Opioid Withdrawal
 From Mdwiki
From Mdwiki | Opioid withdrawal | |
|---|---|
| Other names: Opioid withdrawal syndrome (OWS), dope sick | |
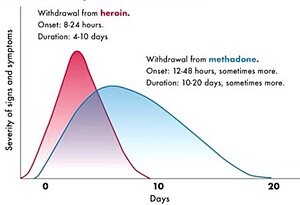 | |
| Course of opioid withdrawal[1] | |
| Specialty | Emergency medicine, psychiatry |
| Symptoms | Runny nose, large pupils, goose bumps, muscle pains, nausea, diarrhea, sweating, fast heart rate, yawning[2] |
| Complications | Dehydration, electrolyte abnormalities[3] |
| Duration | 1-2 week[4][5] |
| Causes | Sudden reduction of opioids or an opioid antagonist[4] |
| Differential diagnosis | Withdrawal from other drugs, stimulant toxicity, opioid use disorder[2][4] |
| Treatment | Opioid replacement therapy (ORT), clonidine, metoclopramide, loperamide[5] |
Opioid withdrawal is a set of symptoms arising from the sudden reduction of opioids or an opioid antagonist after a period of opioid use.[4] Symptoms may include a runny nose, large pupils, goose bumps, muscle pains, nausea, diarrhea, sweating, fast heart rate, and yawning.[2] Symptoms may last a few days.[3] While rarely life threatening, complications may include dehydration and electrolyte abnormalities.[3][6]
All opioids can be followed by withdrawal, regardless of if they were used recreational or by prescription.[4][7] Onset may occur as early as 6 hours following the use of short acting opioids like heroin or as late as 4 days following the use of long acting agents like methadone.[4] Severity of withdrawal is often based on a Clinical Opioid Withdrawal Scale (COWS).[2]
Opioid withdrawal can be treated with opioid replacement therapy (buprenorphine or methadone).[6][5] Symptoms may be improved with clonidine or lofexidine.[8] Without treatment the worst of the symptoms last about a week, though minor symptoms may remain for longer.[4]
About 16 million people use opioids illegally globally.[2] In those who have used heroin in the prior year, withdrawal had occurred in about 60% of them.[4] Many people who continue opioid use, do so in an effort to prevent withdrawal.[5] Opioid withdrawal may have been described as early as the 5th century BC by Hippocrates.[9] Descriptions in the medical literature date to at least 1701.[10]
Signs and symptoms[edit | edit source]
Withdrawal from any opioid produces similar symptoms. The severity and duration of withdrawal depends on the type of opioid taken.
The symptoms of opioid withdrawal may develop within minutes to several days following reduction or stopping.[4] Symptoms can include: extreme anxiety, nausea or vomiting, muscle aches, a runny nose, sneezing, diarrhea, and fever.[4] Males may also experience spontaneous ejaculations whilst awake, and sweating.[4]
Pathophysiology[edit | edit source]
Repeated dosages of opioids can quickly lead to tolerance and physical dependence. This is the marked decrease in opioid receptor sensitivity caused by long-term receptor stimulation triggering receptor desensitisation (in this case receptor internalisation).[3] Tolerance causes a decrease in opioid sensitivity, impairing the efficacy of endogenous (our own body's) opioid molecules that function in multiple brain regions. Opioids partially signal through the decrease in cellular cAMP. Cells with decreased cAMP adapt to regulate cAMP and increase production. In the tolerant brain the sudden withdrawal of opioids coupled with the reduced sensitivity to inhibitory signals from the endogenous opioid systems can cause abnormally high levels of cAMP that may be responsible for withdrawal behaviours.[11] Similar changes may also be responsible for the peripheral gastrointestinal effects such as diarrhea, as there is a reversal of the effect on gastrointestinal motility.[12]
Due to the difference in lipophilicity and mode of release between opioid analgesics, the severity and duration of withdrawal symptoms may differ.
The followings are the general descriptions of duration of opioid withdrawal symptoms:[13]
- High intake for a long duration (> 6 Months) is associated with more severe level of withdrawal symptoms.
- Short-acting or slow-released opioids result in more rapid onset and shorter duration of withdrawal symptoms.
- Longer-acting opioids results in slower onset but longer duration of withdrawal symptoms.
Diagnosis[edit | edit source]

The diagnosis of opioid withdrawal requires recent use or exposure to opioids and symptoms consistent with the disorder.[15] The severity of symptoms can be assessed by validated withdrawal scales, such as the Clinical Opiate Withdrawal Scale (COWS).[16]
Management[edit | edit source]
Treatment for opioid withdrawal is based on underlying diagnostic features. A person with an acute opioid withdrawal but no underlying opioid use disorder can be managed by slowly reducing opioids and treatments aimed at the symptoms.[3]
Acute withdrawal[edit | edit source]
Opioid withdrawal is exacerbated noradrenaline. Alpha 2 adrenergic agonists can be used to manage the symptoms of acute withdrawal. Lofexidine and clonidine are also used for this purpose; both are considered to be equally effective, though clonidine has more side effects than lofexidine.[17]
Opioid replacement[edit | edit source]
The treatment of withdrawal in people with opioid use disorder additionally relies on symptomatic management in addition tapering with medications that replace typical opioids including buprenorphine and methadone. The principle of managing the syndrome is to allow the concentration of drugs in blood to fall to near zero and reverse physiological adaptation. This allows the body to adapt to the absence of drugs in order to reduce the withdrawal symptoms. The most commonly used strategy is to offer opioid drug users with long-acting opioid drugs and slowly taper the dose of the drug. Methadone and buprenorphine are often used in treating opioid withdrawal syndrome.[18]
-
Buprenorphine tablets
-
Buprenorphine patches
Ineffective[edit | edit source]
The cost of opioid replacement treatments have led some people to try treatments with limited evidence. At high doses, loperamide has been reported by some to alleviate syndrome.[19] The doses reported in the literature are associated with a strong risk of damage to the heart.[20]
Society and culture[edit | edit source]
When withdrawal symptoms are due to recreational opioid use – the term opioid use disorder is used; when due to prescribed medications the term prescription opioid use disorder is used.[21]
Newborns[edit | edit source]
Neonatal opioid withdrawal syndrome, also known as the neonatal abstinence syndrome,[22] may occur in babies born to women who used opioids during pregnancy. Common signs include high-pitched crying, reduced sleep, tremors, seizures, gastrointestinal dysfunction, vomiting, sweating, hyperthermia, yawning and sneezing, faster breathing rate, and nasal congestion.[22] Symptoms can develop up to 3 to 7 days after birth.[23]
Treatment of minor symptoms is supportive.[23] In those with severe symptoms an opioid may be provided.[23] Breastfeeding should be encouraged if a women has been stable on either buprenorphine or methadone for more than 90 days.[23]
Many thousands of babies are borne each year after being exposed to opioids].[22] The use of opioids during pregnancy creates a dependency in the newborn which affects the central nervous system (CNS), and the autonomic nervous system (ANS) are affected.
See also[edit | edit source]
References[edit | edit source]
- ↑ Lerner, A; Klein, M (2019). "Dependence, withdrawal and rebound of CNS drugs: an update and regulatory considerations for new drugs development". Brain communications. 1 (1): fcz025. doi:10.1093/braincomms/fcz025. PMID 32954266.
- ↑ 2.0 2.1 2.2 2.3 2.4 Shah, M; Huecker, MR (January 2021). "Opioid Withdrawal". PMID 30252268.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ 3.0 3.1 3.2 3.3 3.4 Volkow, Nora D.; Blanco, Carlos (2020-01-02). "Medications for opioid use disorders: clinical and pharmacological considerations". The Journal of Clinical Investigation. 130 (1): 10–13. doi:10.1172/JCI134708. ISSN 0021-9738. PMC 6934219. PMID 31763992.
- ↑ 4.00 4.01 4.02 4.03 4.04 4.05 4.06 4.07 4.08 4.09 4.10 Diagnostic and statistical manual of mental disorders : DSM-5 (5th ed.). American Psychiatric Association. 2013. pp. 547–549. ISBN 9780890425541.
- ↑ 5.0 5.1 5.2 5.3 Kosten, TR; Baxter, LE (February 2019). "Review article: Effective management of opioid withdrawal symptoms: A gateway to opioid dependence treatment". The American journal on addictions. 28 (2): 55–62. doi:10.1111/ajad.12862. PMID 30701615.
- ↑ 6.0 6.1 Srivastava, AB; Mariani, JJ; Levin, FR (2020-06-20). "New directions in the treatment of opioid withdrawal". Lancet (London, England). 395 (10241): 1938–1948. doi:10.1016/S0140-6736(20)30852-7. PMID 32563380.
- ↑ Treatment, Center for Substance Abuse (2006). 4 Physical Detoxification Services for Withdrawal From Specific Substances. Substance Abuse and Mental Health Services Administration (US). Archived from the original on 25 February 2021. Retrieved 19 May 2021.
- ↑ Rehman, Saif Ur; Maqsood, Muhammad Haisum; Bajwa, Hamza; Tameez Ud Din, Asim; Malik, Mustafa N (2019). "Clinical Efficacy and Safety Profile of Lofexidine Hydrochloride in Treating Opioid Withdrawal Symptoms: A Review of Literature". Cureus. 11 (6): e4827. doi:10.7759/cureus.4827. ISSN 2168-8184. PMC 6682385. PMID 31403015.
- ↑ Zaoutis, Lisa B.; Chiang, Vincent W. (2007-01-01). Comprehensive Pediatric Hospital Medicine. Elsevier Health Sciences. p. 286. ISBN 978-0-323-03004-5. Archived from the original on 2021-08-28. Retrieved 2021-05-19.
- ↑ Abuse, United States Commission on Marihuana and Drug (1973). Drug Use in America: Problem in Perspective: Second Report. U.S. Government Printing Office. p. 305. Archived from the original on 28 August 2021. Retrieved 19 May 2021.
- ↑ Christie, M J (May 2008). "Cellular neuroadaptations to chronic opioids: tolerance, withdrawal and addiction". British Journal of Pharmacology. 154 (2): 384–396. doi:10.1038/bjp.2008.100. ISSN 0007-1188. PMC 2442443. PMID 18414400.
- ↑ Thomas, Jay (2008-01-01). "Opioid-Induced Bowel Dysfunction". Journal of Pain and Symptom Management. 35 (1): 103–113. doi:10.1016/j.jpainsymman.2007.01.017. ISSN 0885-3924. PMID 17981003. Archived from the original on 2020-07-22. Retrieved 2020-07-22.
- ↑ "Opioid withdrawal management: SA Health". www.sahealth.sa.gov.au. Archived from the original on 8 June 2021. Retrieved 28 March 2020.
- ↑ "Opioid Withdrawal Therapy: Autonomic Hypersensitivity Tamed". Taming the SRU. Archived from the original on 16 November 2020. Retrieved 19 May 2021.
- ↑ Kosten, Thomas R.; Baxter, Louis E. (2019). "Review article: Effective management of opioid withdrawal symptoms: A gateway to opioid dependence treatment". The American Journal on Addictions. 28 (2): 55–62. doi:10.1111/ajad.12862. ISSN 1521-0391. PMC 6590307. PMID 30701615.
- ↑ "Clinical Opiate Withdrawal Scale" (PDF). Archived (PDF) from the original on 2019-01-10.
- ↑ Gowing, Linda; Farrell, Michael; Ali, Robert; White, Jason M (2016-05-03). "Alpha 2 -adrenergic agonists for the management of opioid withdrawal". Cochrane Database of Systematic Reviews (5): CD002024. doi:10.1002/14651858.cd002024.pub5. ISSN 1465-1858. PMC 7081129. PMID 27140827.
- ↑ Schuckit, Marc A. (2016-07-28). "Treatment of Opioid-Use Disorders". New England Journal of Medicine. 375 (4): 357–368. doi:10.1056/NEJMra1604339. ISSN 0028-4793. PMID 27464203.
- ↑ Daniulaityte, Raminta; Carlson, Robert; Falck, Russel; Cameron, Delroy; Perera, Sujan; Chen, Lu; Sheth, Amit (2013-06-01). ""I Just Wanted to Tell You That Loperamide WILL WORK": A Web-Based Study of Extra-Medical Use of Loperamide". Drug and Alcohol Dependence. 130 (1–3): 241–244. doi:10.1016/j.drugalcdep.2012.11.003. ISSN 0376-8716. PMC 3633632. PMID 23201175.
- ↑ Borron, Stephen W.; Watts, Susan H.; Tull, Jonathan; Baeza, Salvador; Diebold, Stephanie; Barrow, Alison (July 2017). "Intentional Misuse and Abuse of Loperamide: A New Look at a Drug with "Low Abuse Potential"". The Journal of Emergency Medicine. 53 (1): 73–84. doi:10.1016/j.jemermed.2017.03.018. ISSN 0736-4679. PMID 28501383.
- ↑ Blandthorn, J; Leung, L; Loke, Y (October 2018). "Prescription opioid use in pregnancy". The Australian & New Zealand Journal of Obstetrics & Gynaecology. 58 (5): 494–498. doi:10.1111/ajo.12823. PMID 29744859. S2CID 13665351.
- ↑ 22.0 22.1 22.2 Piccotti, L; Voigtman, B; Vongsa, R; Nellhaus, EM; Rodriguez, KJ; Davies, TH; Quirk, S (1 May 2019). "Neonatal Opioid Withdrawal Syndrome: A Developmental Care Approach". Neonatal Network. 38 (3): 160–169. doi:10.1891/0730-0832.38.3.160. PMID 31470383. S2CID 181561278.
- ↑ 23.0 23.1 23.2 23.3 Patrick, Stephen W.; Barfield, Wanda D.; Poindexter, Brenda B. (26 October 2020). "Neonatal Opioid Withdrawal Syndrome". Pediatrics: e2020029074. doi:10.1542/peds.2020-029074.
External links[edit | edit source]
Categories: [Substance dependence] [Opioids] [Drug rehabilitation] [Withdrawal syndromes] [RTT]
↧ Download as ZWI file | Last modified: 05/29/2024 05:15:19 | 38 views
☰ Source: https://mdwiki.org/wiki/Opioid_withdrawal | License: CC BY-SA 3.0

 KSF
KSF