrieved 17 May 2012.
- ^ a b c Cohen J (April 2005). "A Word from the President: "Filling the Workforce Gap"". Reporter. AAMC. Archived from the original on Oct 26, 2008.
- ^ "U.S. Colleges of Osteopathic Medicine". American Association of Colleges of Osteopathic Medicine. Archived from the original on Aug 10, 2023.
- ^ Barzansky B, Etzel SI (20 September 2022). "MD-Granting Medical Schools in the US, 2021–2022". JAMA. 328 (11): 1112–1122. doi:10.1001/jama.2022.14384. PMID 36125488.
- ^ Maryland Y. Pennell (October 1964). "Statistics on Physicians, 1950-63" (PDF). Public Health Reports. 79 (10): 905–910. doi:10.2307/4592275. JSTOR 4592275. PMC 1915580. PMID 14198580. Archived (PDF) from the original on 2023-02-26. Retrieved 2024-03-14.
- ^ Salsberg E, Grover A (September 2006). "Physician workforce shortages: implications and issues for academic health centers and policymakers". Academic Medicine. 81 (9): 782–787. doi:10.1097/00001888-200609000-00003. PMID 16936479.
- ^ AOA Annual Statistics, 2016
- ^ "AOA Annual Statistics 2016". U.S. Colleges of Osteopathic Medicine. American Association of Colleges of Osteopathic Medicine. January 2016. Archived from the original on 2016-01-25. Retrieved 2016-01-27.
- ^ a b c d "Osteopathic Medical Profession Report" (PDF). Archived from the original (PDF) on 29 June 2017. Retrieved 28 May 2021.
- ^ "U.S. Colleges of Osteopathic Medicine". Aacom.org. Archived from the original on 26 October 2014. Retrieved 9 May 2021.
- ^ a b "2006 Annual Statistical Report on Osteopathic Medical Education". American Association of Colleges of Osteopathic Medicine. February 2007. Archived from the original on 2008-02-27. Retrieved 2008-03-07.
- ^ a b "2011 State Physician Workforce Data Book" (PDF). Association of American Medical Colleges. p. 23. Archived (PDF) from the original on 30 July 2018. Retrieved 9 May 2021.
- ^ Licciardone JC (June 2003). "Awareness and use of osteopathic physicians in the United States: results of the Second Osteopathic Survey of Health Care in America (OSTEOSURV-II)". The Journal of the American Osteopathic Association. 103 (6): 281–289. PMID 12834101.
- ^ Licciardone JC (January 2007). "A comparison of patient visits to osteopathic and allopathic general and family medicine physicians: results from the National Ambulatory Medical Care Survey, 2003–2004". Osteopathic Medicine and Primary Care Practice. 1: 2. doi:10.1186/1750-4732-1-2. PMC 1805772. PMID 17371578.
- ^ a b c d e Gevitz N (March 2006). "Center or periphery? The future of osteopathic principles and practices" (Free full text). The Journal of the American Osteopathic Association. 106 (3): 121–129. PMID 16585378.[permanent dead link]
- ^ a b c d Zuger A (February 17, 1998). "Scorned No More, Osteopathy Is on the Rise". The New York Times. Archived from the original on August 19, 2016. Retrieved February 18, 2017.
- ^ "About Osteopathic Medicine". American Osteopathic Association. Archived from the original on 6 September 2012. Retrieved 30 August 2007.
- ^ Still AT (1902). The Philosophy and Mechanical Principles of Osteopathy. Kansas City, Mo: Hudson-Kimberly Pub Co. pp. 9–20, 185, 210, 270. Version 2.0. Inter Linea Web site. Text version recognised with imperfect OCR.
- ^ Still AT (1902). The Philosophy and Mechanical Principles of Osteopathy. Kansas City, Mo.: Hudson Kimberley Pub. Co. Web page linking to facsimile images of the original book in several formats, including imperfect OCR text and PDF.
- ^ Hansen GP (March 2006). "Beyond OMT: time for a new chapter in osteopathic medicine?" (Free full text). The Journal of the American Osteopathic Association. 106 (3): 114–116. PMID 16585374.
- ^ Chapter 34: Complementary and Alternative Medicine. Goldman: Cecil Textbook of Medicine, 22nd ed. Saunders. 2004.
- ^ a b Gevitz N (May 1998). "The sword and the scalpel—the osteopathic 'war' to enter the Military Medical Corps: 1916–1966" (Free full text). The Journal of the American Osteopathic Association. 98 (5): 279–286. PMID 9615560.[permanent dead link]
- ^ Ober KP (January 1997). "The pre-Flexnerian reports: Mark Twain's criticism of medicine in the United States". Annals of Internal Medicine. 126 (2): 157–163. CiteSeerX 10.1.1.695.316. doi:10.7326/0003-4819-126-2-199701150-00012. PMID 9005751. S2CID 32352763.
- ^ a b c d Gevitz N (June 2009). "The transformation of osteopathic medical education". Academic Medicine. 84 (6): 701–706. doi:10.1097/ACM.0b013e3181a4049e. PMID 19474540.
- ^ "Notable DOs". Kansas City University of Medicine and Biosciences. Archived from the original on 7 January 2016. Retrieved 9 May 2021.
- ^ a b c Howell JD (November 1999). "The paradox of osteopathy". The New England Journal of Medicine. 341 (19): 1465–1468. doi:10.1056/NEJM199911043411910. PMID 10547412.
- ^ a b Gevitz N (2004). The DO's: osteopathic medicine in America. Baltimore, Maryland: Johns Hopkins University Press. ISBN 978-0-8018-7833-6.
- ^ Crum JF (January 1975). "The saga of osteopathy in California". The Western Journal of Medicine. 122 (1): 87–90. PMC 1130289. PMID 1089010.
- ^ Robertson K (March 23, 2012). "Part of cure for doctor shortage: Osteopaths". Sacramento Business Journal. Archived from the original on December 18, 2013. Retrieved June 5, 2012.
- ^ Brotherton SE, Rockey PH, Etzel SI (September 2005). "US graduate medical education, 2004–2005: trends in primary care specialties". JAMA. 294 (9): 1075–1082. doi:10.1001/jama.294.9.1075. PMID 16145028.
- ^ a b Shannon SC. "The Impact of Osteopathic Medicine's Growth on Physician Workforce" (PDF). AAMC. Archived from the original (PDF) on 2008-04-11.
- ^ Tulgan H, DeMarco WJ, Pugnaire MP, Buser BR (May 2004). "Joint clinical clerkships for osteopathic and allopathic medical students: New England's experience". The Journal of the American Osteopathic Association. 104 (5): 212–214. PMID 15176520.
- ^ "Dr. Barbara Ross-Lee". National Library of Medicine. Archived from the original on 10 March 2016. Retrieved 9 May 2021.
- ^ a b Wilson JF. "Osteopathic Medicine's Growing Pains". ACP Internist. Archived from the original on 5 December 2008. Retrieved 28 May 2021.
- ^ a b "Principles Regarding Osteopathic Medicine".; [permanent dead link] "Preamble, Purposes and Principles". AMSA. American Medical Student Association. 2012. Archived from the original on 2012-03-21.
- ^ a b "AMA policy H-295.876" (PDF). Archived (PDF) from the original on 2012-11-04. Retrieved 2012-11-30.
- ^ Thomas M. "Recommendation on Equal Fees for Osteopathic and Allopathic Medical Students" (PDF). Report of the Council on Medical Education (Report 6-A-07). American Medical Association. Archived (PDF) from the original on 12 February 2012. Retrieved 1 July 2012.
- ^ a b Shannon SC, Teitelbaum HS (June 2009). "The status and future of osteopathic medical education in the United States". Academic Medicine. 84 (6): 707–711. doi:10.1097/ACM.0b013e3181a43be8. PMID 19474542.
- ^ Hubbard K (January 17, 2011). "Letter to Touro College of Osteopathic Medicine" (PDF). Missouri Association of Osteopathic Physicians and Surgeons. Retrieved May 4, 2011.[permanent dead link]
- ^ "Single GME Accreditation System". www.acgme.org. Archived from the original on 17 June 2016. Retrieved 24 May 2016.
- ^ Johnson SM, Kurtz ME (August 2001). "Diminished use of osteopathic manipulative treatment and its impact on the uniqueness of the osteopathic profession". Academic Medicine. 76 (8): 821–828. doi:10.1097/00001888-200108000-00016. PMID 11500286.
- ^ Licciardone J, Gamber R, Cardarelli K (January 2002). "Patient satisfaction and clinical outcomes associated with osteopathic manipulative treatment". The Journal of the American Osteopathic Association. 102 (1): 13–20. PMID 11837337.
- ^ Stoll ST, Russo DP, Atchison JW (Winter 2003). "Physicians' and patients' attitudes toward manual medicine: implications for continuing medical education". The Journal of Continuing Education in the Health Professions. 23 (1): 13–20. doi:10.1002/chp.1340230104. PMID 12739255. S2CID 22834761.
- ^ Leiber JD (Nov 2005). "Allopathic family medicine residents can learn osteopathic manipulation techniques in a 1-month elective" (Free full text). Family Medicine. 37 (10): 693–695. PMID 16273444. Archived (PDF) from the original on 2007-09-27. Retrieved 2007-08-31.
- ^ Cohen J. "Following in Flexner's Footsteps". American Medical Association. Archived from the original on 23 February 2013. Retrieved 14 July 2012.
- ^ "Notices" (PDF). 3 October 2005. Archived from the original (PDF) on 2008-04-11. 70 FR 57571
- ^ "International Practice Rights Map". American Osteopathic Association. Archived from the original on 2016-08-19. Retrieved 1 July 2012.
- ^ "AOA International License Summary" (PDF). American Osteopathic Association. Council on International Osteopathic Medical Education and Affairs. [permanent dead link]
- ^ "DOs Around the World". American Osteopathic Association. Archived from the original on 6 September 2012. Retrieved 12 June 2013.
- ^ a b Singer AM. "Debt, Plans and Opinions of Osteopathic Medical Students in 2004". American Association of Colleges of Osteopathic Medicine. Archived from the original on 2014-03-07. Retrieved 2008-02-14.
- ^ Cummings M, Dobbs KJ (July 2005). "The irony of osteopathic medicine and primary care". Academic Medicine. 80 (7): 702–705. doi:10.1097/00001888-200507000-00017. PMID 15980090.
- ^ Graham C (August 2005). "Osteopathic physicians and the family medicine workforce" (Free full text). American Family Physician. 72 (4): 583. PMID 16127950.
- ^ * Norcross JC, Koocher GP, Garofalo A (2006). "Discredited psychological treatments and tests: A Delphi poll". Professional Psychology: Research and Practice. 37 (5): 515–22. doi:10.1037/0735-7028.37.5.515. S2CID 35414392.
- Mac Manus M (July 2008). "Unproven medical devices and cancer therapy: big claims but no evidence". Biomedical Imaging and Intervention Journal (Review). 4 (3): e25. doi:10.2349/biij.4.3.e25. PMC 3097732. PMID 21610999.
- Bledsoe BE (October 2004). "The elephant in the room: does OMT have proved benefit?". The Journal of the American Osteopathic Association. 104 (10): 405–6, author reply 406. PMID 15537794.
- Hartman SE (June 2006). "Cranial osteopathy: its fate seems clear". Chiropractic & Osteopathy. 14: 10. doi:10.1186/1746-1340-14-10. PMC 1564028. PMID 16762070.
- Atwood KC (March 2004). "Naturopathy, pseudoscience, and medicine: myths and fallacies vs truth". MedGenMed. 6 (1): 33. PMC 1140750. PMID 15208545.
- ^ Russell J, Rovere A, eds. (2009). "Craniosacral Therapy". American Cancer Society Complete Guide to Complementary and Alternative Cancer Therapies (2nd ed.). American Cancer Society. pp. 187–189. ISBN 978-0-944235-71-3.
- ^ Ferré JC, Chevalier C, Lumineau JP, Barbin JY (September 1990). "[Cranial osteopathy, delusion or reality?]". Actualites Odonto-Stomatologiques. 44 (171): 481–494. PMID 2173359.
- ^ Cassileth BR (2011). "Chapter 42: Craniosacral Therapy". The Complete Guide to Complementary Therapies in Cancer Care: Essential Information for Patients, Survivors and Health Professionals. World Scientific. pp. 247–250. ISBN 978-981-4335-16-4.
- ^ Ingraham P (October 16, 2020). "Craniosacral Therapy: Does it Work?". PainScience.com. Archived from the original on August 7, 2019. Retrieved February 5, 2021.
- ^ a b Gevitz N (March 2001). "Researched and demonstrated: inquiry and infrastructure at osteopathic institutions" (Free full text). The Journal of the American Osteopathic Association. 101 (3): 174–179. PMID 11329813.[permanent dead link]
- ^ Kelso A, Townsend A. The status and future of osteopathic research. In: Northup G, ed. Osteopathic Research: Growth and Development. Chicago, Ill: American Osteopathic Association; 1987.
- ^ Licciardone JC (February 2007). "Osteopathic research: elephants, enigmas, and evidence". Osteopathic Medicine and Primary Care. 1: 7. doi:10.1186/1750-4732-1-7. PMC 1808471. PMID 17371583.
- ^ Gevitz N (April 1994). "'Parallel and distinctive': the philosophic pathway for reform in osteopathic medical education". The Journal of the American Osteopathic Association. 94 (4): 328–332. doi:10.7556/jaoa.1994.94.4.328. PMID 8027001.
- ^ Teitelbaum HS, Bunn WE, Brown SA, Burchett AW (October 2003). "Osteopathic medical education: renaissance or rhetoric?". The Journal of the American Osteopathic Association. 103 (10): 489–490. PMID 14620084. Archived from the original on 2016-03-05.
- ^ Tatum IV WO (August 2006). "AOA needs to reach out more". The Journal of the American Osteopathic Association. 106 (8): 442–443. PMID 16943511. Archived from the original on 2008-01-25.
- ^ Mychaskiw G (May 2006). "Will the last DO turn off the lights?" (Free full text). The Journal of the American Osteopathic Association. 106 (5): 252–253, 302, 253 302–253. PMID 16717365.[permanent dead link]
- ^ Steier KJ (May 2006). "Time to accept allopathic physicians into AOA-approved residencies?" (Free full text). The Journal of the American Osteopathic Association. 106 (5): 250–252. PMID 16717364.[permanent dead link]
- ^ Tosca M (June 2006). "Future of osteopathic medicine depends on investing in graduate medical education" (Free full text). The Journal of the American Osteopathic Association. 106 (6): 319. PMID 16790537.[permanent dead link]
- ^ Shannon SC (1 February 2008). "What Does the Future Hold?". Inside Osteopathic Medical Education. 2 (2): 1. Archived from the original on 19 January 2013.
- ^ Howell JD (16 March 2000). "Reply: Osteopathic Treatment of Low Back Pain". New England Journal of Medicine. 342 (11): 817–820. doi:10.1056/NEJM200003163421112. PMID 10722333. Archived from the original on 18 February 2003. Retrieved 5 November 2007.
- ^ Johnson SM, Kurtz ME (December 2002). "Perceptions of philosophic and practice differences between US osteopathic physicians and their allopathic counterparts". Social Science & Medicine. 55 (12): 2141–2148. doi:10.1016/S0277-9536(01)00357-4. PMID 12409127.
- ^ Licciardone JC (January 2007). "A comparison of patient visits to osteopathic and allopathic general and family medicine physicians: results from the National Ambulatory Medical Care Survey, 2003–2004". Osteopathic Medicine and Primary Care. 1: 2. doi:10.1186/1750-4732-1-2. PMC 1805772. PMID 17371578.
Further reading
[edit]- Gevitz N (2004). The DOs: Osteopathic Medicine in America (2nd ed.). The Johns Hopkins University Press. ISBN 0-8018-7834-9.
- Stone C, Thornes N (1999). Science in the Art of Osteopathy: Osteopathic Principles and Models. Nelson Thornes. ISBN 0-7487-3328-0.
- DiGiovanna E (2004). An Osteopathic Approach to Diagnosis and Treatment. Lippincott Williams and Wilkins. ISBN 0-7817-4293-5.
 KSF
KSF