Cervical Cancer Staging
 From Mdwiki
From Mdwiki
Cervical cancer staging is the assessment of cervical cancer to determine the extent of the disease. This is important for determining disease prognosis and treatment. Cancer staging generally runs from stage 0, which is pre-cancerous or non-invasive, to stage IV, in which the cancer has spread throughout a significant part of the body.[1]
The International Federation of Gynecology and Obstetrics (FIGO) staging system is used for cervical cancer.[2][3] Prior to the 2018 update, FIGO staging of cervical cancer allowed only the following diagnostic tests to be used in determining the stage: palpation (feeling with the fingers), inspection, colposcopy, endocervical curettage, hysteroscopy, cystoscopy, proctoscopy, intravenous urography, and X-ray examination of the lungs and skeleton, and cervical conization. In 2018, FIGO updated the staging system to include imaging and pathology were as allowable methods to assess disease stage.[4]
Overview of staging[edit | edit source]
FIGO guidelines suggest that lower staging should be assigned whenever possible. Staging is determined after all imaging and pathology reports have been collected and interpreted. The stage of cervical cancer cannot be altered at recurrence.[4]
Imaging[edit | edit source]
The use of imaging can provide more information regarding prognosis, which informs treatment. The goal of staging is to identify the most appropriate treatment method and to minimize dual therapy, which can significantly impact morbidity. The imaging modality used for diagnosis should always be noted. Imaging modalities include ultrasound, MRI, CT, and positron emission tomography (PET).[5]
For primary tumors over 10 mm, MRI is the best method of radiologic assessment.[6] For nodal metastasis over 10 mm, PET-CT is the most accurate modality for diagnosis, as this can differentiate large lymph nodes that are not metastatic (for example, those that are enlarged due to inflammation or infection) from lymph nodes that are enlarged due to metastases. The diagnosis of nodal metastasis can be supplemented with surgical assessment via minimally invasive surgery or laparotomy to collect a biopsy or perform a fine needle aspiration.[7]
Pathology[edit | edit source]
As with imaging, pathologic methods used for diagnosis should always be noted for future evaluation. All cancers must be confirmed by microscopic examination.[5]
There are 10 histopathologic types of cervical cancers:[8]
- Squamous cell carcinoma (keratinizing; non-keratinizing; papillary, basaloid, warty, verrucous, squamotransitional, lymphoepithelioma-like)
- Adenocarcinoma (endocervical; mucinous, villoglandular, endometrioid)
- Clear cell adenocarcinoma
- Serous carcinoma
- Adenosquamous carcinoma
- Glassy cell carcinoma
- Adenoid cystic carcinoma
- Adenoid basal carcinoma
- Small cell carcinoma
- Undifferentiated carcinoma
Cancers can be histopathologically graded as follows:
- GX: Grade cannot be assessed
- G1: Well differentiated
- G2: Moderately differentiated
- G3: Poorly or undifferentiated
Sample collection[edit | edit source]
For microinvasive disease, clinicians should collect a specimen using a loop electrosurgical excision procedure (LEEP) or a cone biopsy. If a patient has a visible lesion, a punch biopsy may be attempted. If the specimen is not satisfactory, a small loop biopsy or cone may be required.[citation needed]
Stages[edit | edit source]
Stage 0[edit | edit source]
- The carcinoma is confined to the surface layer (cells lining) of the cervix. Also called carcinoma in situ (CIS).[4]
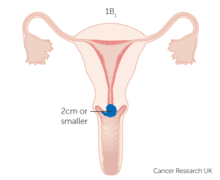
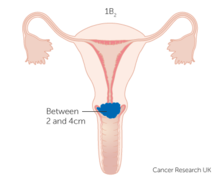
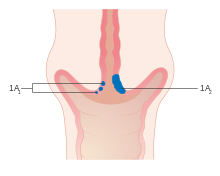 Diagram showing extent of cervical cancer tumor in blue corresponding to sub-stages IA1 and IA2.[9]
Diagram showing extent of cervical cancer tumor in blue corresponding to sub-stages IA1 and IA2.[9]
Stage I[edit | edit source]
- The carcinoma has grown into the cervix, but has not spread beyond it (extension to the corpus would be disregarded). Stage One is subdivided as follows:[4]
- IA: Invasive carcinoma which can be diagnosed only by microscopy on a LEEP or cone biopsy specimen, or on a trachelectomy or hysterectomy specimen, with deepest invasion <5 mm from the base of the epithelium. It can originate from squamous or glandular epithelium. The margins of the specimen should be reported to be negative for disease. Lymphovascular involvement must be noted to inform the treatment plan, although it does not change stage designation.[5]
- IA1: Measured stromal invasion <3.0 mm
- IA2: Measured stromal invasion ≥3.0 mm and <5 mm
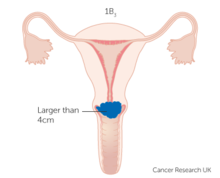
- IB: Invasive carcinoma with measured deepest invasion ≥5 mm, limited to the cervix. The lesions are clinically visible, which differentiates IB from IA. If the margins of the cone biopsy are positive for invasive disease, Stage IB1 is automatically assigned. As with Stage IA, the involvement of vascular or lymphatic spaces does not change the staging, but should be noted to inform the treatment plan.
- IA: Invasive carcinoma which can be diagnosed only by microscopy on a LEEP or cone biopsy specimen, or on a trachelectomy or hysterectomy specimen, with deepest invasion <5 mm from the base of the epithelium. It can originate from squamous or glandular epithelium. The margins of the specimen should be reported to be negative for disease. Lymphovascular involvement must be noted to inform the treatment plan, although it does not change stage designation.[5]
Stage II[edit | edit source]
- Cervical carcinoma invades beyond the uterus, but not to the pelvic wall or to the lower third of the vagina[4]
- IIA: Without parametrial invasion
- IIA1: Tumor <4.0 cm in greatest dimension
- IIA2: Tumor ≥4.0 cm in greatest dimension
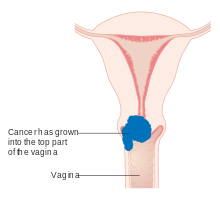 Diagram of sub-stage IIA.[10]
Diagram of sub-stage IIA.[10]
- IIB: With parametrial invasion
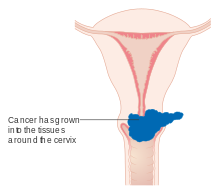 Diagram of sub-stage IIB.[10]
Diagram of sub-stage IIB.[10]
- IIA: Without parametrial invasion
Stage III[edit | edit source]
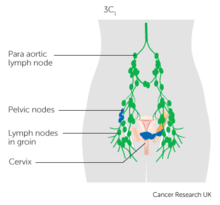
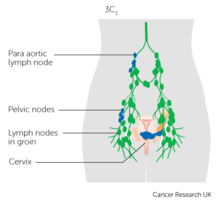
- The carcinoma involves the lower third of the vagina and/or extends to the pelvic wall and/or causes hydronephrosis or non‐functioning kidney and/or involves pelvic and/or para-aortic lymph nodes.[5]
- IIIA: Carcinoma involves the lower third of the vagina, with no extension to the pelvic wall.IIIB: Extension to the pelvic wall and/or hydronephrosis or non‐functioning kidney.
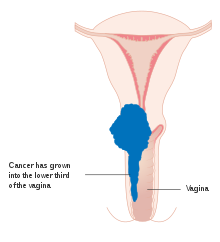 Diagram of sub-stage IIIA.[11]
Diagram of sub-stage IIIA.[11]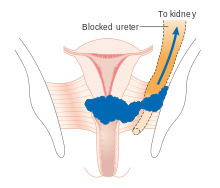 Diagram of sub-stage IIIB.[11]
Diagram of sub-stage IIIB.[11] - IIIC: Involvement of pelvic and/or para-aortic lymph nodes, irrespective of tumor size and extent
- IIIA: Carcinoma involves the lower third of the vagina, with no extension to the pelvic wall.
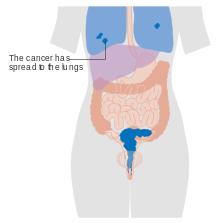
Stage IV[edit | edit source]
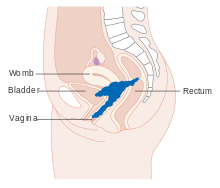
- The carcinoma has extended beyond the true pelvis or has involved (biopsy proven) the mucosa of the bladder or rectum. A bullous edema, as such, does not permit a case to be allotted to Stage IV[4]
History of cervical cancer staging[edit | edit source]
The drive to develop a staging for gynecological malignancies, including cancer of the cervix, was the need to have a uniform method to describe the extent of the disease. Comparing outcomes from different treatments could only be possible if the comparison were made for groups of patients with a similar degree of disease burden.[13]
Major Historical Timepoints[13][edit | edit source]
1929 - League of Nations Classification for Cervical Cancer
1937 - First annual report of statistics on radiotherapy outcomes in cervical cancer patients
1938 - Atlas of Cervical Cancer Staging (Heyman and Strandquist)
1950 - The International Classification of the Stages of Carcinoma of the Uterine Cervix
1954 - Founding of FIGO
1958 - FIGO becomes the official publisher of the Annual Report
1973 - Commencement of triennial publication of the Annual Report on the Results of Treatment in Gynecological Cancer
1976 - The American Joint Committee on Cancer accepts the FIGO stage grouping for gynecological cancers
2018 - Latest triennial FIGO Cancer Report[14]
The most recent updates to cervical cancer staging included in the 2018 edition marked a departure from a system based mainly on clinical evaluation to one that allows imaging and pathological methods to help determine tumor size and extent of disease to assign the stage. A major topic of debate was the impact that newer diagnostic modalities would have on low- and middle-income countries, which bear most of the disease burden.[15] The final recommendations make findings from imaging and pathology optional for staging rather than a requirement.[citation needed]
References[edit | edit source]
- ↑ "Staging". National Cancer Institute. 9 March 2015. Archived from the original on 2015-03-19. Retrieved 2018-11-07.
- ↑ "Cervical Cancer Stages". www.cancer.org. Archived from the original on 2017-01-21. Retrieved 2021-01-02.
- ↑ "Cervical Cancer Stages - NCI". www.cancer.gov. 2022-10-13. Archived from the original on 2023-05-10. Retrieved 2023-05-10.
- ↑ 4.0 4.1 4.2 4.3 4.4 4.5 Bhatla, Neerja; Berek, Jonathan S.; Fredes, Mauricio Cuello; Denny, Lynette A.; Grenman, Seija; Karunaratne, Kanishka; Kehoe, Sean T.; Konishi, Ikuo; Olawaiye, Alexander B.; Prat, Jaime; Sankaranarayanan, Rengaswamy (2019). "Revised FIGO staging for carcinoma of the cervix uteri". International Journal of Gynecology & Obstetrics. 145 (1): 129–135. doi:10.1002/ijgo.12749. ISSN 1879-3479. PMID 30656645.
- ↑ 5.0 5.1 5.2 5.3 Bhatla, Neerja; Aoki, Daisuke; Sharma, Daya Nand; Sankaranarayanan, Rengaswamy (2018). "Cancer of the cervix uteri". International Journal of Gynecology & Obstetrics. 143 (S2): 22–36. doi:10.1002/ijgo.12611. ISSN 1879-3479. PMID 30306584.
- ↑ Bipat, Shandra; Glas, Afina S.; van der Velden, Jacobus; Zwinderman, Aeilko H.; Bossuyt, Patrick M. M.; Stoker, Jaap (October 2003). "Computed tomography and magnetic resonance imaging in staging of uterine cervical carcinoma: a systematic review". Gynecologic Oncology. 91 (1): 59–66. doi:10.1016/s0090-8258(03)00409-8. ISSN 0090-8258. PMID 14529663. Archived from the original on 2022-12-10. Retrieved 2023-05-10.
- ↑ Rose, P. G.; Adler, L. P.; Rodriguez, M.; Faulhaber, P. F.; Abdul-Karim, F. W.; Miraldi, F. (January 1999). "Positron emission tomography for evaluating para-aortic nodal metastasis in locally advanced cervical cancer before surgical staging: a surgicopathologic study". Journal of Clinical Oncology. 17 (1): 41–45. doi:10.1200/JCO.1999.17.1.41. ISSN 0732-183X. PMID 10458216. Archived from the original on 2022-06-16. Retrieved 2023-05-10.
- ↑ Carcangiu, M. L. (2014). WHO Classification of Tumours of Female Reproductive Organs. Robert J. Kurman, Maria Luisa Carcangiu, C. Simon Herrington (4th ed.). Lyon: International Agency for Research on Cancer. ISBN 978-92-832-4487-5. OCLC 958387934.
- ↑ 9.0 9.1 9.2 9.3 "Stage 1 | Cervical cancer | Cancer Research UK". www.cancerresearchuk.org. Retrieved 2021-09-20.
- ↑ 10.0 10.1 "Stage 2 | Cervical cancer | Cancer Research UK". www.cancerresearchuk.org. Retrieved 2021-09-20.
- ↑ 11.0 11.1 11.2 11.3 "Stage 3 | Cervical cancer | Cancer Research UK". www.cancerresearchuk.org. Retrieved 2021-09-20.
- ↑ 12.0 12.1 "Stage 4 | Cervical cancer | Cancer Research UK". www.cancerresearchuk.org. Retrieved 2021-09-20.
- ↑ 13.0 13.1 Odicino, Franco; Pecorelli, Sergio; Zigliani, Lucia; Creasman, William T. (2008). "History of the FIGO cancer staging system". International Journal of Gynecology & Obstetrics. 101 (2): 205–210. doi:10.1016/j.ijgo.2007.11.004. ISSN 1879-3479. PMID 18199437. S2CID 35088101. Archived from the original on 2023-09-13. Retrieved 2023-05-10.
- ↑ "FIGO Cancer Report 2018". Figo. Archived from the original on 2021-09-28. Retrieved 2021-09-20.
- ↑ Bhatla, Neerja; Denny, Lynette (October 2018). "FIGO Cancer Report 2018". International Journal of Gynecology & Obstetrics. 143: 2–3. doi:10.1002/ijgo.12608. PMID 30306587.
Categories: [Oncology] [Infectious causes of cancer]
↧ Download as ZWI file | Last modified: 10/27/2023 08:30:02 | 1 views
☰ Source: https://mdwiki.org/wiki/Cervical_cancer_staging | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed:
 KSF
KSF