Midwifery
 From Nwe
From Nwe  A pregnancy check-up by a midwife |
|
| Focus | Pregnancy Childbirth Postpartum Newborn care Women's health Reproductive health |
|---|---|
| Specialist | Midwife |
Midwifery is the health science and health profession that deals with pregnancy, childbirth, and the postpartum period (including care of the newborn). Midwives may also provide continuing care of the sexual and reproductive health of women throughout their lives. Historically, the profession of midwifery was limited to women, in some cases only to those who had borne a child themselves. Due to lack of medical texts and the availability of medical education to women, their knowledge was generally derived from folk medicine and natural remedies. At times this led to accusations of witchcraft.
Today, midwifery is a recognized health profession with education and training similar to that of nursing. The profession is now open to men, although the great majority of midwives continue to be women. It can be argued that it is more appropriate to have women, particularly those who have experienced childbirth, be trained to care for women who are going through this important and intimate experience.
Definition and etymology
According to the definition of the International Confederation of Midwives, which has also been adopted by the World Health Organization and the International Federation of Gynecology and Obstetrics:
A midwife is a person who has successfully completed a midwifery education programme that is based on the ICM Essential Competencies for Basic Midwifery Practice and the framework of the ICM Global Standards for Midwifery Education and is recognized in the country where it is located; who has acquired the requisite qualifications to be registered and/or legally licensed to practice midwifery and use the title ‘midwife’; and who demonstrates competency in the practice of midwifery.[1]
The word derives from Old English mid, "with," and wif, "woman," and thus originally meant "with-woman," that is, the person who is with the woman (mother) at childbirth.[2] The word refers to midwives of either gender.
History
Ancient history
In ancient Egypt, midwifery was a recognized female occupation, as attested by the Ebers Papyrus which dates from 1900 to 1550 B.C.E. Five columns of this papyrus deal with obstetrics and gynecology, especially concerning the acceleration of parturition (the action or process of giving birth to offspring) and the birth prognosis of the newborn. The Westcar papyrus, dated to 1700 B.C.E., includes instructions for calculating the expected date of confinement and describes different styles of birth chairs. Bas reliefs in the royal birth rooms at Luxor and other temples also attest to the heavy presence of midwifery in this culture.[3]
Midwifery in Greco-Roman antiquity covered a wide range of women, including old women who continued folk medical traditions in the villages of the Roman Empire, trained midwives who garnered their knowledge from a variety of sources, and highly trained women who were considered physicians.[4] However, there were certain characteristics desired in a “good” midwife, as described by the physician Soranus of Ephesus in the second century:
A suitable person will be literate, with her wits about her, possessed of a good memory, loving work, respectable and generally not unduly handicapped as regards her senses [i.e., sight, smell, hearing], sound of limb, robust, and, according to some people, endowed with long slim fingers and short nails at her fingertips.[5]
Soranus also recommended that the midwife be of sympathetic disposition (although she need not have borne a child herself) and that she keep her hands soft for the comfort of both mother and child.[5] Pliny, another physician from this time, valued nobility and a quiet and inconspicuous disposition in a midwife.[6] There appear to have been three “grades” of midwives present: The first was technically proficient; the second may have read some of the texts on obstetrics and gynecology; but the third was highly trained and reasonably considered a medical specialist with a concentration in midwifery.[6]
Midwives were known by many different titles in antiquity, ranging from iatrinē (Gr. nurse), maia (Gr., midwife), obstetrix (Lat., obstetrician), and medica (Lat., doctor).[4] It appears as though midwifery was treated differently in the Eastern end of the Mediterranean basin as opposed to the West. In the East, some women advanced beyond the profession of midwife (maia) to that of gynaecologist (iatros gynaikeios, translated as women's doctor), for which formal training was required. Also, there were some gynecological tracts circulating in the medical and educated circles of the East that were written by women with Greek names, although these women were few in number. Based on these facts, it would appear that midwifery in the East was a respectable profession in which women could earn their livelihoods and enough esteem to publish works read and cited by male physicians. In fact, a number of Roman legal provisions strongly suggest that midwives enjoyed status and remuneration comparable to that of male doctors.[7] One example of such a midwife is Salpe of Lemnos, who wrote on women's diseases and was mentioned several times in the works of Pliny.[6]
The actual duties of the midwife in antiquity consisted mainly of assisting in the birthing process, although they may also have helped with other medical problems relating to women when needed. Often, the midwife would call for the assistance of a physician when a more difficult birth was anticipated. In many cases the midwife brought along two or three assistants.[3] In antiquity, it was believed by both midwives and physicians that a normal delivery was made easier when a woman sat upright. Therefore, during parturition, midwives brought a stool to the home where the delivery was to take place. In the seat of the birthstool was a crescent-shaped hole through which the baby would be delivered. The birthstool or chair often had armrests for the mother to grasp during the delivery. Most birthstools or chairs had backs which the patient could press against, but Soranus suggests that in some cases the chairs were backless and an assistant would stand behind the mother to support her.[7] The midwife sat facing the mother, encouraging and supporting her through the birth. The assistants may have helped by pushing downwards on the top of the mother's abdomen.
Finally, the midwife received the infant, placed it in pieces of cloth, cut the umbilical cord, and cleansed the baby.[6] The child was sprinkled with “fine and powdery salt, or natron or aphronitre” to soak up the birth residue, rinsed, and then powdered and rinsed again. Next, the midwives cleared away any and all mucus present from the nose, mouth, ears, or anus. Midwives were encouraged by Soranus to put olive oil in the baby's eyes to cleanse away any birth residue, and to place a piece of wool soaked in olive oil over the umbilical cord. After the delivery, the midwife made the initial call on whether or not an infant was healthy and fit to rear. She inspected the newborn for congenital deformities and testing its cry to hear whether or not it was robust and hearty. Ultimately, midwives made a determination about the chances for an infant's survival and likely recommended that a newborn with any severe deformities be exposed.[7]
A second-century terracotta relief from the Ostian tomb of Scribonia Attice, wife of physician-surgeon M. Ulpius Amerimnus, details a childbirth scene. Scribonia was a midwife and the relief shows her in the midst of a delivery. A patient sits in the birth chair, gripping the handles and the midwife’s assistant stands behind her providing support. Scribonia sits on a low stool in front of the woman, modestly looking away while also assisting the delivery by dilating and massaging the vagina, as encouraged by Soranus.[6]
The services of a midwife were not inexpensive; this fact suggests poorer women who could not afford the services of a professional midwife often had to make do with female relatives. Also, many families had a choice of whether or not they wanted to employ a midwife who practiced the traditional folk medicine or the newer methods of professional parturition.[7] Like a lot of other factors in antiquity, quality gynecological care often depended heavily on the socioeconomic status of the patient.
Middle Ages
During the Middle Ages in Western Europe, people relied on the medical knowledge of Roman and Greek philosophers, specifically Galen, Hippocrates, and Aristotle.[8] These medical philosophers focused primarily on the health of men, and women's health issues were understudied. Thus, these philosophers did not focus on the baby and they encouraged women to handle women's issues. In fact, William L. Minkowski asserted that a male's reputation was negatively affected if he associated with or treated pregnant patients.[9] As a result, male physicians did not engage with pregnant patients. The prevalence of this mindset allowed women to continue the practice of midwifery throughout most of the Medieval era with little or no male influence on their affairs.
Midwives learned their craft from other women within their communities and from their own childbearing experiences, because there was a lack of training within the field. This absence of training can be attributed to the lack of texts on the topic. Thus, midwives often taught upcoming midwives through their personal experiences.[9] From the time they were small girls, women who would later become midwives were present at the births of other siblings and they observed the birthing process performed by the midwife or other female family members. Men were not allowed to view this birthing process.
The fifteenth century saw advances in medical education with the emergence of European schools and universities. However, many of these early institutions excluded women from their programs and restricted their access to certain subject areas. Meanwhile men monopolized many areas of the medical industry.[9] Thus midwifery became women's primary role within the medical world. This also led to women's usage of natural remedies to help the sick and advance their practice of midwifery, which led to false accusations of witchcraft.
Midwives were involved with births from all social classes to various degrees. The poorest women were typically helped by the women in their family and their neighbors more than the midwives from the towns. In towns, government compensated midwives with "tax exempt status or a small pension" for their service within the community.[9] In more exceptional situations, if the midwife had a much respected reputation, they might also serve as court midwife.
Regulations on the practice of midwifery
Medical practitioners were subjected to more regulation in the Middle Ages. Although the medical field was becoming a male monopoly with these regulations, midwifery was still dominated by women, as men had not had schooling or education in obstetrics.
Unlike male medical practitioners, midwives did not participate in guilds or attempt to organize themselves. The organization of midwives commenced once a medical "hierarchy" was constructed "with male doctors at the top."[9] During this time period society aimed to implement midwives into this medical organization. Lawmakers hoped that regulation would improve the quality of care given by midwives.
Regulation of midwifery was also an ecclesiastical concern: Midwives were instructed on how to properly baptize newborns.[10]
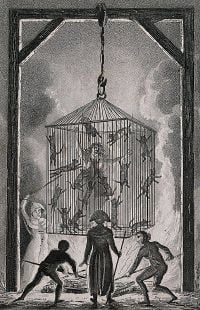
Accusations of witchcraft
Witchcraft became associated with midwifery when unsuccessful pregnancies became apparent to society. Reliance on naturalistic remedies and a lack of training caused rural midwives to have many unsuccessful deliveries during the time. When births were consistently unsuccessful, the accusations of witchcraft began. Regulations on the practice of midwifery and the early witch trials occurred during the same time period.
People feared the knowledge of midwives and equated this to the practice of witchcraft. Additionally, there was fear that midwives would not perform baptisms correctly. During this time, the church and state imposed restrictions on midwives, and required that midwives were supervised. Supervisors guaranteed that midwives followed their religious oath against the practice of witchcraft.[9] Midwives were commonly tried for witchcraft because of their medicinal knowledge. If natural remedies, unknown to the general public, were used, midwives were questioned about their associations with witchcraft.
Modern history
After the Medieval era, midwifery became more structured and professionalized from the influence of legislation passed during the later part of the era and the influence of the medical profession. Over time it became the profession that we know today as midwifery.
From the eighteenth century, a conflict between surgeons and midwives arose, as medical men began to assert that their modern scientific techniques were better for mothers and infants than the folk medicine practiced by midwives.[11][12] As doctors and medical associations pushed for a legal monopoly on obstetrical care, midwifery became outlawed or heavily regulated throughout the United States and Canada.[13]
In Northern Europe and Russia, the situation for midwives was a little easier - in the Duchy of Estonia in Imperial Russia, Professor Christian Friedrich Deutsch established a midwifery school for women at the University of Dorpat in 1811, which existed until World War I. Training lasted for seven months and in the end a certificate for practice was issued to the female students. Despite accusations that midwives were "incompetent and ignorant,"[14] some argued that poorly trained surgeons were far more of a danger to pregnant women. In 1846, the physician Ignaz Semmelweiss observed that more women died in maternity wards staffed by male surgeons than by female midwives, and traced these outbreaks of puerperal fever back to (then all-male) medical students not washing their hands properly after dissecting cadavers, but his sanitary recommendations were ignored until acceptance of germ theory became widespread.[15]
Margaret Bethune (October 2, 1820 – April 20, 1887) was a Scottish midwife who kept a detailed register of the births she attended in Largo parish in Fife. Bethune received midwifery training in Edinburgh in 1852, returning to her family in 1853, where she began working as a midwife or "howdie" in her community.[16] Bethune kept a casebook, recording 1,296 labors she attended, all within the parish of Largo, with only two maternal deaths registered. She was a respected and able midwife, and attended to the vast majority of births in her parish for several decades.[17] Her casebook is preserved in the National Records of Scotland. Bethune's register was featured in a 2015 exhibit in Edinburgh, marking the centenary of the Midwives Act of 1915.
By the late twentieth century, midwives were already recognized as highly trained and specialized professionals in obstetrics. However, the medical perception of pregnancy and childbirth as potentially pathological and dangerous still dominated Western culture. Midwives who work in hospital settings also have been influenced by this view, although by and large they are trained to view birth as a normal and healthy process.
Education and training
The education and training for a midwife is similar to that of a nurse, in contrast to obstetricians and perinatologists who are physicians (doctors). In many countries, midwifery is either a branch of nursing or has some links to nursing such as a shared regulatory body, though others regard them as entirely separate professions. Midwives are trained to recognize variations from the normal progress of labor and understand how to deal with deviations from normal. They may intervene in high risk situations such as breech births, twin births, and births where the baby is in a posterior position, using non-invasive techniques. For complications related to pregnancy and birth that are beyond the midwife's scope of practice, including surgical and instrumental deliveries, they refer their patients to physicians or surgeons. In many parts of the world, these professions work in tandem to provide care to childbearing women.
Men in midwifery
Men rarely practice midwifery for cultural and historical reasons. In ancient Greece, midwives were required by law to have given birth themselves, which prevented men from joining their ranks.
In seventeenth century Europe, some barber surgeons (barbers, who, possessing razors and coordination indispensable to their trade, performed surgical procedures including bloodletting, cupping therapy, pulling teeth, and amputation particularly for soldiers during wartime but were also used by individuals in peacetime), all of whom were male, specialized in births requiring the use of surgical instruments. This eventually developed into a professional split, with women serving as midwives and men becoming obstetricians.
Today, most developed countries allow men to train as midwives. However, it remains very rare. In the United Kingdom, even after the passing of the Sex Discrimination Act 1975, the Royal College of Midwives barred men from the profession until 1983.[18] In the US, there remain a small number of male midwives with full scope training (CNMs/CMs), comprising approximately 1 percent of the membership of the American College of Nurse-Midwives.[19]
In some Southeast Asian cultures, some or even most of the traditional midwives are men.[20]
Main areas of practice
According to the International Confederation of Midwives:
The midwife is recognised as a responsible and accountable professional who works in partnership with women to give the necessary support, care and advice during pregnancy, labour and the postpartum period, to conduct births on the midwife’s own responsibility and to provide care for the newborn and the infant. This care includes preventative measures, the promotion of normal birth, the detection of complications in mother and child, the accessing of medical care or other appropriate assistance and the carrying out of emergency measures.
The midwife has an important task in health counselling and education, not only for the woman, but also within the family and the community. This work should involve antenatal education and preparation for parenthood and may extend to women’s health, sexual or reproductive healthand child care.
A midwife may practise in any setting including the home, community, hospitals, clinics or health units.[1]
Pregnancy
A normal pregnancy lasts about nine months and has three trimesters (trimester meaning three months).[21]
Prenatal care changes as the pregnancy progresses through these trimesters. During the first trimester the midwife will take a full medical history, offer screening tests, and discuss any issues that arise during pregnancy.
The mother visits the midwife monthly or more often during the second trimester. The mother's partner and/or the labor coach may accompany her. The midwife will discuss pregnancy issues such as fatigue, heartburn, varicose veins, and other common problems such as back pain. Blood pressure and weight are monitored and the midwife measures the mother's abdomen to see if the baby is growing as expected. Lab tests may also be scheduled if called for.[22]
Third trimester
In the third trimester the midwife will see the mother every two weeks until week 36 and every week after that. Weight, blood pressure, and abdominal measurements will continue to be taken. Lab tests with additional testing may be carried out for at-risk pregnancies. The midwife discusses birthing with the mother and prepares a birth care plan.[23]
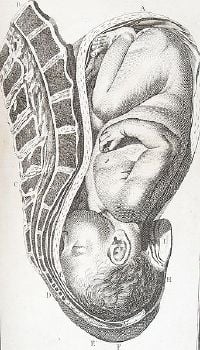
Childbirth
Midwives are qualified to assist with a normal vaginal delivery while more complicated deliveries are handled by a health care provider who has had further training. The midwife assists the baby as needed and, when fully emerged, cuts the umbilical cord or prepares it for the father to cut if so desired.
Throughout labor and delivery the mother's vital signs (temperature, blood pressure, and pulse) are closely monitored and her fluid intake and output are measured. The midwife also monitors the baby's pulse rate, palpates the mother's abdomen to monitor the baby's position, and does vaginal checks as needed. If the birth deviates from the norm at any stage, the midwife requests assistance from a more highly trained health care provider.
Following the birth, the midwife does regular assessments for uterine contraction, fundal height, and vaginal bleeding.[24]
Postpartum period
For women who have a hospital birth, full postnatal assessments of mother and baby are conducted daily whilst inpatient, or more frequently if needed.
In the community, the community midwife sees the woman at least until day ten, although not necessarily daily. Postnatal checks include neonatal screening test (NST, or heel prick test) around day five. The baby is weighed and the midwife plans visits according to the health and needs of mother and baby. They are discharged to the care of the health visitor.
Care of the newborn
At birth, the baby receives an Apgar score, assessing the baby on five different areas. The midwife checks the baby for any obvious problems, weighs the baby, and measure head circumference. The midwife ensures the cord has been clamped securely and the baby has the appropriate name tags on (if in hospital). These checks are performed as close to the mother as possible, and the midwife returns the baby to the mother quickly. Skin-to-skin is encouraged, as this regulates the baby's heart rate, breathing, oxygen saturation, and temperature, and promotes bonding.
Midwifery-led continuity of care
Midwifery-led continuity of care is where one or more midwives have the primary responsibility for the continuity of care for childbearing women, with a multidisciplinary network of consultation and referral with other health care providers. This is different from "medical-led care" where an obstetrician or family physician is primarily responsible. In "shared-care" models, responsibility may be shared between a midwife, an obstetrician and/or a family physician.
A 2013 Cochrane review revealed that "women who received midwife‐led continuity models of care were less likely to experience intervention and more likely to be satisfied with their care with at least comparable adverse outcomes for women or their infants than women who received other models of care."[25]
Midwifery-led care effects included the following:[25]
- a reduction in the use of epidurals, with fewer episiotomies or instrumental births.
- a longer mean length of labor as measured in hours
- increased chances of being cared for in labor by a midwife known by the childbearing woman
- increased chances of having a spontaneous vaginal birth
- decreased risk of preterm birth
- decreased risk of losing the baby before 24 weeks' gestation, although there appears to be no differences in the risk of losing the baby after 24 weeks or overall.
There was no difference in the number of Caesarean sections. All trials in the Cochrane review included licensed midwives, and none included lay or traditional midwives. Also, no trial included out of hospital birth.[25]
The authors concluded:
Midwife‐led continuity of care confers important benefits and shows no adverse outcomes. However, due to the exclusion of women with significant maternal disease and substance abuse from some trials of women at mixed risk, caution should be exercised in applying the findings of this review to women with substantial medical or obstetric complications.[25]
Notes
- ↑ 1.0 1.1 Definitions International Confederation of Midwives. Retrieved September 30, 2020.
- ↑ Douglas Harper, midwife (n.) Etymology Online. Retrieved September 30, 2020.
- ↑ 3.0 3.1 Jean Towler and Joan Bramall, Midwives in History and Society (Routledge Kegan & Paul, 1986, ISBN 978-0709924531).
- ↑ 4.0 4.1 Rebecca Flemming, Medicine and the Making of Roman Women (Oxford: Oxford University Press, 2001, ISBN 978-0199240029).
- ↑ 5.0 5.1 Owsei Temkin (trans.) Soranus' Gynecology (The Johns Hopkins University Press, 1991, ISBN 978-0801843204).
- ↑ 6.0 6.1 6.2 6.3 6.4 Ralph Jackson, Doctors and Diseases in the Roman Empire (Norman, OK: University of Oklahoma Press, 1988, ISBN 978-0806121673).
- ↑ 7.0 7.1 7.2 7.3 Valerie French, Midwives and Maternity Care in the Roman World Leopoldo Costa (ed.), Stravaganza, February 19, 2012. Retrieved October 1, 2020.
- ↑ Peter Dear, Revolutionizing the Sciences: European Knowledge and its Ambitions, 1500-1700 (Red Globe Press, 2008, ISBN 978-0230545168).
- ↑ 9.0 9.1 9.2 9.3 9.4 9.5 William L. Minkowski, Women healers of the Middle Ages: Selected aspects of their history American Journal of Public Health 82(2) (1992): 288–295. Retrieved October 1, 2020.
- ↑ Peter Biller and Joseph Ziegler (eds.), Religion and Medicine in the Middle Ages (York Medieval Press, 2001, ISBN 978-1903153079).
- ↑ Edwin R. Van Teijlingen, George W. Lowis, Peter G. McCaffery, and Maureen Porter (eds.), Midwifery and the Medicalization of Childbirth: Comparative Perspectives (Nova Science Publishers, 2011, ISBN 978-1560726807).
- ↑ Charlotte Borst, Catching Babies: The Professionalization of Childbirth, 1870-1920 (Harvard University Press, 1995, ISBN 978-0674102620).
- ↑ Barbara Ehrenreich and Deirdre English, Witches, Midwives and Nurses: A History of Women Healers (The Feminist Press at CUNY, 2010, ISBN 978-1558616615).
- ↑ Helen Varney, Varney's Midwifery (Jones & Bartlett Learning, 2003, ISBN 978-0763718565).
- ↑ Historical perspective on hand hygiene in health care WHO Guidelines on Hand Hygiene in Health Care: First Global Patient Safety Challenge Clean Care Is Safer Care. Retrieved October 1, 2020.
- ↑ Exhibition to celebrate centenary of new standards for midwives The Courier, October 12, 2015. Retrieved October 1, 2020.
- ↑ Jane Rendall, Elizabeth Ewan, Siân Reynolds, and Rose Pipes (eds.), The New Biographical Dictionary of Scottish Women (Edinburgh University Press, 2018, ISBN 978-1474436281).
- ↑ Theo Merz, No job for a man? Meet the male midwives The Telegraph, November 3, 2014. Retrieved October 2, 2020.
- ↑ The ACNM Core Data Survey American College of Nurse-Midwives, 2010. Retrieved October 2, 2020.
- ↑ Rosemary Gianno, 'Women are not brave enough' Semelai male midwives in the context of Southeast Asian cultures Bijdragen tot de Taal-, Land- en Volkenkunde 160(1) (2004): 31-71. Retrieved October 2, 2020.
- ↑ Prenatal care in your first trimester Medline Plus. Retrieved October 2, 2020.
- ↑ Prenatal care in your second trimester Medline Plus. Retrieved October 2, 2020.
- ↑ Prenatal care in your third trimester Medline Plus. Retrieved October 2, 2020.
- ↑ Postpartum care: What to expect after a vaginal delivery Mayo Clinic. Retrieved October 2, 2020.
- ↑ 25.0 25.1 25.2 25.3 Jane Sandall, Hora Soltani, Simon Gates, Andrew Shennan, and Declan Devane, Midwife‐led continuity models versus other models of care for childbearing women Cochrane Systematic Review - Intervention, April 28, 2016. Retrieved October 2, 2020.
References
ISBN links support NWE through referral fees
- Biller, Peter, and Joseph Ziegler (eds.). Religion and Medicine in the Middle Ages. York Medieval Press, 2001. ISBN 978-1903153079
- Borst, Charlotte. Catching Babies: The Professionalization of Childbirth, 1870-1920. Harvard University Press, 1995. ISBN 978-0674102620
- Dear, Peter. Revolutionizing the Sciences: European Knowledge and its Ambitions, 1500-1700. Red Globe Press, 2008. ISBN 978-0230545168
- Ehrenreich, Barbara, and Deirdre English. Witches, Midwives and Nurses: A History of Women Healers. The Feminist Press at CUNY, 2010. ISBN 978-1558616615
- Flemming, Rebecca. Medicine and the Making of Roman Women. Oxford: Oxford University Press, 2001. ISBN 978-0199240029
- Jackson, Ralph. Doctors and Diseases in the Roman Empire. Norman, OK: University of Oklahoma Press, 1988. ISBN 978-0806121673
- Rendall, Jane, Elizabeth Ewan, Siân Reynolds, and Rose Pipes (eds.). The New Biographical Dictionary of Scottish Women. Edinburgh University Press, 2018. ISBN 978-1474436281
- Temkin, Owsei (trans.). Soranus' Gynecology. The Johns Hopkins University Press, 1991. ISBN 978-0801843204
- Towler, Jean, and Joan Bramall. Midwives in History and Society. Routledge Kegan & Paul, 1986. ISBN 978-0709924531
- Van Teijlingen, Edwin R., George W. Lowis, Peter G. McCaffery, and Maureen Porter (eds.). Midwifery and the Medicalization of Childbirth: Comparative Perspectives. Nova Science Publishers, 2011. ISBN 978-1560726807
- Varney, Helen. Varney's Midwifery. Jones & Bartlett Learning, 2003. ISBN 978-0763718565
External links
All links retrieved November 9, 2022.
|
|||||||||||||||||
Credits
New World Encyclopedia writers and editors rewrote and completed the Wikipedia article in accordance with New World Encyclopedia standards. This article abides by terms of the Creative Commons CC-by-sa 3.0 License (CC-by-sa), which may be used and disseminated with proper attribution. Credit is due under the terms of this license that can reference both the New World Encyclopedia contributors and the selfless volunteer contributors of the Wikimedia Foundation. To cite this article click here for a list of acceptable citing formats.The history of earlier contributions by wikipedians is accessible to researchers here:
The history of this article since it was imported to New World Encyclopedia:
Note: Some restrictions may apply to use of individual images which are separately licensed.
↧ Download as ZWI file | Last modified: 02/04/2023 04:53:08 | 149 views
☰ Source: https://www.newworldencyclopedia.org/entry/Midwifery | License: CC BY-SA 3.0
 ZWI signed:
ZWI signed: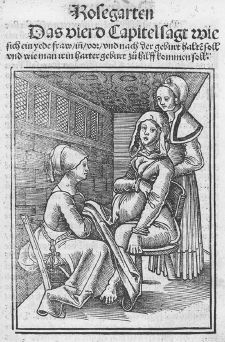





 KSF
KSF